Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.4 Cape Town nov. 2016
TRAUMA
Computerised Tomographic Angiography (CTA) in extremity trauma - A level one hospital experience
P JordaanI; S RocheII; S MaqungoII
IRegistrar, Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
IIConsultant Orthopaedic Surgeon, Groote Schuur Hospital
ABSTRACT
INTRODUCTION: The aim of this study was to audit the use of Computerised Tomographic Angiography (CTA) in assessing extremity vascular injuries at our institution and to compare it to international standards.
The primary aim was to assess the number of CTAs performed and the indications for doing them. The secondary aim was to look at CTA results and clinical findings and to correlate the two.
METHODS: This is a retrospective review of all patients aged 13 years and older who had CTA performed for suspected extremity vascular injuries due to blunt trauma or gunshot injuries, who presented from January 2012 to December 2012.
RESULTS: Two hundred and eighty five (285) CTAs were performed in 2012 and 137 met our inclusion criteria. Eleven cases were excluded due to insufficient data, leaving a total of 126 cases suitable for analysis. Eighty three patients (66%) had a normal CTA. The indications for CTA were as follows: decreased pulse in 46 patients (42%), absent pulse in 19 patients (17%), presumed knee dislocation in 18 patients (16%), injuries in the proximity of large vessels in 12 patients (11%), haematoma in 8 patients (7%), bleeding in 5 patients (4%) and an abnormal Doppler in 2 patients (2%). When comparing pulse examination to CTA results, the clinical assessment of pulses had a sensitivity of 74.4%, specificity of 53.7%, positive predictive value (PPV) of 45.7% and a negative predictive value (NPV) of 80%.
CONCLUSION: Incorrect indications are being used when ordering a CTA in extremity vascular trauma. Clinical examination is suboptimal and not a reliable indicator of vascular injury in our setting, leading to a lower threshold for ordering a CTA.
Key words: Computerised Tomographic Angiography, extremity vascular trauma
Introduction
In the last two decades, Computerised Tomographic Angiography (CTA) has replaced formal Digital Subtraction Angiography as the gold standard in evaluating vascular trauma. 1,2,3,4 Correct diagnosis of vascular injuries is of great importance as isolated vascular injuries of the lower extremity have a mortality rate of 2.8% and an amputation rate of 6.5%.5 Most of our knowledge of vascular injuries has been gained from wars and conflicts.6,7 This has seen an improvement in amputation rate from 49% in World War II to 13% in the Vietnam conflict, mostly due to early evacuation and treatment of patients,7 stressing the importance of early surgical management of these injuries. The incidence of vascular injuries in long bone fractures is less than 1%. In certain high risk injuries, like knee dislocations, this increases to 16%.8
Physical examination remains the most important tool in the evaluation of the injured extremity and many authors have observed that injuries not found with initial and serial clinical examinations pose no long-term adverse risk to these patients.4,9 Clinical features of vascular injuries can be divided into 'hard' signs and 'soft' signs.8,10 (Table 1)
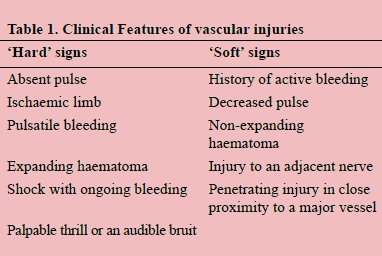
In the presence of 'hard' signs a patient should be taken to theatre for an emergency exploration. A patient who presents with 'soft' signs should undergo further imaging.8,9,11
The use of the Ankle-Brachial Index (ABI) and Arterial Pressure Index (API) has been shown to be reliable in excluding vascular injuries in both blunt and penetrating trauma.9,12,13
Patients with a normal examination should be observed or have an API performed and where the API is less than 0.9 a CTA should be performed.9
A delay of more than 8 hours increases the amputation rate to 86%, which means delaying surgery to perform unnecessary investigations could worsen the outcome.8
The aim of this study was to audit the use of CT Angiography in assessing extremity vascular injuries at our institution and to compare it to international standards.
Method
This is a retrospective review of all patients aged 13 years and older who had CTA performed for suspected extremity vascular injuries due to blunt trauma or gunshot injuries, who presented from January 2012 to December 2012 to our level one (Tertiary) trauma centre. All patients were primarily assessed and managed by the trauma team, including the trauma surgeons, before being referred to orthopaedic surgery for the management of their orthopaedic injuries. Patients younger than 13 years and patients who sustained stab wounds were excluded. Data obtained included patient demographics, mechanism of injury, associated injuries, pulse and neurological assessment, capillary refill time and temperature of the affected limb, result of Doppler examination, indication for CTA, CTA result and whether any further intervention was performed. The primary aim was to assess the number of CTAs performed and the indications for doing them. The secondary aim was to look at CTA results and clinical findings and to correlate the two.
This study was approved by our Department of Surgery Research Committee and Ethics Committee.
Results
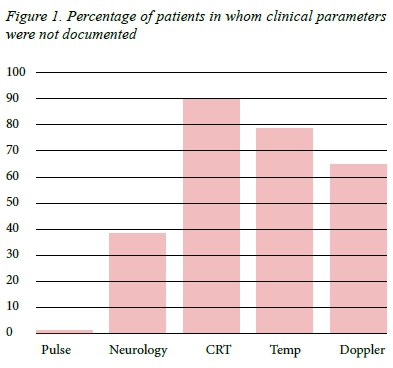
Two hundred and eighty five (285) CTAs were performed in 2012 and 137 met our inclusion criteria. Eleven cases were excluded due to insufficient data, leaving a total of 126 cases suitable for analysis (Figure 1). One hundred and five (83%) were male and 21 (17%) female. The average age was 30 years (range 14-86 years). Mechanism of injury was as follows: gunshots in 63 patients (50%), motor vehicle collisions in 21 patients (17%), pedestrian-vehicle collisions in 20 patients (16%), falls in 8 patients, sports injuries in 5 patients and blunt assaults in 3 patients. In a number of patients the following clinical parameters were not documented: pulse examination (1 patient), neurological function (49 patients), capillary refill time (113 patients), temperature of affected limb (99 patients) and Doppler examination (82 patients) (Figure 2). No ABI/APIs were performed. The indications for CTA were as follows: decreased pulse in 46 patients (42%), absent pulse in 19 patients (17%), presumed knee dislocation in 18 patients (16%), injuries in the proximity of large vessels in 12 patients (11%), haematoma in 8 patients (7%), bleeding in 5 patients (4%) and an abnormal Doppler in 2 patients (2%).
Ninety five patients (75%) had associated orthopaedic injuries: 77 fractures, 15 knee dislocations/multi-ligamentous knee injuries and 3 patella dislocations.
Two patients (1.6%) had amputations. The first one was involved in a pedestrian-vehicle collision and sustained bilateral open tibia fractures with an absent pulse on the one side and an abnormal CTA on the other. The surgeons performed an 'on-table angiogram' and arterial repair, but the patient later required a below-knee amputation. The second patient sustained a gunshot wound to the distal thigh with a distal femur fracture and a pulseless, cold foot with altered sensation (ischaemic limb). CTA showed a complete superficial femoral artery cut off and the patient had a failed arterial bypass with eventual above-knee amputation.
Results of pulse examination
Of the 55 patients who had a normal pulse, 12 had an abnormal CTA and 6 of these patients had further intervention. (Table 2) Of the patients with a normal pulse, 31 had normal neurological function documented. In this group, there were 7 abnormal CTAs, of which 4 had further intervention. In one of these cases a vascular injury was noted with further investigation, which was a profunda femoral artery injury mentioned earlier, which had proximity to an artery as indication for the CTA. (Table 3) Of the 70 patients with an abnormal pulse, 32 (46%) had an abnormal CTA and 38 (54%) had a normal CTA. Of these patients 19 had further surgical intervention.
One patient had no pulse status documented. The CTA was performed due to active bleeding and showed a possible arteriovenous fistula, but the formal angiogram was normal.
When comparing pulse examination to CTA results, the clinical assessment of pulses had a sensitivity of 74.4%, specificity of 53.7%, positive predictive value (PPV) of 45.7% and a negative predictive value (NPV) of 80%.
CTA results
Eighty three patients (66%) had a normal CTA, of which 2 patients had further intervention: the first one had an absent pulse and was taken to theatre where a bleeding vein was tied off and the second patient had a decreased pulse and a fasciotomy was performed to release a tight compartment.
Forty three patients (34%) had a CTA which showed a vascular injury, of which 24 had further intervention. Eighteen of these cases had vascular pathology at further exploration. Six of these had normal vascular anatomy at time of exploration or formal angiography and one of them proceeded to a fasciotomy for a compartment syndrome.
Results as per indication
In only 110 patients a request for the CTA could be located or an indication was noted.
Absent pulse (Hard sign)
Of the 19 patients (17%) with absent pulses, 16 had abnormal CTA results and 11 of these patients (57.8%) required further intervention. Clinical documentation of neurological deficits was poor, but 4 patients in this group had neurological deficits and all of them required intervention. Only one patient had good documentation of clinical signs suggesting an ischaemic limb. This patient had a failed bypass ending in an above-knee amputation.
Decreased pulse (Soft sign)
Forty six patients (42%) had a decreased pulse as an indication for their CTA, of which 10 had a CTA showing vascular injury. Only 3 of these patients had further surgical intervention.
Mechanism of injury (Soft sign?)
Eighteen patients (16%) had a CTA performed for a presumed knee dislocation. Further imaging showed 3 of these patients to have patella dislocations. Three patients had an abnormal CTA: an intimal injury and external compression of the anterior tibial artery, both receiving no further intervention and one patient with a popliteal artery occlusion requiring a bypass. This last patient had a decreased pulse on clinical examination.
Proximity to a major artery (Soft Sign) All of the 12 patients (11%) in this group had normal pulses on examination. Three patients had an abnormal CTA and one of these patients required further intervention. This patient had a completely normal vascular and neurological assessment and required a stent for a profunda femoral artery injury.
Haematoma (Hard/Soft Sign)
This group includes patients who had a CTA performed for a haematoma or swelling. In none of the cases did the requesting doctor differentiate between an expanding or non-expanding haematoma making it impossible to determine whether it was a hard or soft sign. This group had a total of 8 patients (7%) with 3 abnormal CTAs of which one patient was too unwell for theatre. One had a negative exploration and the other had a normal 'on-table angiogram', but required fasciotomies for a compartment syndrome.
Bleeding (Hard/Soft Sign)
Depending on the history of bleeding this can be interpreted as a hard or a soft sign, but this differentiation was not made on the request forms. This group included 5 patients (5%) and all had an abnormal CTA of which one showed venous bleeding and had no further surgical intervention. The other 4 all had further intervention: exploration and anterior tibial artery ligation, a normal 'on-table angiogram', a normal Digital Subtraction Angiogram and a pseudo aneurysm managed with coiling.
Abnormal Doppler
An abnormal Doppler examination was noted to be the indication for CTA in 2 patients (2%). This is not a hard or soft sign. One patient had a normal CTA and one had an abnormal CTA, a posterior tibial artery filling defect requiring no further intervention.
Discussion
The most striking observation is the poor documentation of clinical parameters, which makes interpretation of results very difficult. The indication for CTA was not clearly documented for all patients, which explains the discrepancy in numbers. Furthermore, the indication for CTA and the pulse examination are different in certain cases; for example, a patient with a decreased pulse had mechanism of injury as indication and therefore the results are presented separately as per indication and pulse examination.
CTA has become the primary investigation for vascular trauma,6 but opinions regarding the threshold for using CTA are very different. Many authors state that clinical examination should be the primary tool in assessment of possible vascular injuries and advocate against the routine use of CTA.4,11,12,13,14,15,16 Patterson et al 15 concluded that arteriography only delays the time to definitive repair and commented that: "It is important to not underestimate the value of a warm hand on a cold foot." Mills et al reviewed the use of the ABI in knee dislocations and using 0.9 as a cut off had a specificity, sensitivity, NPV and PPV of 100%. They argued that arteriography just delays repair of vascular injuries.12 Lynch and Johansen published a series of cases comparing the API to arteriography and concluded that screening arteriography is rarely positive and that often clinically irrelevant lesions are discovered. They showed that the API may be just as reliable as arteriography.13 The argument that arteriography may be useful to locate the level is valid only in cases of multiple injuries to the same limb, because with knee dislocations the injury is between the adductor canal and the soleus arch14 and in single penetrating injuries the vascular injury will be in the area of the penetrating injury. Injuries distal to the trifurcation often do not need any further intervention and the confirmation of these injuries rarely contributes to further management.
Other authors recommend the liberal use of arteriography. Nitecki et al advise liberal use of CTA, but this was in a combat setting.17 According to Barnes et al, pulse examination is not reliable and recommends liberal use of arteriography, specifically in knee dislocations.18
Out of a total number of our 126 patients, 34% had an abnormal CTA and 19% required further intervention. Defining an acceptable pick up rate is very difficult. How many negatives can you accept to be satisfied that no injuries are missed? When comparing our results to others we noticed a variable spread of results. Nitecki et al with a liberal use of CTA in a combat setting had abnormal CTAs in 14.5% of cases.17 Busquets et al 19 noted abnormal CTAs in 26.3% of cases and Inaba et al 4 in 34.9% of cases. Seaman et al performed an ABI in patients with soft signs and only did a CTA where the ABI was less than 0.9. In 21 months they performed 21 CTAs and found vascular injuries in 42.9% of cases.2
The most common mechanism of injury in our cohort was gunshot wounds (50%). According to Jawas et al,20 road traffic accidents should be the most common in a civilian population, but Inaba et al4 and Lynch and Johansen13 found gunshot wounds to be the most common.
Our results suggest that clinical examination is unreliable with a sensitivity of 74.4%, specificity of 53.7% and NPV and PPV of 80% and 45.7% respectively. Barnes et al agrees with this stating that an abnormal pulse is not sensitive in predicting surgical lesions.18 Miranda et al found a NPV of 100% with clinical examination.14 Various other authors state that a thorough and sometimes repeated clinical examination is sufficient to rule out vascular injuries.4,15 According to James et al, clinical examination alone is equivalent in safety and accuracy to any other modality.16 Dueck et al stated that, in the absence of hard signs, all significant vascular injuries can be identified by serial clinical examination and injuries discovered do not lead to limb loss.9
An absent pulse (19 patients) is regarded as a hard sign, but due to poor documentation it is not possible to determine whether this group had truly ischaemic limbs or whether they were warm pulses limbs with good capillary refill. Using altered sensation as a surrogate for ischaemia, we found the group with both an absent pulse and altered sensation (5 patients) all required further intervention. Most authors agree that patients with hard signs should undergo emergency exploration.8,919 Both patients in our series who had amputations had an absent pulse on clinical examination and thus, according to international recommendations, should have been taken to theatre for an on-table angiogram and exploration without doing a CTA.
The 'mechanism of injury' group refers to patients with knee dislocations, which is not noted to be a sign of vascular injury, but up to 20% of cases with a knee dislocation and vascular injury will have an amputation15 and this leads to a fear of missing these injuries14 which in turn has led to routine arteriography for knee dislocations. According to Miranda et al,14 physical examination had a NPV of 100% and they recommend that radiological tests are not necessary in the setting of normal physical examination. Using an ABI of 0.9 as a cut off, Mills et al12 showed a sensitivity, specificity, NPV and PPV of 100% in patients with knee dislocations. The use of an ABI or API is not part of the management protocol of patients in our department and not a single one was performed. Of greater concern is the fact that 3 of these patients had patella dislocations.
Proximity to a large vessel as indication for further imaging has been disputed in the literature. In our series using proximity as an indication, one patient with a completely normal physical examination did have a profunda femoral artery injury discovered on CTA, which required intervention. Some authors still advocate that proximity alone should not be an indication for further imaging.8,16 They state that an asymptomatic intimal flap does not need further management and serial clinical examination is sufficient to pick up any deterioration.16,19 According to James et al, only 1.3% of proximity injuries needed surgical intervention and in their series all patients with delayed onset of hard signs presented within a week and had surgical repair without limb loss or morbidity.16 Significant injury is rare in the absence of hard or soft signs.8
The retrospective nature of this review, poor clinical documentation and the lack of a management protocol for patients with suspected vascular injuries are weaknesses of this study.
Conclusion
In our setting, clinical examination is suboptimal and therefore pulse examination is not a reliable indicator of vascular injury. This has led to a lower threshold for ordering CTA and thus substituting a good clinical examination with CTA. Incorrect indications are being used as evidenced by the number of pulseless patients who had CTA performed. Patients with hard signs of vascular injury require emergency on-table angiography and exploration which should not be delayed by obtaining further imaging. The routine use of CTA in patients with knee dislocations should be reconsidered.
We recommend the introduction of a management protocol for patients with a suspected vascular injury, utilising the ABI/API.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
1. Uyeda JW, Anderson SW, Sakai O, Soto JA. CT Angiography in Trauma. Radiol Clin N Am. 2010;48:423-438. [http://dx.doi.org/10.1016/j.rcl.2010.02.003] [PMID: 20609881] [ Links ]
2. Seamon MJ, Smoger D, Torres DM et al. A prospective validation of a current practice: The detection of extremity vascular injury with CT Angiography. J Trauma.2009;67:238-244. [http://dx.doi.org/10.1097/ta.0b013e3181a51bf9] [PMID: 19667874] [ Links ]
3. Rieger M, Mallouhi A, Tauscher T, Lutz M, Jaschke WR. Traumatic arterial injuries of the extremities: Initial evaluation with MDCT angiography. AJR. 2006;186:656-664. [http://dx.doi.org/10.2214/ajr.04.0756] [PMID: 16498092] [ Links ]
4. Inaba K, Potzman J, Munera F, et al. Multi-slice CT angiography for arterial evaluation of the injured lower extremity. J Trauma. 2006;60:502-507. [http://dx.doi.org/10.1097/01.ta.0000204150.78156.a9] [PMID: 16531846] [ Links ]
5. Kauvar DS, Sarfati MR, Kraiss LW. National trauma databank analysis of mortality and limb loss in isolated lower extremity vascular trauma. J Vasc Surg. 2011;53(6):598-603. [http://dx.doi.org/10.1016/j.jvs.2011.01.056] [PMID: 21514772] [ Links ]
6. Patterson BO, Holt PJ, Cleanthis M, Tai N, Carrell T, Loosemore TM. Imaging Vascular trauma. Br J Surg. 2012;99:494-505. [http://dx.doi.org/10.1002/bjs.7763] [PMID: 22190106] [ Links ]
7. Rich NM, Rhee P. A Historical tour of vascular injury management. Surg Clin North Am. 2001;81(6):1199-1215. [http://dx.doi.org/10.1016/s0039-6109(01)80005-0] [PMID: 11766173] [ Links ]
8. Halvorson JJ, Anz A, Langfitt M, et al. Vascular Injury Associated with Extremity Trauma: Initial Diagnosis and Management. J Am Acad Orthp Surg. 2011;19:495-504. [PMID: 21807917] [ Links ]
9. Dueck AD, Kucey DS. The Management of Vascular Injuries in Extremity Trauma. Curr Orthop. 2003;17:287-291. [http://dx.doi.org/10.1016/s0268-0890(03)00104-x] [ Links ]
10. Davenport R, Tai N, Walsh M. Vascular trauma. Surgery. 2009 27(8):331-336. [http://dx.doi.org/10.1016/j.mpsur.2009.06.008] [ Links ]
11. Kohli A, Singh G. Management of Extremity Vascular Trauma: Jammu Experience. Asian Cardiovasc Thorac Ann. 2008;16:212-214. [http://dx.doi.org/10.1177/021849230801600307] [PMID: 18515670] [ Links ]
12. Mills WJ, Barei DP, McNair P. The Value of Ankle-Brachial Index for Diagnosing Arterial Injury After Knee Dislocation: A Prospective Study. J Trauma. 2004;56:1261-1265. [http://dx.doi.org/10.1097/01.ta.0000068995.63201.0b] [PMID: 15211135] [ Links ]
13. Lynch K, Johansen K. Can Doppler pressure measurement replace "exclusion" arteriography in the diagnosis of occult extremity arterial trauma? Ann Surg. 1991;214(6):737-741. [http://dx.doi.org/10.1097/00000658-199112000-00016] [ Links ]
14. Miranda FE, Dennis JW, Veldenz HC, Dovgan PS, Frykberg ER. Confirmation of the Safety and Accuracy of Physical Examination in the Evaluation of Knee Dislocation for Injury of the Popliteal Artery: A Prospective Study. J Trauma. 2002;52:247-252. [http://dx.doi.org/10.1097/00005373-200202000-00008] [PMID: 11834983] [ Links ]
15. Patterson BM, Agel J, Swointkowski MF, Mackenzie EJ, Bosse MJ. Knee dislocations with vascular injury: Outcomes in the lower extremity assessment project study. J Trauma. 2007;36:855-858. [http://dx.doi.org/10.1097/ta.0b013e31806915a7] [PMID: 18090017] [ Links ]
16. Denis JW, Frykberg ER, Veldenz HC, Huffman S, Menawat S. Validation of non-operative management of occult vascular injuries and accuracy of physical examination alone in penetrating extremity trauma. J Trauma. 1998;44(2):243-253. [http://dx.doi.org/10.1097/00005373-199802000-00001] [PMID: 9498494] [ Links ]
17. Nitecki SS, Karram T, Ofer A, Engel A, Hoffman A. Management of Combat Vascular Injuries Using Modern Imaging: Are We Getting Better? Emerg Med Int. 2013;2013:1-6. [http://dx.doi.org/10.1155/2013/689473] [PMID: 23365755] [ Links ]
18. Barnes CJ, Pietrobon R, Higgins LD. Does pulse examination in patients with traumatic knee dislocation predict a surgical arterial injury? A meta-analysis. J Trauma. 2002;53:1109-1114. [http://dx.doi.org/10.1097/00005373-200212000-00013] [PMID: 12478036] [ Links ]
19. Busquets AR, Acosta JA, Colon E, Alejandro K, Rodriguez P. Helical Computed Tomographic Angiography for the Diagnosis of Traumatic Arterial Injuries of the Extremities. J Trauma. 2004;56:625-628. [http://dx.doi.org/10.1097/01.ta.0000053546.28739.cf] [PMID: 15128135] [ Links ]
20. Jawas A, Abbas AK, Nazzal M, Albader M, Abu-Zidan FM. Management of war-related vascular injuries: experience from the second gulf war. World J Emerg Surg. 2013;8:22. [http://dx.doi.org/10.1186/1749-7922-8-22] [PMID: 23816260] [ Links ]
 Correspondence:
Correspondence:
P Jordaan
pieter.suzanne@gmail.com














