Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.55 no.1 Cape Town Mar. 2017
PLASTIC SURGERY
The circumareolar approach to gynecomastia and transgender surgery: modifications to provide correct nipple areolar complex position and shape
T Jay; K Segwapa
Department of Plastic and Reconstructive Surgery Sefako Makgatho Health Science University, Pretoria South-Africa
ABSTRACT
BACKGROUND: In surgery for gynaecomastia, excision with minimal scarring and correct position of the nipple areolar complex (NAC) are key to a successful outcome. We report on a pilot study on the use of a circumareolar excision and the use of mathematical vector calculation to position the NAC and execute surgery and report on the outcomes.
METHODS: From 2014 to 2015, the authors operated on 9 gynecomastia or transgender patients. Based on research performed by Gertrude Beer, Beckenstein and Shulman we designed a mathematical modification of the technique described by Persichetti to provide correct NAC positioning as well as aesthetically pleasing NAC shape. We utilised the technique in 6 patients, 4 males with gynecomastia and 2 transgender patients. Liposuction was performed as an adjunct as needed
RESULTS: In 5 of the patients, the NAC did move in the direction of the desired vector. The NAC was on average within 0.4 cm of the desired nipple to mid-sternal position. The lateral movement averaged 0.6 cm. We found the modified circumareolar approach to deliver good aesthetic results with predictable NAC movement. Seroma formation was the most common complication.
CONCLUSION: The mathematically modified circumareolar approach to transgender and gynecomastia surgery may provide better aesthetic outcomes. Several factors need to be considered in deciding how the oval shaped vector should be designed intraoperatively. The study was limited by small sample size and short follow-up.
Gynecomastia refers to enlargement of the male breast. Hormonal changes play a role, thus changes are observed during infancy, adolescence and advanced age.1 Histologically, breast tissue may consist of various amounts of ductal tissue, stroma or fat.2 Whilst the most common cause of gynecomastia remains idiopathic, there are many other causes (pharmacological, endocrine, neoplastic or physiological) that need to be considered. Patients deserve a thorough work-up before surgery is considered (Figure 1). Female to male transgender patients request the removal of breast tissue as part of the desired transformation from female to male phenotype.
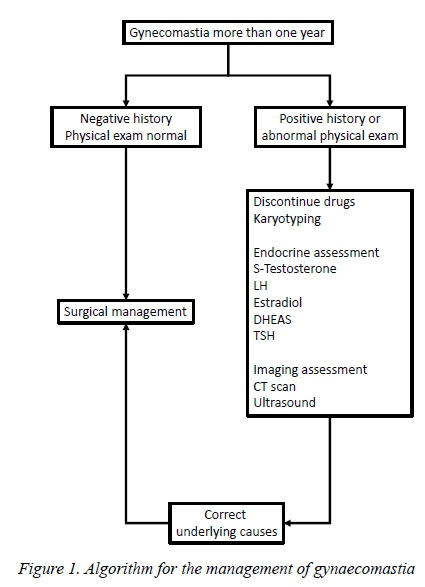
Florid gynecomastia presents with increased ductal tissue, vascularity and minimal fat. Fibrous types have more stromal fibrosis and few ducts. The intermediate type is a mixture between these entities. The fibrous type is more common where gynecomastia has been present for more than one year. Various classification systems have been described, the most useful of these being that of Simon, Hoffman and Kahn3 (Table 1).
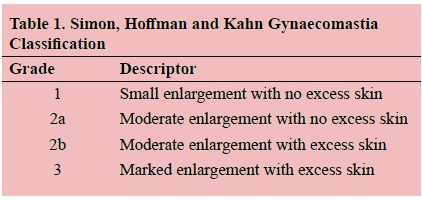
Traditional treatment techniques include liposuction for Simon grade 1, 2a and 2b. Alternatively, a peri-areolar incision at the junction of the skin and areola is utilised. When skin resection is performed for Simon grade 2b and 3 lesions, a multitude of techniques is used including superior and inferior peri-areolar incisions, omega incisions, nipple transpositions on pedicles and liposuction with skin excision.1
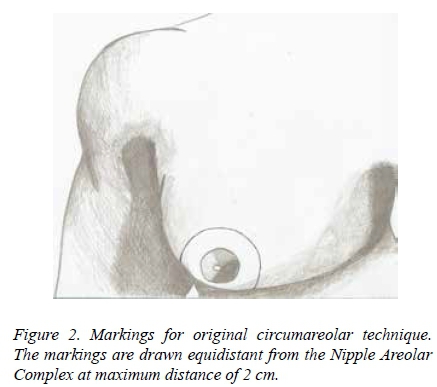
Paolo Persichetti's technique described in 2001 provided for the concentric circle design with a maximum 2 cm distance from the nipple areolar complex (NAC). The NAC was not purposefully moved on the chest, although retrospectively the NAC ended up higher and more medial on the chest than planned for. The NAC was round in shape.5
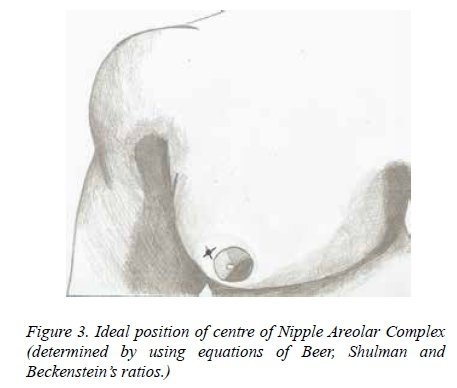
According to studies done by Gertrude Beer in 2001, 91 per cent of males have oval shaped NAC's, with only 5 per cent of males having round nipples. Beer mathematically derived an equation by which the ideal distance between the nipple and the mid-sternal line was determined.6 This position could be correlated with studies done by Shulman and a ratio proposed by Beckenstein. 7,8 These methods have never been applied to the Persichetti technique. As noted by Lindsay, the tendency was to place the nipples too high or medially on the chest in transgender patients. The study sought to correct this whilst using a technique that causes less scarring than that of traditional techniques.9
The aim of this pilot study was to determine correct NAC position in transgender and gynecomastia patients utilising scientific calculations and modification of the Persichetti technique and evaluate the placement and final cosmetic result.
Patients and Methods
A prospective study was performed at Dr George Mukhari Academic Hospital from January 2014 to February 2015.
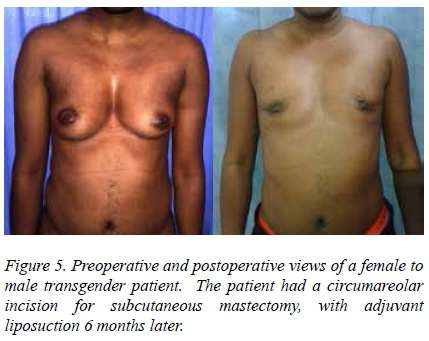
The authors operated on 9 patients with either gynecomastia or requiring transgender subcutaneous mastectomy. Patients could be operated with traditional submammary incisions or a circumareolar approach where the NAC would be moved. Explanations were given of these techniques with the aid of drawings or pictures. Of the 9 patients, 6 patients (4 with idiopathic gynecomastia, and 2 female to male transgender patients) opted to undergo gynecomastia surgery or subcutaneous mastectomy utilizing a periareolar or circumareolar approach. Three patients were excluded as they opted for other techniques. Two patients had Simon grade 2b, and 2 patients had Simon Grade 3 gynecomastia. Two patients were transgender females with 36B-cup sized breasts. The patients were between the ages of 7 and 41 years old. Informed consent was obtained.
The height of the patients was measured from heel to vertex with a standard height measuring device. The chest circumference was measured using a measuring tape at the level of the NAC. The original nipple to mid-sternal line was measured, as well as the right and left suprasternal notch to nipple distances. The measurements were performed with the patient in the upright position. These measurements were recorded on a data sheet and data subsequently entered into electronic tables.
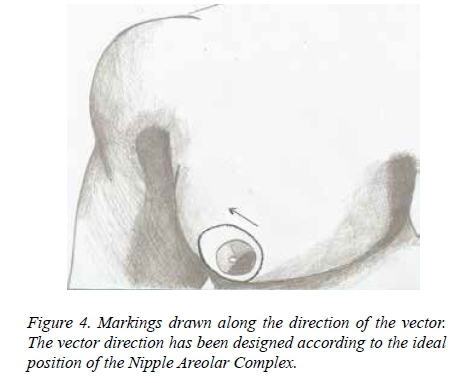
Utilising the equation provided by Gertrude Beer the ideal inter-nipple distance was determined by 2x (2.4 + (0.09 x thoracic circumference at nipple level)). According to research done by Shulman the ideal suprasternal notch to nipple distance was determined by (0.120 x height of the patient in cm) -2.782. A value ranging between 18.5 cm and 21.5 cm was within the normal range according to Beer. (20 + - 1.5 cm) A value between 16.8cm and 19.94cm was within the normal range according to Shulman. (18.37+ - 1.57). The ratio of the original measurements was also compared to ratios derived from Beckenstein's studies. According to this the ratio of inter-nipple distance, supra-sternal notch to nipple distance is equal to 1:1.05 (21cm:20 cm). By considering the difference between the ideal NAC position and the original NAC position, a vector was determined for movement of the NAC during surgery. According to this vector, the circumareolar incision is drawn to be oval in shape rather than round and angled in a superior or inferior direction depending on whether the NAC needs to be moved up or down. Consideration needs to be given to the fact that even in the absence of this angulation, the NAC is likely to move 1-2 cm up on the chest postoperatively. Lindsay proposed the vector may often be in a lateral direction, as male NACs tend to be more laterally located on the chest. 9 Based on studies by Gertrude Beer the NAC was designed to run parallel to the fibres of the pectoralis major.6
Incisions were made around the junction of the skin and the NAC and along the oval shaped line drawn along the vector of movement. In 1 patient, the NAC was not moved in the direction of a vector as the patient was a child and time was given for growth and development. As far as possible, the width of the skin to be removed was kept to a maximum of 2 cm, but certain parts of the oval had broader sections removed. Skin in between these two lines was excised and de-epithelialisation performed (Figures 2, 3 and 4). A semi-circular incision was performed below the NAC and a superomedial pedicle developed. One centimetre of tissue was left posterior to the areola to ensure adequate blood supply. Breast tissue was resected in all four quadrants, removed and weighed. Haemostasis was obtained and bilateral quarter inch drains left in situ through an inferolateral incision. For closure, Monocryl 4/0 was used to approximate the parenchyma and Monocryl 4/0 or PDS utilised to do a subcutaneous purse-string suture to close the skin around the NAC. A light compression bandage was wrapped around the chest postoperatively. A compression garment was worn for 4 weeks postoperatively.
The position of the NAC immediately postoperatively was measured and recorded. The position of the NAC at between 4 and 6 months postoperatively was measured and recorded and compared to original measurements, as well as measurements done in the immediate postoperative setting. Final follow-up was at 1 year.
The procedure was followed with liposuction 3-6 months later if required. NAC revisions to reduce NAC size was performed on those who requested it at 3-6 months postoperatively.
Results
Patients' heights ranged from 126 to 175 cm (average 163 cm). Chest circumference ranged from 62 cm to 100 cm (average 84 cm).
In 5 of the 6 patients, the NAC did move in the direction of the desired vector. There was a marked difference in measurements done prior to surgery, immediately postoperatively and at 4-6 months follow-up.
The nipple placement comparator measurements are shown in Table 2. In the immediate postoperative setting, the NAC position was on average within 0.2 cm of the desired nipple to mid-sternum position (range 0 - 0.5 cm).
There was a progressive lateral movement of the NAC between immediate postoperative measurements and at 6-month follow-up. The lateral movement ranged from 0.4 to 0.8 cm. Average movement was 0.6 mm in a lateral direction. The final NAC was on average within 0.4 cm of the desired nipple to mid-sternum position.
Between the immediate postoperative suprasternal notch to nipple distance (SSNN) and the 6-month follow-up SSNN there was an average of 0.9 cm difference, with NAC moving in an inferior direction. The range of movement was from 0.2 to 1.6 cm.
Combining the medial, lateral and inferior movements of the NAC consistently gave a vector in the desired direction at immediate postoperative follow-up as well as at 6-month follow-up period.
All 6 patients were consistently satisfied with the cosmetic appearance of the NAC and chest postoperatively, at 6-month follow-up and at 1-year follow-up. Two patients requested liposuction (both transgender patients) and 3 (2 transgender and 1 gynecomastia patient) requested reduction in NAC size which was performed with satisfactory cosmetic results. All patients were satisfied with the amount of scarring.
Examples of the aesthetic outcomes are shown in Figures 5-7.


Discussion
The position of the NAC may be altered during the complete circumareolar technique. The ideal position of the NAC on the male chest may be derived from mathematical equations based on the work done by Beckenstein, Beer and Shulman in their published works. In all patients the NAC moved by means of changing the circular shape of the original Persichetti incision to an oval shape drawn by means of a vector in the direction of a point on the chest that represents this ideal nipple position.
There remains a variation in what is deemed an aesthetically pleasing suprasternal notch to nipple distance between authors. This measurement was also the most difficult to control during surgery. The inter-nipple distance was easier to manipulate. In keeping with Lindsay's findings, the NAC position should be moved inferior on the chest rather than superior. It is the natural tendency of the NAC to move superiorly during circumareolar techniques as demonstrated by Persichetti, and this must be born in mind during planning of surgery.
Other methods utilised in practice to determine correct NAC position include placing the NAC just medial to the border of the pectoralis major or in the 5th intercostal space. These structures however are not always easy to palpate in the obese patient, and once again there is variation in position between patients. The mathematical equations, though initially cumbersome, give a more scientific base for determining correct NAC position.
There was some variation between immediate postoperative results and results after 4-6 months with the NAC moving in an inferolateral position. This appeared to be of insignificant consequence as the NAC was still on average within the range described by Shulman and Beer.
Two patients developed uncomplicated seromas postoperatively, and this underscores the importance of using a pressure bandage for one month over the chest postoperatively, as well as limiting excessive movement or exercise for six weeks postoperatively. No other complications were noted. NAC revision was offered to 3 patients to reduce the size of the NAC, but none were dissatisfied with initial post-operative appearance. It must be born in mind that the size of the NAC may increase with postoperative stretching of tissues, so another option may be to make the NAC smaller from the outset, and to use a permanent suture such as Polytetrafluoroethylene.
Another compromise to consider is that, although the normal oval NAC is usually aligned parallel to the fibres of the pectoralis major, this may need to be compromised if an oval vector is designed with a downward slant. It is up to the artistic discretion of the surgeon to decide which of these two suggestions or rules will be followed, namely orienting the NAC in a direction parallel to the fibres of the pectoralis muscle or moving the NAC in a lateral and downward position.
In conclusion, the correct NAC position may be determined by mathematical equations, but several factors need to be considered in deciding how the oval shaped vector should be designed intraoperatively. These factors include the natural tendency of the NAC to move upward during surgery, the natural tendency of the NAC to move in an inferolateral direction postoperatively, and the influence of liposuction used as an adjunct. Of greater importance may be the attempts to ensure symmetry in final position between the two nipples. The study was limited by small sample size and short follow-up. A larger study with separate or comparative evaluation of transgender and gynecomastia patients may be of value.
REFERENCES
1. Thorne CH. Grabb and Smith's Plastic Surgery 7th Ed. Lippencott, Williams and Wilkens. 2014. [ Links ]
2. Hage JJ, van Kesteren PJM. Chest-wall contouring in female- to-male transsexuals: Basic consideration and review of the literature. Plast. Reconstr. Surg. 1995;96:386. [ Links ]
3. Simon BE, Hoffman S, Kahn S. Classification and surgical correction of gynecomastia. Plast. Reconstr. Surg. 1973;51:48. [ Links ]
4. Letterman G, Schuster M. The surgical correction of gynecomastia. Ann Surg. 1969;35:322. [ Links ]
5. Persichetti P, Berloco M, Casadei RM, Marangi GF, Di Lella F, Nobili AM. Gynecomastia and the Complete Circumareolar Approach in the Surgical Management of Skin Redundancy. Plast. Reconstr. Surg. 2000;948. [ Links ]
6. Beer M, Srecko B, Burkhardt S, Morgenthaler W, Infanger M, Meyer V. Configuration and Localization of the Nipple-Areola Complex in Men. Plast.Reconstr. Surg. 2001;1947. [ Links ]
7. Shulman O, Badani E, Wolf Y, Hauben DJ. Appropriate Location of the Nipple-Areola Complex in Males. Plast. Reconstr. Surg. 2000;348. [ Links ]
8. Beckenstein MS, Windle BH, Stroup RT Jr. Anatomical parameters for nipple position and areolar diameter in males. Ann. Plast. Surg. 1996;36:33. [ Links ]
9. Lindsay WRN. Creation of a male chest in female transsexuals. Ann Plast. Surg. 1979;3:39. [ Links ]
 Correspondence:
Correspondence:
T Jay
drtonijay@gmail.com














