Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.3 Cape Town Sep. 2016
ORIGINAL ARTICLES
Outcomes in laparoscopic cholecystectomy in a resource constrained environment
S Z MbathaI; F AndersonII
IConsultant, Addington Hospital. Department Of Surgery, Nelson R Mandela School ofMedicine, University of KwaZu-lu-Natal
IIHead of Department - Specialised Surgery, Inkosi Albert Luthuli Hospital. Department of Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
ABSTRACT
BACKGROUND: Laparoscopic cholecystectomy (LC) is a common surgical procedure performed for symptomatic gallstones. There is a trend towards early cholecystectomy for patients with acute cholecystitis who present timeously. Local inflammation has been identified as a risk factor for bile duct injuries. This study sought to assess the outcomes of LC in patients managed within a resource constrained environment where late presentation is common.
METHODS: We performed a retrospective analysis of laparoscopic cholecystectomy performed from January 2010 to June 2011. The mode of presentation, co-morbidities, timing of cholecystectomy and complications were analysed.
RESULTS: One hundred and sixty seven patients were evaluated. The median age was 43 years with range (17-78) years and 93% were female and 7% male. There were 44%, 23%, 20% and 13% who presented with biliary colic, acute pancreatitis, acute cholecystitis and obstructive jaundice respectively. Nine (5.4%) patients required conversion to an open cholecystectomy. Complications occurred in 16.2% and bile duct injuries and bile leaks in 1.2% and 1.8% respectively. One patient died.
CONCLUSIONS: Most patients had a delayed laparoscopic cholecystectomy. There was no difference in outcomes for the different presentations and the complications are similar to other reports.
Key words: laparoscopic, cholecystectomy, complications
Introduction
Gallstones are found in 9.7% (2.5-13.9%) of the population in South Africa.1 The common modes of presentation of gallstone disease are biliary colic, acute cholecystitis, acute pancreatitis and obstructive jaundice. Laparoscopic cholecystectomy is one of the most commonly performed operations in general surgery2 and is considered the standard of care for symptomatic gallstones. In patients with acute cholecystitis, early cholecystectomy within 72 hours of symptom onset is commonly practised and results in a shorter hospital stay without an increase in conversion rates or complications.3 In our environment, laparoscopic cholecystectomy is performed in regional hospitals which act as referral centres for patients referred from primary and district services. Prolonged interhospital transfer invariably leads to delayed admission.
Bile duct injuries and bile leaks are recognised as the most serious complications of laparoscopic cholecystectomy and have a reported incidence of 0.5% and 0.38% respectively.2 Risk factors for bile duct injuries include inflammation resulting in anatomical distortion, as well as anatomical variations. The prevention of bile duct injury may be aided by the use of intraoperative cholangiography4 and ensuring a critical view of safety prior to ligation of the cystic artery and duct. 5
Despite being a regional hospital, there are challenges which result in delays in cholecystectomy. These include the availability of theatre time, delay in obtaining a preoperative ultrasound, a lack of intraoperative screening facilities and the absence of on-site endoscopic retrograde cholangiopancreatography (ERCP) services resulting in delay in the preoperative clearance of bile duct stones. We performed an audit to assess our outcomes in relation to international norms.
Patients and methods
We performed a retrospective chart review of all patients who underwent a laparoscopic cholecystectomy from January 2010 to June 2011. The patient list was extracted from a theatre register and the charts retrieved from the Medical Records Department. Patients planned for open cholecystectomy were excluded. We only perform cholecystectomy in adults and the youngest patient was 17 years old. We analysed patient demographics, co-morbidities, mode of presentation, timing of cholecystectomy, conversion rate, perioperative complications and mortality.
Patients with biliary colic were booked on the elective theatre list. Acute cholecystitis was treated with a full course of antibiotics and patients who responded were booked for the LC on the next available elective list a few weeks after discharge. In patients with cholestasis at presentation, serial monitoring of the liver function tests was performed, and in those showing resolution by day 5-7, laparoscopic cholecystectomy was performed on the next available elective list. Those with persistent cholestasis and those with cholangitis had preoperative ERCP for biliary decompression. Intraoperative cholangiography was not performed due to resource constraints and preoperative ERCP was performed in all patients with suspected choledocolithiasis.
In this series, four ports were used with emphasis on lateral retraction of the gallbladder neck and obtaining the critical view of safety before ligation of the cystic duct and artery.
Statistical analysis was conducted using the IBM SPSS package Version 2.0. Descriptive analysis was conducted and chi-square tests (Pearson and Fischer exact) applied to assess for statistical significance between various associations. Results were considered statistical significant if the p-value < 0.05. The study was approved by ethics committees of University of KwaZulu-Natal (Ethics Ref no: BE014/13) and Provincial Department of Health.
Results
Clinical records of 167 (80%) of 210 consecutive patients who had laparoscopic cholecystectomy during this period were found to be complete and were considered adequate for analysis.
Demographics, clinical parameters and outcomes of patients for the different clinical presentations are shown in Table 1.
The median age was 43 years with range (17-78) years. Ninety-five (57%) had comorbidities. Fifty-four (32%) had hypertension and/or diabetes. The majority of patients presented with biliary colic. There was no difference in the mean age of patients between the different presentations of gallstone disease. Four (11.8%) of the 34 patients with acute cholecystitis presented within 72 hours and had cholecystectomies within a week of admission as a result of a failed strategy of initial conservative management. The remainder presented later than 72 hours and had symptom resolution with antibiotics.
One patient with biliary colic developed acute cholecystitis while awaiting surgery. There were no recurrent symptoms in the rest of the patients whilst awaiting LC.
Seventy-one per cent (n=15) of patients with obstructive jaundice had ERCP prior to surgery; the others showed improvement in liver function tests (LFTs) and had LC once bilirubin and enzymes normalised.
There were 20 (12%) patients who were infected with HIV and 9 were on antiretroviral therapy. Seven of the 20 HIV infected patients had obstructive jaundice at presentation (p=0.009). One female had features suggestive of AIDS cholangiopathy at ERCP and EUS (Endoscopic Ultrasound). She was on antiretroviral therapy with a CD4 count of 334. She had an uneventful cholecystectomy 5 days after ERCP and was discharged 2 days later. There was no significant correlation between HIV infection and complications. Fifty per cent (n=10) of the HIV infected patients had inflamed gallbladders at surgery (p=0.111) and 15% (n=3) developed complications (p=0.978).
At surgery 34% (57/167) of gallbladders were reported as inflamed and 11% had adhesions around the gallbladder. Of the patients with complications, 59% (16/27) had an inflamed gallbladder at surgery (p=0.003) and 38.9 % (7 of 27) had adhesions (p=0.012).
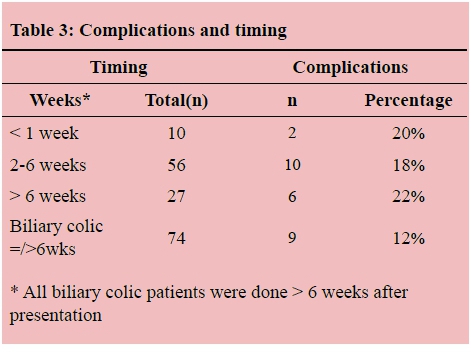
The overall complication rate was 16.2%. The spectrum of significant complications is illustrated in Table 2, whilst Table 3 shows complications in relation to the timing of operations.
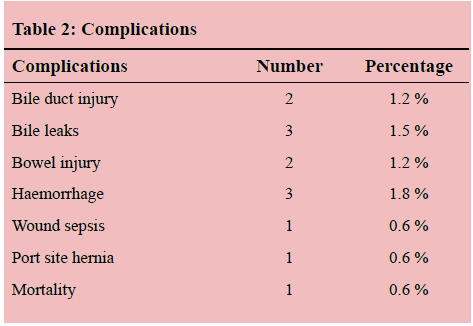
Two patients (1.2%) sustained common bile duct injuries.
One was 38 years old, presented with gallstone pancreatitis and had a cholecystectomy 4 weeks after initial presentation. She was found to have an inflamed gallbladder adherent to the bile duct. A major Strasberg Type D duct injury was recognised intraoperatively and a successful hepatico-jejunostomy was performed. The second patient had a minor bile leak (Strasberg Type D) postoperatively which was managed endoscopically.
Three patients (1.8%) had bile leaks postoperatively. The first is mentioned above. The second had a slipped cystic duct Liga-clip (Strasberg Type A Injury) successfully managed laparoscopically. The third patient had a Mirizzi Type stricture managed by an open cholecystectomy. She had a retained stone at ERCP and required a hepatico-jejunostomy because of an associated distal bile duct stricture (Strasberg Type E1). She recovered after a prolonged hospital stay.
Bowel injury occurred in two patients. One had an umbilical hernia and another had previous abdominal surgery. Both were converted to open procedures and an injury to the colon and small bowel were repaired respectively. Both had an uneventful postoperative course.
Three patients had significant bleeding, according to the operating surgeon. Two were from the liver bed and were managed laparoscopically and the third from a port site which required open surgical exploration to ligate the offending vessel.
Nine (5%) patients required conversion to an open cholecystectomy for various reasons: bile duct injury (n=1), inflamed GB with empyema and colonic injury (n=1), lateral tear of dilated cystic duct (n=1), Mirizzi syndrome (n=3), adhesions from previous laparotomy (n=1), adhesions and small bowel injury (n=1), sealed GB perforation with adhesions (n=1).
Six (3.6%) patients had gallbladder perforations with stone spillage. One of these developed postoperative pneumonia and adrenal insufficiency which were successfully managed. None of the other patients had complications associated with spilled stones.
At review after discharge, 1 patient had a pelvic fluid collection which was successfully managed expectantly. Another patient had persistent cholestasis without retained stones at ERCP. This had resolved at 6 months. In another, port sepsis was successfully managed with antibiotics and in another a retained stone was managed by ERCP. One patient developed an umbilical site hernia at 4 months.
One patient died. This was a 76-year-old female with hypertension who presented with acute cholecystitis and non-resolving sepsis with antibiotics. A gangrenous gallbladder with a sealed perforation was removed. She died as a result of severe sepsis.
Despite the delays to surgery, the recovery was rapid with 148 (87%) patients discharged within 72 hours of their surgery. Table 4 presents the follow-up periods.
Discussion
Laparoscopic cholecystectomy is the standard of care for symptomatic gallstones. Gallstones present with biliary colic, acute cholecystitis, gallstone pancreatitis and obstructive jaundice related to choledocolithiasis or Mirizzi syndrome. Acute cholecystitis varies from mild inflammation to severe disease associated with systemic sepsis and/or empyema, gangrene and perforation of the gallbladder. In patients presenting with severe acute gallstone pancreatitis, jaundice and cholangitis may require urgent biliary decompression.
The timing of cholecystectomy in acute cholecystitis has evolved with good results demonstrated in patients who undergo early cholecystectomy within 72 hours,6,7 from onset of symptoms. Early cholecystectomy may result in more conversions to open surgery89 whereas delays in cholecystectomy are associated with recurrent symptoms.10 In a meta-analysis that analysed early (within 7 days) versus late (after 6 weeks) cholecystectomy for acute cholecystitis, early cholecystectomy was associated with a reduced total hospital stay, longer operation time and no difference in overall postoperative morbidity or conversion rates.3 The circumstances within our local health care system dictate that the majority of our patients fall into the category of delayed laparoscopic cholecystectomy. In this study, only 11.8 % of acute cholecystitis patients presented within 72 hours and 68% of operations were performed between 2-6 weeks, with a complication rate that is similar to published studies. Our timing of operations was significantly influenced by availability of theatre time and tended to be similar for all presentations except biliary colic; and most operations were performed in the 2-6 week period for the other three presentations, with slightly higher complication rate occurring in operations done after 6 weeks (17% vs 22% respectively). We had more complications in patients presenting with pancreatitis and obstructive jaundice than in those with acute cholecystitis.
The means available to prevent bile duct injury are routine intraoperative cholangiography (IOC) and ensuring a critical view of safety. The routine use of intraoperative cholangiography is controversial11 and the critical view of safety may be more effective with less cost.8 Cholangiography may then be limited to assessing for suspected bile duct stones.9 Waage & Nilsson, in their large population-based study, examined risk factors for iatrogenic bile duct injury (BDI) and found that their data 'suggest a protective effect of IOC against BDI, reducing the risk by 34%,'12 whilst Törnqvist et al. found that the use of IOC was associated with a reduced risk of bile duct injury only in acute cholecystitis.13 Due to limited access to IOC, we place more emphasis on the surgical technique and obtaining the critical view of safety. Chronic or severe acute inflammation and adhesions resulted in anatomical distortions and difficulty obtaining the critical view of safety. Five of the nine conversions had severe inflammation with three having Mirizzi syndrome. Despite not performing IOC, our bile duct injuries were in line with previous studies and we only had one patient with a retained CBD stone. We sent patients for ERCP prior to surgery in suspected bile duct stones which were found in 35% of the ERCPs. The conversion rate of 5% compares to a previous study with 3.6%.14
Stone spillage occurs in 5-40% of laparoscopic procedures and results in complications in < 1% of cases. Routine conversion to an open procedure is not recommended.15,16 In this series, stone spillage occurred in 6 (3.6%) patients without complications at outpatient review.
Conclusion
Few patients presented early with complicated gallstones in this study. Patients undergoing cholecystectomy after 6 weeks had more complications and performing cholecystectomies earlier than 6 weeks may improve our complication rates. There is no difference in the complication and conversion rates between the different modes of presentation of gallstones and these are comparable to other published series. HIV infection did not influence the outcomes.
References
1. Brett M, Barker D. (1976) The world distribution of gallstones. International journal of epidemiology. 5(4):335-41. [ http://dx.doi.org/10.1093/ije/5.4.335] [PMID: 1010661] [ Links ]
2. MacFadyen Jr B, Vecchio R, Ricardo A, et al (1998) Bile duct injury after laparoscopic cholecystectomy. Surgical endoscopy. 12(4):315-21. [http://dx.doi.org/10.1007/s004649900661] [PMID: 9543520] [ Links ]
3. Siddiqui T, MacDonald A, Chong PS, et al (2008) Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. The American Journal of Surgery. 195(1):40-7. [http://dx.doi.org/10.1016/j.amjsurg.2007.03.004] [PMID: 18070735] [ Links ]
4. Alvarez F, de Santibanes M, Palavecino M, et al (2014). Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. British Journal of Surgery. 101(6):677-84. [http://dx.doi.org/10.1002/bjs.9486] PMID: 24664658] [ Links ]
5. Strasberg SM. (2002) Avoidance of biliary injury during laparoscopic cholecystectomy. J Hep Bil Pancr Surg. 9(5):543-7. [http://dx.doi.org/10.1007/s005340200071] [PMID:12541037] [ Links ]
6. Lo C-M, Liu C-L, Fan S-T, et al (1998) Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Annals of surgery. 227(4):461. [http://dx.doi.org/10.1097/00000658-199804000-00001] [PMID: 9563529] [PMCID: PMC1191296] [ Links ]
7. Stevens KA, Chi A, Lucas LC, et al (2006) Immediate laparoscopic cholecystectomy for acute cholecystitis: no need to wait. The American journal of surgery.192 (6):756-61. [http://dx.doi.org/10.1016/j.amjsurg.2006.08.040] [PMID: 17161089] [ Links ]
8. Avgerinos C, Kelgiorgi D, Touloumis Z, et al (2009) One thousand laparoscopic cholecystectomies in a single surgical unit using the "critical view of safety" technique. Journal of Gastrointestinal Surgery.13 (3):498-503. [http://dx.doi.org/10.1007/s11605-008-0748-8] [PMID: 19009323] [ Links ]
9. Sanjay P, Fulke JL, Exon DJ (2010) "Critical view of safety" as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. Journal of Gastrointestinal Surgery. 14(8):1280-4. [http://dx.doi.org/10.1007/s11605-010-1251-6] [PMID: 20535578] [ Links ]
10. Mercer SJ, Knight JS, Toh SK, et al (2004) Implementation of a specialist-led service for the management of acute gallstone disease. British journal of surgery.91 (4):504-8. [http://dx.doi.org/10.1002/bjs.4458] [PMID: 15048757] [ Links ]
11. Ford J, Soop M, Du J, et al (2012) Systematic review of intraoperative cholangiography in cholecystectomy. British Journal of Surgery.99 (2):160-7. [http://dx.doi.org/10.1002/bjs.7809] [PMID: 22183717] [ Links ]
12. 15. Waage A, Nilsson M, (2006) Iatrogenic Bile Duct Injury: A Population-Based Study of 152 776 Cholecystectomies in the Swedish Inpatient Registry. Archives of Surgery. 141(12):1207-1213. [http://dx.doi.org/10.1001/archsurg.141.12.1207] [ Links ]
13. Törnqvist B, Strömberg C, O. Akre O. et al (2015) Selective intraoperative cholangiography and risk of bile duct injury during cholecystectomy. BJS 102: 952-958 [http://dx.doi.org/10.1002/bjs.9832] [ Links ]
14. Cuschieri A, Dubois F, Mouiel J, et al (1991) The European experience with laparoscopic cholecystectomy. The American journal of surgery. 161(3):385-7. [http://dx.doi.org/10.1016/0002-9610(91)90603-B] [PMID: 1825763] [ Links ]
15. Sathesh-Kumar T, Saklani A, Vinayagam R, et al (2004) Spilled gall stones during laparoscopic cholecystectomy: a review of the literature. Postgraduate medical journal. 80(940):77-9. [http://dx.doi.org/10.1136/pmj.2003.006023] [PMID: 14970293] [PMCID: PMC1742934] [ Links ]
16. Hawasli A, Schroder D, Rizzo J, et al (2002) Remote complications of spilled gallstones during laparoscopic cholecystectomy: causes, prevention, and management. Journal of Laparoendoscopic & Advanced Surgical Techniques. 12(2):123-8. [http://dx.doi.org/10.1089/10926420252939664] [PMID: 12019573] [ Links ]
 Correspondence:
Correspondence:
Mbatha, Sikhumbuzo Zuke
sizumba@live.com














