Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.4 Cape Town Nov. 2016
PLASTIC SURGERY
Macromastia and gigantomastia: efficacy of the superomedial pedicle pattern for breast reduction surgery
V Chetty; E Ndobe
ABSTRACT
BACKGROUND: Reduction mammoplasty procedures in patients with macromastia and gigantomastia can prove a major challenge to the plastic surgeon. Although several techniques have been described to reduce very large breasts, they can often result in vascular compromise to the nipple-areola complex (NAC) and skin flaps, decrease in NAC sensation and inability to breast-feed. The superomedial pedicle (SMP) procedure is often used in patients with moderate to large breast reductions. For extremely large breast reductions, macromastia and gigantomastia breast amputation with a free nipple graft is often recommended. For large resections and long suprasternal notch-nipple (N-N) distances there is no consensus in terms of approach
OBJECTIVE: To evaluate the efficacy and complication rate of the SMP reduction mammoplasty technique for extremely large, macromastia and gigantomastic breasts at two institutions in Johannesburg
METHODS: Retrospective review of patient records with macromastia and gigantomastia who had undergone the SMP technique reduction mammoplasty between 2008 and 2012. Complications were assessed at 1 week, 3 weeks, 6 months and a mean of one year postoperatively
RESULTS: There was a total of 31 patients, 62 breasts, with macromastia and gigantomastia who had an SMP pattern of reduction. The mean age was 30.1 years, mean BMI was 28.1 and average resection weight from each breast was 1835 g. The mean N-N was 44.13 cm. The majority, 90% of patients had a good aesthetic outcome with less than 20% having any long-term complications, which were all relatively minor
CONCLUSION: The SMP reduction mammoplasty efficiently reduces extremely large breasts while preserving the vascular integrity and sensation of the NAC, while simultaneously providing a well-shaped, projecting breast in macromastia and gigantomastia patients
Key words: SMP, NAC viability, reduction mammoplasty.
Introduction
Extremely large and oversized breasts can be disturbing to women by causing a host of both physical as well as psychological symptoms. Macromastic or gigantomastic breasts are usually heavy and pendulous with nipples and areolas facing down.1,2 Macromastia is defined as an excess of breast tissue greater than 1 (> 1) and less than (< 2) 2 kg per breast. Gigantomastia is defined as a resection weight above 2.0 kg.13
Large volume breasts cause shoulder, neck and back pain, distortion of posture and often skeletal problems.1,2 Rashes under the breast are not uncommon. In more severe cases, the chest weight can cause breathing difficulty, which can make exercise difficult or impossible.3,4 The large breast size can dominate a woman's appearance and contribute to a poor quality of life.5,6 Bilateral breast reduction (BBR) offers advantageous physical benefits. Psychological benefits are vast and include improved self-esteem, sexual function, quality of life, as well as improving related anxiety and depression.7,8
Long-term functional and aesthetic results after BBR remain important aspects for evaluating the success of different surgical techniques.
The SMP reduction technique has been previously demonstrated as a safe and effective method of reduction in cases of mild to moderate hypertrophy. They also show less bottoming out of the inferior mammary pole compared to inferior pedicled techniques. Results have not been previously published for the use of the SMP procedure in reduction of large or gigantic breasts with long N-N distances. The aim of this study, therefore, was to determine the efficacy of the SMP in patients with extremely large breasts, macromastia and gigantomastia with long N-N distances.
Patients and methods
This study was a retrospective review of patients with macromastia and gigantomastia who underwent a SMP reduction pattern, performed at the Rand Clinic and Chris Hani, Baragwanath hospitals between 2008 and 2012.
Inclusion criteria were healthy females, aged between 19 and 59 years, no previous breast surgery, BMI less than or equal to (<) 35 kg.m2 and non-smokers. Other inclusion criteria included a breast resection weight of greater than 1500 g per breast, and an N-N distance of greater than (>) 40 cm. Women with poorly controlled co-morbid illnesses were excluded. Two surgeons performed all procedures. Approval was obtained from the Human Research Ethics Committee, Medical University of the Witwatersrand.
The preoperative patient assessment followed routine assessment guidelines for BBR patients.3
Surgical markings and technique
The patient was marked in the standard manner for BBR with SMP and Wise pattern skin excision and closure.9 The technique needed to be adapted for the patients with macromastia and gigantomastia as follows:
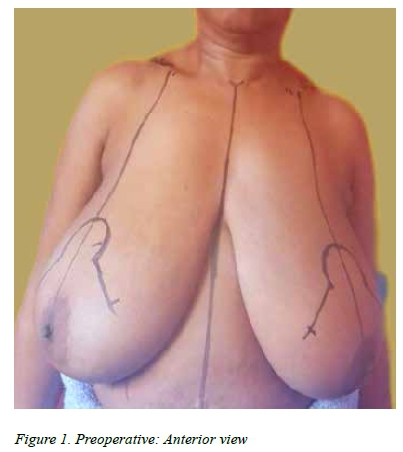
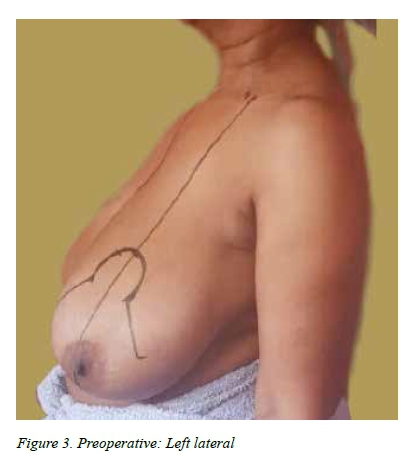
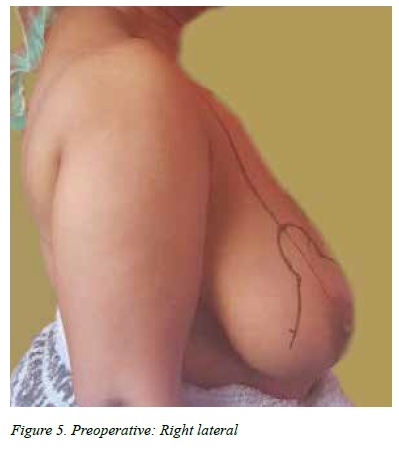
• The patients were marked in the standing position (Figure 1).
• The new nipple position is marked on the breast meridian.
• A deliberate decision was taken to err on marking the new nipple position lower, rather than too high. The new nipple was marked at a slightly lower mean height, of 23-24 cm.
The SMP pattern is marked with a base as broad as possible in the superomedial quadrant, while still making allowance for the pedicle to rotate away from the midline into the top of the keyhole of the Wise pattern. Avoid torsion. The new NAC is preserved on a dermoglandular pedicle based superior and medially. Inferiorly vertical and horizontal ellipses of parenchymal tissue are removed en bloc. Specifically, the lateral breast pillar is thinned while the medial pillar is kept comparatively full. Of importance to note in this method is to limit the undermining of the skin from the underlying breast parenchyma of both the pillars. The NAC is preserved and the parenchyma under the dermis is maintained at a minimum of 2 cm thickness. Preserve the superficial tissue. The inferior boarder of the SMP becomes the lateral pillar entering the Wise keyhole. Vertical pillar sutures are used to provide additional shaping of the breast. Meticulous hemostasis reduces the chances of hematoma, one of the main causes of delayed wound healing. The final tailoring is performed in a curvilinear fashion to mimic the curve on a spherical surface. The skin envelope is closed in the regular inverted T- pattern.
Postoperative dressings to support the breast are essential, with a window facility to inspect the nipple and areola without opening the dressing. Additional post operative care is as for routine BBR. A snugly-fitting bra is worn immediately postoperatively and the patient is advised to continue its use for a period of 3 months.
Data collected included demographics, size of breast both by standard distances measured and weight of breast tissue removed. Early and late complications were assessed and included: loss of sensation, nipple viability, changes in pigmentation and scarring. An assessment of the aesthetic outcome including projection, symmetry, shape and scar formation was done after 1 year by 4 independent medical practitioners.
Results
There were 31 patients who met the inclusion criteria for macromastia and gigantomastia which had been reduced by the SMP reduction pattern. All procedures went well and all patients were discharged 1-2 days postoperatively.
The mean (SD) age of the cohort was 29.3 (9.27) years and a mean (SD) BMI of 28.1 (2.5) kg. The mean (SD) weight removed from the right breasts was 1842 (0.31) g and from the left breasts was 1828 (0.31) g. There was no significant difference in weight removed between the right and left breasts (p=0.4216, paired t-test).
The mean (SD) notch to nipple length (N-N) was 44.7 (19.2) cm for the right breast and 44.8 (20.1) cm for the left breast with no significant difference (p=0.0707 paired t-test) between the right and left breasts. The mean (SD) elevation distance of the NAC, was 22.4 (3.3) cm for the right breast and 22.8 (3.3) cm for the left breast. The elevation distance for the left breast was significantly longer than the right breast (p=0.0023 paired t-test).
Complications were minor and self-limiting (Table 1). All patients showed preserved NAC viability postoperatively. There were no patients with necrosis greater than 15% of the superficial NAC surface area. In a quarter of patients, there were small areas of wound breakdown occurring at the T-junction within the first weeks which were managed conservatively with wound dressings and prophylactic antibacterial gel. None required surgical intervention. Fat necrosis was clinically diagnosed in 4 breasts during the postoperative periods, all small, treated conservatively, and surgery was not deemed necessary. Final NAC sensation was tested at a mean time of one year. 95.2% of NAC maintained sensation post operatively. Of these 14.5% experienced a decrease. 4.8% lost NAC sensation altogether as a result of surgery. The median extent of NAC hypopigmentation was 20%. No problems of NAC hyperpigmentation were recorded (Table 4).
There was no significant difference over time in sensation changes for the right breast (p=0.1063), but there was a significant reduction for the left breast over the same period of time (p=0.0159 both Fishers Exact test).
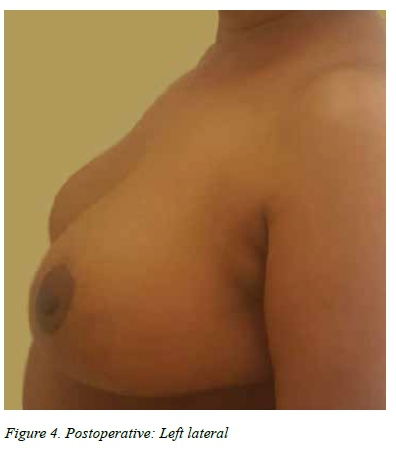
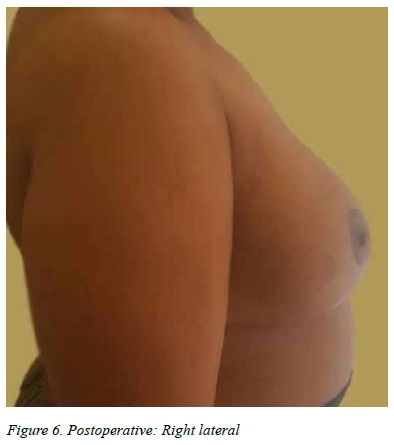
In terms of final outcome of contour and aesthetics, at 1 year, most patients were independently judged* to have a good outcome, 74.2% good projection, 93.5% had good symmetry, 93.5% had good shape and 83.8% of patients were judged to have a good scar formation. The rest of the patients had a fair result for these parameters, while no patients were judged as poor.
Discussion
Our results showed that in 62 macromastia and gigantomastia breasts, with long N-N and large resection weights, the SMP reduction mammoplasty pattern was safely used. A small number of breasts had early superficial necrosis and T-junction breakdown. The symptoms were short lived and resolved with conservative wound management, without need for surgical revision.
In 2007, Davidson et al10 in a cohort of 216 breast reduction patients showed that the SMP with various skin resection patterns, was a safe reliable technique for small and moderate reductions with a broad range of skin patterns, and provided a consistent breast contour, nipple viability and superomedial fullness. The overall complication rate was 18%.
This study's complication rates were comparable, partial superficial nipple necrosis in 11.5%. T-junction breakdown occurred in 24.2% of patients, no nipples were lost. A total of 6.4% (2 patients) had absent sensation at 1 year, 83.8% of patients deemed their sensation to be the same as before surgery. 50% of the patients who had minor T-junction breakdown, and 55% of the patients who had partial NAC necrosis also had a high BMI, > 30. This is in keeping with current literature, which supports the fact that patients with a high BMI are more likely to have delayed wound healing after breast reduction surgery.11
The breasts with the longest N-N = 49.5 and 49 cm each side, did well and showed neither NAC necrosis nor T-junction breakdown. While the patient with the highest resection weight, 2 670 g, showed minor T-junction wound breakdown but no NAC necrosis and sensation was preserved. Landau and Hudson13 reviewed 61 gigantomastia patients who had the SMP reduction pattern. The mean average resection weights were 1379 g, and the mean N-N lengths 35 cm. They showed complication rates of 6.5% and 18% for partial areola necrosis and T-junction breakdown respectively. Our complication rate was higher, 11.5% and 24.2% respectively, but with larger breast resection volumes and longer N-N, i.e. mean breast resection weights of 1 835 g and mean N-N=44.12 cm. When comparing the 2 studies, the breast resection weight was larger by 33% and the N-N longer by 26%, while the complication rate increased by 34% and 76% for T-junction breakdown and NAC necrosis respectively. When compared, they showed that as the breast resection weight and N-N distances increased, the incidence of complication rates increased.
Limitations
A limitation is the relatively small numbers in this study (62 breasts), other study numbers reviewing breast reduction cohorts do so over longer periods and have numbers over 100 breasts. A prospective study needs to look at pre-breastfeeding cohort of macromastia and gigantomastia to study the effect of the SMP pattern on breastfeeding.
BMI maybe a factor to warrant individualised patient weight loss programmes prior to BBR surgery.
Results were favorable at a mean follow up of 1 year, a longer-term follow up would give an interesting indication as to the longevity of breast shape and projection over time. While patients were unanimously satisfied with their new breasts, a standardised patient poll would give a better reflection of the precise impact surgery has on her body and lifestyle.
Conclusion
BBR surgery generally enjoys excellent patient satisfaction levels. Our data on the SMP presents a technique that is safe, efficacious and reproducible for macromastia and gigantomastia breasts, specifically with very long N-N lengths of > 40 cm and resection weights > 1 500 g.
The viability and sensation of NAC are well preserved, while simultaneously producing a good superomedial breast fullness and hence a good shape. There was also preservation of NAC viability and sensation, good breast projection and symmetry.
REFERENCES
1. Agbenorku P. Reduction mammoplasty in a developing country: a guideline for plastic surgeons for patient selection. Aesthetic Plast Surg. 2002;36(1):91-6. No doi or PMID. [ Links ]
2. Blomqvist L, Brandberg Y. Three-year follow-up on clinical symptoms and health-related quality of life after reduction mammaplasty. Plast Reconstr Surg. 2004;114(1):49-54. [http://dx.doi.org/10.1097/01.PRS.0000127794.77267.14] [ Links ]
3. Hernanz F, Santos R. Treatment of symptomatic macromastia in a breast unit. World J Surg Oncol. 2010;8(1):93.[http://dx.doi.org/10.1186/1477-7819-8-93] [ Links ]
4. Iwuagwu OC, Platt AJ, Stanley PW, et al. Does reduction mammaplasty improve lung function test in women with macromastia? Results of a randomized controlled trial. Plast Reconstr Surg. 2006;118:1-6; discussion 7. [http://dx.doi.org/10.1097/01.prs.0000220457.98094.b9] [ Links ]
5. Jones SA, Bain JR. Review of data describing outcomes that are used to access changes in quality of life after reduction mammaplasty. Plast Reconstr Surg. 2001;108(1):62-67. [http://dx.doi.org/10.1097/00006534-200107000-00010] [ Links ]
6. Freire M, Neto MS, Garcia EB, et al. Quality oflife after eduction mammaplasty. Scand J Plast Reconstr Hand Surg. 2004;38:335-339. [http://dx.doi.org/10.1080/02844310410034295] [ Links ]
7. Chadbourne EB, Zhang S, Gordon MJ, et al. Clinical outcomes in reduction mammaplasty: a systematic review and meta-analysis of published studies. Mayo Clin Proc. 2001;76(5):503-510. [http://dx.doi.org/10.4065/76.5.503] [ Links ]
8. Miller BJ, Morris SF, Sigurdson LL, et al. Prospective study of outcomes after reduction mammaplasty. Plast Reconstr Surg. 2005;115:1025-1031. [http://dx.doi.org/10.1097/01.prs.0000154212.10845.54] [ Links ]
9. FR. Nahai Foad Nahai. MOC-PSSM CME: Breast Reduction. Plast Reconstr Surg. 2008;121(1) suppl:1-13. [http://dx.doi.org/10.1097/01.prs0000294705.85848.cf] [ Links ]
10. Davison SP, Mesbahi AN, Ducic I, Sarcia M, Dayan J, Spear SL. The versatility of the superomedial pedicle with various skin reduction patterns. Plast Reconstr Surg. 2007 Nov;120(6):1466-76. [http://dx.doi.org/10.1097/01.sap.0000095656.18023.6b] [ Links ]
11. Platt AJ1, Mohan D, Baguley P. The effect of body mass index and wound irrigation on outcome after bilateral breast reduction. Ann Plast Surg. 2003 Dec;51(6):55 [http://dx.doi.org/10.1097/01.sap.0000095656.18023.6b] [ Links ]
12. Serra MP, Longhi P. Haubeden. The superomedial dermal-glandular pedicle mammoplasty with Wise pattern: an easy technique with a shorten learning curve. Is it the gold standard for severe gigantomastia? Ann Ital Chir. 2010 Sep-Oct;81(5):369-75 [ Links ]
13. Landau AG, Hudson DA. Choosing the superomedial pedicle for reduction mammaplasty in gigantomastia. Plast Reconstr Surg. 2008 Mar;121(3):735-9. [http://dx.doi.org/10.1097/01.prs.0000299297.20908.66] [ Links ]
* By an independent panel: 2 Plastic surgeons, 1 Breast surgeon, 1 Anesthetist.