Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.4 Cape Town Nov. 2016
HEAD AND NECK SURGERY
A fifteen year experience of total thyroidectomy for the management of simple multinodular goitres in a low medium income country
A O AfolabiI, II; O O AyandipoI, II; O O AfuwapeI, II; O A OgundoyinII
IDepartment of Surgery, College of Medicine, University of Ibadan, Ibadan, Nigeria
IIDepartment of Surgery, University College Hospital, Ibadan, Nigeria
ABSTRACT
INTRODUCTION: Total thyroidectomy as a treatment for simple multinodular goitre is not well recognised in most centres in low middle income countries.
METHODS: This paper is a retrospective review of outcomes of total thyroidectomy for simple multinodular goitres in the last fifteen years in a tertiary hospital in Nigeria.
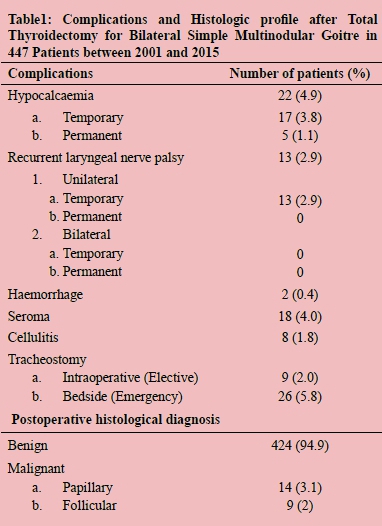
RESULTS: A total of 652 thyroidectomies were done from January 2001 to December 2015. Simple multinodular goitres were indication for a total thyroidectomy in 447 patients (68.6%) with a male to female ratio of 1:6. Postoperative complications were hypocalcaemia in 22 (4.9%), unilateral recurrent laryngeal nerve palsy in 13 (2.8%) and haemorrhage in 2 patients. Others were seroma and cellulitis. Tracheostomy was required in 35 (5.8%) patients but none was permanent.
CONCLUSION: Total thyroidectomy is a relatively safe treatment option for patients who have simple multinodular goitre. It provides a permanent cure with a low postoperative morbidity risk. The burden of replacement l-thyroxine needs to be discussed with the patients.
Introduction
The sequelae of the incomplete surgical management of a bilateral simple multinodular goitre include a risk of recurrence1 which progressively increases as the time elapses from the first operation.2-6 A recent Cochrane review comparing total or near total thyroidectomy versus subtotal thyroidectomy for multinodular nontoxic goitre in adults concluded that goitre recurrence was lower for total thyroidectomy compared to subtotal thyroidectomy.7 The other possible complications include persistence of the initial preoperative symptoms,1 incomplete histological diagnosis and a potential need for a completion-thyroidectomy with its 20-fold increased risk of damage to the parathyroid glands and the Recurrent Laryngeal Nerves (RLN).1
Generally, in low to middle income countries, there is paucity of qualified anaesthetic and surgical personnel, lengthy operative waiting lists, and out-of-pocket health care finance burden. These factors make access to safe surgery difficult. Secondly, an increased risk of complication attributable to a completion thyroidectomy must be weighed against the merits and demerits of partial thyroidectomy or a single definitive treatment paradigm of Total Thyroidectomy (TT).
The rationale for choosing TT with its potential risk is based on the pre- and intraoperative finding of the involvement of both lobes of the thyroid gland in long standing simple multinodular goitre;8 and the assertion that the best way to avoid recurrence is to remove all pathological tissues.9,10 Moreover, the risk of postoperative complications involving the RLN and the parathyroid glands is equivalent for both total thyroidectomy and subtotal thyroidectomy.11,7 Other advantages of a TT include achieving a definitive histology when a possibility of a thyroid malignancy exists and lastly, thyroid hormone replacement therapy with l-thyroxine is easily monitored using a simple blood test.1,12
The balance between an appropriate one-stop surgery with the potential complication and the setting in which a surgical practice is situated must be considered always. There is a paucity of knowledge in the literature on the practice of total thyroidectomy as the treatment of choice for goitre in a low middle income country. We therefore reviewed our experience with total thyroidectomy as the procedure for managing patients who presented with simple multinodular goitre in the University College Hospital, Ibadan, Nigeria.
Methodology
The study was conducted in the Division of Endocrine Surgery, Department of Surgery, University College Hospital, Ibadan. Ethical approval was obtained from the ethical review committee and conduct was in compliance with the guidelines of the Helsinki declaration on biomedical research in human subject. Confidentiality of the identity of the patients and personal health information was maintained. All the cases of simple multinodular goitre subjected to a TT in the 15-year period between January 2001 and December 2015 were enrolled in the study. Data was retrieved from a thyroid surgery data base that was retrospectively generated from patients' case folders, operative theatre details and histopathology reports. Patients with histology proven thyroid carcinoma; primary or secondary hyperthyroidism, retrosternal goitre, recurrent goitre and solitary thyroid nodule who had partial thyroidectomy were excluded. The aim of the exclusion was to have a cohort that had preoperative and intraoperative findings of bilateral simple multinodular goitre (SMG) and consented to a TT only for review. This is because the risk of complication is complete if both lobes along with the important paired organs - parathyroid gland, RLN, and external branch of the Superior Laryngeal Nerve (SLN) - are all subjected to the same extent of dissection. All procedures were performed by consultant endocrine surgeons in a general surgery sub-speciality unit of Endocrine and Hepatobiliary surgery. The data analysed included age, gender, clinical presentation and signs, and thyroid function, surgical approach, and type of procedure undergone, histology and postoperative complications using the SPSS version 17.0. Variables were coded, entered into the computer and data analysed. Descriptive data was summarised using percentages, ratios and proportions for categorical data and means or medians for continuous variables.
Preoperative
All the patients had a clinical examination, thyroid function test, plain radiographs of the neck and thoracic inlet, preoperative serum Ca2+ and PCm assay, an ultrasound guided Fine Needle Aspiration Biopsy (FNAC) along with size, morphology and relationship of the goitre to contiguous structure. Often times a Computerised Tomographic (CT) scan of the neck is not indicated. Laryngoscopy (direct or indirect) is carried out by the otorhinolaryngologic surgeon.
Operative Technique
A collar skin crease incision is deepened; followed by the raising of superior and inferior flaps. The midline is localised for the separation of the strap muscles. The thyroidectomy is accomplished with the techniques of capsular dissection.13,14 This commences at the lateral margin of the lobe all the way to the Berry's ligament which is the immediate superior relation of the RLN running into the larynx at this point. Ligation of the tertiary branches of the inferior thyroid artery that ramify only on the gland ensures preservation of the branches supplying the individual parathyroid gland. The same manoeuvre is carried out on the contralateral side following which the now freely mobile gland is dissected off the trachea. The pyramidal lobe, if present, is dissected to its most superior extent (hyoid bone) to complete the excision of the goitre. A closed vacuum drain is inserted selectively based on the size of the goitre and the extent of the dissection and is removed within 48 to 72 hours.
Our protocol is to identify the RLN only at the area of the Berry's ligament and as many orthotopically placed parathyroid glands as possible, with the immediate mincing and re-implanting of a gland in the ipsilateral sternocleidomastoid muscle, if it is inadvertently de-vascularised or removed. An intraoperative assessment of the trachea for inherent weakness may necessitate continuous postoperative intubation or a tracheostomy, if postoperative intubation exceeds 48-72 hours.
Postoperative Management
Serum calcium and phosphate are assayed at 48 hours post-surgery or, if it is indicated by clinical features, before then. An indirect laryngoscopy is performed if indicated. L thyroxine is commenced on the third day with discharge occurring approximately 96 hours after surgery. However, if serum Ca2+ and PO4 showed hypocalcaemia (< 8.0 mg/dl +/-symptoms and signs), intravenous calcium gluconate and oral calcium lactate is commenced based on the severity, with further Calcium assay ordered as indicated.
Outpatient follow up clinic visits are at two weeks (histology and wound review), six weeks (adequacy of l-thyroxine dose), 12 weeks and 24 weeks to ascertain if the hitherto noted symptoms - hoarseness, hypocalcaemia, voice clarity, voice fatigue etc. - have fully recovered or not. Those requiring a tracheostomy for either tracheomalacia or RLN injury were re-admitted and subsequently de-cannulated by 4th week post-surgery on the otorhinolaryngology surgical service. All the symptoms of hypercalcemia or vocal cord paralysis extending beyond 6 months were classified as permanent while, if it resolved before, was labelled temporary.
Results
Between January 2001 and December 2015 a total of 652 thyroidectomies were done; of these 447 (68.6%) patients had SMG necessitating a TT; Figure 1 shows the number done per year. They consisted of 62 (13.8%) male and 385 (86.2%) females (ratio 1:6.2). The median age was 39 years with a range of (15-74). About two-thirds (222, 62.0%) were referred by the family physician, while 169 (35%) were direct referrals from peripheral hospitals. All patients reside in urban/semi-urban locations as at the time of presentation with 214 (48%) having resided in a rural area during the course of their life. Iodised salt diet history was identified in 318 (71.1%) only. A few patients 8 (1.5%) reported pain as a primary complaint, while 158 (35.3%) complained of voice changes (hoarseness, fatigue, change), swallowing difficulty and painful swallowing of different severity. Cosmesis 264 (59.1%) and others 17 (3.8%) accounted for other presenting complaints.
A total of 52 patients (11.6%) had a family history of goitre. The median duration of the anterior neck swelling was 190 months (range of 1-420 months). Clinical and radiological evidence of trachea deviation / compression was seen in 176 (39%). All patients were euthyroid as at time of presentation; 19 (4.3%) had been placed on some form of thyroid supplementation by the referring physician and 421 (94.2%) patients had normal vocal cord findings with 26 (5.8%) patients having either right or left vocal cord paresis/paralysis at preoperative laryngoscopy.
Using the WHO grading scale14 24 (5.5%), 51 (11.5%), 196 (43.9%) and 176 (39.1%) were Grade 1A, 1B, 2 and 3 respectively. Assisted (fibre optic or bouginage) endotracheal intubation was done in 75 (16.7%). The median specimen weight was 450 g (range 52-1300 g) and 278 (62.2%) had a closed active (vacuum) drain inserted in the thyroid bed. Only 6 (1.3%) patients needed to have a parathyroid gland immediately re-implanted in the body of the ipsilateral sternocleidomastoid muscle following iatrogenic devascularisation or removal. Immediate or delayed endotracheal extubation after surgery was done in 401 (89.7%) and 46 (10.3%) patients respectively. About one in twenty patients (5.8%) had an urgent/ emergency bedside tracheostomy done, while intraoperative tracheostomy was instituted in 9 (2.0%) patients for reasons attributable to size, duration of disease and tracheomalacia. The median duration of hospital stay was 4 days (range of 3-7 days). Postoperative hoarseness was noted in 16 (3.6%) patients, while hypocalcaemia was seen in 22 (6.0%) patients, this resolved in 17 (4.9%) completely within a median duration of 4.4 months (range 1-8months) with permanent hypocalcaemia occurring in 5 patients (1.16%). Seroma was aspirated in 18 (4%) patients and nonsuppurative cellulitis occurred in 8 (1.8%) patients. Reactionary haemorrhage necessitating re-exploration occurred in 2 patients (0.4%). Unilateral RLN (temporary) palsy occurred in 13 (3%) patients with no evidence of permanent paralysis. The RLN palsy however persisted in 6 patients (1.3%) for a median duration of 8 months with a range of 7-9 months. Table 1 highlights the complication and histology profile. We did not have any case of bilateral RLN palsy. Occult malignancy noted included papillary 14 (3.1%) and follicular carcinoma 9 (2%). The median duration of follow up was 18 months (range of 2-48 months). Complete resolution of preoperative symptoms (dysphagia, odynophagia, dysphonia or voice fatigue) was noted in 137 patients (30%) followed up for a minimum duration of 7 months and above (range of 6-48months). Most of the patients 393 (88%) were euthyroid as at the time of last clinical review.
Discussion
The perceived increased risk of postoperative complications and the subsequent need for hormonal replacement initially curtailed the use of TT as one of the operative options in managing benign thyroid disorders. Although its use remains controversial, it is increasingly being used in the management of benign diseases, alike, of the thyroid gland.1,7,11,15 It is however accepted as the standard surgical treatment of thyroid malignancy.11,16,18-20. The knowledge that TT nullifies the risk of recurrence strengthened our resolve that it should be the preferred option in the management of benign thyroid disease with a possibility for recurrence (absence of macroscopically normal tissue) because repeat / completion thyroidectomy procedure for a recurrent goitre has a significantly higher risk than the initial surgery.1,21-24 The caveat however is that the postoperative complication profile must be within acceptable limits. Our 0% permanent RLN and 1.1% permanent hypocalcaemia rates compare favourably with findings from other centres.25-28 We have been able to show that TT can be undertaken with minimal morbidity in patients with benign thyroid condition. The capsular dissection technique, visualisation and preservation of the parathyroid gland and its blood supply along with identification of the RLN at its most vulnerable point29,30 (Ligament of Berry) clearly enhanced our reduced postoperative complication rates. A reactionary haemorrhage rate of 0.4% closely mirrors that of other specialised centre1; we attribute this to the findings that haemostasis is better achieved with a TT,1,30-32 wherein all vessels are ligated as opposed to a sub-total thyroidectomy where residual vascularised thyroid tissue is left behind.21,23 Temporary vocal cord palsy that occurred in 3% of patients is akin to the other published reports.22,33,34 The finding of reduction in voice fatigue along with disappearance of dysphagia, dysphonia and odynophagia postoperatively in our patients supports the assertion that the resolution of preoperative pressure symptoms after a TT is more marked than a sub-total thyroidectomy.34,35
Although the timing of blood sampling (post TT) differs across board, it is agreed that hypocalcaemia is when total serum calcium is < 8 mg/dl.36 A 6% level of transient hypocalcaemia (48 hours postoperatively) is lower than the 19-38% range quoted by a recent review and meta-analysis,36 the varied timing from surgery to calcium assay may explain this wide margin (various authors assay serum calcium between 6 to 72 hours after surgery); however, calcium values generally may be influenced by perioperative factors like postoperative haemodilution, handling of parathyroid gland leading to calcitonin release, urinary calcium excretion facilitated by surgical stress, Vitamin D deficiency and hungry bone syndrome.37,38
Serum Calcium assay is ideal for the low middle income country (LMIC) because it is cheap to run and easy to interpret as opposed to ionised calcium sampling which is dependent on transport, pH, and tourniquet application.38 Of note also is the fact that the timing of calcium estimation impacts on the pick-up rate (diagnosis) of hypocalcaemia, in that the closer the sampling to the time of surgery, the lower the rates of hypocalcaemia will be.38 The consensus presently is to assay for calcium 24 hours after TT,37 with the recommendation that serum parathyroid hormone be obtained in hypercalcaemic patients to serve as a reference value to check parathyroid hormone function recovery during follow-up.38 The concept of protracted hypoparathyroidism introduced by Promberger et al.40 best suits the greater percentage of our patients whose hypocalcaemia all resolved between 4-6 weeks respectively post-surgery. The duration of resolution in this review however extends beyond the postulated two weeks by Promberger et al.; we thus support the call by other authors38,39,41,42 of extending the duration for protracted hypocalcaemia to 6 weeks. Our agreement with the suggestion that parathyroid gland identification has an influence on postoperative hypocalcaemia44 is because our practice is also to visualise the glands in their respective orthotopic location. Risk factors however inherent in our patients as a reason for permanent hypoparathyroidism include heavier thyroid gland specimen45 due to an average gland weight of SD 310+/- 120 g. Most authors agree that auto-transplantation results in higher hypocalcaemia;46-49 we cannot deduce this from our review because the number who had re-implantation was small and none of them manifested hypocalcaemia. Occult malignancy occurred in about 5% of the patients which is akin to reports7,50,51 from centres where TT is also practised; these patients were appropriately referred for thyroid scan thereafter. Long-term euthyroidism is achievable in 90% of cases with l-thyroxine supplementation,1,53 with the fulcrum being the classic negative feedback hormonal mechanism seen in the hypothalamo-pituitary-thyroid axis.
In conclusion, total thyroidectomy is a relatively safe treatment option for patients who have simple multinodular goitre in a low middle income country. It provides a permanent cure with a low postoperative morbidity risk. The burden of replacement /-thyroxine needs to be discussed thoroughly with the patient in comparison with the risk associated with completion-thyroidectomy for incidental carcinoma and a recurrence of the goitre with time. The postoperative morbidity of total thyroidectomy is not higher than that of partial thyroidectomy; patients should therefore not be denied its benefit and should be referred to centres where the expertise is available. The limitation of this study is the retrospective nature of study.
REFERENCES
1. Efremidou EI, Papageorgiou MS, Liratzopoulos N, Manolas K. The efficacy and safety of total thyroidectomy in the management of benign thyroid disease: A review of 932 cases. Canadian Journal of Surgery. 2009;52(1):39-44. [ Links ]
2. Wadström CI, Zedenius J, Guinea A, Reeve T, Delbridge L. Multinodular goitre presenting as a clinical single nodule: how effective is hemithyroidectomy? Aust NZ J Surg. 1999;69(1):34-6. [ Links ]
3. Botelho LS, Rosenthal D, Machado FA, Figueiredo JG. Nontoxic multinodular goiter: evaluation of recurrence rate and function after partial thyroidectomy. Retrospective analysis of 39 cases. Rev Assoc Med Bras. 1992;38(2):85-9. [ Links ]
4. Reeve TS, Delbridge L, Brady P, Crummer P, Smyth C. Secondary thyroidectomy: a twenty-year experience. World J Surg. 1988;12(4):449-452. [ Links ]
5. Jenny H, Block MA, Horn RC, Miller JM. Recurrence following surgery for benign thyroid nodules. Arch Surg. 1966;92(4):525-9. [ Links ]
6. Röjdmark J, Järhult J. High long term recurrence rate after subtotal thyroidectomy for nodular goitre. Eur J Surg. 1995;161(10):725-7. [ Links ]
7. Cirocchi R, Trastulli S, Randolph J, Guarino S, Di Rocco G, Arezzo A, et al. Total or near-total thyroidectomy versus subtotal thyroidectomy for multinodular non-toxic goitre in adults. Cochrane Database of Systematic Reviews, Issue 8, 2015. [ Links ]
8. Friguglietti CU, Lin CS, Kulcsar MA. Total thyroidectomy for benign thyroid disease. The Laryngoscope. 2003;113(10):1820-26. [ Links ]
9. Gemsenjäger E, Heitz PU, Staub JJ, Girard J, Barthe P, Benz UF. Surgical aspects of thyroid autonomy in multinodular goiter. World J Surg. 1983;7(3):363-71. [ Links ]
10. Barbier J, Kraimps JL, Sudre Y, Carretier M, Jardel P. Nodular recurrence after thyroid surgery, excluding cancer. Chirurgie. 1985;111(2):119-23. [ Links ]
11. Gough IR, Wilkinson D. Total thyroidectomy for management of thyroid disease. World J Surg. 2000;24(8):962-5. [ Links ]
12. England MC, Hershman JM. Serum TSH concentration as an aid to monitoring compliance with thyroid hormone therapy in hypothyroidism. AM J Med Sci. 1986; 292(5):264-6 [ Links ]
13. Delbridge L1, Reeve TS, Khadra M, Poole AG. Total thyroidectomy: the technique of capsular dissection. Aust NZ J Surg. 1992;62(2):96-9. [ Links ]
14. Bliss RD, Gauger PG, Delbridge LW. Surgeon's approach to the thyroid gland: surgical anatomy and the importance of technique World J Surg. 2000;24(8):891-7. [ Links ]
15. World Health Organisation, United Nations Children's Fund and International Council for Control of Iodine Deficiency Disorders. Indicators for Assessing Iodine Deficiency Disorders and the Control through Salt Iodization. Geneva: WHO/NUT/94.6,World Health Organisation 1994;1-55. [ Links ]
16. Bron LP, O' Brien CJ. Total thyroidectomy for clinically benign disease of the thyroid gland. Br J Surg. 2004;91:569-74 [ Links ]
17. Phillips AW, Fenwick JD, Mallick UK, Perros P. The impact of clinical guidelines on surgical management in patients with thyroid cancer. Clin Oncol (R Coll Radiol). 2003;15(8):485-9. [ Links ]
18. Beenken S1, Roye D, Weiss H, Sellers M, Urist M, Diethelm A, et al. Extent of surgery for intermediate-risk well-differentiated thyroid cancer. Am J Surg. 2000;179(1):51-6. [ Links ]
19. Kebebew E, Duh QY, Clark ON. Total thyroidectomy or thyroid lobectomy in patients with low-risk differentiated thyroid cancer: Surgical decision analysis of a controversy using a mathematical model. World J Surg. 2000;24:1295-1302. [ Links ]
20. Solomon BL, Wartotsky L, Burman KD. Current trends in the management of well differentiated papillary thyroid carcinoma. J Chin Endocrinol Metab. 1996;81:333-39. [ Links ]
21. Bellantone RI, Lombardi CP, Bossola M, Boscherini M, De Crea C, Alesina P, et al. Total thyroidectomy for management of benign thyroid disease: review of 526 cases. World J Surg. 2002;26(12):1468-71. [ Links ]
22. Liu Q, Djuicin G, Pring RA. Total thyroidectomy for benign thyroid disease. Surgery. 1998;123:2-7. [ Links ]
23. Bearhs OH, Vandertoll DJ. Complications of secondary thyroidectomy. Surg Gynecol Obstet. 1963;117:535-39. [ Links ]
24. Reeve TS, Delbridge L, Brady P. Secondary thyroidectomy: a twenty year experience. World J Surg. 1988;12:449-53. [ Links ]
25. Thompson NW, Narness JK: Complication of total thyroidectomy for carcinoma. Surg Gynecol Obstet. 1970;131:861. [ Links ]
26. Barradough BH, Reeve TS. Post-operative complication of thyroidectomy: A comparison of 2 series at an interval of 10 years. Aust NZ J Surg. 1975;45:4. [ Links ]
27. Clark ON. Total thyroidectomy: The treatment of choice for patients with differentiated thyroid cancer. Ann Surg.1982;196: 361. [ Links ]
28. Jacobs JK, Aland JW, Ballinger JF. Total thyroidectomy: a review of 213 patients. Ann Surg. 1983;197:542. [ Links ]
29. Love JM. Practical anatomical considerations in thyroid tumour surgery. Arch Otolaryngol. 1983;109:568. [ Links ]
30. Thompson NW, Olsen WR, Hoffman GL. The continuing development of the technique of thyroidectomy surgery. Surgery. 1973;73:913. [ Links ]
31. Zambudio AR, Rodriguez J, Riquelme J, et al. Prospective study of post-operative complications after total thyroidectomy for multinodular goitre by surgeons with experience in endocrine surgery. Ann Surg. 2004;240:18-25. [ Links ]
32. Shaha AR, Juffe BM. Practical management of post thyroidectomy hematoma. J Surg Oncol. 1994;57:235-238. [ Links ]
33. Perzik SL. The place of total thyroidectomy in the management of 909 patients with thyroid disease. Am J Surg. 1976;132:480-483. [ Links ]
34. Reeve TS, Delbridge L, Cohen A, Crummer P. Total thyroidectomy. The preferred option for multinodular goiter. Ann Surg. 1987;206(6):782-6. [ Links ]
35. Khadra MI, Delbridge L, Reeve TS, Poole AG, Crummer P. Total thyroidectomy: its role in the management of thyroid disease. Aust NZ J Surg. 1992;62 (2):91-5. [ Links ]
36. Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. 2014;101(4):307-20. [ Links ]
37. Wu J, Harrison B. Hypocalcemia after thyroidectomy: The need for improved definitions. World J End Surg. 2010;2:17-20. [ Links ]
38. Lorente-Poch L, Sancho JJ, Munoz-Nova JL, Sanchez- Velazquez P, Sitges-Serra A. Defining the syndromes of parathyroid failure after total thyroidectomy. Gland Surg. 2015;4(1):82-90. [ Links ]
39. Sitges-Serra A, Ruiz S, Girvent M, Manjón H, Duenas JP, Sancho JJ. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg. 2010;97:1687 1695. [ Links ]
40. Promberger R, Ott J, Kober F, Mikola B, Karik M, Freissmuth M, et al. Intra and post- operative parathyroid hormone kinetics do not advocate for auto-transplantation of discoloured parathyroid during thyroidectomy. Thyroid. 2010;20:1371-75. [ Links ]
41. Hallgrimsson P, Nordenström E, Almquist M, Bergenfelz AO. Risk factors for medically treated hypocalcemia after surgery for grave's disease: a Swedish multicentre study of 1157 patients. World J Surg. 2012;36:1933-42. [ Links ]
42. Bergenfelz A, Jansson S, Kristoffersson A, Mártensson H, Reihnér E, Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicentre audit comprising 3660 patients. Langenbeck's Arch Surg. 2008;393:667-73. [ Links ]
43. Vanderlei FA, Vieira JG, Hojaij FC, Cervantes O, Kunii IS, Ohe MN, et al. Parathyroid hormone: an early redictor of symptomatic hypocalcemia after thyroidectomy. Arg Bras Endocrinol Metabol. 2012,56:168-72. [ Links ]
44. Sheahan P, Mehanna R, Basheeth N, Murphy MS. Is systematic identification of all four parathyroid glands necessary during total thyroidectomy? A prospective study. Laryngoscope. 2013;123:2324-28. [ Links ]
45. Thomusch O, Machens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, et al. Multivariate analysis of risk factors for postoperative complications in benign goitre surgery: prospective multicentre study in Germany. World J Surg. November 2000.1335-41. [ Links ]
46. Gourgiotis S, Moustafellos P, Dimopoulos N, Papaxoinis G, Baratsis S, Hadjiyannakis E. Inadvertent parathyroidectomy during thyroid surgery: The incidence of a complication of thyroidectomy. Langenbeck's Arch Surg. 2006;391:557-60. [ Links ]
47. Ondik MP, McGinn J, Ruggiero F, Goldenberg D, Unintentional parathyroidectomy and hypothyroidism in secondary central component surgery for thyroid cancer. Head and Neck. 2010;32:462-66. [ Links ]
48. Sakorafas GH, Stafyla V, Bramis C, Kotsifopoulos N, Kolettis T, Kassaras G. Incidental parathyroidectomy during thyroid surgery: an underappreciated complication of thyroidectomy. World J Surg. 2005;29:1539-43. [ Links ]
49. Lo CY, Tam SC. Parathyroid autotransplantation during thyroidectomy: documentation of graft function. Arch Surg. 2001;136:1381-85. [ Links ]
50. Tezelman S, Borukui, Senyurek G, Tunca F, Terzioghi T. The change in surgical practise from subtotal and near total thyroidectomy in the treatment of patients with benign multinodular goitre. World J Surg. 2009;33:410-415. [ Links ]
51. Ozbas S, Kasbak S, Aydingtag S. Comparison of the complication of subtotal, near total and total thyroidectomy in the management of multinodular goitre. Endocrine Journal. 2005;52:199-205. [ Links ]
52. Sanjeera K, Chandra B, Balakrishna MA, et al. Clinico-epidemiological study and treatment outcome of ultinodular goitre at a tertiary hospital. Journal of Clinical and Diagnostic Research. 2005. [ Links ]
53. Moussa AQ, Seydon T, Ibrahim S, Kadiaton S, et al. Total thyroidectomy in multinodular goiter. An African Experience. Surgical Science. 2015;6:527-31. [ Links ]
 Correspondence:
Correspondence:
O O Ayandipo
yokebukola@yahoo.com














