Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.55 n.1 Cape Town Mar. 2017
PLASTIC SURGERY
Surgical anatomy of reduction mammaplasty: a historical perspective and current concepts
A O WamalwaI; T StaschII; F W NangoleIII; S O KhaingaIV
IPlastic Surgery Registrar, School of Medicine, University of Nairobi
IIConsultant Plastic, Reconstructive, Aesthetic and Hand Surgeon, Valentis Clinic, Nairobi, Kenya
IIIConsultant Plastic Surgeon & Lecturer
IVConsultant Plastic Surgeon & Associate Professor; Department of Surgery (Plastic), University of Nairobi, P.O. Box 30197, Nairobi, Kenya
SUMMARY
Reduction mammaplasty is the volumetric reduction in the bulk of the breast. Techniques have evolved from primarily reducing the breast bulk to reducing with emphasis on functional and aesthetic outcome. The deeper understanding of the surgical anatomy of the breast has guided this development. While Paulus Aegina (sixth century AD), Dieffenbach (1848) and Gaillard-Thomas (1882) set the pace in glandular reduction; Pousson (1897) and Dehner (1908) focused on breast ptosis. It took quite some time before the enigma of the vascularization to the nipple areolar complex could be solved. Progress over a decade saw Thorek's (1922) free nipple grafting replaced by the periareolar de-epithelialization introduced by Schwarzmann (1930); which subsequently gave way to the Gillies and Mclndoe (1939) skin-gland undermining technique. The era of breast remodeling while preserving the nipple areolar complex was soon ushered forward. This was driven by Arie (1957), Strombeck (1960) and Pitanguy (1961). The preservation of the subdermal plexus became crucial whilst retaining sensory supply to the breast as the pectoral fascia was spared. Skoog's (1963) nipple transposition without skin-gland undermining formed the basis for modern day reduction mammaplasty. Aesthetics was in mind throughout this period as different skin incisions were developed and advanced following Dieffenbach's small submammary incision in 1848. Surgical landmarks that ensured reproducible aesthetic outcomes were described by Penn (1955) and Wise (1956). Liposuction-assisted reduction was introduced by Teimourian in 1985 and is best utilised in patients with predominantly fatty breast tissue.
Introduction
Reduction mammaplasty is the removal of excess fatty tissue, glandular tissue and skin from the breast. Over the centuries, the priority of breast reduction surgery has evolved from mainly volumetric reduction to significant emphasis on both functional and aesthetic outcomes. Techniques in breast reduction pioneered in Europe and later modified in the United States all aimed at solving challenges encountered during this procedure.
History of reduction mammaplasty
The origins
The abnormal breast has raised concern for centuries, thus giving rise to the art and science of reduction mammaplasty. This volumetric reduction in the breast bulk is done to either alleviate clinical symptoms or to improve body image. Greek physician Paulus Aegina described breast reduction for gynaecomastia in the seventh century AD (see Figure 1), while German Hans Schaller reported breast amputation for gigantomastia in 1561 and later on Briton William Durston reported breast reduction for breast hypertrophy in 1669. However, it was the German Dieffenbach who precisely described performing a lower pole breast reduction by excising the lower two-thirds of the breast and its posterior segment whilst hiding the scar in the inframammary fold.1

Gland resection and breast ptosis
American Gaillard Thomas undertook significant glandular resection via the submammary route in 1880s. While Guinard in 1903 excised the posterior segments of the breast without skin excision, Frenchman Morestin in 1908 excised both glandular tissue with the skin. Resulting breast ptosis was tackled by Pousson in 1897 and Dehner in 1908 by anchoring the upper pole of the gland to the pectoralis major muscle or the periosteum of the third rib respectively.2 Later on, Gobell in 1927 utilized fascia lata to fix the gland to the third rib. As growing concern over breast ptosis grew, Goulian in 1971 developed the dermodermal dermopexy which provided better results than the preceding dermoglandular, dermomuscular and dermohypodermal dermopexies.
Free NACgrafting, NAC transposition and the neurovascular supply
To improve the appearance of the breast following reduction, free nipple grafting was introduced by Thorek in 1922 and Lexter in 1925.3 This technique was not popular and in 1923 Aubert described nipple transposition that permitted variability in the site and volume of breast reduction. However, this came with the difficulty of ensuring that both the remaining glandular stump and the nipple were well vascularized by either an external pedicle or internal pedicle or both. Gland remodeling was also employed to avert contour deformities, scarring and residual breast deviation.
A landmark technique was introduced in the 1930s by Schwarzmann who incorporated periareolar de-epithelialization enabling increased resection of glandular volume while maintaining the Nipple Areolar Complex (NAC) blood supply via a dermoglandular pedicle.4 Several modifications were made to this technique including the Gillies and McIndoe V-shaped resection of the upper middle breast segment. The skin-gland undermining technique limited the amount of glandular resection possible; beyond which necrosis occurred.
Subsequent techniques focused on maintaining the perforating vessels. While Maliniac in 1945 adopted a two-stage breast reduction, Barnes in 1948 and Aufricht in 1949 resected only the superior portion of the breast. Despite poorly understanding the vascular supply to the NAC, clearly the consensus was that its survival was dependent on the medially and laterally based vascular pedicles. The blood supply to the breast skin was also poorly understood as May in 1943 intimated that the NAC survived on primarily the dermal vessels rather than the subdermal plexus. Arie in 1957 proposed the principle of avoiding any undermining between skin and gland; and this ushered the age of even more extensive glandular resection and modeling whilst preserving the NAC. Strombeck in 1960 and Pitanguy in 1961 applied this and performed "keel-shaped" and "hourglass-shaped" resections. Although Strombeck's horizontal dermal pedicle flap helped maintain sensory supply to the NAC, Muller et al. reported in 1974 that none of the patients were able to lactate. Skoog is credited with developing nipple transposition without any skin-gland undermining, and this formed the basis for definition of various pedicles (see Table 1).5

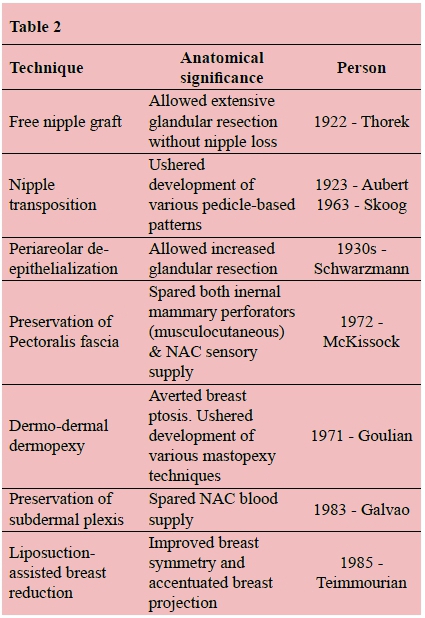
McKissock in 1972 perpetuated the importance of retaining the pectoralis fascia, essentially protecting the musculocutaneous perforator of the internal mammary artery.6 While promoting the vertical bipedicle technique, he had unknowingly not only defined vascularity to the central and inferior pedicles but also uncovered NAC sensory preservation. In retrospect, Biesenberger in 1928 had unwittingly defined the superficial glandular blood supply (septocutaneous mammary perforators) when he advocated for limited dissection of suspensory ligaments of Cooper, lest one encounters skin and breast necrosis.7 Modifications to these techniques cemented the importance of the subdermal vascularization during periareolar de-epithelialization, permitting unlimited breast reduction and remodeling. Galvao in 1983 preserved the subdermal plexus while transposing the NAC; Cardoso used three dermal pedicles, while Reno in 1985 reported a periareolar mastopexy.
Aesthetics and skin incisions
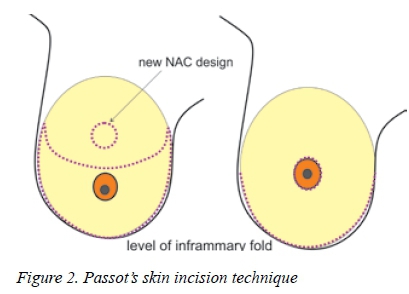
Aesthetically pleasing incisions were a priority since Dieffenbach's small submammary incision. Passot in 1925 described transposition of the nipple areolar complex (NAC) through a button-hole without a resulting vertical scar (see Figure 2).8 Hollander in 1924 proposed the inferolateral skin incision as an alternative to the Kraske-developed inverted T-incision.
Whereas Penn in 1955 emphasized bilateral uniformity of the NAC by utilising the equilateral triangle across the sternal notch and the two nipples with a distance of about 21 cm, Wise in 1956 is credited for developing the reproducible technique of designing breast skin flaps that preserve both vascular and sensory supply.
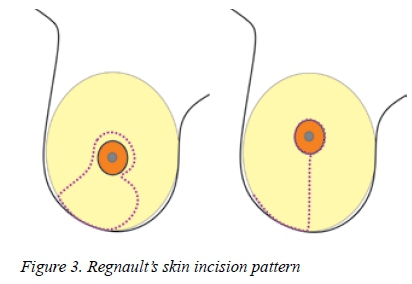
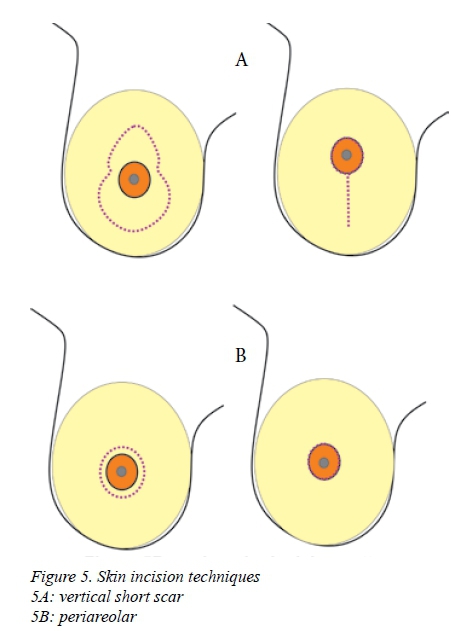
Other skin incision techniques including the B-technique by Regnault in 1974 (see Figure 3), L-plasty by Meyer and Kesselring in 1983(see Figure 4), vertical mammaplasty as described by Lassus and popularized by Lejour in 1989, and the periareolar mammaplasty with double-skin technique by Sampaio-Goes in 1991(see Figure 5) were developed to improve aesthetic outcomes by limiting scarring.

Other trends
Since the introduction of liposuction to reduction mammaplasty by Teimmourian in 1985, the technique was then popularized by Matarazzo and Courtiss in 1991 and Courtiss in 1993.9 Breast reduction with ultrasound-assisted lipoplasty technique has also been utilised. Liposuction is for predominantly fatty breasts with minimal ptosis and can be used as an adjunct to gland resection.
Current concepts in the surgical anatomy of reduction mammaplasty
Lying on the anterior thoracic wall, the base of the breast extends from the second to sixth ribs vertically, and from the sternal edge to near the midaxillary line horizontally. The axillary tail of Spence extends into the medial axillary wall and may rarely be found adjacent to the axillary lymph nodes. The varying ratio of fatty tissue to glandular tissue influences choice of technique in reduction mammaplasty. Predominantly fatty breasts are ideal for liposuction-assisted reduction. Postoperative liposuction applied to the preaxillary and lateral chest wall region accentuates the breast projection and can optimize symmetry. As the loose connective tissue of the retromammary space delineates the breast from the underlying pectoralis major, the suspensory ligaments of Cooper anchor the breast onto the pectoralis major fascia and the dermis. Lax ligaments result in breast ptosis and exaggeration of the inherent fuller lower pole of the breast. Wuringer et al. described a fibrous connective tissue septum, containing vessels and nerves, running horizontally from the pectoral fascia along the fifth rib towards the nipple.10 Its extensions, the medial and lateral ligaments, hold the breast as sling and can be utilised in reshaping the breast. Successful postoperative lactation depends on preservation of underlying breast parenchyma.
Prior to reduction, the breast should be defined in terms of the height or diameter of the base, the forward projection and any ptosis present (glandular or cutaneous). The midsternal vertical line and the breast meridian are important fixed surgical landmarks used to aid the surgeon to determine new nipple position and design the skin flaps in a standing patient. This should be correlated to the patient's height, weight, structure of rib cage and spine, soft tissue thickness and patient's wishes. The utility of patient anthropometrics as a predictor of resection weight in reduction mammaplasty is well documented.11
The arterial supply to the breast is derived from branches of the internal mammary artery, lateral thoracic artery, intercostal artery and pectoral branch of the thoracoacromial axis (see Figure 6). Variable anastomoses exist among these vessels providing a robust supply to the breast skin, via the subdermal plexus and the breast parenchyma. The internal mammary artery provides about 60% of the blood supply to the breast mainly through its second and third perforating branches, usually found at the breast meridian. This superficial source supplies the superior or superomedial based pedicle.12 A large musculocutaneous perforator (through the pectoralis major muscle) from either the fifth or sixth branch sustains the inferior or central based pedicle and is found just medial to the breast meridian about 2 to 4 cm above the inframammary fold. The medially or superomedially based pedicle is the basis for the Hall-Findlay developed vertical reduction mammaplasty technique (see Figure 7).
The posterior intercostal perforators, mainly the fourth and fifth, contribute to the inferior pedicle. The musculocutaneous and fasciocutaneous mammary branches of the lateral thoracic artery provide about 30% of the blood supply to the breast. Prudent infiltration of adrenaline is warranted to minimize bleeding. The blood supply to the NAC is symmetric and is mainly and most reliably from superomedial source vessels (internal mammary artery).13 Venous drainage from the glandular tissue and circumareolar venous plexus is by valve-containing veins accompanying the arterial supply. This system can be significantly compromised during gland remodeling or after making a circumferential incision of the areola. To minimize residual gland venous congestion with increased fullness, a full thickness pedicle resection should include its superficial venous drainage.
In the presence of varied vascular anatomy and varied glandular distribution within the breast, strict adherence to preoperative patient markings for proscribed skin resection patterns and pedicle design may lead to unpredictable results. It is often tricky to avoid these undesirable suboptimal and sometimes disastrous outcomes, like NAC necrosis and breast asymmetry (breast volume or NAC complex). Revisionary or secondary breast surgery calls on surgical experience to avert further dismay. Thus the steep learning curve in reduction mammoplasty.
The NAC receives sensory innervation mainly from the lateral cutaneous branch of the fourth intercostal nerve.14 The posterior branch runs along the pectoralis fascia till the level of the breast meridian where it makes an almost perpendicular turn, vertically coursing towards the NAC (see Figure 8). Preservation of a full thickness pedicle with its attached pectoralis fascia is crucial to NAC innervation which serves the suckling reflex. During tissue resection, unnecessary exposure of the pectoralis fascia risks increased bleeding and loss of sensation. Additional supply to the NAC is via a plexus formed by the terminal fourth and fifth anterior cutaneous nerves, as well as the fifth lateral cutaneous intercostal nerve.

When performing a free nipple graft, the nipple-areolar graft should be placed on a richly innervated dermal bed to facilitate prompt sensory recovery. Current indications for free NAC graft include: female to male gender reassignment, presence of severely redundant inelastic skin (present after massive weight loss, in severe gynaecomastia or gigantomastia) and intraoperatively determined threatened NAC viability.15 There is no consensus on cut-off weight of breast tissue excised that warrants free NAC graft.
The dermatomal sensory innervation to the breast is provided by the third to fifth lateral cutaneous branches to the lateral breast region, the second to fifth anterior cutaneous nerves to the medial side and minor contribution from the intermediate group of supraclavicular nerve to the superior and lateral aspect of the breast (see Figure 9).

Conclusion
The evolution of techniques in reduction mammaplasty was guided by the better understanding of the surgical anatomy. In appreciating this, a plastic surgeon's goal is to achieve a predictable result, retain nipple sensitivity with possibility of lactation, and obtain an excellent aesthetic outcome. However, variable anatomy still poses a challenge and suboptimal results may result, irrespective of adherence to surgical principles.
Conflict of interest
The authors declare that we have no competing interests.
REFERENCES
1. Dieffenbach JF. Die extirpation der bruestdruese. In: Dieffenbach JF. (ed.) Die Operative Chirurgie, Leipzig: Brockhaus; 1848: 359-73. [ Links ]
2. Pousson M. Bulletin et Memoire de la Societe de Chirurgie de Paris. 1903;26:597. [ Links ]
3. Thorek M. Possibilities in reconstruction of the human form. NY Med J. 1922;116:572-5. [ Links ]
4. Schwarzmann E. Die technic der mammaplastik. Chirurgica. 1930; 2:932-43. [ Links ]
5. Skoog T. A technique of breast reduction. Transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126: 453-65. PMID: 14072329 [ Links ]
6. McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49(3):245-52. Available from: http://dx.doi.org/10.1097/00006534-197203000-00001. PMID: 4551235 [ Links ]
7. Biesenberger H. Eine neue method der mammaplastik. Zbl Chir. 1928; 38:2382-7. [ Links ]
8. Passot R. La correction esthetique du prolapses mammaire par le procede de la transposition du mamelon. Presse Med. 1925;33:317. [ Links ]
9. Teimourian B, Massac Jr E, Wiegering CE. Reduction suction mammaplasty and suction lipectomy as an adjunct to breast surgery. Aesthetic Plast Surg. 1985; 9(2):97-100. Available from: http://dx.doi.org/10.1007/bf01570336. PMID: 4025056 [ Links ]
10. Wuringer E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg. 1998;101(6):1486-93. Available from: http://dx.doi.org/10.1097/00006534-199805000-00009. PMID: 9583477 [ Links ]
11. Kececi Y, Sir E. Prediction of Resection Weight in Reduction Mammaplasty Based on Anthropometric Measurements. Breast Care (Basel). 2014;9(1): 41-5. Available from: http://dx.doi.org/10.1159/000358753] [PMID: 24803886] [ Links ]
12. Corduff N, Taylor GI. Subglandular breast reduction: the evolution of a minimal scar approach to breast reduction. Plast Reconstr Surg. 2004;113(1):175-84. Available from: http://dx.doi.org/10.1097/01.PRS.0000095945.27892.48. PMID: 14707635 [ Links ]
13. Seitz IA, Nixon AT, Friedewald SM et al. 'NACsomes": A new classification system of the blood supply to the nipple areola complex NAC) based on diagnostic breast MRI exams. J Plast Reconstr AesthetSurg. 2015;68(6):792-9. Available from: http://dx.doi.org/10.1016/J.BJPS.2015.02.027. PMID: 25733199 [ Links ]
14. Purohit S. reduction mammoplasty. Indian J Plast Surg. 2008;41(Suppl):S64-79. PMID: 20174545 [ Links ]
15. Erian A, Dass A. Free nipple areolar graft reduction mammaplasty. In: Shiffman MA. (Ed.). Mastopexy and breast reduction: Principles and practice. Berlin Heidelberg: Springer- Verlag; 2009:555-6. [ Links ]
 Correspondence:
Correspondence:
A O Wamalwa
aleoke@gmail.com














