Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.4 Cape Town nov. 2016
TRAUMA
Enhanced recovery after surgery (ERAS) in penetrating abdominal trauma: A prospective single-center pilot study
M R Moydien; R Oodit; S Chowdhury; S Edu; A J Nicol; P H Navsaria
Trauma Centre, Department of Surgery, Groote Schuur Hospital and University of Cape Town
ABSTRACT
BACKGROUND: Enhanced recovery after surgery (ERAS) programmes employed in elective surgery have provided strong evidence for decreased lengths of hospital stay without increase in postoperative complications. The aim of this study was to explore the role and benefits of ERAS implemented in patients undergoing emergency laparotomy for penetrating abdominal trauma.
METHODS: Institutional University of Cape Town Human Research Ethics Committee (UCT-HREC) approved study. A prospective cohort of 38 consecutive patients with isolated penetrating abdominal trauma undergoing emergency laparotomy were included in the study. The enhanced recovery protocols (ERPs) included: early urinary catheter removal, early nasogastric tube (NGT) removal, early feeding, early mobilisation/physiotherapy, early intravenous line removal and early optimal oral analgesia. This group was compared to a historical control group of 40 consecutive patients undergoing emergency laparotomy for penetrating abdominal trauma, prior to the introduction of the ERP. Demographics, mechanism of injury, injury severity scores (ISS) and penetrating abdominal trauma index (PATI) were determined for both groups. The primary end-points were length of hospital stay (LOS) and incidence of postoperative complications (Clavien-Dindo classification) in the 2 groups. The difference in means was tested using the t-test assuming unequal variances. Statistical significance was defined as p-value less than 0.05 (p < 0.05).
RESULTS: The two groups were comparable with regards to age, gender, mechanism of injury, ISS and PATI scores. The mean time to solid diet, urinary catheter and nasogastric tube (NGT) removal was 3.6 (non-ERAS) and 2.8 (ERAS) days [p < 0.035], 3.3 (non-ERAS) and 1.9 (ERAS) days [p < 0.00003], 2.1 (non-ERAS) and 1.2 (ERAS) days [p < 0.0042], respectively. There was no difference in time from admission to time of laparotomy 313 (non-ERAS) vs 358 (ERAS) minutes [p < 0.07]. There were 11 and 12 complications in the non-ERAS and ERAS groups, respectively. When graded as per the Clavien-Dindo classification, there was no significant difference in the 2 groups (p < 0.59). Hospital stay was significantly shorter in the ERAS group: 5.5 (SD 1.8) days vs. 8.4 (SD 4.2) days [p < 0.00021].
CONCLUSION: This pilot study shows that ERPs can be successfully implemented with significant shorter hospital stays without any increase in postoperative complications in trauma patients undergoing emergency laparotomy for penetrating abdominal trauma.
Introduction
Enhanced recovery after surgery (ERAS) or enhanced recovery protocols (ERP) is a concept first described by Kehlet in the early 1990s.1 Since its introduction, ERAS protocols have been successfully used in elective gastrointestinal surgery (colorectal, hepatobiliary and gastric), and there has been widespread acceptance and implementation in other surgical disciplines including urology, vascular and thoracic surgery and orthopaedics.1-8 The approach employs a multimodal perioperative care pathway designed to attenuate the surgical stress response and accelerate postoperative recovery.2 Implementation of ERPs across a range of surgical disciplines has led to improved patient outcomes including reductions in postoperative complications and hospital length of stay. Trauma centres in developing countries constantly battle with reduced bed availability and restricted health care budgets. Optimization of health care practice is therefore urgent, particularly in trauma surgery. The benefits of ERAS/ERPs are well established. They have shown faster physiological patient recovery, and reduced length of hospital stay without an increase in postoperative complications.7,8 These benefits should be easily transferable to the trauma patient population, if not greater, since trauma patients are generally younger, fitter and metabolically stable. Penetrating abdominal trauma is a major cause of morbidity and mortality in large urban trauma centres. It accounts for a significant number of hospital admissions and consumes a large portion of the health care budget. We developed and implemented an ERP for patients undergoing emergency laparotomy for isolated penetrating abdominal trauma and analysed the effect of this protocol.
Methods
Approval for the study was granted by the Department of Surgery Research Committee and the University of Cape Town Faculty of Health Sciences Human Research Ethics Committee. Stable patients presenting to Groote Schuur Hospital Trauma Centre (GSHTC) with isolated penetrating abdominal trauma (stab (SW) and gunshot (GSW) wounds) that required an emergency laparotomy over a one year period from 1 January to 31 December 2013 were analysed. Patients with extra-abdominal injuries, those that required damage control surgery, and patients requiring intensive care unit admission for postoperative support were excluded from the study.
During the first half of the year patients were recruited into the control group. In July 2013, we implemented our ERP and began treating patients that met all the inclusion criteria as per our ERP. We recruited 38 consecutive patients from July to December 2013. Based on ERAS consensus guidelines, an ERP was designed.2 The ERP included: early nasogastric tube (NGT) removal, early urine catheter removal, early intravenous line removal, early feeding with early fluid and solid diet initiation, early mobilization/physiotherapy, and early optimal oral analgesia. Postoperative day 1 was defined as the 'early' target which we aimed to achieve. Criteria for early discharge included: tolerance of solid diet, pain control on oral analgesia and independent mobilization. We aimed for 'early' discharge on postoperative day 3 to 4. In our study, the postoperative pain protocol consisted of a morphine infusion for up to 48 hours and paracetamol infusion for 24 hours. Thereafter patients where converted to oral analgesia (paracetamol and tramadol) and intramuscular morphine for breakthrough pain. All patients were mobilized on the first postoperative day with the help of nursing staff and physiotherapists, with the goal of having all patients fully independent by day 3. This approach to postoperative pain control and mobilization was already well established in our unit and all patients in both the control and study group benefited from it. Early mobilization and early optimal oral analgesia was therefore similar for both groups.
The ERP was implemented and a prospective cohort of 38 consecutive patients analysed (July - December 2013). This group was compared to a historical control group of 40 consecutive patients (January - June 2013) undergoing emergency laparotomy for penetrating abdominal trauma, prior to introduction of the ERP. Demographic data, adherence to the ERP, length of hospital stay and postoperative complications as per Clavien-Dindo classification were analysed. The primary end-points were length of hospital stay and incidence of postoperative complications. Statistical analysis was performed using Microsoft Excel and Stata. T-test was performed comparing means and statistical significance was defined as a p-value < 0.05.
Results
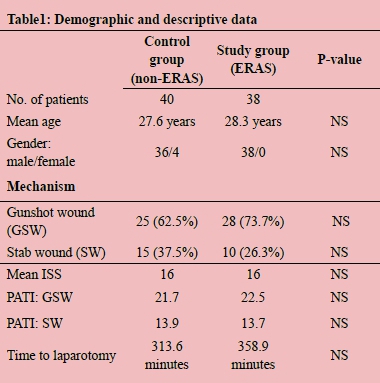
The study included 78 patients (38 - ERAS and 40 - nonERAS). The 2 groups were comparable with regard to age, gender, mechanism of injury, injury severity scores (ISS), penetrating abdominal trauma index (PATI) score and time to laparotomy (Table 1). The mean time to initiation of solid diet, urinary catheter removal and NGT removal was 3.6 (non-ERAS) and 2.8 (ERAS) days [p < 0.035], 3.3 (nonERAS) and 1.9 (ERAS) days [p < 0.00003], 2.1 (non-ERAS) and 1.2 (ERAS) days [p < 0.0042], respectively (Figure 1). Patients in the ERAS group had statistically significant earlier removal of NGTs, urinary catheters and earlier initiation of solid diet. The Clavien-Dindo classification system was used to record postoperative complications (Table 2). There were 11 and 12 complications in the non-ERAS and ERAS group, respectively. When graded as per the Clavien-Dindo classification, there was no statistically significant difference in postoperative complications grade for grade, and overall between the non-ERAS and ERAS group (p < 0.59). Mean hospital length of stay (LOS) was 5.5 days (SD 1.8) in the ERAS group and 8.4 days (SD 4.2) in the non-ERAS group (Figure 1). The shorter LOS in the ERAS group was statistically significant, (p < 0.00021).


Discussion
ERAS programmes have consistently been shown to have both cost-related and patient-related benefits.
King et al. examined the influence of an ERP on clinical outcome, cost and quality of life after surgery for colorectal surgery.9 They found that hospital stay was significantly reduced when patients where managed according to an ERP, with a 49% reduction in length of stay in the ERP group compared to the conventional care arm. They also showed no transfer of costs onto another health care industry. In a meta-analysis of randomized controlled trials evaluating health outcomes and resource utilization, patients adhering to the ERP had reduced length of stay of 2.5 days, and this was a reproducible improvement in the quality of care by enabling standardization of health care processes.10 Similarly, our study confirms this concept with a 35% reduction in hospital stay. Duration of hospital stay and perioperative morbidity and complication rates are key determinants of cost. Abdominal surgery is associated with postoperative pain, paralytic ileus, reduced pulmonary function and loss of muscle mass and function, all of which may contribute to postoperative morbidity and need for prolonged hospital stay. ERPs aim to reduce these postoperative complications by preserving the normal preoperative physiology. In the trauma patient, we aim to maintain the 'pre- injury' physiological status. Improving patient outcomes with reduced morbidity and early hospital discharge enables us to reduce the cost of treating this group of patients. The presence of trans-urethral catheters increases the incidence of urinary tract infection and hinders patient mobilization. Patients treated as per an ERP frequently achieve their treatment targets and this avoids treatment deviation by different treating physicians. This was evident in the ERAS arm of our study, where urine catheters were consistently removed earlier in the ERAS group compared to the non-ERAS group (1.9 days vs 3.3 days). There were no urinary tract infections observed in either group and all patients achieved early independent mobilization after urinary catheter removal. Preservation of body composition is vital in order to reduce postoperative morbidity. Early oral nutrition with protein drinks will preserve lean body mass and maintain work performance. All our patients were started on Fresubin protein drinks on postoperative day 1 (2 x 200 ml Fresubin 2 kcal/ml drink per day providing 40 g protein and 800 kcal). Full ward diet was initiated by day 2 to 3. In the ERAS arm of our study, patients were initiated on solid diet by 2.8 days compared to 3.6 days in the traditionally treated arm, showing earlier initiation of solid diet, if patients are managed as per the ERP. The presence of a nasogastric tube has been shown to hinder initiation of oral intake. As per our ERP, NGTs were consistently removed earlier, after 1.2 days compared to 2.1 days in the traditionally treated arm. This earlier removal of NGTs facilitated earlier initiation of oral intake. Early removal of NGTs, early initiation of liquid and solid diet and early ambulation is associated with earlier return of bowel function and earlier discharge from hospital. In our study, 4 patients in the ERAS arm and 2 patients in the traditionally treated arm developed postoperative ileus. All cases resolved successfully within 3 to 4 days. We were able to demonstrate early removal of NGTs with early initiation of oral nutrition and early mobilization. Early optimal analgesia and early mobilization with physiotherapy are means of improving pulmonary function. Our patients received dedicated chest physiotherapy and were given and taught how to administer a positive end-expiratory pressure (PEEP) bottle which has been shown to reduce pulmonary atelectasis. However, 2 patients developed nosocomial pneumonia requiring antibiotics. This was diagnosed by the increased oxygen requirements, pulmonary crepitations, radiological changes on chest radiograph, and elevated white cell counts. Implementation of ERAS programmes are feasible as long as they are safe. The shortened LOS is of no benefit, if it leads to increase incidence of postoperative complications. There were 12 complications in the ERAS arm and 11 in the traditionally treated arm. However, when analysed there was no statistically significant difference between the 2 groups. This showed that the benefit of reduced LOS can be achieved without any increase in incidence of postoperative complications.
Conclusion
This small pilot study shows that enhanced recovery protocols can be successfully implemented with significant shorter hospital stays without any increase in postoperative complications in a select group of trauma patients undergoing emergency laparotomy for isolated penetrating abdominal trauma. Furthermore, the study shows that enhanced recovery protocols can also be applied to patients undergoing emergency surgery. Given the fact that penetrating abdominal trauma remains a substantial burden of disease, especially in developing countries such as South Africa, this proven approach to patient care in elective surgery can now be safely employed in the trauma and emergency setting.
REFERENCES
1. Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;(78):606-617. [ Links ]
2. Lassen K, Soop M, Nygren J, et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144(10):961-969. [ Links ]
3. Wind J, Polle SW, Fung Kon Jin PHP, et al. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006:800-809. [ Links ]
4. Throop PP. Infrarenal aortic surgery with a 3-day hospital stay: a report of success with a clinical pathway. J Vasc Surg. 1999;(29):787-792. [ Links ]
5. Tovar EA, Roethe RA, Weissig MD, et al. One-day admission for lung lobectomy: An incidental result of a clinical pathway. Ann Thorac Surg. 1998;(65):803-806. [ Links ]
6. Arumainayagam N, McGrath J, Jefferson KP, et al. Introduction of an enhanced recovery protocol for radical cystectomy. BJU Int. 2008;(101):698-701. [ Links ]
7. Nicholson A, Lowe MC, Parker J, et al. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg. 2014;101(3):172-188. [ Links ]
8. Anderson ADG, McNaught CE, MacFie J, et al. Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg. 2003;(90):1497-1504. [ Links ]
9. King PM, Blazeby JM, Ewings P, et al. The influence of an enhanced recovery programme on clinical outcomes, costs and quality of life after surgery for colorectal cancer. Color Dis. 2006;(8):506-513. [ Links ]
10. Adamina M, Kehlet H, Tomlinson GA, et al. Enhanced recovery pathways optimize health outcomes and resource utilization: A meta-analysis of randomized controlled trials in colorectal surgery. Surgery. 2011;830-840. [ Links ]
 Correspondence:
Correspondence:
Pradeep H Navsaria
pradeep.navsaria@uct.ac.za














