Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.4 Cape Town nov. 2016
NEUROSURGERY
Acute extradural haematomas in children: A 12-year experience from a single neurosurgery unit
B EnickerI; H LouwI; T MadibaII
IDepartment of Neurosurgery Inkosi Albert Luthuli Central Hospital, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
IIGeneral Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
ABSTRACT
BACKGROUND: Acute extradural haematomas (AEDHs) occur infrequently in children. This study was undertaken to review our experience with management and outcomes of this condition in children treated in the Neurosurgery Unit at Inkosi Albert Luthuli Central Hospital.
METHODS: A retrospective review of medical records of all children (age less than or equal to (<) 12 years) with a diagnosis of AEDH admitted from January 2003 to December 2014 was performed. Records were analyzed for demographics, mechanisms of injury, clinical presentation, neuroradiology findings, management and outcomes at discharge.
RESULTS: A total of 150 children with AEDHs were admitted during this period. The mean age was 6.6 ± 3.8 years with a peak incidence in the 7-9 year age group. There were 84 (56%) males, (M: F= 1.3:1). Sixty AEDHs resulted from road traffic crashes (40%). On admission 104 (69.3%) children were Glasgow coma scale (GCS) 13-15, 26 (17.3%) GCS 9-12 and 20 (13.4%) GCS 3-8. Haemoglobin was less than (<) 8 g/dl in 56% of infants (p < 0.001). Skull fractures were identified in 78% of cases. Surgical management was undertaken in 83% of children and the mean hospital stay was 6.9 ± 6.1 days. Four children (2.7%) died during in-hospital stay period. One hundred and forty one (94%) children had a favourable Glasgow outcome scale (GOS) at discharge.
CONCLUSION: AEDHs in children carry a good prognosis, but can be potentially fatal. A vigilant approach is required when assessing these children, as early diagnosis and treatment yields gratifying results.
Keywords: Acute extradural haematoma, children, craniotomy
Introduction
Traumatic brain injury (TBI) is a major public health problem in South Africa (SA).1
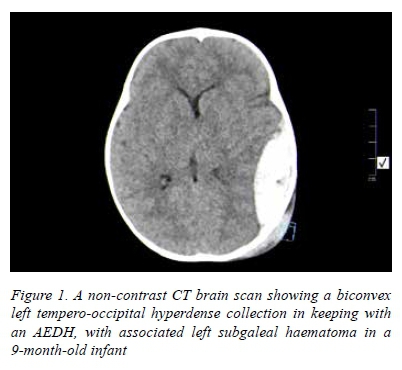
It is one of the leading contributors to morbidity and mortality of children both locally and internationally.2,3,4 Reports suggest that children less than (<) 4 years of age are the most vulnerable to sustain TBI and in almost all instances these injuries are preventable.4 An acute extradural haematoma (AEDH) is defined as accumulation of blood between the inner table of the skull, including its periosteal layer and the dura mater (Figure 1).5 AEDHs occur relatively infrequently in children, but when they do occur, they present as an emergency and can have devastating consequences when not treated timeously. The Province of KwaZulu-Natal (KZN), which has an area of 94,361 km2 and an estimated population 10.69 million, has only one Neurosurgery Unit (NU), which is located at Inkosi Albert Luthuli Central Hospital (IALCH) and provides the only public sector paediatric neurosurgery service in this Province.6 We undertook this retrospective study to evaluate our experience with AEDHs in children in this single unit with respect to their clinical presentation, management and outcomes over a 12-year period.
Materials and methods
This was a retrospective review of medical records of all children (age less than or equal to (<) 12 years) with a diagnosis of traumatic AEDH admitted to the NU at IALCH from January 2003 to December 2014. The records were reviewed for demographics, mechanism of injury, clinical presentation, Glasgow coma scale (GCS), pupillary reactivity, haemoglobin (Hb) on admission, computerized tomography (CT) scan findings, associated intracranial haematomas, extracranial injuries, management and outcomes at discharge using the Glasgow outcome scale (GOS). The GOS was categorized as favourable (GOS 4-5) and unfavourable (GOS 1-3).7
The inclusion criterion used was the diagnosis of only post-traumatic AEDHs. Children older than 12 years of age were excluded from the study. A CT brain scan was utilized to make the diagnosis of an AEDH and was performed either at the referring hospital or at IALCH when facilities were not available at the base hospital. Indications for surgery and conservative management used in our unit were based on the surgical management of TBI guidelines.8 Surgical management consisted of a craniotomy or craniectomy performed under general anesthesia. Postoperatively, children were managed either in the intensive care unit (ICU), when neurocritical treatment was indicated as per Brain Trauma Foundation guidelines9,10 or in the paediatric high care ward. Children who were managed conservatively were admitted into the latter ward where strict neuro-observations were performed. We undertake a measured approach when performing follow-up CT brain scans in those children managed conservatively and each case is individualised based on the clinical condition of the child, as exposure to repeated radiation in young children is of concern in our unit.11 The study was granted ethical approval by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (Ref BE 449/14).
Statistical analysis
Descriptive statistics such as frequencies, proportions, mean, standard deviations and percentages were used to summarise the data. Fisher's exact test was used for categorical data when indicated. A p < 0.05 was considered statistically significant.
Results
The NU at IALCH admitted a total of 1805 cases of traumatic AEDHs from January 2003 to December 2014, and 150 (8%) of these were diagnosed in children. The annual admission rate is shown in Figure 2. The mean age was 6.6 ± 3.8 years (range 1 month to 12 years). The peak incidence was in the 7 to 9-year age group (Figure 3). There were 84 (56%) boys, giving a male to female ratio of 1.3:1.


The mechanisms of injury are shown in Table 1. Headaches (46; 31%) were the most common clinical presentation followed by vomiting (38; 25%), seizures (25; 17%) and irritability (17; 11%). The median GCS on admission was 15 (range 3-15). The GCS was 13-15 in 104 (69.3%) children, 9-12 in 26 (17.3%) and 3-8 in 20 (13.4%). Clinical examination revealed subgaleal haematomas (77; 51%), hemiparesis (21; 14%) and dilated non-reactive pupils (14; 9%). There was unilateral pupillary dilatation in 12 children and it was bilateral in two.
The mean Hb on admission was 10.5 ± 2.3 g/dl (range 3.115.8 g/dl). One hundred and thirteen (75%) children presented with Hb greater than or equal to (>) 10 g/dl, 19 (13%) with Hb of 8-9.9 g/dl and 18 (12%) with Hb < 8 g/dl on admission. Of the children with Hb < 8 g/dl, 10 (56%) were < 1 year of age and 8 (44%) were > lyear of age (p < 0.001). All 10 infants had associated subgaleal haematomas. Twenty-nine (19%) children required blood transfusion during the admission period.
Thirteen (9%) children presented with associated extracranial injuries mainly orthopaedic injuries (11), including fractures of the tibia (5), femur (2), humerus (2) and clavicle (2). The other two children suffered from rib fractures with underlying pneumothorax and lung contusion respectively. The CT brain scan findings are shown in Table 2. Surgical management in 125 children (83%) involved craniotomy (105) and craniectomy (20), while the other 25 children were managed conservatively. The mean duration of the surgical procedure was 2 ± 0.7 hours (45 minutes to 5.3 hours). Intraoperatively, an active bleeding source was identified in 68 (54%) children, which was venous in 55 (81%) and arterial (middle meningeal artery) in 13 (19%). The venous sources of bleeding were: (i) fracture site (28), (ii) dura (18) and (iii) superficial venous sinuses (9).
Thirty-four (21%) children were admitted into the ICU for both ventilation and intracranial pressure (ICP) monitoring (23) and for ventilation and resuscitation only, without ICP monitoring (11). The mean ICU stay was 4.5 ± 3.6 days (range 1-18 days). Three (2.4%) children had re-accumulation of the AEDH during the immediate postoperative period and were taken back to theatre for re-evacuation, whilst one child developed post-traumatic hydrocephalus which required ventriculoperitoneal shunting. The mean hospital length of stay was 6.9 ± 6.1 days (range 1-36 days). Ten (6.7%) children were referred to child protection services for investigation of the circumstances of their injuries and assessment of the home environment. The GOS was favourable in 141 (94%) children and unfavourable in 9 (6%). Four (2.7%) children died as a consequence of their injuries and their profiles are shown in Table 3. None of the children who died had been managed conservatively. Of the 146 children alive at discharge only 44 (30%) were followed-up with a mean follow-up period of 2.4 ± 1.9 months (range 1-9 months). All had a favourable GOS of 5 at follow-up.
Discussion
Our study shows that AEDHs occur less frequently in children when compared to adults in our environment. The reason is that the dura mater is more tightly adherent to the inner table of the skull in children, limiting the potential space for accumulation of haematomas.12 Our results show AEDHs are even less common in infants making up 12% of children affected in our study.
In a local study by Okyere-Dede et al., only 1% of 78 children with intracranial haematomas admitted in a General Pediatric Surgical Unit had AEDHs and these were referred for neurosurgical intervention.13 The main mechanism of injury resulting in AEDHs in this series was road traffic crashes (RTCs). Interestingly, previous reports of the SA experience by Pillay et al. 20 years ago, showed a preponderance of falls over RTCs.14 The higher prevalence of RTCs in our study can be explained by an increase in the number of cars in the streets of SA over the last two decades, a testament to rapid urbanization. This also highlights the contribution of RTCs to mortality in SA, with reports putting the annual mortality rate of children involved in RTCs at 3.89 per 100 000.15,16 The World Health Organization (WHO) identified falls as one of the leading causes of death in children especially those under the age of 6 years.17 Infants and toddlers tend to fall from beds, or are accidentally dropped by preoccupied caregivers. As children grow up and become more adventurous, they tend to fall from trees and buildings. Assaults by peers or child abuse cases are worrying phenomena, and require investigation by the child protection services after stabilization of the life threatening injuries, in order to limit violence against children. The clinical presentation of children with AEDHs is variable and can be non-specific, ranging from asymptomatic to mildly symptomatic (with headaches, nausea, irritability and vomiting) to altered level of consciousness, thus emergency physicians should be on high alert when assessing children with TBI. The majority of children in our unit presented with a good GCS, as young children tolerate an increase in ICP better than adults since the source of bleeding is mainly venous, causing gradual haematoma expansion in contrast to rapid arterial haematoma expansion commonly experienced in adults.18 Young children also have open fontanelle and large extra-cerebral spaces, which aid to accommodate raised ICP.18 Subgaleal haematomas were present in 51% of children in this series and they are of particular significance in infants as accumulation of blood in the subgaleal space can result in hypovolaemia and anaemia, because of an infant's small total blood volume.19 However, when a child presents in hypovolaemic shock with anaemia following TBI, other sources of blood loss such as abdominal organ injuries or long bone fractures should be excluded and it is imperative that blood products should be available on standby when young children, in particular infants, are taken to theatre for evacuation of AEDHs. In our study, we identified skull fractures in 78% of children, which is a significant finding as the skull in children has abundant diploic veins making these the main source of bleeding.18
The majority of AEDHs are managed surgically, with craniotomy being performed more frequently than craniectomy.20 Vigilant postoperative observations are essential as there is always a risk of re-accumulation of the haematoma in the immediate postoperative period as was the case in 2.4% of children in our series. However, these were detected timeously and addressed appropriately with no associated morbidity and mortality. Successful conservative management has been reported by other authors and was not associated with morbidity and mortality in our series.21
The mortality rate in our study was 2.7% which falls within the reported rate of 0-12%.5,8,12,20,21 The variation in mortality rate is secondary to unique regional referral patterns, ease of access to CT scans, pre-hospital management, time to surgery and postoperative care across different NUs. Admission GCS of < 8, bilaterally dilated non-reactive pupils, sustained hypoxia (PaO2 < 60 mmHg or oxygen saturation < 90%) and hypotension (systolic blood pressure below the 5th percentile for age) are amongst the predictors of a poor outcome;8,10 and these contributed to mortality in our study. The injured brain in children is vulnerable to hypotension due to loss of autoregulation resulting in decreased cerebral perfusion, the end result being irreversible cellular damage.22 These can be prevented or have their effect ameliorated by applying Advanced Trauma Life Support (ATLS®) principles at initial assessment with emphasis on airway control with intubation when indicated, ensuring adequate ventilation, maintaining appropriate haemodynamic status and cerebral perfusion pressure followed by prompt evacuation of the AEDH.
This study does have some limitations. The retrospective nature of the study makes it inherently vulnerable to bias. The results are from a single NU and focused on children treated in the public health sector in KZN and excluded children treated in private hospitals and those not accepted for treatment at IALCH. Trauma is not routinely followed-up in our unit, making it difficult to assess long-term functional status.
Conclusions
Children account for 8% of patients with AEDH in the NU in KZN. These lesions carry a good prognosis, but can potentially be fatal. It is incumbent on the emergency physicians to be vigilant when assessing children with TBI, as symptoms of AEDHs can often be non-specific especially in infants and toddlers. Treatment yields gratifying results when diagnosed and treated in a timely fashion. The injury mechanisms in our setting are preventable and we recommend that government departments, i.e. health, transport and child protection services, work together with communities in crafting and implementing strategies to firstly prevent these injuries and lastly to improve outcomes.
Conflict of interest
The authors do not have a conflict of interest with regards to the preparation and writing of this manuscript.
REFERENCES
1. Zulu BMW, Mulaudzi TV, Madiba TE, Muckart DJJ. Outcome of head injuries in general surgical units with an off-site neurosurgical service. Injury. 2007;38(5): 576-583. [http://dx.doi:10.1016/j.injury.2007.01.002] [ Links ]
2. Schrieff LE, Thomas KGF, Dollman AK, Rohlwink UK, Figaji AA. Demographic profile of severe traumatic brain injury admissions to Red Cross War Memorial Children's Hospital, 2006 - 2011. S Afr Med J. 2013;103(9): 616-620. [http://dx.doi:10.7196/SAMJ.7137] [ Links ]
3. Semple PL, Bass DH, Peter JC. Severe head injury in children - preventable but forgotten epidemic. S Afr Med J. 1998;88(4):440-444. [ Links ]
4. Parslow RC, Morris KP, Tasker RC, Forsyth RJ, Hawley CA. Epidemiology of traumatic brain injury in children receiving intensive care in the UK. Arch Dis Child. 2005;90:1182-1187. [http://dx.doi:10.1136/adc.2005.072405] [ Links ]
5. Duthie G, Reaper J, Tyagi A, Grimmins D, Chumas P. Extradural haematomas in children: A 10-year review. Br. J Neurosurg. 2009;23(6):596-600. [http://dx.doi:10.3109/02688690902978157] [ Links ]
6. Mid-year population estimates 2014. Statistical release P0302/Statistics South Africa, Pretoria, 2014. Available at: http://beta2.statssa.gov.za (Accessed 20 March 2015). [ Links ]
7. Jennet B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;27(7905):370-378. [ Links ]
8. Bullock MR, Chesnut R, Ghajar J, et al. Surgical management of acute extradural hematomas. Neurosurgery. 2006;58(Suppl 2):S7-S15. [http://dx.doi:10.1227/01.neu.0000210363.91172.a8] [ Links ]
9. Brain Trauma Foundation: Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24(Suppl 1):S1-S106. [http://dx.doi:10.1089/neu.2007.9998] [ Links ]
10. Adelson PD, Bratton SL, Carney NA, et al. Guidelines for the management of severe traumatic brain injury in infants, children and adolescents. Pediatr Crit Care Med. 2003;4(Suppl 3):S1-S491. [http://dx.doi:10.1097/01.ccm.0000067635.95882.24] [ Links ]
11. Sikwila CT, Amod K, Cupido BD, Sabri A. Multi-detector computed tomography radiation doses in the follow-up of paediatric neurosurgery patients in KwaZulu-Natal: a dosimetric audit. S Afr J Rad. 2014;18(1):1-4. [http://dx.doi:org/10.4102/sajr.v18i1.588] [ Links ]
12. Rocchi G, Caroli E, Raco A, Salvati M, Delfini R. Traumatic epidural hematoma in children. J Child Neurol. 2005;20(7):569-571. [http://dx.doi:10.1177/08830738050200070501] [ Links ]
13. Okyere-Dede EK, Nkalakata MC, Nkomo T, Hadley GP, Madiba TE. Paediatric head injuries in the KwaZulu-Natal Province of South Africa: a developing country perspective. Trop Doct. 2013;43:1-4. [http://dx.doi:10.1177/0049475513480490] [ Links ]
14. Pillay R, Peter JC. Acute extradural haematomas in children. S Afr Med J. 1995 85(7):672-674. [ Links ]
15. Road traffic accident deaths in South Africa, 2001-2006: Evidence from death notification. Available from: http://www.statssa.gov.za/publications/report-03-09-07/report-03-09-07. (Accessed 28 February 2015). [ Links ]
16. Howlett JB, Aldous C, Clarke DL. Injuries sustained by passengers travelling in the cargo area of light delivery vehicles. S Afr J Surg. 2014;52(2):49-52. [http://dx.doi:10.7196/sajs.1963] [ Links ]
17. Peden M, Oyegbite K, Ozanne-Smith J, et al. World report on child injury prevention. Available from: http://www.whqlibdoc.who.int/publications/2008/9789241563574_eng. (Accessed 29 March 2015). [ Links ]
18. Jamjoom A, Cummins B, Jamjoom ZA: Clinical characteristics of traumatic extradural haematoma: A comparison between children and adults. Neurosurg Rev. 1994;17(4):277-281. [ Links ]
19. Ciurea AV, Kapsalaki EZ, Coman TC, et al. Supratentorial epidural hematoma of traumatic etiology in infants. Childs Nerv Syst. 2007;23(3):335-341. [http://dx.doi:10.1007/s00381-006-0230-4] [ Links ]
20. Chowdhury SM, Raihan MZ, Chowdhury FH, Ashadullah ATM, Sarkar MH, Hossain SS. Surgical management of traumatic extradural haematoma: Experiences with 610 patients and prospective analysis. 2008;5(2):75-79. [http://dx.doi:10.1016/s0973-0508(08)80004-4] [ Links ]
21. Balmer B, Boltshauser E, Altermatt S, Gobet R. Conservative management of significant epidural haematomas in children. Childs Nerv Syst. 2006;22(4):363-367. [http://dx.doi:10.1007/s00381-005-1254-x] [ Links ]
22. Figaji AA, Fieggen AG, Argent AC, Le Roux PD, Peter JC. Does adherence to treatment targets in children with severe traumatic brain injury avoid brain hypoxia? A brain tissue oxygenation study. Neurosurgery. 2008;63(1):83-92. [http://dx.doi:10.1227/01.neu.0000313113.43447.0c] [ Links ]
 Correspondence:
Correspondence:
Basil Enicker
basilenicker@yahoo.com














