Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.2 Cape Town Jun. 2016
ABSTRACTS
Abstracts of the 43rd Annual Meeting Surgical Research Society of Southern Africa
Plenary session
Prize Session: Bunny Angorn and Bert Myburgh
LAPAROSCOPY (TO DETECT OCCULT DIAPHRAGM INJURY) VERSUS CLINICAL AND RADIOLOGICAL FOLLOW UP TO DETECT DIAPHRAGM INJURY AND HERNIATION, IN PATIENTS WITH ASYMPTOMATIC LEFT THORACOABDOMINAL STAB WOUNDS: A PROSPECTIVE RANDOMIZED CONTROLLED STUDY
G F Malherbe, P H Navsaria, A J Nicol, S Edu, S Chowdhury
Trauma Centre, Groote Schuur Hospital, University of Cape Town, South Africa
Background: The need to exclude occult diaphragmatic injury in left thoracoabdominal (TA) stab wounds continues to be controversial. Current trauma guidelines recommend either routine diagnostic thoracoscopy or laparoscopy and repair of an injury if found.
Objective: To determine if asymptomatic patients with left sided (TA) stab wounds can be treated with careful clinical and chest X-ray follow up to ascertain healing of occult injuries.
Methods: A parallel-group, prospective, randomized control study was conducted at the Trauma Centre at the Groote Schuur Hospital from 01 September 2009 through to 01 November 2014. All patients with asymptomatic left TA stab wounds included in the trial were randomized into two groups. Group A underwent diagnostic laparoscopy to exclude a diaphragm injury, and Group B underwent clinical and radiological follow up.
Results: Twenty seven patients were randomized to Group A (n=27) and thirty one to Group B (n=31). All patients were young males with a median age of 26 years (range from 18 to 48). The incidence of occult diaphragm injury in group A was 29%. Occult injuries found at laparoscopy were all repaired. All patients in group 2 had normal chest X-rays and no symptoms at their last visit. The mean follow up time was 24 months (range of 0 to 58). There was no morbidity nor mortality associated with the conservative management of occult diaphragmatic injuries. The mean hospital stay for the patients in Group A was 5 days (SD 1.3), compared to a mean hospital stay of 2.9 days (SD, 1.5) p < 0.001, in Group B.
Conclusions: Clinical and radiological follow up is feasible and appears to be safe in patients with occult diaphragm injuries after left TA stab wounds.
DOES THE REPORTING OF UPPER GASTROINTESTINAL ENDOSCOPY AT A TERTIARY HOSPITAL MEET THE MINIMAL STANDARD TERMINOLOGY?
S P Maharaj, M A Noorbhai, T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban, South Africa
Background: The Minimal Standard Terminology (MST) was developed in order to standardise endoscopic reporting.
Purpose: This study was aimed at assessing the current reporting at a tertiary hospital and whether it meets MST criteria.
Methods:
• Setting: Gastrointestinal Unit, King Edward VII Hospital, Durban, a tertiary teaching hospital.
• Design: Retrospective observational study to compare our reporting to the MST reporting standard (version 3.0). Data were extracted from 100 random endoscopy reporting forms from January to June 2014.
• Study endpoints: The Noorbhai Maharaj Gastrointestinal Reporting Score was devised as a tool to assess and grade the quality of reporting and it incorporates demographic details, indication for endoscopy, report legibility and sedation use variables listed in MST as well as use of known classification systems to describe pathology.
• UKZN Ethics reference: BE379/14
Results: One hundred upper endoscopy reports were analysed. Indications for endoscopy were stated in only 51 reports. Use of pre-procedural sedation was not stated in 51 reports. The endoscopist was registrar in training (54), junior consultant (36), senior consultants (9) and illegible (1). Four reports were illegible [conducted by junior consultant (1) forth year registrar (2) and unknown endoscopist (1)].
Distance to the O-G Junction was not recorded in 70 reports. Among 22 reports of oesophagitis, the LA classification was complete (9), incomplete (3) and not used at all (10).
Reports on gastritis were left blank (14) or reported as "No abnormality" (18). Gastritis was graded in 3 with no use of any classification. Four of 10 reports on ulceration used Forrest classification and none used Johnson classification. Reports on 'masses' made no mention of site or biopsy. Report on duodenitis was left blank (25) or reported as 'No abnormality' (68).
Conclusion: Endoscopy reporting in our setting is inadequate and does not meet MST standards.
MAJOR ARTERIAL INJURY OF THE LOWER LIMB: OUTCOME OF REPAIR
E Schroeder
Division of Surgery, University of Stellenbosch
Introduction: Lower limb vascular injury is a common presentation to our high volume level one trauma centre. It may be associated with high volume blood loss and distal limb ischaemia. A high rate of amputations is anticipated if these injuries are not managed in a timeous and expert manner.
Aims: The primary aim is to evaluate our Trauma Surgery Unit's performance in managing these injuries by determining secondary amputation rates. A secondary aim is to identify factors associated with worse outcomes, thereby developing a profile of the high risk patient to be recognized on admission and prioritized for rapid surgical evaluation.
Methods: A retrospective cohort study was designed, including all repairs of major penetrating arterial injuries from the infra-inguinal femoral vessels up to the infra-genicular popliteal vessels, performed on adults during the six year study period. Repairs performed on vessels below the trifurcation of the popliteal artery were excluded. Cases were identified from complete emergency theatre records for the study period, from January 2008 to December 2013. Subgroup analysis of the outcomes for each named vessel, as well as for mechanism of injury and associated injuries were performed.
Results: The final analysis consisted of 76 patients of which 96% were male, with a median age of 25 years (range 14- 45 years). Most injuries were to the superficial femoral artery (57.9%), followed by the popliteal artery (26.3%), the profunda femoris artery (10.5%) and the common femoral artery (7.9%). Most injuries were caused low velocity gunshot wounds (71%). The overall secondary amputation rate was 6.6%. The highest incidence of secondary amputation (20%) occurred in the popliteal artery injury group, compared to a secondary amputation rate of 2.2% for superficial femoral artery injuries. Compartment syndrome was documented in 38.8% of the study group with an associated amputation rate of 17.8%. Factors associated with a high risk of amputation were gunshot wounds (p=0.001), compartment syndrome (p=0.001) and concurrent fracture of the femur (p=0.002).
The majority of patients (60.6%) were successfully operated on clinical suspicion alone without the need for pre-operative imaging.
Conclusion: Lower limb arterial injury is associated with a high rate of secondary amputation if caused by gunshot wounds that involve the popliteal segment. Patients with suspected popliteal artery injury and signs of distal ischaemia require urgent surgical evaluation and repair to ensure limb salvage.
CLINICOPATHOLOGICAL SPECTRUM OF NEUROENDOCRINE TUMOURS IN THE KWAZULU-NATAL TEACHING HOSPITALS
P N Mthethwa, T E Madiba
Department of Surgery & The SAMRC/UKZN Gastrointestinal Cancer Research Centre, University of KwaZulu-Natal, Durban, South Africa.
Ethics approval: UKZN BREC Ref No.: BE229/13
Background: Neuroendocrine tumours (NETs) are rare epithelial tumours of the diffuse neuroendocrine system of the gastrointestinal tract. There is scarcity of data on NETs in South Africa.
Aim: To establish hospital prevalence and clinicopathologic characteristics of NETs in our geographical setting.
Methods:
• Study setting: Surgical Gastroenterology Unit at a Tertiary Teaching Hospital.
• Study design: Retrospective analysis (2000-2014) of an on-going prospectively collected NET database into which all patients from KZN Province of South Africa are enrolled. Data included demographics, clinical presentation, disease distribution, histopathological assessment, treatment and follow-up.
• Study endpoints: clinicopathologic spectrum, treatment outcome.
Results: A total of 57 patients have been enrolled during the period of 14 years, comprising of Indians (40.3 %), Africans (40.3 %), Whites (14.0%) and Coloureds (5.2 %). The median age was 62.5 years. Twenty seven were males (M:F ratio 1:1). Common clinical features were abdominal pain (32), change in bowel habit (6) and abdominal mass (3). Median duration of symptoms was 6 months. Tumour complications were carcinoid syndrome (8), obstruction (3) obstructive jaundice (1) and incarcerated hernia (1). The most common sites involved were the rectum (13), pancreas (9), stomach (9) and small bowel (9).Thirty patients had metastatic disease with metastases, with target organs being liver (25) and lungs (6). Chromogranin A was assessed in 22 patients and 10 patients underwent WHO grading. Twenty one patients underwent resection. Oncology treatment was chemotherapy (16), radiotherapy (2), Octreotide (13) and no treatment (17). During the median follow-up of 55 months, five patients developed new metastases and there were 9 confirmed deaths.
Conclusion: The rectum is the most common anatomical location. Neuroendocrine carcinoma is the most common histological type. The disease tends to present at an advanced stage with a high metastatic rate resulting in a reduced resection rate. Lack of immunohistochemical staining sometimes renders disease grading inadequate.
PATTERN AND DISTRIBUTION OF PERIPHERAL ARTERIAL DISEASE IN DIABETIC PATIENTS WITH CRITICAL LIMB ISCHEMIA (RUTHERFORD CLINICAL CATEGORY 4-6) M Motsumi, N G Naidoo
Groote Schuur Hospital, University of Cape Town
Background: The literature tends to support the notion that diabetic patients typically suffer from tibio-peroneal artery occlusive disease with relative sparing of the foot arteries.
Aim: To study the pattern and distribution of Peripheral arterial disease and the arterial foot arch status (complete, incomplete and absent) in diabetic patients with critical limb Ischemia and then stratifying the results according to: age group (<40 years, 40-54 years and > 55 years), risk factor profile (diabetes, hypertension, dyslipidemia, smoking, ex-smoker) and gender.
Methods: This is a one year prospective study -(January 2014 to December 2014) carried out on consecutive patients seen at Groote Schuur Hospital, Vascular Department. The inclusion criteria is: diabetic patients >18 years of age with critical limb ischemia who had pre- and post-intervention vascular imaging. All 12 main arteries from infra-renal aorta to crural arteries had their patency levels graded from category 1 to category 5 (widely patent to occluded). The calculated minimum sample size of 63 limbs [756 patency levels (63x12)] was needed to achieve a power of 86% to detect a difference of 0.1900 (19%) with a target significance level of 0.05 (using PASS 11 software). The equality of distribution of categories was analysed using the One sample Chi-square test (SPSS 22) with our Null hypothesis (N0) assuming that categories occur with equal proportions.
Results: Seventy-one patients were analyzed: 38/71 females and 33/71 males. Eight hundred and twenty (820) patency categories were recorded [8 patients did not have their aorto-iliac segment imaged (8x4=32)]. When all diabetics were analyzed as one group, there were relatively more category 5 and category 4 (occlusions and high grade- stenosis) patency levels in the tibioperoneal segment with statistically significant disproportion (p<0.001 for both categories). Females had relatively less severe grades of patency levels. Group 3(DM, HPT, dyslipidemia, smoker) have a different distribution pattern, with more occlusions in the femoropopliteal segment (p<0.001). Group 1 (DM, HPT, Dyslipidemia) and group 2(DM, HPT, dyslipidemia, exsmoker) had more occlusions in the tibioperoneal segment (p<0.001). Only 10/71 patients had an absent foot arch; 28/71 patients had an incomplete foot arch; 31/71 had a complete foot arch and 2/71 had a poorly imaged foot arch. Female diabetic patients had predominantly complete foot arches (22/37;59%) (p=0.004). Male patients had predominantly incomplete foot arches (17/32;53% (p =0.048)). Group 2 patients had predominantly complete foot arches 9/13. For group 1 and group 3 the proportions in the arterial arch status categories were almost the same with slight predominance of incomplete foot arch, followed by complete arch (p<0.05). The predominant age group (>55) also have a predominantly complete arterial foot arch (p=0.028).
Conclusion: Diabetic patients in general have severe tibio-peroneal disease. Gender and patients older than 40 years have the same disproportionate distribution of severe lesions to distal segments. However female patients have less severe grades of disease. Group 3 patients have a disproportionate distribution of occlusions (p<0.001) with more occlusions in the femoropopliteal segment. Group 1 and group 2 had a disproportionate distribution of occlusions to distal segments (p<0.001). Female diabetics tends to have a complete arterial foot arch (p=0.004) as opposed to male patients who have predominantly incomplete foot arches (p=0.048). Group 2 have predominantly complete arterial foot arch while group 1 and group 3 predominantly have an incomplete arterial foot arch. The predominant age group (>55) also have a predominantly complete arterial foot arch (p=0.028).
PROMOTING COAGULATION-FACILITATED METASTASIS - A PRELIMINARY ASSESSMENT OF THROMBIN-MEDIATED & MCF-7-MEDIATED PLATELET ACTIVATION STATUS AND ULTRA-STRUCTURAL ALTERATIONS
T N Augustine, L L Kaberry, W J van der Spuy
School of Anatomical Sciences, Faculty of Health Sciences, University of the Witwatersrand
In cancer patients thromboembolic complications are identified as the second most common cause of morbidity and mortality, with thromboembolism risk linked to the stage of cancer presentation. Thrombin mediates platelet activation and aggregation, and the development of fibrin networks in vivo; both of which are implicated in facilitating coagulation-mediated metastasis. We thus investigated firstly, the effects of a range of exogenous thrombin concentrations (0U/ml - 20U/ml) on platelet activation status and ultrastructure in whole blood. Secondly, we assessed platelet activation status and ultrastructure following exposure of whole blood to the MCF-7 human breast cancer cell line. Flow cytometry was used to identify platelets (CD41) and assess activation status (CD62p). Scanning electron microscopy was used to assess platelet ultrastructural changes and the formation of fibrin networks.
We identified that subthreshold concentrations of thrombin did not affect baseline CD62p expression; however, exposure to 0.05U/ml and 0.1U/ml thrombin showed a substantial increase in CD62p expression. This was substantiated by ultrastructural assessment showing an increase in platelet activation and aggregation, and dense fibrin network formation. Subsequent to exposure to MCF-7 cells, platelets revealed an increased CD62p expression equivalent to that of 0.05U/ml thrombin concentration as well as the formation of dense, non-porous fibrin networks.
The results presented have implications for the heterotypic aggregation of cancer cells and platelets in metastasis, as well as the increased probability of venous thrombus formation seen in breast cancer patients.
A MULTICENTER EVALUATION OF EMERGENCY ABDOMINAL SURGERY WITHIN SOUTH AFRICA: RESULTS FROM THE GLOBALSURG-1 (SA) STUDY
R Spence1, E Panieri1, S Rayne2 on behalf of the Globalsurg South Africa collaboration:
N Ngayu, R Moore, V Jennings (Chris Hani Baragwanath Academic Hospital); H Kretzmann, D Nel, K Connor (Frere Hospital); C Sampson, R Spence, E Panieri (Groote Schuur Hospital); S Rayne, N Sishuba (Helen Joseph Hospital); M Tun, J-O Carreira, A M Mphatsoe (Leratong Hospital); M Wagener, E Teasdale (Ngwelezana Hospital)
1 Department of Surgery, University of Cape Town, South Africa
2 Department of Surgery University of Witwatersrand, South Africa
Introduction: GlobalSurg-1 was a multicenter international evaluation of emergency abdominal surgery to identify common, modifiable best practice processes that took place during July-November 2014. Any hospital in the world performing acute care surgery was eligible to enter. The national data from South Africa that contributed to GlobalSurg is presented here.
Aims: The primary aim is to describe the risk-adjusted surgical outcomes following emergency abdominal surgery amongst centers within South Africa that contributed to GlobalSurg.
Materials and Methods: A multi-center, prospective cohort study was carried out within a defined two-week period during July-November 2014. 44 Perioperative data variables were audited for every emergency abdominal surgery (excluding Caesarian section) that took place and entered into the REDCap (Research Entered Data Capture) system. Multivariable binary logistic regression was used to test the influence of the demographic and process of care variables as well as location on in-hospital mortality. Ethics for this study was approved by local hospital management as well as from the affiliated universities.
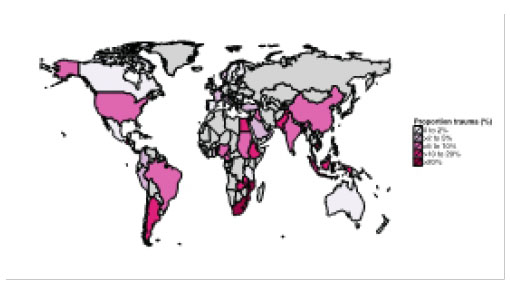
Results: 172 Emergency abdominal surgeries were included in 6 hospitals. Mean age was 35 years (range 9-82) and 68% were male. Most common diagnoses were penetrating trauma (27%), appendicitis (23%) and blunt trauma (7%). The outcome measures included POMR-24 of 3.4%, inhospital POMR of 8.9%, mean LOS 8.5 days (range 0-31), reoperation rate of 13.3% and in-hospital morbidity of 13.4%. Independent risk factors for in-hospital mortality (p<0.05) included age, ASA score, current smoking status, time from admission to knife-to-skin >24 hrs and location of surgery. Worldwide, South Africa had the highest global incidence of trauma (Figure 1).
Conclusions: Emerging web-based technology increases the capacity for local audits and surgical outcomes research within South Africa.
PILOT SURVEY AMONGST HEALTH CARE WORKERS ON SKIN DONATION
N L Allorto, K Okyere-Dede, D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan, University of KwaZulu Natal
Introduction: A cadaver skin bank is needed in South Africa as one of the strategies to improve survival of major burn injuries. Organ donation is on the decrease and tissue donation is largely unknown. There are cultural and religious challenges to organ and tissue donation in South Africa. As part of research into the development of a campaign to raise awareness about skin donation we surveyed a small number of health care workers in order to gauge willingness to become a skin donor.
Methods: Five hundred health care workers were approached by an African Zulu speaker and 150 African health care workers agreed to be surveyed (this included nurses, pharmacy and therapy assistants, porters and cleaners) in Edendale Hospital, which is a regional hospital that includes a burn service. It was explained that skin donation occurs after death and a thin layer of skin is taken from the body, cleaned, tested and stored. This donated skin could save the life of a major burns patient. After this explanation they were asked if they would donate their skin after death and if no, what was the reason. Age and gender was recorded as well whether they had worked in a burn unit before. The answers recorded were anonymous.
Results: One hundred and fifty African health care workers took the survey of which 119 were female (79%) and 65 (43%) had worked in a burns ward or unit before. The majority of respondents, 53, were 30 to 39 years old (35%), with 26 (24%) between 20 and 29 years, 27 (18%) between 40 and 49 years and only 16 (11%) over 50 years and in 18 there was no age recorded.
Forty-eight (32%) surveyed yes to donate their skin after death. Twenty-nine (24%) women surveyed yes to skin donation, while 19 (61%) men surveyed yes. In the group that had worked in burns before only 18 (28%) surveyed yes and 47 no to tissue donation compared to the group that had never worked in burns before where 30 (35%) surveyed yes and 55 no. Reasons for not donating skin were cultural in 50, religious in 18, health in 4, fear in 6, personal in 21 and family in 3.
Conclusion: The majority of respondents were woman. Men appear to be more willing to donate their skin than woman. Agreeing to skin donation was surprisingly higher in the group that had never worked in burns previously. Religious and cultural barriers remain the challenge in improving tissue donation in South Africa. We need a broader sample that includes all races and cultures in South Africa as well as a more detailed questionnaire in order to better represent and understand the issues surrounding skin donation. However in this sample one third would donate which is promising and there is hope that a skin donation drive will have success.
ARE WE DOING TOO MANY COMPRESSION ULTRASOUNDS FOR SUSPECTED ACUTE LOWER LIMB DEEP VENOUS THROMBOSIS IN TERTIARY INPATIENTS?
C R de Jager, N E Pearce
Department of Surgery, University of the Free State
Introduction: It is difficult to strike a balance between unnecessary investigations and missing the diagnosis, in patients suspected of having a DVT. The impact of scoring systems on referral patterns, at our institution, is unknown.
Objectives: We aim to establish whether changing the referral form for compression ultrasound (CUS), to the Vascular Laboratory, for in-patients at Universitas Academic Hospital, to include the Wells score and D-dimer, would effect a change in referral habits.
Method: We compared a prospective cohort (2014), to a retrospective control group (2009-2013). The new form was introduced in 2014 and data collected prospectively. A retrospective review of patient records, for patients referred for CUS, was done for the period 2009-2013. The total number of admissions to Universitas Hospital, for the respective periods, was the population sampled in each instance. All in-patients referred for CUS for the study period (2009-2014) were eligible. Patients were excluded if the admission diagnosis was DVT, if the suspected DVT was in the upper limb or if they had chronic venous insufficiency. Repeat referrals were also excluded. Ethical approval was obtained from the Ethics Committee of the University of the Free State (ECUFS 171/2013). Statistical analysis was conducted using Fisher's exact test or Chi-Square, as appropriate. A p value of < 0.05 was considered significant.
Results: From 2009 to 2013 0.84% of admissions were sent for CUS as compared to 0.63% in 2014. (p=0.0093). We found no statistical difference in the numbers of DVTs diagnosed, as a proportion of the number of hospital admissions, for the 2 periods (p=0.93). (See Table.)
Conclusion: The inclusion of the Wells score and D-dimer to the new request form, effected a decrease in the amount of referrals, without a change in number of DVTs found, in relation to number of admissions. We concluded that implementation of the new form, altered referral patterns for CUS.
Oral Presentations
EMERGENCY LAPAROTOMIES IN THE DEVELOPING WORLD
V Soldati, M Scriba , J Bruce, D Clarke, G Laing G
University of Kwa-Zulu Natal
Emergency laparotomy is a common procedure performed by surgeons all over the world. The aim of this paper is to review the spectrum of aetiology in patients requiring emergency laparotomy at Grey's Hospital which is a tertiary institution in Pietermaritzburg, South Africa. These findings will then be compared with findings from other developing countries such as India and contrasted with the Western World. This is a retrospective study with data collected using the Hybrid Electronic Medical Registry (HEMR) at Grey's Hospital over a 2 year period from December 2012 to December 2014. The inclusion criteria was all patients presenting to Grey's Hospital accident and emergency unit over the above mentioned time period with features of perforation peritonitis, requiring an emergency laparotomy. Exclusion criteria were: all paediatric patients; trauma aetiology; Non-therapeutic laparotomy; Gynaecological findings. This left us with a sample size of 891 patients. The objectives set include establishing the spectrum of aetiology in patients requiring emergency laparotomy in South Africa. The end point would be to therefore prove that the spectrum of aetiology is similar across developing countries and different to that of the developed world. Data collected from HEMR was analysed through Microsoft Excel and results depicted through tables and graphs on a spreadsheet. HEMR has full ethics approval to maintain a surgical database and to use data for clinical audit: BCA 221/13. The results show that the commonest finding during emergency laparotomy in our setting is: Perforated Appendix (56%); followed by Adhesive Bowel Obstruction (13%); Peptic Ulcer Disease (12%); Tuberculosis of the Abdomen (9%); Large Bowel Obstruction (6%). Overall mortality was 10%. We can therefore conclude that results are comparable to findings in India where the causes for perforation peritonitis include: Peptic Ulcer Disease; Perforated Appendix; Typhiod and Tubercular perorations in that order. We can also contrast this to the U.K where perforation of the large bowel was the most common indication of emergency laparotomy.
EVALUATION OF LAPAROSCOPIC CHOLE-CYSTECTOMIES IN A TERTIARY TEACHING HOSPITAL IN SOUTH AFRICA
V M Nair, M Govender, G Laing, C Aldous, L Ferndale L
Background and Aim: Symptomatic cholelithiasis is prevalent in the public health sector in South Africa. Laparoscopic cholecystectomy is the procedure of choice in management. Greys Hospital is a tertiary referral centre for all complicated gallbladder pathology in the Western KwaZulu Natal drainage area. The objective of this study was to evaluate the laparoscopic cholecystectomies performed here.
Materials and Methods: This was a retrospective study of all patients who underwent laparoscopic cholecystectomy (LC) between December 2012 and December 2014. The Department of Surgery's electronic database and patient's case files were used. Patient demographics and case details were reviewed. Surgical details and complications were also assessed. Ethics approval is BCA221/13 from BREC.
Results: A total of 281 patients underwent LC. The average age was 46. The majority of patients were female (86.8%). Twenty one cases were converted to open procedure (7.47%). The average age of those requiring conversion was 56 (p<0.05), Conversion rate was 5.7% in females and 18.9% in males. The average time taken to perform a LC was 1 hour 14 minutes. Twenty five laparoscopic partial cholecystectomies were performed with an average duration of 1 hour 59 minutes. If converted to an open operation, the average operating time was 2 hour 16 minutes (p=0.13) Complications included two iatrogenic bile duct injuries (0.7%), one bile leak (0.35%), one bowel injury (0.35%) and one postoperative haemorrhage (0.35%).
Conclusion: The complexity of the gallbladder pathology referred to Greys hospital makes laparoscopic cholecystectomy challenging. This combined with prolonged waiting periods may contribute to the relatively high complication rate seen in this audit.
LAPAROSCOPIC VENTRAL HERNIA REPAIR: THE TYGERBERG ACADEMIC HOSPITAL EXPERIENCE
S Visagie, A Lambrechts
Division of Surgery, University of Stellenbosch
Background: Incisional herniation remains the most common complication after laparotomy. Together with umbilical, para-umbilical and epigastric hernias, ventral hernias represent a major burden in terms of theatre time, hospital beds, cost and patient morbidity. Despite the introduction of various new techniques, major complication and recurrence rates after repair are high. Laparoscopic ventral hernia repair by mesh prosthesis was introduced at Tygerberg Academic Hospital in an effort to improve the outcome of these repairs.
Aim: To investigate the complication rates of laparoscopic ventral hernia repair performed at Tygerberg Academic Hospital, as well as factors responsible for their occurrence.
Methods: A retrospective cohort study was conducted on laparoscopic ventral hernia repairs performed at Tygerberg Academic Hospital between August 2009 and April 2014. During this period all cases of ventral hernia were considered for laparoscopic repair. Cases were identified from complete theatre records for the study period. Adult (>18 years) patients who underwent elective laparoscopic ventral hernia repair with mesh were included. Exclusion criteria were inguinal hernias and emergency procedures.
Results: The study included one hundred consecutive cases of laparoscopic ventral hernia repair with mesh. Ninety seven cases were completed laparoscopically, with three cases converted to open repair. There was no peri-operative mortality. The average age and weight of patients were 52.8 years and 92 kg respectively. Incisional hernias represented 67% of the repairs performed. Three iatrogenic enterotomies occurred, of which two were followed by conversion to open repair. Mean operative time was 128 min and patients were discharged after a mean of 2.7 days post-operatively.
The recurrence rate after a median follow up of 22 months was 15.5%. The main contributing factors to recurrence were hernia type, size of the defect and surgical experience. Recurrence only occurred in the incisional hernia group and none in the primary ventral hernia group (p=0.01). Average mesh size used in the incisional hernia group was 390cm2 versus 240cm2 in the rest of the study group (p=0.041). Repairs by consultant surgeons recurred at a rate of 5,7%, while 23,8% of cases repaired by registrars recurred (p=0.042). Post-operative seromas complicated 29.4% of cases and wound infection occurred in 5.1%. One infected mesh required removal.
Conclusion: Our data is acceptable with respect to peri-operative complication rates while operative time and recurrence rates are higher when compared to international literature.
RETROSPECTIVE AUDIT OF LAPAROSCOPIC INGUINAL HERNIA REPAIRS DONE AT THE DR GEORGE MUKHARI ACADEMIC HOSPITAL
B Moodie, M Z Koto
Department of Surgery, Sefako Makgatho Health Sciences University, Dr George Mukhari Academic Hospital
Background: Laparoscopic Inguinal hernia repair (LIHR) is a described alternative to open repair with comparable outcomes. LIHR is rarely considered in the setting of the South African Public sector due to financial constraints and high patient load.
Aim: To assess the feasibility of doing LIHR at a Tertiary Teaching hospital
Materials and Methods: Retrospective Observational study. All cases of inguinal hernias that were repaired Laparoscopically during November 2011- April 2015. This includes emergency and elective repairs done via Total Extraperitoneal hernia repair (TEP), Transabdominal reperitoneal repair (TAPP) and conversion of TEP to TAPP or LIHR to open repair. Primary open repair cases were excluded.
Results: Of the 152 cases, 96.7% (147) were TEP repairs and 1.3% (2) TAPP repairs. Two cases were converted from TEP to TAPP 1.3% (2) and two TEP repairs converted to open repair 1.3% (2). Three incarcerated and two strangulated hernias were repaired via the TEP repair method. The male: female ratio was 14:1 with 93.4% (142) males. Right sided pathology predominated with 64.9% (96) of repairs on the right side and 19.1% (26) left side. Bilateral repairs were done in the remaining 15.5% (23). LIHR done in 5.2% (8) being <20 years old, 29.6% (45) between 21-40 years, 39.5% (60) between 41-60 years and 25.7% (39) above 61years.
Conclusion: Our series demonstrates a male, right sided predominance mainly presenting between 41-60 years of age. The great majority were TEP repairs with a low conversion to open rate. Our series demonstrates that the LIHR technique may be utilised effectively in a Public General Surgery training centre.
DIAGNOSTIC AND THERAPEUTIC LAPAROSCOPY FOR LEFT LOWER THORACIC STAB WOUNDS
G Uanivi, B L Warren
Division of Surgery, University of Stellenbosch
Background: Penetrating diaphragmatic injuries not detected in the acute setting may remain clinically silent, only to present later with complications associated with diaphragmatic herniation. Early diagnostic laparoscopy is an attractive option for the diagnosis and treatment of left-sided diaphragmatic injuries following stab wounds to the left lower chest.
Aim: To establish the incidence of diaphragmatic injury following left-sided lower thoracic stab wounds and the effectiveness of laparoscopy in diagnosing and treating diaphragmatic injuries.
Methodology: A retrospective and prospective collection of data of all patients admitted to the Tygerberg Academic Hospital Trauma Surgery Unit for diagnostic laparoscopy after left lower chest stab wounds (below a line joining the left nipple anteriorly and the inferior tip of the left scapula posteriorly). Diaphragm injuries due to gunshot wounds and blunt trauma were excluded. The period under review was from June 2010 to May 2014. Diagnostic laparoscopy findings and simultaneous repair of diaphragmatic injury either during laparoscopy or at open surgery were recorded.
Results: The inclusion and exclusion criteria were met by 114 patients of whom 95% (n=108) were male. Diagnostic laparoscopy was performed on all 114 patients. The mean age of included patients was 27 years (range 10-63). Twenty eight patients (25%) sustained a diaphragmatic injury. The repair was completed laparoscopically in 25 patients (89,3%) and via a mini-laparotomy in 2 patients (7,1%). One patient (3.6%) underwent repair through the stab wound. No postoperative complications were recorded.
Conclusion: The incidence of diaphragmatic injury associated with stab wounds of the left lower chest is high. Laparoscopy is an effective diagnostic modality and concurrent laparoscopic repair is feasible in the majority of cases.
THE ROLE OF LAPAROSCOPY IN MANAGEMENT OF STABLE PATIENTS WITH PENETRATING ABDOMINAL TRAUMA AND ORGAN EVISCERATION
O Y Matsevych, S R Motilall, N Kumar, M Z Koto
Department of Surgery, Sefako Makgatho Health Science University, Faculty of Medicine,
Dr George Mukhari Academic Hospital, Pretoria, South Africa
Background: The high rate of nontherapeutic laparotomies after penetrating trauma to the abdomen resulted in the strategy of selective nonoperative management. It is clear that certain stable patients without peritonitis may be managed without operation, even if they present with organ evisceration. However, the operative management of the patients who failed nonoperative management will be delayed and may result in increased morbidity. The rate of nontherapeutic laparotomy in patients with organ evisceration remains high. The aim of the study is to determine the significance of organ evisceration in stable patients with penetrating abdominal trauma (PAT). The accuracy of laparoscopy to identify intraabdominal injuries were also assessed.
Material and methods: The patients presenting with PAT between January 2012 and December 2014 were retrospectively analyzed. Only haemodynamically stable or responsive to initial resuscitation patients who underwent laparoscopy for organ evisceration were included into the study. According to our policy all unstable patients are selected for open exploration and they were excluded from the study. The cases with missing or inconclusive records were excluded. The intraoperative findings were analysed.
Results: A total of 189 stable patients were treated with laparoscopy for PAT. Thirty nine (29.6%) patients were presenting with organ evisceration. Fifteen (38%) patients had bowel evisceration and 24 (62%) had evisceration of the omentum. Eleven (73%) patients with bowel evisceration and 14 (58%) patients with omental evisceration had significant intraabdominal injuries requiring therapeutic laparoscopy. In total 25 (64%) patients required therapeutic laparoscopy and 14 (36%) patients underwent diagnostic laparoscopy. We did not have missed injuries. There were neither conversions nor significant complications in postoperative period. All patients received benefit of minimally invasive surgery and 14 patients avoided nontherapeutic laparotomy.
Conclusion: Organ evisceration in stable patients with PAT associated with the high rate of significant intraabdominal injuries and mandate the abdominal exploration. Laparoscopic management is the method of choice. It has high accuracy to identify intraabdominal injuries, provides all benefits of minimal invasive surgery and protects patients from nontherapeutic laparotomy.

LAPAROSCOPIC COMMON BILE DUCT EXPLORATION: USE OF A RIGID URETEROSCOPE
I I Sardiwalla, M Govender, M Z Koto
Department of Surgery, Sefako Makgatho Health Science University, Faculty of Medicine
Dr George Mukhari Academic Hospital, Pretoria, South Africa
Introduction: Laparoscopic common bile duct exploration (LCBDE) offers an additional approach to complicated gallstone disease. However it requires advanced laparoscopic skills and expensive equipment. Flexible choledochoscopes are marketed for this purpose but are fragile and easily damaged in a multi-user environment. We use the rigid ureteroscope effectively to confirm clearance of the bile duct.
Aim: To describe the technique and results of laparoscopic common bile duct exploration using a rigid ureteroscope at Dr George Mukhari Academic Hospital.
Methods: All cases performed by the HPB Unit were reviewed retrospectively from January 2014 to December 2014 at the above institute. The procedure was performed using two 12mm ports and two 5mm ports placed in a standard manner for laparoscopic cholecystectomy. Care was taken to ensure the upper midline 12mm port (UMP) was placed to the right of the falciform ligament. The dissection of Calot's triangle and ligation of the cystic duct and cystic artery was performed first. The duct and artery were transected. All cases had transductal exploration. Stones were retrieved with either Fogarty vascular or ERCP biliary extraction balloons. A rigid ureteroscope (Karl Storz®) was used to confirm duct clearance. Once the common bile duct was opened the 10mm telescope was changed to the ureteroscope. The proximal ducts were explored via the umbilical port and the distal duct via the UMP. The choledochotomy was closed with 4/0 polydioxanone suture and the cholecystectomy completed.
Results: 10 cases were performed. All were female with an age range from 27 to 77. Eight patients underwent preoperative ERCP which failed to achieve duct clearance. Two cases were converted due to an impacted stone in one and a cirrhotic liver in another. One case did not have complete visualization of the ducts due to equipment failure. The latter had a postoperative ERCP and complicated with pneumonia. One patient had bleeding from the umbilical port site requiring resuturing and one patient developed intra-abdominal collections requiring laparotomy. The rigid ureteroscope is more robust than the flexible scope used previously by the authors. Stones can also be pushed into the duodenum with the scope. There is no need for a second camera head to accommodate the choledochoscope. The scope cannot be maneuvered into the distal duct in cirrhotic patients even in open laparotomy.
Conclusion: The rigid ureteroscope provides adequate visualisation of the biliary tree during LCBDE and may be superior to the flexible scope in most cases. In a resource constrained environment the same instrument can be used by two departments (urology and surgery). A larger study must be undertaken to compare the rigid ureteroscope to the flexible choledochoscope.
TRANSANAL ENDOSCOPIC OPERATION (TEO) - LOCAL EXPERIENCE IN A SOUTH AFRICAN SETTING
P Karjiker, R Baigrie
Department of Surgery, University of Cape Town
Background: The best surgical approach for early stage rectal cancer is uncertain. Radical surgery offers the best chance of cure, but at the cost of significant morbidity, mortality and expense. Local tumour excision avoids the complications of radical surgery. Transanal endoscopic operation (TEO) and Transanal endoscopic microsurgery (TEM) have been widely adopted as the treatments of choice for large rectal adenomas and selected rectal cancers but has been under-employed in South Africa with the exception of two centres in Cape Town.
Aim: The primary outcome of this review is to assess the local recurrence after TEO excision of benign or malignant disease and the secondary outcome, to ascertain the incidence of complications following a TEO.
Methods: A retrospective audit was undertaken of all patients undergoing resection of benign and malignant rectal tumours by TEO at a private (Kingsbury Hospital) and public health institution (Groote Schuur Hospital). Electronic records, including operation notes, histology and radiology were reviewed. Data is currently being collected. Stata was used to perform the statistical analysis. Ethical approval for the study has been granted by the UCT Departmental Research Committee and the Health Sciences Human Research Ethics Committee.
Results: 71 patients were identified. The mean height of the tumours from the anal verge was 6.5cm and the average size was 25cm2. 66 patients had a histologically clear margin. Fourteen patients had adenocarcinoma (11 with T1 and 3 with T2). 3 patients with benign disease had recurrences which were subsequently treated. 9 patients had complications:
4 with asymptomatic anal stricture, 1 with bleeding, 1 with urinary retention, 2 perforations and 1 death from a confirmed myocardial infarction.
Conclusion: TEO can be performed safely in this environment. All cancers were of an acceptable T stage and were completely resected. The recommendation is for a wider introduction of TEO in South Africa with the provision of adequate training.
INCIDENCE OF COMPLICATIONS POST COLOSTOMY AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
S Phaleng, F O Ghoor, N M Latakgomo, N Singh
Department of Surgery, Sefako Makgatho Health Science University, Faculty of Medicine
Dr George Mukhari Academic Hospital, Pretoria, South Africa
Background: Colostomies are frequently required in colorectal conditions either as temporary or permanent stomas. The main indications for faecal diversion are distal bowel obstruction, colorectal injuries, rectovaginal fistulae, perineal sepsis and to divert fecal load from a low rectal anastomosis. Complications from these may arise early or late. Early complications include wound sepsis, ischemia and skin excoriation. Late complications include stomal prolapse, parastomal hernia, stenosis, retraction and persistent faecal drainage (overspill).
Aims & Objectives: To determine the indications and frequency of complications associated with the construction of colostomies at Dr George Mukhari hospital.
Methods: This is a retrospective study over a 12 months period from March 2014 to February 2015. All patients who had a colostomy done were included. Complications in the form of wound sepsis, ischemia, prolapse,, parastomal hernia, stenosis, retraction or persistent faecal drainage (overspill) were noted.
Results:
38 colostomies were done in 38 patients. Types of colostomy
• Sigmoid loop colostomy 34/38 (89%)
• End Colostomy &
• Hartmann procedure 4/38 (11%)
• Indications for colostomy
• Anorectal carcinoma 18/38 (47%)
• Rectovaginal fistula 7/38 (18%)
• Trauma 6/38 (15.8%)
• Sigmoid Volvulus 3/38 (7.8%)
• Anal sepsis/warts 4/38 (10.5%)
• Complications
• Complications occurred in 6/38 patients (15.8%)
• Prolapse 4/38 (10.5%)
• Wound sepsis 1/38 (2.6%)
• Leakage (Persistent
• Faecal drainage) 1/38 (2.6%)
Conclusion: The most common indication for colostomy in our setting was for anorectal malignancy (47%). The overall complications rate was low (15.8%) with the most common complication being prolapse (10.5%). The rate of septic complication was very small (2.6%). No parastomal hernia was seen during this period. The majority of colostomies were loop colostomies (34/38) with all the complications occurring in these loop colostomies (although the number of end colostomies were too small to make this a valid comparison).
COLORECTAL CANCER: IS THERE AN ASSOCIATION BETWEEN HIV INFECTION AND THE CLINICOPATHOLOGICAL PICTURE? S K Pillay, Z Moolla, T E Madiba
Colorectal Unit, Department of Surgery, University of KwaZulu-Natal, Durban
Introduction: A link between colorectal cancer (CRC) and HIV has not been extensively studied.
Purpose: This study aims to establish the existence of such a link.
Methods:
• Study setting: Colorectal unit at a tertiary institution
• Study design: This is an analysis of prospectively collected data from a colorectal cancer database archived in the Department of Surgery, University of KwaZulu-Natal, over a 10 year period from 2005 to 2014. Demographic details, HIV status, anatomical site, stage and treatment were documented. Data were then analysed using Excel®.
• Study endpoints: Disease presentation, stage and anatomical site.
• UKZN Ethical Approval: E198/04
Results: A total of 1308 patients were analysed. Voluntary counselling and testing was performed on 241 patients (139 males), of whom 201 tested negative and 52 tested positive. Median age was 44 and 56 years among HIV positive and negative patients respectively. Proximal: distal colon ratio was 1.3:1 among HIV positive patients and 1:1.2 among HIV negative patients. Rectal disease occurred with equal frequency in both groups. Twenty HIV positive patients (38%) presented with Stage IV disease compared to 51 HIV negative patients (25%). Resection rate was 48% and 65% for HIV positive and HIV negative patients respectively. Follow-up was shorter for HIV positive patients (6.3 vs 9.2 months). Forty seven patients have been confirmed dead, 13 among HIV positive (25%) and 34 among HIV negative (17%).
Conclusion: HIV positive patients tended to present at a younger age with more proximal disease which presented at an advanced stage. Resection rate was lower among HIV positive patients.
ACHIEVING SURGICAL COMPETENCE FOR DISTRICT LEVEL HOSPITALS IN BOTSWANA
M Kwati1 & M S Walsh1,2
1 Princess Marina Hospital
2 University of Botswana
Introduction: There is a deficit in surgical care in low to middle income countries, where a lack of surgical providers is a barrier to surgical care1. Death due to diseases requiring surgery is an increasing burden2. Surgical procedures delivered in low-resource settings are cost effective1. Worldwide basic surgical trainees (BST) struggle to achieve competence in surgical procedures. In Africa this may be partly due to the low numbers of trained surgeons to provide supervision. To improve access to surgery The Botswana Ministry of Health (MoH) has proposed basic surgical competencies for Medical Officers (MO).
Aims: The aims were to assess if the MoH competencies were attainable with 1 year of training, and compare this to the training of BST in the developed world. Following this period of training we assessed if the MO would be capable of operating independently in a District Hospital.
Methods: A retrospective logbook review of procedures performed by a MO supervised in the department of surgery in a referral hospital in Botswana was performed. This was compared to the competencies drawn up by the MoH and data available from Ireland3. Subsequently the Medical Officer would then operate unsupervised to assess his ability to safely carry out similar surgical procedures.
Results: The MO was involved in over 90 major and intermediate operations, 29 as assistant, 30 performed assisted by consultant, 11 with consultant present not scrubbed and 20 with consultant available but not in theatre. 69 minor operations and 29 bedside procedures were performed. The table below gives samples of data from the 1 year in Botswana and 2 year means for Irish BSTs. The final column gives data for the independent operating period. During this time telephone advice was sought during 5 procedures and in 1 a consultant had to attend. (See table.)
Conclusions: The basic surgical competencies drawn up by the Botswana MoH were achieved in 12 months. Compared to similar level trainees in Ireland the caseload with supervision would appear to enable the trainee to gain considerable experience. The outcome of the unsupervised period of training would support the deployment of Medical Officers to District Hospitals to perform appropriate levels of surgery following a short focused training period.
REFERENCES
1. Dure J. A, Grimes C. E, Gillies R, et al. Global Surgery: defining an emerging global health field. www.thelancet.com Vol 384 December 20/27, 2014
2. Hoyler M, Finlayson S, Meara J, Hagander L. Shortage of surgeons, obstetricians and anaesthesiologist in low and middle income countries. Proceedings of the 141st Annual Meeting and Expo of the American Public Health Association, November 2-6, 2013, Boston, MA, USA (abstr).
3. Lonergan et al. BMC Medical Education 2011, 11:70
TEACHING LIFE SAVING SKILLS USING TASK TRAINERS
H J C du Plessis, G Owen Muller
Lecturer, Department of Surgery, Faculty of Health Sciences, University of Pretoria; National Chairman, ATLS South Africa; Course Coordinator, ATLS Northern Region
Introduction: The Advanced Trauma Life Support© (ATLS) course was developed in Nebraska, USA, in the late 1970's. It was adopted by the American College of Surgeons (ACS) as the basic resuscitation course for trauma patients, and has since spread internationally to more than 60 countries, including South Africa. An important component of the course is the practical lifesaving skills taught in the animal laboratory or mortuary. The increasing cost of animals and the unavailability of suitable cadavers prompted the development of suitable alternatives to teach these skills. The TraumaMan trainer was approved by the ACS, but it is prohibitively expensive for countries outside the USA. A South African company developed task trainers to use for teaching these skills, and these models were tested against TraumaMan.
Methods: Students on 2 ATLS provider courses were taught the surgical skills by surgeon instructors on both TraumaMan and the South African trainers. They were then asked to participate in the evaluation of the utility of the trainers by completing a questionnaire comparing the two models. Each skill was rated on a 5 point Likert scale (from 1 = very poor, to 5 = excellent). A further 3 questions addressed the ethical concerns (using trainers to replace animal models), cost implications (TraumaMan is expensive) and all factors.
Results: On 2 ATLS course 36 students and 9 instructors were asked to participate, but only 24 students and 6 instructors returned the questionnaires. The response rate was 66% in both groups. Not all questions were answered on the returned forms, and because of the small number of instructors that participated, the results were pooled.
For all the skills (except pericardiocenthesis) the participants preferred TraumaMan, but none of these were statistically significant. Both models were considered equally suitable for teaching and acquiring the skills.
Conclusion: Both TraumaMan and the South African trainers are equally suitable to teach the surgical skills on the ATLS course. When cost is a factor, the South African models are a good alternative to use as it is not significantly different to TraumaMan.
THE RESEARCH COMPONENT OF SPECIALISATION: HOW TO GET IT DONE
C Aldous1, D Clarke2
1 Academic Leader for Research, UKZN
2 Academic Director of Trauma PMTS
Background: Since 2011, the research component for specialisation has become compulsory, without consideration of time for the registrar to do the research, supervisors to mentor the work or the skills required to carry out or mentor research. The authors have designed a Gantt chart (Table 1) with beacons spread through the four year registrar program and support materials to facilitate the process of research project completion in time for registration as a specialist after the final exams and completion of time. This program was tested on a group of four registrars amongst the first for whom the research component was compulsory.
Methods: We report on the four students who began their specialization in 2011 under the mentorship of the authors. All were registered to specialize in surgery in the Pietermaritzburg Academic Hospital Complex which included Edendale Hospital (Regional) and Greys hospital (Tertiary).
Results: All the registrars published their research in time to register for specialization after completing their time at the end of 2014.
Conclusions: A time management plan and suitable support materials can result in successful completion of the research component of their specialization within their registrar time. It is important to note that unless a registrar has their own valid and feasible research question for study, a ready bank of data and research questions held by the department is important for this approach to succeed.
Sceales Antrobus Prize Session
BREAST CANCER RESPONSE TO NEO-ADJUVANT CHEMOTHERAPY AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
D H Mokone, M P Ratlabala, J H R Becker, S Montsho, D Mphane
Sefako Makgatho Health Sciences University, Dr George Mukhari Academic Hospital
Introduction: Neo-adjuvant chemotherapy (NAC), initially used to downstage inoperable locally advanced Stage III tumours, has since been extended to Stage IIb tumours, making them more suitable for breast conserving surgery. The majority of studies showed no benefit in disease free (DF) and over-all survival (OS) but suggested that response of a tumour is a measure of its chemo-sensitivity and thus pathological complete response correlates with outcome and should be one of the primary goals of neo-adjuvant therapy.
Aim: The aim of this study is to assess tumour response to neo-adjuvant chemotherapy in the population of patients seen at Dr George Mukhari Academic Hospital.
Methods: A retrospective study. Hospital records and histology results (biopsy and surgery) of patients who received NAC for Stage lib and Stage III breast cancer at the Breast Oncology Clinic between January 2012 and December 2014, were reviewed. Patients with Stage IV disease were excluded. 70 records/patients were identified.
70 Patients received NAC, 52 (74.3%) 4-6 cycles of CAF, 10 (14,3%) CMF, and 8 (11,4%) 4 cycles of CAF followed by 4 cycles of docetaxel.
6 patients (8,6%) had Stage IIb disease, 27(38.6%) Stage IIIa disease and 37 (52,9%) Stage IIIb disease.
Results: 6 patients (8,7%) achieved clinical complete response (cCR); 33 (47,8%) clinical partial response (cPR) and 30 (43,5%) had stable or progressive disease. One patients' clinical response was not recorded.
6 out of 52 patient (11,5%) achieved pathological complete response (pCR); 21 (40,4%) partial pathological response and 25 (48,1%) poor pathological response. In 18 patients, pathological response was not documented. Pathological completes response (pCR) was achieved in 2 out of 25 patients (8%) with luminal intrinsic/molecular subtype of breast cancer; 1 out of 15 patients (6,7%) with Her2 positive cancer and 2 out of 22 patients (9%) with triple negative cancer.
Overall clinical response of 58% was achieved and the overall pathological response was 51,9%.
Conclusion: The pCR of 11,5% achieved in this study is low compared to the average of 18% across different studies in literature. (16,6 - 21,5). One study had a pCR of 3%.
We did not identify any tumour characteristics (Ki67 index, molecular subtype, Grade), associated with tumour response.
ANAEMIA IN RECEPTOR NEGATIVE BREAST CANCER PATIENTS
A Maraj; A Mannell; T E Luvhengo
Department of Surgery, Charlotte Maxeke Johannesburg Academic Hospital and University of the Witwatersrand.
Introduction: Outcomes in patients with breast cancer are determined by the stage of the disease and molecular profile. Aggressive breast cancers are more likely to be receptor negative with lympho-vascular invasion. Anaemia is common in breast cancer patients and may be a result of malignancy, complication of treatment or pre-existing co-morbidities. The presence of anaemia can delay treatment such as surgical intervention or chemotherapy. Anaemia with a hemoglobin level below 10g/dL may blunt response to chemotherapy and radiotherapy due to tissue hypoxia.
Aim: To determine the prevalence and type of anaemia in patients with receptor negative breast cancer at Charlotte Maxeke Johannesburg Academic Hospital.
Materials and Methods: This was a retrospective review of patients from the Breast Unit at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) over 2002-2012. Data was obtained from the National Health Laboratory records of all breast cancer patients seen from January 2002 to December 2012. Data on demography, Human Immunodeficiency Virus (HIV) result, tumour stage, histological subtypes, hormone receptor status and pre-treatment hemoglobin as well as mean corpuscular volume were collected. This study was approved by the Postgraduate Committee of the University of the Witwatersrand and the Human Research Ethics Committee (HREC) of the University of the Witwatersrand (M130439).
Results: Records of 440 patients were examined. Majority were females (female:male = 109:1) with a mean age was 55 years. Most of the patients had stage II disease. Anaemia was present in 15% of patient population in this study (p Value = 0.0001). Of the patients with triple negative breast cancer (TNBC), 25% were anaemic.
Conclusion: Anaemia is common in TNBC irrespective of stage. Anaemia was clinically significant at presentation. A low pre-treatment haemoglobin impairs the patients' general condition and hence their response to adjuvant therapies. Patients should be investigated for the cause of anaemia and this should be corrected without recourse to blood transfusions.
FACTORS AFFECTING ADHERENCE TO ENDOCRINE THERAPY IN HORMONE-RECEPTOR POSITIVE BREAST CANCER
S Rayne1, K Schnippel2,3, P Mapunda1, C Firnhaber2,3, and C A Benn1
1 Helen Joseph Breast Care Clinic, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
2 Clinical HIV Research Unit, Faculty of Health Sciences, University of the Witwatersrand, South Africa
3 Right to Care, Johannesburg, South Africa
Background: Internationally non-adherence to endocrine therapy in breast cancer can vary from 15-60% and is associated with increased all-cause mortality. There are very few studies assessing adherence rates or describing side-effects in an African country.
Aim: This study is describing side-effects and other factors which impact on adherence in an urban South African breast cancer population.
Material and Methods: A descriptive, survey based study of a convenience sample of breast cancer survivors at a government breast care clinic in Johannesburg, South Africa was carried out. All patients had ER+ tumours. Questions around patient background, transport logistics, medication cost, SE and compliance were asked. Relative risk was analysed using Poisson regression with robust standard errors to produce incidence rate ratios for common outcomes. Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee.
Results: Of the 59 patients who completed the questionnaire, the age ranged from 27 to 80 years (mean 55.4; IQR 4366) and 22 were pre-menopausal, 36 post-menopausal and 1 unknown. 21 (35.6%) respondents had stopped or been tempted to stop (average length of treatment 30 months). Reasons to stop cited were bad side-effects (7), doctor's advice (6), inability to refill prescription (5) and recurrence (3).
45 patients (76.3%) experienced side effects. The most common side effects were flushing (30; 50.9%), weight gain (11; 18.6%), anxiety (10, 16.9%) and dry vagina (9, 15.3%). Most side effects were unrelated to a decision to stop however patients experiencing anxiety were 2.94 times more likely to report that Tamoxifen was not worth the side effects [95% CI: 0.83 to 10.47] and 1.96 times more likely to stop [95% CI: 1.01 to 3.81]. Most patient felt the benefits were worth the side-effects. Belief that Tamoxifen was effective in reducing recurrence halved the risk of stopping [RR: 0.50, 95% CI: 0.26 to 0.95].
Conclusion: At least one-third of patients eligible for endocrine therapy have considered cessation. Given the risk in recurrence and mortality conferred by this treatment modality on breast cancer it is imperative that better education and support is available to help women with side-effects and motivation to continue treatment.
IT'S NOT JUST CANCER: UNDERSTANDING THE VARIETY OF BREAST DISEASE SEEN IN A GOVERNMENT SPECIALIST BREAST CLINIC IN JOHANNESBURG
N Lince-Deroche1, C Hendrickson1, C Firnhaber2,3, C A Benn4,5, and S Rayne4,5
1 Health Economics and Epidemiology Research Office, Faculty of Health Sciences, University of the Witwatersrand, South Africa
2 Clinical HIV Research Unit, Faculty of Health Sciences, University of the Witwatersrand
3 Right to Care, Johannesburg
4 Helen Joseph Breast Care Clinic, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
Background: Most breast-related research focuses on cancer. However, it is critical to understand the total burden of breast diseases for service planning, especially in resource-constrained settings.
Aim: To characterise the presentation and management of breast disease at a large, public hospital offering comprehensive breast-related services in Johannesburg, South Africa
Material and Methods: A retrospective file review was performed of patients first presenting for breast care from between April 2011 and June 2012. Patients were eligible if they were >18 years and had a file available for review. All eligible men were included; women were selected using a systematic random sample. Demographics, clinical characteristics, management and final diagnoses were collected from first visit through 12 months of follow-up. Data analysis included simple proportions and means/medians with standards deviation. Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee.
Results: 4836 individuals attended the clinic during the study period; 330 (326 women) were included in the sample. The median (IQR) age was 42.8 (30.1-53.8) years. 72% were Black/African, and 9% had a recorded HIV-positive status.
Having a mass (51%) and/or pain (27%) were the most common presenting symptoms. 78% required radiological assessment. 25% and 4% required histological or lab-related testing/diagnostics respectively.
Breast cancer was diagnosed in 13.9% of patients. Other diagnoses included fibroadenoma (15.2%), breast pain (14.2%), infections (5.2%), duct ectasia (3.6%), and other benign conditions (13.3%). 1.8% underwent breast reduction. 50% of the men presented with gynecomastia. Most patients (23.6%) had no detected abnormalities.
Conclusion: Non-cancer related breast diagnoses conditions far outweighed cancer diagnoses for this population. As breast cancer awareness increases due to media and health campaigns, facilities offering breast care must be prepared to manage an extensive range of non-cancer related conditions as well as voluntary presentation for screening, in addition to their focus on cancer care.
FIVE-YEAR REVIEW OF BREAST-CONSERVING THERAPY (BCT) FOR BREAST CARCINOMA: SURGICAL MARGINS, RE-EXCISION AND LOCAL RECURRENCE IN A SINGLE TERTIARY CENTER
P Nashidengo, E Panieri, T Naiker, L Cairncross
University of Cape Town
Introduction: Breast cancer is the most common cancer in women in the developed world and the burden of breast cancer is on the increase in the developing world. Breast conserving therapy (BCT) has become and continues to be the mainstay treatment for patients with early breast cancer presenting to the Groote Schuur Hospital's surgical oncology unit, Cape Town South Africa. There has not been a formal audit to review the outcomes of BCT in the unit. The aim of this study is to audit BCT in the unit with a focus on excisional margins, re-excision and local recurrence rates.
Methods: A retrospective review of the patients that have undergone BCT for early breast cancer at Groote Schuur Hospital surgical oncology unit from the 1st of January 2006 until the 31st of December 2010 was performed. Approval for the study was obtained from the University of Cape Town's Faculty of Health Sciences Human Research Ethics Committee. Data points accrued included patient age, pathological tumor size and nodal status, histological tumor type, volume of specimen excised, margin status, management of involved or close margins i.e. repeated resection versus mastectomy, radiotherapy, recurrence and total duration of follow up.
Results: A total of 192 patients had BCT in the study period. The age mean was 53 years (range 25 to 84 years). An average of 400 cm3 volume of specimen was excised (range 4 to 10530 cm3). Infiltrating ductal carcinoma associated with ductal carcinoma-in-situ was the commonest histological sub type at 40.6%. 42.7% were T1 tumors, 49.0% T2 tumors and 2.6 %T3. The closest resection margin was >10mm in 17.2%, 6 - 10mm in 23.4%, 1 - 5mm in 35.9%, <1mm in 8.3% and involved in 15.1%. A total of 27 (14.0%) patients required re excision. Of these, 16 (8.3%) had repeat BCT and 11 (5.7%) had a mastectomy. Residual tumor was present in 14 of the re excised specimens. 80.8% patients completed radiotherapy treatment post wide local excision. A total of 11 (5.7%) patients had a local recurrence. Time to recurrence averaged at 46 months (range 12 to 106 months). The average period of follow up was 53.9 months (range 1 to 108 months).
Conclusions: The re-excision and local recurrence rates in our unit are acceptable and comparable other units in South Africa (5.5% recurrence rate at 65 months of follow up, Mannell, Department of Surgery, University of the Witwatersrand, and Linksfield Park and Park Lane Clinics, Johannesburg, 2005). In the prospective randomized trials conducted internationally, 10-year local recurrence rates ranged from 4% to 20% with breast-conserving surgery and radiation therapy.
LONG-TERM FOLLOW UP OF INTRAOPERATIVE RADIOTHERAPY (IORT) FOR EARLY BREAST CANCER IN A RESOURCE RESTRICTED COUNTRY Z Keyser, J P Apffelstaedt, K Baatjes
Division of Surgery, University of Stellenbosch, Tygerberg Hospital
Introduction: Definitive single dosage intraoperative radiation is accepted for early breast cancer patients in well-resourced environments despite a lack of long-term data on its safety and oncologic efficacy. We here present 12-year outcome data of an initial series of definitive, single dosage IORT in a developing country.
Methods: From 2002-2005 patients with TNM stage 0-II breast cancer, qualifying for breast conservation had a tumour excision. In the same session a locally designed low cost applicator was inserted into the tumour bed and afterloaded with an Ir192 source to a single dose of 21Gy. Demographic, histopathologic, clinical and oncologic outcome data were analysed in this prospective cohort study.
Results: Thirty-nine patients with a mean age of 54.7 (35-68) years were treated. Tumours were clinically staged T0 (n=1), T1C (n=18) and T2 (n=20) and N1 (mean tumour diameter 16.8mm) in 6 patients. Mean histopathologic tumor diameter was 19 mm; 36 tumors were infiltrating ductal, 2 infiltrating lobular and one mucinous; 30 tumors were ER receptor positive, 4 patients had nodal involvement. The median follow-up of the entire group is 120 months. At last follow up, ASTRO guidelines on APBI suitable (n=3), cautionary (n=28) and unsuitable (n=8) cases, 0, 3 and 1 cases respectively suffered an isolated local recurrence after 1, 3, 5 and 8 years. Three of these were salvaged by mastectomy and are alive without disease; 1 declined further treatment and progressed to distant recurrence. No demographic/histopathologic parameter was associated with local recurrence. Seven other patients suffered distant recurrence. At 12 years, the local recurrence, disease-specific and overall survival rates were 12, 72 and 68%.
Conclusion: Long-term recurrences were rare despite the majority of cases falling into ASTRO '' cautionary/ unsuitable'' groups. In all breast conservation patients, a cheap applicator used with existing afterloaders, may make IORT an effective option in financially constrained environments, especially for ASTRO suitable and cautionary cases.
A NOVEL INCISION FOR SKIN-SPARING MASTECTOMY - THE DOUBLE MOON DESIGN
Y Brakovsky1, I Buccimazza2
1 Department of Plastic & Reconstructive Surgery, Nelson R. Mandela School of Medicine, University of Kwa-Zulu Natal, Durban
2 Department of Surgery and Breast Unit, Nelson R. Mandela School of Medicine, University of Kwa-Zulu Natal, Durban
Introduction: Standard incisions for Skin-Sparing Mastectomy (SSM) differ in the extent of surgical access they provide as well as cosmetic outcomes they produce. A novel incision which follows the neo-areola border is proposed and compared to the traditional incisions.
Aim: The study aimed to answer two questions. The first was to assess whether it improved surgical access and the second was whether the cosmetic outcomes were superior to standard methods.
Patients & Methods: This was a retrospective chart and photographic review of all patients who underwent SSM with immediate expander/ acellular dermal matrix-based reconstruction at the Breast Unit, Inkosi Albert Luthuli Central Hospital, over a 40 month period between December 2011 and April 2015. We included patients with a small breast size (A or B cup) and minimal ptosis, and excluded patients with large, ptotic breasts treated with reduction pattern SSM or straight line closure. Data collected included patient demographics; area of surgical access in all approaches, calculated using mathematical formulas (Figure 1); post-operative measurements of the neo-NAC position, and a patient questionnaire. Pre-and post-operative photographs were obtained for each patient. Data was stored on an excel spreadsheet.
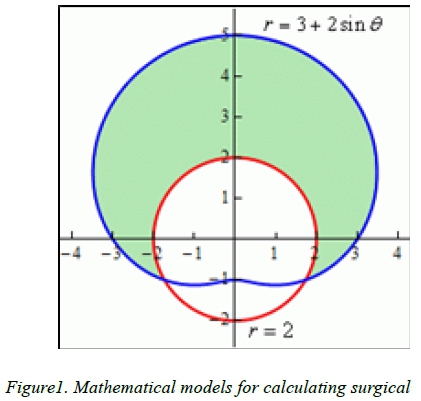
Results: 20 patients (22 breasts) met the inclusion criteria. The average age was 46.6 years (range 32-59 years). The majority were Indian (n=12) and three patients were from rural areas. The calculated area of surgical access offered over a three-fold increase in access when compared to nipple-areola complex excision only (38.68cm2 vs 12.56cm2), and compared favourably with other standard SSM incisions. The final scar position was maintained in the central nipple-areola complex area in all cases. 18 patients preferred the new incision to straight line closure. Two patients had no specific preference.
Conclusions: The new incision offers a significant increase in surgical access for an oncologically safe mastectomy, and good access to all breast quadrants due to the central position. The site of the scar along the neo-areola border facilitates future reconstruction of the nipple-areola complex.
Oral presentations
INDICATIONS FOR USE OF DAMAGE CONTROL SURGERY IN CIVILIAN TRAUMA PATIENTS: A CONTENT ANALYSIS AND EXPERT APPROPRIATENESS RATING STUDY
D J Roberts2,3,4, N Bobrovitz5, DA Zygun2,6, C G Ball1,4,7, A W Kirkpatrick1,4, P D Faris8, K Brohi9, S D'Amours10, T C Fabian11, K Inaba12, A K Leppaniemi13, E E Moore14, P H Navsaria15, A J Nicol15, N Parry16 and H T Stelfox2,3,17
1 Departments of Surgery, University of Calgary
2 Community Health Sciences, University of Calgary
3 Critical Care Medicine, University of Calgary
4 Regional Trauma Program, University of Calgary and the Foothills Medical Centre
5 Nuffield Department of Primary Care Health Sciences, University of Oxford
6 Division of Critical Care Medicine, University of Alberta
7 Department of Oncology, University of Calgary
8 Alberta Health Sciences Research - Research Analytics, University of Calgary and the Foothills Medical Centre
9 Centre for Trauma Sciences, Blizard Institute, Queen Mary University of London
10 Department of Surgery, University of New South Wales
11 Department of Surgery, University of Tennessee Health Science Center
12 Department of Surgery, University of Southern California
13 Department of Surgery, Helsinki University Central Hospital
14 Department of Surgery, University of Colorado
15 Trauma Centre, Department of Surgery, Groote Schuur Hospital, University of Cape Town
16 Divisions of General Surgery and Critical Care Schulich School of Medicine and Dentistry, Western University and the Trauma Program, London Health Sciences Centre, London, Ontario, Canada
17 Department of Medicine, University of Calgary
Background: Although damage control (DC) surgery may improve survival in select, severely injured patients, the procedure is associated with significant morbidity, suggesting that it should only be used when appropriately indicated.
Aim of Study: To characterize and evaluate indications for use of DC surgery in civilian trauma patients.
Materials and Methods: Two investigators used an abbreviated grounded theory method to synthesize indications for DC surgery reported in peer-reviewed articles between 1983 and 2014 into a reduced number of named, content-characteristic codes representing unique indications. An international panel of trauma surgery experts (n=9) then rated the appropriateness (expected benefit-to-harm ratio) of the coded indications for use in adult civilian trauma patients.
Results: The 1,107 indications identified in the literature were synthesized into 123 unique pre- (n=36) and intraoperative (n=87) indications. The panel assessed 101 (82.1%) of these indications to be appropriate. The indications most commonly reported and assessed to be appropriate included pre- and intraoperative hypothermia (median temperature <34°C), acidosis (median pH <7.2), and/or coagulopathy. Others included 5 different injury patterns, inability to control bleeding by conventional methods, administration of a large volume of packed red blood cells (median >10 units), inability to close the abdominal wall without tension, development of abdominal compartment syndrome during attempted abdominal wall closure, and need to reassess extent of bowel viability.
Conclusions: This study identified a comprehensive list of candidate indications for use of DC surgery in adult civilian trauma patients. These indications provide a practical foundation to guide surgical practice while studies are conducted to evaluate their impact on patient care and outcomes.
REAL TIME ELECTRONIC INJURY SURVEILLANCE IN A LEVEL 1 TRAUMA CENTER
E Zargaran1 R Spence2,3, P Navsaria2,4, A Nicol2,4, S Edu2,4, L Roodt2,4
1 General Surgery, University of British Columbia, Vancouver, Canada
2 University of Cape Town, Cape Town, South Africa
3 Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston, USA
4 Trauma Surgery, Groote Schuur Hospital, South Africa
Background: Injury surveillance is difficult to sustain in low resource countries because of cost and complexity. The electronic Trauma Health Record (eTHR), designed for front-line clinicians for documentation of trauma patients and with the ability to wirelessly upload research and policy relevant data to a real-time trauma registry was created. We hypothesized this novel injury surveillance tool could successfully be implemented in a high-volume, low-resource, African trauma center.
Aim: To implement a superior electronic trauma registry with no workflow hindrance at a busy level 1 Trauma Center in South Africa
Materials & Methods: A prospective cohort study was designed to describe and evaluate the burden of trauma at Groote Schuur Hospital (GSH), Cape Town's Level I trauma center. Consecutive trauma patients treated at GSH for a 12-month period formed the study cohort. Clinician generated eTHR admission records, operative notes, and discharge summaries completed on iPads were used as the data capture tool to create a real-time electronic trauma registry. eTHR's database was used for immediate evaluation of the demographics, mechanisms, and predictors of injury. Prospective calculation of the Revised Trauma Score (RTS), Injury Severity Score (ISS), and the Kampala Trauma Score (KTS) were obtained. Using geographic information systems (GIS), real-time maps of the incidence of traumatic events and flow of trauma patients within Cape Town were generated. eTHR's trauma quality improvement audit filters allowed for the analysis of trauma care delivery and patient outcomes.
Results: Over 12 654 trauma presentations were documented and analysed in real-time by the new, clinically integrated electronic injury surveillance system. There was a predictable predominance of young males and violent mechanisms of injury with associated drug intoxication in the study cohort. GIS analyses demonstrated clusters of injuries originating mainly from vulnerable and low-income neighborhoods. Spectrums of surgical interventions were noted. Barriers to patient care were revealed. Hospital complications were accurately captured and graded. Issues with implementation were related to connectivity to a strong cellular signal and stability of storing large amounts of trauma data on local network servers.
Conclusions: The affordable and self-populating trauma registry created at GSH opens the possibility for other highvolume, low-resource trauma centers to begin the first steps in the development of their own organized systems of trauma care - a development that may allow unprecedented advances in injury control globally.
LAPAROSCOPIC-ASSISTED APPROACH IN MANAGEMENT OF PATIENTS WITH PENETRATING ABDOMINAL TRAUMA
O Y Matsevych, M Z Koto, S R Motilall, N Kumar
Department of Surgery, Sefako Makgatho Health Science University, Faculty of Medicine,
Dr George Mukhari Academic Hospital, Pretoria, South Africa
Background: Therapeutic laparoscopy for trauma remains a controversial issue. It requires high operating team performance, advanced laparoscopic skills and fine feel of the turning point where conversion is necessary. Multiple injuries become a real challenge during laparoscopy and usually lead to conversion. Laparoscopy assisted approach may be helpful in the case of multiple injuries and still provide the benefit of minimally invasive surgery.
Aim: To assess the feasibility of laparoscopic-assisted approach in the setting of penetrating abdominal trauma (PAT).
Methods: We retrospectively reviewed all patients with PAT managed with laparoscopic-assisted approach in Dr George Mukhari Academic Hospital from January 2012 to December 2014. The mechanism, location of injury, intraoperative findings, performed procedures and significant complications were analysed.
Results: A total of 189 patients were managed with laparoscopy. Therapeutic laparoscopy was performed on 111 patients. Laparoscopic-assisted approach was utilized in 51 patients. Twenty five patients sustained stab wounds and 26 sustained gunshot wounds. Commonly performed procedures were organs repair, resection and anastomosis, and hemicolectomies. There were no conversion or missed injuries. Nine patients had complications. Two had negative re-laparoscopy. One patient had re-laparoscopy and one had laparotomy for septic intraabdominal haematoma. One patient underwent laparotomy for bleeding from anastomosis site and three days later developed fatal pulmonary embolism. Two patients developed enterocutaneous fistula. One developed cellulitis and one had port site sepsis. (See table.)
Conclusion: Laparoscopic-assisted approach is feasible in management of patients with PAT. It offers the versatility and speed of open surgery and preserves the benefits of minimally invasive approach.
RELATIONSHIP BETWEEN SHOCK INDEX AND INJURY SEVERITY SCORE IN TRAUMA PATIENTS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL (DGMAH)
N Kumar, S R Motilall, O Y Matsevych, M Z Koto
Trauma Unit, Department of General Surgery, Sefako Makgatho Health Science, Faculty of Medicine, Dr George Mukhari Hospital, Pretoria
Background: At present there is no score that accurately predicts with high sensitivity and specificity a severely injured patient and correlates injuries with outcome. The Shock Index (ratio of heart rate to systolic blood pressure) has been advocated to better risk stratify patients for increased transfusion requirements (SI>0.9) and early mortality.
Aim: To assess Shock Index (SI) as a simple measure of predicting severity of injury and mortality in trauma patients.
Material and Methods: This is a retrospective review of patient data collected from April 2014 to March 2015. The data (demographics, diagnosis, date of presentation, heart rate, systolic blood pressure, mortality) was collected from the trauma unit database. Inclusion was of P1 and P2 patients. Exclusion was of all cases with missing or incomplete records. All patients were resuscitated according to ATLS principles. ISS and SI were then calculated. The SI values were divided into three groups and correlated with the ISS using the IBM SPSS Statistics 22 software with the PearsonChi Square tests. P values < 0.05 were significant.
Results: A total of 300 patients were traced in the trauma database of which 166 patients were identified for the study as having complete data. Of these patients, the average age was 29.5 years with 38 being female and 128 being male. 10 patients were paediatric patients andthe rest were adults. A very high correlation was noted between a higher value of shock index and a higher value of ISS as well as between mortality and SI and ISS with the p value for both being <0.05. All mortalities were observed in the group of patients with SI>0.9.

Conclusion: Patients with a high Shock Index on admission are most likely to have a higher value of ISS. In our study, SI>0.9 was associated with mortality and high ISS.
AN AUDIT OF TRAUMATIC DIAPHRAGMATIC INJURY IN PIETERMARITZBURG
N D Souza, G L Laing, J L Bruce, D L Clarke
University of Kwa Zulu Natal
Introduction: Traumatic diaphragm injury (TDI) can result following both penetrating and blunt thoraco-abdominal trauma and can present acutely as a simple injury or a diaphragmatic herniation (DH) and as a chronic (DH). This audit of our experience with diaphragmatic injury from a busy South African trauma service reviews the spectrum of the pathology and highlights our current approaches to these injuries.
Methodology: The Pietermaritzburg Metropolitan Trauma Service (PMTS) has maintained and Electronic Surgical Registry (ESR) and a Hybrid Electronic Medical Record (HEMR) system since January 1st 2012. All cases of TDI managed between the 1st January 2012 and the 31st May 2014 were extracted from the registries and analysed.
Results: A total of 105 TDIs were identified and repaired during the study period. The mean patient age was 30 years (range 15-68 years - SD 9.7). The majority (92.4%) of patients were male (97/105). Penetrating trauma was the leading mechanism of injury (94%). 75 patients sustained TDI from SWs, and the remaining 24 injuries resulted from gunshot wounds (GSWs). 69 (69.7%) of these 99 injuries presented acutely and underwent emergency laparotomy (63), thoracotomy (1), or combined thoracotomy and laparotomy (5). Seven patients underwent surgical intervention following a delayed presentation by way of thoracoscopy (2), laparotomy (4) and combined thoracotomy and laparotomy (1). Twenty three patients underwent semi-elective laparoscopy (22) and thoracoscopy (1).
Conclusion: TDI is a fairly uncommon injury with a local incidence of 1.59%. It presents in a spectrum from the obvious to the occult. Our results have shown that diagnostic laparoscopy is a valuable tool to diagnose and repair TDIs.
OPERATIVE RESULTS FOR FREE PERITONEAL FLUID WITHOUT SOLID ORGAN INJURY DIAGNOSED BY COMPUTED TOMOGRAPHY AFTER BLUNT ABDOMINAL TRAUMA
R van Rensburg, A Lambrechts
Division of Surgery, University of Stellenbosch
Background: Opinion is divided regarding the safety of a selective non-operative management strategy for isolated free peritoneal fluid in the absence of solid organ injury, as revealed by computed tomography (CT scan) in the setting of blunt abdominal trauma. Despite the high sensitivity of CT scan for the diagnosis of solid organ injury, the sensitivity for injuries of the mesentery or hollow viscera is suspect. In an institution under extreme pressure with regard to personnel, resources and theatre time, non-operative management is an attractive yet potentially dangerous strategy.
Aim: To describe the operative findings of laparotomy performed for free peritoneal fluid without solid organ injury as diagnosed by CT scan after blunt abdominal trauma.
Methods: A single institution retrospective cohort study was performed, spanning the period from June 2010 to May 2015. Cases were identified from the prospectively generated Tygerberg Academic Hospital Trauma Surgery Database, as well as the radiology database. Adult patients (>18 years) who received a laparotomy for the indication of free fluid without solid organ injury on CT abdomen after blunt abdominal trauma were included. Patients with other established indications for laparotomy after blunt abdominal trauma and suspicious findings on CT scan were excluded. The analysis included age, gender, mechanism and intra-operative findings.
Results: The inclusion and exclusion criteria were met by 44 patients. The median age of the study population was 32 years (range 18 to 58 years), of which 33 (79%) were male. The mechanism of injury was motor vehicle accident in 16 (38%), pedestrian vehicle accident in 17 (40%) and assault in 9 (21%) of patients.
Therapeutic laparotomies were performed in 22 (52%) patients. The most common injuries were small bowel perforations (27%) and bleeding mesenteric injuries (27%). Less common injuries were bleeding greater omentum (14%), bladder (14%), pelvic fractures requiring packing (9%), gallbladder (5%) and an incidental tubo-ovarian complex (5%). Twenty laparotomies were non-therapeutic (48%).
Conclusion: The high percentage of therapeutic laparotomies and hollow viscus perforations suggest that a non-operative management strategy for patients with isolated free fluid on CT abdomen following blunt abdominal trauma is unsafe.
SELECTIVE NON-OPERATIVE MANAGEMENT OF STAB WOUNDS TO THE POSTERIOR ABDOMEN IS SAFE
V Y Kong, B Sartorius, G V Oosthuizen, D L Clarke
University of Kwa Zulu Natal, Pietermaritzburg Metropolitan Trauma Service
Introduction: The selective non-operative management (SNOM) of stab injuries of the anterior abdomen is well established, but its application to the posterior abdomen remains controversial.
Materials and Methods: A retrospective review of 1,013 patients was undertaken at a major trauma service in South Africa over a five-year period.
Results: Ninety per cent of patients were males, and the mean age was 25 years. The mean time from injury to presentation was 4 hours and 73% of all injuries were inflicted by knives. A total of 9% (93) of patients required a laparotomy [Group A] and 82% (833) were successfully observed without the need for operative intervention [Group B]. CT imaging was performed on 52 patients (5%) who had haematuria [Group C], 25 (3%) who had neurological deficits [Group D], and 10 (1%) with retained weapon injuries [Group E]. The accuracy of physical examination for identifying the presence of organ injury was 88%. All observed patients who required laparotomy declared themselves within 24 hours. There were no mortalities as direct result of our current management protocol.
Conclusions: Selective management based on active clinical observation and serial physical examination is safe, and when coupled with the judicious use of advanced imaging, is a prudent and reliable approach to in a resource constrained environment.
THE SPECTRUM OF INJURIES FOR POSTERIOR ABDOMINAL WALL STAB INJURIES
V Y Kong, G V Oosthuizen, D L Clarke
University of Kwa Zulu Natal, Pietermaritzburg Metropolitan Trauma Service
Introduction: The indications for surgery and the spectrum of injury associated with anterior abdominal stab wounds is well established. The literature on the spectrum of organ injury associated with SW to the posterior abdomen (PA) however, is limited.
Materials and Methods: We reviewed our experience of 105 consecutive patients who had established indications for laparotomy managed over a four year period in a high volume trauma service in South Africa.
Results: Ninety-two per cent (97/105) of patients were males and the mean age was 24 years. Fifty-seven (54%) of the 105 patients had immediate indications for laparotomy. The remaining 48 (46%) patients were actively observed, and the indications for laparotomy became apparent during the observation period. Forty-seven of the 48 observed patients developed peritonitis. Of the 105 laparotomies performed, 94 were positive (90%) and 11 were negative. Of the 94 positive laparotomies, 92 were therapeutic and 2 were non-therapeutic. A total of 176 organ injuries were identified: 50 of the 94 (53%) patients sustained a single organ injury, while the remaining 44 (47%) patients sustained multiple organ injuries. The most commonly injured organs were: colon (63), spleen (21) and kidney (19).
Conclusions: The pattern of intra-abdominal injuries secondary to SW to the posterior abdomen is different to that seen with the anterior abdomen. Colonic injury is most commonly encountered followed by injuries to the spleen and kidney. Our approach of SNOM is safe but clinicians must remain vigilant of the potential occult injuries.
AUDIT OF THE USE OF TEMPORARY ABDOMINAL CLOSURE IN A TERTIARY HOSPITAL IN PIETERMARITZBURG
C J Steenkamp
Introduction: Temporary abdominal closure (TAC) is required for a number of acute surgical conditions. This study reviews the use of TAC and its outcomes in a regional hospital in South Africa.
Method: This study is a retrospective review of all patients that had an open abdomen managed with Temporary Abdominal Closures. This includes all patients documented in the PMB trauma database ranging from December 2012, up to February 2015.
Results: A total of 138 (38 female and 100 male) patients were left with Temporary Abdominal Closures. 50 Were closed with a Bogota bag and 11 of these were done at repeat laparotomy. The remaining 88 were closed with an Opsite sandwich, of which 17 were applied at repeat laparotomy. 89% of all of these patients were African, with 5% Asian, 4% caucasian and 2% coloured. The majority of patients (49%) were between the age of 18 - 40, 22% between 41 - 60, 9% older than 60, 8% between 12-18 years and 12 % below the age of 12. The pathology leading to TAC included: Trauma (blunt and penetrating) 36%, perforated appendicitis 22%, Intra-abdominal sepsis after an initial laparotomy 7%, perforated ulcer 7%, anastomotic breakdown 6%. Less common indications included abdominal compartment syndrome and necrotizing pancreatitis. Thirty-eight per cent of (TAC) Temporary abdominal closures were applied as part of damage control surgery and 86% of the patients were admitted to ICU post-operatively.
Conclusion: Temporary abdominal closures is used widely in Pietermaritzburg in both trauma and general surgery. It is mostly applied during damage control laparotomies and for the management of intra-abdominal sepsis.
EMERGENCY LAPAROTOMIES IN THE DEVELOPING WORLD
V Soldati; M Scriba; J Bruce; D Clarke; G Laing
University of KwaZulu-Natal
Emergency laparotomy is a common procedure performed by surgeons all over the world. The aim of this paper is to review the spectrum of aetiology in patients requiring emergency laparotomy at Grey's Hospital which is a tertiary institution in Pietermaritzburg, South Africa. These findings will then be compared with findings from other developing countries such as India and contrasted with the Western World. This is a retrospective study with data collected using the Hybrid Electronic Medical Registry (HEMR) at Grey's Hospital over a 2 year period from December 2012 to December 2014. The inclusion criteria was all patients presenting to Grey's Hospital accident and emergency unit over the above mentioned time period with features of perforation peritonitis, requiring an emergency laparotomy. Exclusion criteria were: all paediatric patients; trauma aetiology; Non-therapeutic laparotomy; Gynaecological findings. This left us with a sample size of 891 patients. The objectives set include establishing the spectrum of aetiology in patients requiring emergency laparotomy in South Africa. The end point would be to therefore prove that the spectrum of aetiology is similar across developing countries and different to that of the developed world. Data collected from HEMR was analysed through Microsoft Excel and results depicted through tables and graphs on a spreadsheet. HEMR has full ethics approval to maintain a surgical database and to use data for clinical audit: BCA 221/13. The results show that the commonest finding during emergency laparotomy in our setting is: Perforated Appendix (56%); followed by Adhesive Bowel Obstruction (13%); Peptic Ulcer Disease (12%); Tuberculosis of the Abdomen (9%); Large Bowel Obstruction (6%). Overall mortality was 10%. We can therefore conclude that results are comparable to findings in India where the causes for perforation peritonitis include: Peptic Ulcer Disease; Perforated Appendix; Typhiod and Tubercular perorations in that order. We can also contrast this to the U.K where perforation of the large bowel was the most common indication of emergency laparotomy.
THE ABSOLUTE NUMBER OF REPEAT OPERATIONS FOR COMPLEX INTRA-ABDOMINAL SEPSIS IS NOT A USEFUL PREDICTOR OF NON-SURVIVAL
M F Scriba, G L Laing, J L Bruce, D L Clarke
Department of Surgery, Pietermaritzburg Hospital Complex. University of KwaZulu Natal. Pietermaritzburg, KwaZulu-Natal, South Africa
Introduction/Background: When multiple relaparotomies are required to manage intra-abdominal sepsis questions about futility of treatment frequently arise. This study focuses specifically on patients who required two or more repeat laparotomies and describes the spectrum of disease necessitating multiple repeat laparotomies and the associated outcomes in the hope of clarifying the issue.
Methods: This study was conducted over a 20 month study period (December 2012 - July 2014) at Greys Hospital, Pietermaritzburg, South Africa. Prospective data entered into an electronic registry was retrospectively analysed. Full ethical approval to maintain and use the registry and full ethical approval for this study were both granted by the University of KwaZulu-Natal Biomedical Ethics Committee (BCA221/13 and BREC BE047/14). All adult patients, inclusive of general surgical and trauma patients, who needed at least two relaparotomies were included in the study.
Results: Seventy-two patients were included in the study and required a total of 182 relaparotomy operations. Demographics showed a male predominance (75% male). The average age was 39 years. General surgical patients accounted for 60% (43) and trauma patients for 40% (29) of the total. The majority of patients required only two relaparotomies (65 %), while two patients required a total of 6 relaparotomies each, both with an initial diagnosis of appendicitis and both these patients survived. Temporary abdominal closure (TAC) was performed in 36 % (26) of initial laparotomies, while 46 % (33) of patients had an open abdomen at the time of discharge or death. Sixty percent (43 patients) required intensive care or high care unit (ICU/HCU) admission and 53 patients (74 %) had a total of 71 documented morbidities. Total mortality for this study was 21 % (15), however there was no correlation between number of procedures and mortality (Table 1).

Conclusion: This study highlights the underlying pathologies necessitating multiple relaparotomies in our setting and the associated outcomes in these patients. The total number of procedures is associated with increased morbidity rates but not necessarily with increased mortality rates. This is important to consider when the issue of futility of treatment arises, as the absolute number of repeat laparotomies is a poor marker of futility and other factors must be considered.
PLANNED VERSUS ON-DEMAND RELAPAROTOMY IN A DEVELOPING WORLD TERTIARY LEVEL SURGICAL SERVICE
M F Scriba, G L Laing, J L Bruce, D L Clarke
Department of Surgery, Pietermaritzburg Hospital Complex. University of KwaZulu Natal, Pietermaritzburg, KZN
Introduction/Background: Little international literature exists to support the practice of planned relaparotomy (PR), with an on-demand (OD) relaparotomy strategy being the preferred management choice in most centres. However, data from the developing world on this topic is lacking. This study compares OD versus PR in a developing world setting. The aim is to identify and refine local practices and ultimately to improve outcomes in these patients.
Material and Methods: This study was conducted over a 20 month study period (December 2012 - July 2014) at Greys Hospital, Pietermaritzburg, South Africa. All adult patients, inclusive of general surgical and trauma patients, who needed a single relaparotomy, were included in the study. Prospective data entered into an electronic registry was retrospectively analysed. Full ethical approval for the registry and this study was granted by the University of KwaZulu-Natal Biomedical Ethics Committee.
Results: A total of 102 patients were included, with a 71% male predominance and an average age of 36 years. General surgical conditions accounted for 75 % of index operations, with complicated appendicitis and stab abdomen being the most prevalent underlying diagnoses. PR and OD operations accounted for 49% and 51% respectively. Baseline characteristics between the groups on admission showed no difference in age, gender, blood pressure or temperature, but the PR group did have a higher prevalence of tachycardia and higher Modified Early Warning System (MEWS) scores. Comparisons between the two groups showed no statistically significant differences between negative relaparotomy rate, rate of open abdomen at time of death/discharge or overall mortality. PR was associated with higher Intensive Care Unit (ICU) admission rates (60% vs. 27%), but lower morbidity rates (44% vs. 67%) and much shorter average time interval between initial laparotomy and relaparotomy (59 hours vs. 130 hours) (Table 1).
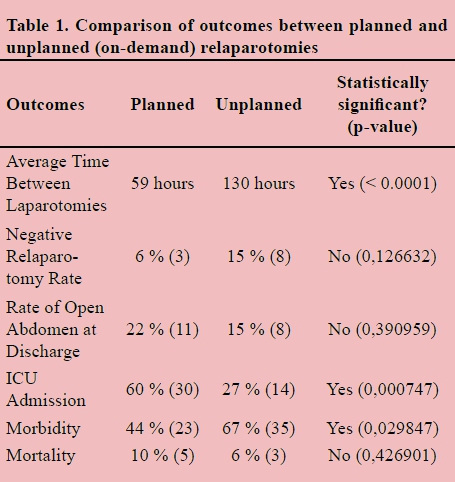
Conclusion: This study reveals a relatively high volume of complicated intra-abdominal sepsis in young patients in our setting. We have an aggressive surgical approach with a low threshold for temporary abdominal closure (TAC) and re-operation. It would appear that this approach is justified by the fact that the ultimate rate of TAC is low and by the low negative relaparotomy rate. In our environment the OD approach is associated with long delays between index operation and re-operation and this likely translates into a high morbidity rate. An aggressive PR approach does place a greater burden on post-operative ICU resources, however if we wish to adopt an OD approach we need to improve our systems to make sure that patients requiring relaparotomy are identified promptly and that their repeat surgery is expedited.
THE PREVALENCE OF SUPPRATIVE PELVIC COLLECTIONS POST LAPAROSCOPIC APPENDECTOMY: A RETROSPECTIVE STUDY AT DR GEORGE MUKHARI HOSPITAL
S N Phaleng, M Z Koto
Department of Surgery, Sefako Makgatho Health Sciences University and Dr George Mukhari Academic Hospital
Background and objectives: Laparoscopy has been considered the operation of choice in uncomplicated appendicitis. The role of laparoscopic appendectomy has been regarded controversial in complicated appendicitis. Recent studies have reported an increase risk of intra-abdominal collections (abscess formation) following laparoscopic operation for perforated appendicitis. The objective of the study was to determine the prevalence of pelvic abscess (collections) post laparoscopic appendectomy.
Methods: Data was collected retrospectively for patients who underwent laparoscopic appendectomy (LA) over an 18 month period (from November 2011 to April 2013). Analysis included demographics, clinical findings, laboratory tests (results), intraoperative procedures, intraoperative findings e.g. presence of pre-existing fluid and type of appendicitis, the complicated (perforated or gangrenous) at surgical or pathological assessment or simple and operative management and complications.
Results: The review identified 180 patients with diagnosis of appendicitis. One hundred and thirty nine (139) patients underwent laparoscopic appendectomy, forty one patients were excluded from the study, fifteen were converted to open, twelve patient records could not be retrieved, seven patients had incomplete medical records and seven did not turn up for interval appendectomy.
63,3% of patients had acute simple appendicitis, 25.9% had perforated appendectomies, 3,6% had gangrenous appendicitis , 4,32% had normal appendix and 2,88% had an appendicular abscess.
96,4% patients were black, 2,88% white and 0,72% were Indian.
Male to female ratio was 4:1.
The prevalence of pelvic collections was 5%. Two patients had postoperative pelvic collection, which were diagnosed clinically and managed conservatively. Four patients developed postoperative right iliac fossa and pelvic collections. One patient had only pelvic collections.
All the collections were in the cases of perforated appendicitis.
Conclusion: Laparoscopic appendectomy appears to be a safe procedure even in the presence of complicated appendicitis. Our intra abdominal abscess rate was 5%. It is comparable with other studies.
LAPAROSCOPIC APPENDECTOMY FOR APPENDICITIS COMPLICATED BY INTRA-ABDOMINAL ABSCESSES AT SEBOKENG HOSPITAL
I Bombil1, W S Lunda1, A Maraj2
1 Department of Surgery, Sebokeng Hospital and Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa
2 Department of Surgery, University of Witwatersrand, Johannesburg, South Africa.
Corresponding author: I Bombil (bombil@telkomsa.net)
Introduction: There is a concern that laparoscopic appendicectomy for appendicitis complicated by intra-abdominal abscesses is associated with a higher incidence of recurrent intra-abdominal sepsis. In this study, the results of appendicitis complicated by gross intra-abdominal sepsis and managed laparoscopically are reviewed.
Aim: The aim of the study was to determine the incidence of recurrent intra-abdominal sepsis and the overall outcome of the cases.
Materials and Methods: This was a retrospective review of prospectively collected data of all cases of appendicitis treated laparoscopically both in the paediatric and adult population at Sebokeng Hospital from November 2011 to October 2012. Patients without intra-abdominal pus collections at the initial operation were excluded. The following parameters were analysed: patient demographics, length of hospital stay, number of Intensive Care Unit (ICU) admissions, repeated operations, mortality, 30 day re-admission rate, available histology results, intra-abdominal abscesses (IAA) sites at initial surgery and as post operative complications. Ethical approval was obtained from the Human Research Ethics Committee (HREC) of the University of the Witwatersrand
Results: One hundred and sixty seven laparoscopic appendicectomies were performed between November 2011 and October 2012. Thirty four percent (57 patients) had appendicitis complicated by IAA. There were 40 males and 17 females. The mean age was 24 years (range 5-75 years). Twenty one percent (12 patients) developed recurrent IAA of which five patients required repeated operations and the remaining seven patients were treated conservatively. Five percent (3/57) of patients were admitted in ICU and there was no mortalities. Overall, 91.3% (52/57) of patients did not require re-intervention.
Conclusion: Laparoscopic appendicectomy for appendicitis complicated by IAA was associated with a 21% incidence of recurrent IAA for which 5 of these 12 patients required repeated surgery.
LAPAROSCOPIC MANAGEMENT OF RUPTURED APPENDIX WITH 4 QUADRANT PUS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL (DGMAH)
T Sumbana, M Z Koto
Sefako Makgatho Health Science, Faculty of Medicine, Dr George Mukhari Hospital, Pretoria
Background: Perforated appendix with generalised peritonitis has been traditionally treated surgically with laparatomy. The role of laparoscopy in uncomplicated appendicitis is comparable with open appendectomy with laparoscopy having low wound infection rates. The high rates of pelvic abscess have been associated with laparoscopic appendectomy. The role of laparoscopy in patients with generalised peritonitis is unclear. There is always fear of missing collections.
Aim: To present our experience with the use of laparoscopy in the setting of 4 quadrant pus.
Methods: Retrospective review of data collected prospectively on patients with acute appendicitis treated laparoscopically during the period January 2012 to December 2014 at DGMAH. We identified patients with 4 quadrant pus that form the basis of the study. Four quadrant pus was defined as pus in the right upper quadrant, left upper quadrant, lower abdomen; pelvis ,right iliac fossa ,left iliac fossa. The patients were offered laparoscopic surgery after resuscitation. Operative techniques was under General Anaesthesia ,we use 3 port technique with camera port left upper quadrant, two working ports midline suprapubic and left iliac fossa. Pneumoperitoneum was achieved using open hasson technique. Pus was suctioned out and appendectomy done specimen sent for MC&S. Washout in some patients, other pts were only offered suction of the pus. All patients received antibiotics and analgesia.
Results: From a total of 458 patients with appendicitis treated laparoscopic, 70 patients (15%) with ruptured appendix and four quadrant pus were identified for analysis. Demographics: 68, 57 % (48) Male; 31, 43% (22) female; average age 23 range 4-74years. Morbidity of 4,29%; Relooks 15,71%; Conversion rate 10%; Mortality of 5,80%. Hospital stay 3-16 days average of 6days.Operative time ranging from 27-203 minutes average 125 minutes.
Conclusion: Laparoscopy has a role in patients with ruptured appendix with four quadrant pus with the morbidity and mortality at 4, 29% and 5, 80% respectively .However this group of patients still poses a significant management challenge.
SURGICAL OUTCOMES OF APPENDICECTOMY IN HIV-INFECTED PATIENTS
S Sobnach1, C J Ede2, G D van der Linde3, A Bhyat2, D Kahn1
1 Department of Surgery, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, Anzio Road, Observatory, Cape Town, Western Cape 7925, South Africa
2 Department of Surgery, Kimberley Hospital, Kimberley, South Africa
3 National Health Laboratory Services, Kimberley, South Africa
Background: The Human Immunodeficiency Virus (HIV) pandemic has added a new dimension to the management and outcomes of many surgical conditions. The aim of this study is to describe and compare the outcomes of appendicectomy in HIV-infected (HIV+) and HIV-negative (HIV-) patients.
Methods: Ethics approval was obtained for this study. This is a prospective cohort study of patients undergoing appendicectomy at a large regional hospital over a 12-month period. Demographic data, duration of pre-hospital symptoms, HIV status, surgical approach, operative findings, histopathology reports, hospital stay and complications were recorded. Differences between the HIV+ and HIV- patients were then described, analysed and compared.
Results: The study group comprised 134 patients; 18 (13.4 %) tested positive for HIV. HIV+ patients were significantly older (mean age of 29.3 vs. 20.3 years, p= 0.002) and had longer duration of pre-hospital symptoms (mean of 3.94 vs. 2.57 days, p= 0.03). Postoperative complications (44.4 % vs. 17.2 %, p= 0.03) and lengthier hospital stay (7.28 days vs. 5.95 days, p= 0.004) were also more frequently seen in the HIV+ patients. There were no differences in appendiceal rupture rates, histopathological findings and mortality.
Conclusion: HIV infection is common in patients admitted with clinical features of acute appendicitis in South Africa. Presentation in HIV+ patients is delayed and surgery is associated with significant postoperative morbidity and longer hospital stay.
PIG AND HORSE MUCINS AND THE INHIBITION OF HIV-1
A S Mall1, S T Pillay1, J R Dorfman2
1 Division of General Surgery, University of Cape Town, South Africa
2 ICGEB and Division of Immunology, University of Cape Town, South Africa
Background: Sub-Saharan Africa is the world's worst HIV-AIDS affected region. More interventions to manage this pandemic are urgently required. We have previously shown that human saliva and cervical mucus, together with purified salivary, breast milk and cervical mucins inhibit HIV-1 in an in vitro assay. To obtain mucus in larger amounts we tested the hypothesis that mucins from an animal model will display similar inhibition of HIV-1 as human mucins.
Materials and Methods: This study was approved by The University of Cape Town Research and Ethics Committee (AEC REF NO: 013/027). Pig gastric and salivary mucus was extracted in 6M guanidinium hydrochloride and 0.02% NaN3 + 0.2M NaCl respectively, and a cocktail of protease inhibitors, pH 6.5. Sepharose 4B gel filtration was used to separate salivary mucins into V0 (Muc5b + Muc19) and Vi (Muc7). Gastric mucins were purified by density-gradient ultra-centrifugation in caesium chloride. It then underwent Sepharose 2B gel filtration to separate the V0 (Muc5ac + Muc6) from contaminating proteins. Horse saliva mucus was extracted in the same buffer as the pig gastric mucus, and also underwent Sepharose 4B gel filtration. Dot blots determined the purity and identity of the mucins. The inhibitory activity of crude and purified mucins was tested by their incubation with DU422.1 (a Durban derived strain) subtype C HIV-1 pseudovirus and infection of susceptible epithelial tumour cells (genetically modified cervical cell line i.e. TZM-BL cells that express HIV co-receptors required for infection).
Results: Crude and purified pig saliva (Muc5b, Muc19 and Muc7) as well as purified pig gastric mucins (Muc5ac+Muc6) inhibited HIV-1 in the above assay. Horse salivary mucins (Muc5b, Muc19 and Muc7) showed inhibition, but had a higher IC50 than its pig counterpart. Our current data indicate that the V0 of purified pig gastric mucins has the best inhibition of HIV-1, the IC50 of which, are lower than our human salivary data. The neutralisation capability of Muc5ac+Muc6 appears to be greater than the other mucins we have investigated.
Conclusion: Pig mucins (salivary and gastric) and horse salivary mucins inhibited HIV-1 in an in vitro pseudoviral assay, the best inhibition came from the V0 of purified pig gastric mucins Muc5ac+Muc6.
DIFFERENCE IN ARTERIAL BLOOD GAS (ABG) READINGS AS INFLUENCED BY CORE BODY TEMPERATURE
C Arnold, P H Navsaria, S Edu, S Chowdhury, A J Nicol
Trauma Center, Groote Schuur Hospital and University of Cape Town
Background: The influence that body temperature had on ABG readings was unclear at the time that the study was proposed with no clear answer found in the literature.
Methods: A prospective study of patient's that arrived at Groote Schuur Hospital's Trauma Center resuscitation area during the period of March 2015 - April 2015 was conducted. Routine ABG samples were taken and core body temperature measurements recorded as per protocol during a resuscitation. The blood gas machine then automatically produced two readings pertaining to pH, pO2 and pCO2; one reading at the default temperature setting of 37.0°C and the second reading corrected for the patient's body temperature.
Results: Of the 45 patients that were recruited, all ABG readings pertaining to pH, pO2 and pCO2, differed from the default temperature setting (37.0°C) and the patient's actual body temperature. As a general overview the patient's with corrected body temperatures of below 37.0°C (i.e. a relative hypothermia), we found that the corrected pO2 and pCO2 was actually lower than the default temperature setting and the exact opposite was true for patients with a body temperature above 37.0°C. Even though the difference between temperatures between 36.0°C and 38.0°C were not marked enough to necessarily change the management of patients. There was a more marked difference in values, the lower the body temperature got from the default temperature.
Conclusion: Body temperature correction on a blood gas machine does make a difference in pH, pO2 and pCO2 results when compared to the default setting of 37.0°C. The more marked the difference between the actual temperature and the default temperature settings the more marked the difference in pH, pO2 and pCO2 results.
SCREENING FOR HUMAN PAPILLOMAVIRUS IN HIV POSITIVE KIDNEY TRANSPLANT RECIPIENTS
J Botha1, E Muller1, G Learmonth2, H Wainwright2
1 Department of Surgery, University of Cape Town, Groote Schuur Hospital, Cape Town, South Africa
2 Department of Anatomical Pathology, University of Cape Town, Groote Schuur Hospital, Cape Town
Background & Aim: Human Papillomavirus is a common sexually transmitted infection, associated with condylomata acuminata, anogenital squamous intraepithelial lesions, and ultimately invasive squamous cell carcinoma. The first aim of the study was to determine the incidence of HPV of the anus in HIV positive kidney transplant recipients and the second aim was to determine whether the incidence of HPV-associated cancers are increased in HIV positive compared HIV negative transplant recipients.
Materials and Methods: 13 HIV positive on anti-retroviral therapy and 14 HIV negative renal transplant recipients were enrolled from the Groote Schuur Transplant unit outpatients department. Ethics approval was obtained from the UCT Ethics committee. Informed consent was obtained from all participants. To determine whether HPV and/or squamous in-situ lesions of the anus were present cytological brushings of anorectal junction were performed with a cytobrush and fixed with cytological fixative. The anoretal junction was then stained for 2 minutes with a 5% acetic acid solution, after which any abnormal white stained areas were biopsied, preserved in 10% formalin. A Papanicolaou stain was used to diagnose the cytological presence of HPV and squamous in situ lesions and was reported as per the 2001 Bethesda guidelines. Cytology and histology was correlated with clinical findings. The statistics were analysed with Stata® software.
Results: Of the 13 HIV positive patients, 2 had anal condylomata (15.4%), 7(53.8%) had cytological evidence of squamous in situ lesions and 4 (30.7%) had evidence of HPV on histology compared to 1 (7.1%), 6 (42.9%) and 0 in the control group. (Table 1).

Conclusion: An attenuated immune response to the HPV antigen in the HIV positive group is responsible for a higher incidence of squamous carcinoma in situ, HPV on histology as well as an increased incidence of anal condylomata. Because of a small sample size the difference was not statistically significant between the study and control group.
THE UTILITY OF GAMMA-GLUTAMYL TRANSFERASE AS INDICATOR OF ASYMPTOMATIC CHOLEDOCHOLITHIASIS
L Human, N C Pearce, V C Simmons
Department of Surgery, University of the Free State
Introduction: The presence of common bile duct (CBD) stones should be suspected in all patients presenting with symptomatic gallstones. Up to 20% of patients, undergoing cholecystectomy for cholelithiasis, have co-existing CBD stones. The detection and management of CBD stones pre-operatively, decreases operative risk, morbidity and mortality. Apart from Endoscopic Retrograde Cholangiography (ERC), which is reserved for therapeutic intervention, Magnetic Resonance Cholangiography (MRC) is the most reliable, pre-operative diagnostic modality for CBD stones. MRC is expensive and not universally available. The role of an isolated Gamma Glutamyl Transferase (GGT), as a predictor of CBD stones, in this setting, requires elucidation.
Aim: To evaluate GGT as a screening tool, in patients with symptomatic gallstones, in order to optimize the yield of MRC pre-operatively, for the diagnosis of CBD stones; while not compromising patient safety.
Method: A retrospective review of case files on patients that underwent MRC for possible CBD stones, before cholecystectomy, was conducted. Ethical Committee approval was obtained prior to data collection from the University of the Free State Ethics committee (ECUFS number 21/2014). All patients with symptomatic gallstones, who had a MRC, prior to cholecystectomy at Universitas Academic Hospital, from January 2012 to December 2013, had case files reviewed. Patients were excluded if they were jaundiced, had a bilirubin of > 60μmol/L, only had a post-operative MRC or a MRC for another indication, had missing clinical data, were not primarily seen at the department of Surgery of the UFS Academic Hospital Complex. Categorical data were compared using Fisher's exact test. Sensitivity, Specificity and odds ratios were calculated. P values and confidence intervals were reported. A P value of < 0.05 was considered significant.
Results: Eighty-three patients with symptomatic gallstones were identified, from a total of 239 MRCs. The male: female ratio was 1:5.4. The median age was 51 years. The median GGT was 111u/L. The median total bilirubin was 11μmol/L. Twelve of 83 patients (14%) had CBD stones on MRC. Their median age was 55 years. The median GGT was 204u/L. For patients without CBD stones, the median age was 51 years and the median GGT was 103u/L. A GGT cut-off value of 100u/L or more was more common in the group with CBD stones (92% vs. 53% respectively, p=0.0235, OR 9.8, 95% CI 1.2-80.3). For a cut-off value of 100 u/L the sensitivity was 92% (95% CI 60-100) and the specificity was 47% (95% CI 35-59).
Conclusion: Our findings suggest that a GGT of > 100 u/L in our population may be a useful pre-operative screening tool, in patients with symptomatic gallstones, prior to referral for MRC. The majority of patients with a GGT < 100 u/L may precede directly to cholecystectomy. Whether an intra-operative cholangiogram should be done in these patients, requires further study.
SPECTRUM OF COAGULATION PROFILE IN SEVERELY INJURED PATIENTS. A SUBGROUP ANALYSIS FROM THE FIRST TRIAL
S Sobnach1, M F M James2, A J Nicol1, P H Navsaria1
1 Trauma Centre & Department of Surgery, Groote Schuur Hospital and University of Cape Town
2 Department of Anaesthesia, Groote Schuur Hospital and University of Cape Town
Background: Acute Traumatic Coagulopathy (ATC) is present in up to 25% of all major trauma patients and is associated with a four-fold mortality. The diagnosis of ATC is confirmed by a 'signature trace' on the Thromboelastogram (TEG) and parameters (K-time, α-angle, MA, Ly30) in keeping with a state of hypocoagulability. The aim of this study is to describe and compare the coagulation profile of a sample of severely injured patients by two different modalities, namely standard TEG parameters and a calculated Coagulation Index (CI).
Methods: Ethics approval was obtained for this study. All patients enrolled in the FIRST (Fluids in Resuscitation of Severe Trauma) trial who had a TEG on hospital admission were included. The coagulation status was then determined using traditional TEG parameters and a calculated Coagulation Index (CI).
Results: Data from 87 patients ( Penetrating: 50, Blunt: 37) were analysed. The mean ISS and INR were 22.5 and 1.81 respectively. About a quarter of our patients were hypocoagulable on hospital admission. With the use of the CI, a smaller proportion of patients ( 37% vs. 69%) were deemed hypercoagulable (Table 1).

Conclusion: ATC is seen in about one quarter of our patients; this corroborates with previous published reports.TEG parameters and a calculated Coagulation Index (CI) result in major disparities when determining hypercoagulability.The clinical significance of hypercoagulability in trauma needs further investigation.
LIBERAL TRANSFUSION STRATEGIES STILL THE TREND IN GENERAL SURGERY
N L Allorto, M D T Smith, D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan Complex, University of Kwa-Zulu Natal.
Introduction: Blood is a limited resource in low-middle income countries such as South Africa. Transfusion is associated with complications and expense. We aimed to ascertain the opinion of a broad spectrum of surgeons regarding haemoglobin triggers and targets in order to understand the rationale and bias that drives current transfusion practice in our setting.
Methods: We formulated a questionnaire which listing operations for elective, emergency and burn surgery. Respondents including, surgeons and anaesthetists, were asked for their opinion on acceptable pre-operative and postoperative haemoglobin targets for the list of operations.
Results: One hundred and fifty questionnaires were handed out and 103 (69%) were completed. Surgeons answered the majority with only 15 by anaesthetists.
The average proposed pre-operative and post-operative haemoglobin was 9.3g/dL and 8.4g/dL respectively. The differences in haemoglobin levels are compared for different operations. The majority of respondents (60% in elective surgery, 43% in emergency surgery and 60% in burn surgery) would like pre-operative haemoglobin to be 10g/dL and above. Only 38 (40%) doctors wound accept a conservative post-operative haemoglobin of 7,5g/dL in a burns patients.
Discussion: Research suggests that a restrictive blood transfusion approach is being increasingly implemented as best practice. However despite the growing body of literature, our surgical community does not seem to accept a restrictive strategy as part of blood management principles. A shift in this practice could result in clinical benefit by reducing complications as well as cost saving in our resource constrained setting. A broader sample would be useful to determine whether this is the predominant opinion.
THE ANTI-HIV-1 ACTIVITY OF THE CERVICAL MUCUS AND ITS MUCINS
B Mhlekude1,3, S Pillay1, J Peacock1, M Tyler1, M Kgatle2, D Kahn1, C Goffinet3, A Mall1
1 Department of Surgery, University of Cape Town, Groote Schuur Hospital, South Africa
2 Department of Hepatology, University of Cape Town, Groote Schuur Hospital, South Africa
3 TWINCORE, Institute of Experimental Virology, Hannover, Germany
4 Helmholtz Centre for Infection Research, Inhoffenstrasse, Germany
Background: Sexual intercourse is the major route of HIV transmission. It has been reported in our laboratory that purified cervical mucins from normal subjects inhibit HIV-1 whilst the crude cervical mucus does not. This study aimed to confirm those findings and to further compare the inhibition of HIV-1 by mucus and mucins from normal and HIV infected subjects.
Methods: Cervical mucus samples were collected from 15 HIV negative and 8 HIV positive subjects and stirred overnight to solubilise the mucins, which were then purified by CsCl density gradient ultra-centrifugation. Purified mucins were characterized by SDS-PAGE and Western blot, and their antiviral activity was tested using a luminometric TZM-bl cell assay. Purified mucins were probed against HIV-1 pseudoviral (DU422.1) and HIV-1 replication competent (NL4.3 and YU-2) strains prior to infection of susceptible TZM-bl cells. We are currently cloning, and will be expressing and purifying his-tagged MUC5AC and MUC5B proteins in Human Embryonic Kidney 293 mammalian cells (Hek293) prior to use in an HIV pseudoviral neutralization assay.
Results: SDS-PAGE confirmed the purity of the mucins including MUC5AC and MUC5B, which were further detected by Western blot. Using an in vitro TZM-bl cell assay, we found that the crude cervical mucus and purified cervical mucins from HIV positive and HIV negative subjects inhibit all tested HIV-1 strains in a dose-dependent manner. However, the antiviral potency displayed inter-donor variability.
Conclusion: These findings suggest that both crude cervical mucus and its cluster of purified mucins inhibit HIV-1 in an in vitro assay, independent of the HIV status of the mucus donors.
EFFECTS OF CARDIOTONIC STEROIDS ON CELLULAR ARGININE TRANSPORT
M Nel and G P Candy
Department of Surgery, University of the Witwatersrand, Johannesburg
Introduction: Cardiotonic steroids have been implicated in cardiovascular and renal disease and substances such as digoxin has been used in heart failure for 2000 years. It is well known that these substances influence the ubiquitous Na+/K+-ATPase pump and hence affect sodium handling. Arginine is the precursor of the arterial vasodilator nitric oxide (NO). Arginine limits NO production and crosses cell membranes by y+ and y+L transport and it is y+L transport which appears primarily responsible for NO production. We determined the effects of ouabain and digoxin on arginine uptake into ECV304 cells.
Methods: ECV304 cells were grown to confluence, depleted of arginine and pre-incubated with or without (10-300μmol) ouabain or digoxin. Initial rate of labelled [3 H]L-arginine uptake was measured with unlabelled arginine. The selective inhibitor of y+ uptake, N- ethylmaleimide (NEM) was added to determine y+L activity, and y+ activity was calculated from the (total uptake) - ( uptake in the presence of NEM). Data was recorded in EXCEL and analysed using Graphpad Prism.
Results: Ouabain inhibited y+L transport by 25% at concentrations up to 50 μmol and 75% at 300 μmol. In contrast, ouabain had no effect on arginine uptake by y+ transport. Digoxin had mixed effects on arginine uptake. A control using a cholesterol based detergent, CHAPSO, was without effect on uptake other than a 3000 μmol concentrations.
Conclusion:
• Ouabain inhibited arginine uptake by y+L transport whereas y+ appeared unaffected, whereas digoxin had mixed effects;
• The link between Na/K-ATPase inhibition and arginine uptake is not known : whether Na+/K+ flux or Na/K-ATPase activity is linked to arginine transport or whether cardiotonic steroids directly affect arginine uptake requires further investigation;
• These are the first data suggesting cardiotonic steroids directly affect arginine uptake and suggest an alternative mechanism of action of these substances - i.e. reducing NO production.
PRESENTATION OF CHRONIC PANCREATITIS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
F Mosai, M Govender
Department of Surgery, Sefako Makgatho Health Sciences University and Dr George Mukhari Academic Hospital (DGMAH)
Introduction: Chronic pancreatitis (CP) is a disease often misdiagnosed and inappropriately managed. A Hepatopancreatobiliary (HPB) Unit was established at DGMAH on 1 November 2013 in the Department of Surgery. Patients with CP were reviewed.
Aim: To describe the presentation of patients with CP to a newly established HPB Unit at DGMAH.
Methods: All records of patients referred to the HPB Unit were retrospectively reviewed from 01 November 2013 to 31 March 2015. Patients with confirmed CP based on radiological and clinical features as described in the published South African Guidelines for diagnosis and treatment of CP were included in this study.
Results: Twenty two patients (6%) were diagnosed with CP based on radiological and clinical. All patients had a history of chronic alcohol abuse. Patients were predominantly male (95%). The age range was 34 to 81 with an average of 50.5. The index presentation was chronic pain in 7 (32%), obstructive jaundice without cholangitis in 5 (23%), obstructive jaundice with cholangitis in 1(4.5%), portal hypertension with variceal bleeding in 2(9%), acute pancreatitis in 2(9%), a massive pseudocyst in 1(4.5%), and other pathologies in 3(13.6%). Five patients (23%) were diabetic with 2 patients being newly diagnosed having presented with pain. All diabetic patients were poorly controlled and required repeated admissions for establishing an appropriate treatment regimen. Six patients had exocrine dysfunction based on history and require chronic enzyme replacement. Two patients had previous laparotomies for presumed complications of CP. Both patients had their surgery more than a decade prior to presentation to the unit. Both patients had recurrence of their previous symptoms. Portal hypertension was due to splenic vein thrombosis in 1(4.5%) and portal vein thrombosis in 2(9%). Two patients underwent a Frey procedure and biliary bypass. One patient had an operative biliary bypass due to failed endoscopic removal of a fully covered metal stent after 6 months. One patient had a laparoscopic cystgastrostomy and another had an open Roux-en-Y cystojejunostomy. Only 2 patients were employed. Three patients were considered unemployable due their age and 3 patients due to their underlying chronic pancreatitis or comorbidities. The remaining 16 patients were considered employable. One patient died from hypoglycaemia while awaiting thoracic surgery for a lung abscess.
Conclusion: CP accounts for 6% of the patients presenting to the HPB unit but the multiple complications, repeated interventions and admissions increases the unit workload and ultimately the cost.
A CLINICAL AUDIT OF ACUTE UPPER GASTROINTESTINAL BLEEDING PRESENTING TO A TERTIARY REFERRAL HOSPITAL IN THE EASTERN CAPE, SOUTH AFRICA
M M Walsh
Walter Sisulu University
Introduction: Upper gastrointestinal bleeding is a common cause of hospital admission and is associated with a significant mortality between 4 and 10%. Aetiology of upper gastrointestinal bleeding varies according to geographic region and socioeconomic status. Livingstone Hospital (LVH) is a tertiary hospital, which also serves as a district hospital to Nelson Mandela Bay Metropolitan (NMBM). There is no published data on the outcomes of our population.
Aim: The aim of this study was to assess the outcomes over 72 hour period, in patients presenting to the acute Surgical on Call unit at Livingstone Hospital (SOC).
Materials and Methods: Retrospective audit of paper records in SOC, from January 1 to December 31, 2013. All patients over 18 were included. Data included demographics (age, gender, place of residence), haemoglobin and outcomes. Endoscopy reports were individually examined to define the cause of bleeding.
Data was collected in excel. Statistical Package for Social Science (SPSS 21) was used for analysis. Parametric variables were analysed with the two-sample t-test. Nominal variables were analysed with chi-squared test (x2). P-values >0.05 was considered statistically significant. Ethical approval was granted from LVH and WSU ethics committee.
Results: A total number of 232 cases were referred during the study period. 50 patients were excluded as incorrect referral or incomplete medical data. 182 patients were included in the study of upper gastrointestinal bleeding. The gender distribution was 89 females (48.9%) and 93 males (51.1%).
The mean age was 59 years (24-93 years). The mean age of female patients was 65 years and the mean age of male patients was 54 years.
The average haemoglobin of presenting patients was 6.0g/dL (range 1.9-14.5g/dL). Tere was no difference in Hb for males and females.
The mortality rate was 16/182 (8.8%). Of the 16 patients who died prior to endoscopy, their mean Hb was 7.0g/dL. The mean for females who died was 6.6g/dL and for males was 7.4g/dL.
The Hb for patients within the NMBM was 5.9g/dL and outside the NMBM the Hb was 6.3g/dL. 166 patients had endoscopy. The most common finding was peptic ulcer disease (46.6%), followed by inflammation (12%), varices (9%), malignancy (7.8%), Mallory Weiss and other 6%. There were 31/166 (18.7%) normal scopes.

Conclusion: The mortality rate for patients presenting to SOC was in line with international reports. There was equal gender incidence for UGIB. The mean age was 59 years. 16 patients died prior to endoscopy with no formal diagnosis. The most common cause for upper gastrointestinal bleeding was peptic ulcer disease followed by inflammation.
SURGEON PERFORMED INTERVENTIONAL RADIOLOGY: A NECESSITY FOR ESTABLISHING AHPB SERVICE IN A DEVELOPING COUNTRY
M Zimba, O Y Matsevych, M Govender
Department of Surgery, Sefako Makgatho Health Sciences University and Dr George Mukhari Academic Hospital (DGMAH)
Aim: Interventional radiology is an essential part of Hepatopancreatobiliary (HPB) services. However the expertise is not widely available in a developing country. We present our experience in surgeon performed interventional procedures.
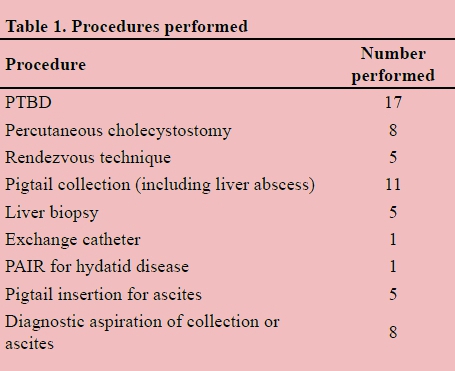
Methods: All procedures performed at Dr George Mukahri Academic Hospital were reviewed retrospectively from 01 November 2013 to 31 December 2014. A Toshiba® Model SSA-590A ultrasound was used. When required a General Electric Brivo® C-arm was used for fluoroscopy. Omnipaque™ (Iohexol) contrast was used diluted in a 1:1 ratio with water. All patients had local lignocaine injected for skin puncture and were sedated with midazolam and fentanyl titrated to effect. Patients who failed emergency endoscopic biliary drainage (ERCP) were immediately turned from prone to supine and had a percutaneous biliary drainage (PTBD) performed. If the guidewire passed into the duodenum easily a rendezvous technique was done immediately else a catheter was left in the bile duct.
Results: We performed 61 procedures on 48 patients with an age range from 27 to 83. A radiologist was present for 5 cases to assist with ultrasonography. Table 1 highlights the procedures performed. Thirteen patients had repeat procedures for dislodged or blocked catheters. Two patients had a bile leak from a dislodged catheter requiring laparoscopic washout. One patient developed a pneumothorax from insertion of a PTBD and required an intercostal drain. One patient had a non-representative liver biopsy which was repeated laparoscopically.
Conclusion: Interventional radiology is an essential component of HPB units. Surgeons may acquire the necessary skills and continue to provide HPB services.
THE USE OF UPPER ENDOSCOPY PRIOR TO CHOLECYSTECTOMY IS BENEFICIAL
G Green, A Noorbhai, B Sartorius, T E Madiba
Departments of Surgery and Biostatistics, University of KwaZulu-Natal, Durban, South Africa
Introduction: Surgical intervention for symptomatic cholelithiasis, without upper endoscopy, may result in coexisting gastrointestinal pathology being missed.
Purpose: This study established the prevalence of upper gastrointestinal pathology in patients with confirmed cholelithiasis and assessed the predictive value of symptoms these symptoms.
Methods: Study setting: A tertiary training hospital in Durban Study design: Retrospective chart review of patients with ultrasonography-proven symptomatic cholelithiasis. Patients underwent upper endoscopy prior to a planned elective cholecystectomy. Symptoms of cholelithiasis were analysed to predict positive endoscopic findings. Data collected included demographics, clinical presentation and physical examination. Ultrasound findings were extracted from ultrasound report cards and endoscopic findings from gastrointestinal unit reports. Surgical intervention and outcome were extracted from patient files and theatre records.
Study endpoints: Upper gastrointestinal pathology and change in management Ethical approval: UKZN BREC (Ref.: BE130/14).
Results: All 106 patients underwent upper endoscopy prior to cholecystectomy of whom 101 were female. Mean age was 45.68 (+ 14.51). Findings on examination were normal abdominal examination (4), right upper quadrant pain (58), Murphy's sign (3), epigastric pain (35) and right iliac fossa pain (1). Endoscopic findings were normal endoscopy (37), gastric inflammation (58), hiatus hernia (21), oesophagitis (10) and oesophageal candidiasis (2). Nausea had a PPV of 69% and abdominal pain had a PPV of 66%. A triad of abdominal pain, nausea and vomiting was strongly associated with a higher chance of additional gastrointestinal pathology. Cholecystectomy was laparoscopic (66) and open (40). There were no deaths.
Conclusion: Symptoms of abdominal pain, right upper quadrant pain, nausea and vomiting with symptomatic cholelithiasis were strongly suggestive of additional upper gastro-intestinal pathology. Upper endoscopy is valuable in excluding other upper gastro-intestinal pathology. We recommend that all patients should undergo an upper endoscopy prior to a planned laparoscopic cholecystectomy.
THE PATTERN OF GASTRIC CANCERS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
T Sumbana, M Z Koto
Department of Surgery, Sefako Makgatho Health Sciences University and Dr George Mukhari Academic Hospital (DGMAH)
Background: Gastric cancer have different pattern in terms of anatomical sites, histopathological subtypes.
This is influenced by geographic area and socioeconomic status. In developing areas of low socioeconomic status distal cancers are more common as opposed to developed areas where proximal cancers predominate. However there are reports of predominance of proximal cancers in certain developing rural areas of low socioeconomic status. In terms of histology adenocarcinoma is the most common histological pattern but the next most common histology differs with geographic region.
Aims: The aim is to report on the patterns of gastric cancers which are seen at DGMAH .The reason being that every area has its own pattern sometimes not following known trends reported in the literature.
Methods: This was a retrospective study where histological confirmed gastric cancer seen at DGMAH between January 2007 and August 2014 were reviewed. The gastroscopy reports where used to identify patients and determine the anatomical sites of the cancers. The hospital files where used to determine socioeconomic status based on financial income and for patients demographics. The NHLS database was used to identify histological subtypes.
Findings: 80 patients were identified for the study. Demographics: 56,25% males and 43,75% females, 43,75% were above 60yrs of age, 17,50% were less than 40years,38,75% between 40 and 60 years, all patients were classified as low socioeconomic status. Anatomical sites 82, 50% were distal cancers; 16, 25% were proximal and 1, 25% involve the whole stomach. The histological subtypes in the order of occurrence was adenocarcinoma 83,75%; GIST at 6,25%; Kaposi sarcoma 2,50%; lymphoma 2,50%; NETS 2,50%; MALT lymphoma 1,25%; small cell carcinoma 1,25%.
Conclusion: The anatomical sites followed reported trends where distal cancers predominate in developing areas. The most common histology is still adenocarcinoma as reported, but what is different is that GIST are second followed by Kaposi sarcoma; lymphoma; NETS all occurring in similar proportion these is different from what has been reported. Even though these are a small sample to draw conclusion from but it is evidence that in terms of histology following adenocarcinoma they may differ with geographic area.
CLINICOPATHOLOGIC SPECTRUM OF SMALL BOWEL OBSTRUCTION AND MANAGEMENT OUTCOMES: EXPERIENCE FROM THE PIETERMARITZBURG ACADEMIC HOSPITAL COMPLEX
M Mthethwa, C Aldous, T E Madiba
Department of Surgery, University of KwaZulu-Natal and the Pietermaritzburg Academic Hospital Complex
Background: Delay in the surgical management of patients with small bowel obstruction results in increased incidence of complications and mortality.
Purpose: To evaluate the patterns of small bowel obstruction in a busy regional hospital in terms of the aetiology, clinical presentation and impact on outcome.
Methods:
• Study setting: Tertiary Teaching Hospitals in the Pietermaritzburg Academic Hospital Complex
• Study design: Prospective, observational, cross-sectional study conducted between 01 August 2013 and 31 July 2014.
• Patients: All patients presenting to Edendale and Grey's hospitals with small bowel obstruction were included in the study. Structured interviews were conducted. Demographics, clinical details, investigations, operative findings, in-hospital progress and outcomes were all documented.
• Study endpoints: Clinical presentation and treatment outcome
• Ethical Approval: UKZN BREC; Ref.: BE207/13
Results: There were 156 patients enrolled with a mean age of 40.7 (range 13-86) years. The M:F ratio was 1.4:1. The main causes of obstruction were adhesions (99; 63%) and hernia (31; 19.9%). Non-operative management was feasible in 58 (37%) patients and was successful in 72%. In 114 operations, small bowel ischaemia was present in 47 patients (41%) and small bowel resection was undertaken in 57 of 114 operated patients (50%). Patients presenting late had a higher small bowel resection rate (odds 1.29 vs 0.42), odds ratio 3.06 (95% CI 1.21 - 7.75, p=0.015) higher admission to intensive care units (odds 0.45 vs 0.23), odds ratio 1.98 (95% CI 068 to 5.78, p=0,206). This group also had longer hospital stay (9.3 vs 4.8 days), multiple re-laparotomies odds ratio 2.73 (95% CI 0.86 to 8.65, p=0.079) and higher complication rates, odds ratio 4.79 (95% CI 1.9 to 12.02, p=0.0004). The mortality rate was 5.8%, all from the delayed presenting group.
Conclusion: The main cause of small bowel obstruction presenting to our academic hospitals are adhesions followed by hernias. Most patients present late and this has a major impact on morbidity, need for re-laparotomies, duration of ICU and hospital stay, and mortality.
AN AUDIT OF PENETRATING NECK TRAUMA IN PIETERMARITZBURG
A Madsen, G L Laing, J L Bruce, G V Oosthuizen, D L Clarke
Introduction: This study reviews and validates the practice of selective non-operative management (SNOM) of penetrating neck injury (PNI) in a South African trauma service and reviews the impact new imaging modalities have had on the management of this injury.
Methodology: This study was performed within the Pietermaritzburg Metropolitan Trauma Service, in the city of Pietermaritzburg, Kwazulu-Natal, South Africa. A prospectively maintained trauma registry was retrospectively interrogated. All patients with PNI treated over a 46-month period were included within the study.
Results: A total of 510 patients were included in the study. There were 452 stab wounds (SW) and 58 gunshot wounds (GSW). A total of 202 patients sustained isolated PNI, the remaining 308 patients sustained trauma to at least one additional anatomical region. An airway injury was identified in 29 (6%) patients; a pharyngo-oesophageal injury in 41 (8%) patients and a vascular injury in 86 (17%) patients. Associated injuries included, three penetrating cardiac injuries (PCI) and 146 patients with haemo-pneumothoraces. Of the total cohort, 387 patients (76%) underwent CT Angiography (CTA), of which 70 (18%) demonstrated a vascular injury. Formal catheter directed angiogram (CDA) was performed on 16 patients with positive CTA but confirmed injury in only half of these patients. Of 212 patients (42%) who underwent water-soluble contrast swallow (WS-swallow), an injury was demonstrated in 29 (14%) cases. A total of 402 (79%) patients were successfully managed conservatively for PNI and 108 (21%) surgically or by endovascular intervention. Only four (1%) patients failed a trial of SNOM and required surgery. The in-hospital mortality rate was 2%. No deaths could be attributed to a failure of SNOM.
Conclusion: SNOM of PNI is a safe and appropriate management strategy. The conservative management of isolated pharyngeal injuries is well supported by our findings but the role of conservative treatment of oesophageal injuries needs to be further defined. The SNOM of small nondestructive upper airway injuries seems to be a safe strategy, while destructive airway injuries require formal repair. Imaging merely for proximity, is associated with a low yield. CTA has a significant false positive rate and good clinical assessment remains the cornerstone of management.
AN AUDIT OF THE BURDEN OF PAEDIATRIC TRAUMA TREATED BY THE PIETERMARITZBURG METROPOLITAN TRAUMA SERVICE
V Manchev, G L Laing, J I Bruce, D L Clarke
Introduction: The Pietermaritzburg Metropolitan Trauma Service (PMTS) has run a systematic Quality Improvement (QI) program since 2006. A key component included the development and implementation of an effective surveillance system in the form of an Electronic Surgical Registry (ESR). This study utilised data from the ESR to review the incidence, spectrum and outcome of paediatric trauma in Pietermaritzburg, South Africa.
Methodology: The ESR was reviewed and all cases of pediatric trauma managed the 1st January 2012 and 30th July 2014 were retrieved for analysis.
Results: During the study period 1041 paediatric trauma patients were managed by the PMTS. This equates to an average monthly admission rate of 36 paediatric patients. The average age was 10.9 years (SD 5,4). There were 724 (69.5%) male and 317 (30.5%) female patients. The mechanism of injury (MOI) was blunt trauma in 753 (72.3%) patients and penetrating trauma in 170 (16.3%) patients. The remainder of the MOIs are recorded in tables 1-5. Pedestrian vehicle collisions (PVC) accounted for 20 % of cases and Motor Vehicle Collisions (MVC)'s for a further 10%. Falling off the back of a moving vehicle refers to patients who fell off the back of a 'flat-bed' truck. This accounted for a further 4% of cases. 88 patients sustained a bite-injury (78 snake bites, 7 dog bites and 3 human bites). Intentional trauma accounted for 282 patients (25%) and self inflicted for 14 (1.2%) cases. An overview of weapons used in the cases of assault is provided in Table 5, while radiological investigations utilised during diagnostic workup is detailed in Table 6. A total of 315 patients required a total of 1179 operative interventions which is an average of 3.7 operative interventions per patient. There were 90 patients admitted to the intensive care unit (ICU) and 51 required high dependency unit (HDU) admission. There were 17 deaths, equating to a in-hospital mortality rate of 1.7 %. During the study period a total of 172 children (less than 17 years of age) died on the scene of an incident. There were 35 road traffic related deaths, 26 suicides by hanging, 27 deaths from blunt assault and 23 deaths from penetrating assault. The overall mortality rate for paediatric trauma was 18%.
Conclusion: The ESR has proven to be an effective surveillance system and has enabled the accurate quantification of the burden of paediatric trauma in Pietermaritzburg. This has improved our understanding of the mechanisms and patterns of injury and has identified a high incidence of intentional and penetrating trauma as well as road traffic collisions. This data can be used to
MORTALITY PREDICTION IN A REGIONAL SOUTH AFRICAN BURNS SERVICE USING FIRST WORLD COMPOSITE MODELS
M T D Smith, B Sartorius, N L Allorto, D L Clarke
University of Kwa-Zulu Natal
Background: Thermal injury is often devastating and survival of significant injuries is dependent on costly resources. Many die regardless of resource availability because the injury itself may not be survivable.
Many composite scores have been formulated to predict the outcome of patients with burns. 8 models were found to be methodologically sound. These scores are: the modified Baux score, the Abbreviated Burn Severity index, Total Burn Surface index, Coste et al. model, Ryan et al. model, McGwin et al. model, Galerias et al. model and the Belgian Outcome of Burn injury score (BOBI).
These scores have not been validated in Southern Africa and could possibly be used as quality improvement tools, a means of identifying high risk patients or even to guide resource distribution.
Aim: to validate first world predictive models in a regional south African burn service.
Method: This study is a retrospective chart review of all consecutive burns admissions to Edendale hospital (EDH) over 6 months (May 2013-October 2013). Delayed admissions were excluded. Descriptive statistics and regression analysis were used to evaluate the categorical data. Patient data were scored against the composite models. Discrimination analysis was used to find optimal break points for our sample and validated against the same sample.
Results: 173 patients were included in the study (mean 15 years). The mean %TBSA was 9% (0.25-100). 57% of the patients were male. The actual mortality rate was 7.5% (13 patients). A logistical regression analysis revealed that a patient with full thickness burns was more than 10 times more likely to die (odds ratio 10,7 CI) and inhalation injury increased the risk of death by almost 84 times (see figure1).
2 models were rejected due to lack of data and 2 were found to be unsuitable. The remaining tests lacked sensitivity but were highly specific. New optimal cut-off points were lower than the primary scores.
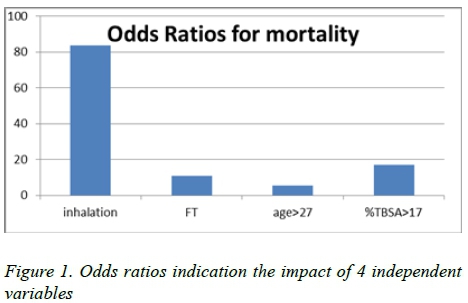
Discussion: First world models can be used in a developing setting if new sample-specific cut-off values are used. Scores with high sensitivities (ABSI) may be useful in recognising patients needing a higher level of care. More specific scores (Coste and BOBI).may aid in scarce resource allocation . Accurate scores are useful as quality improvement tools.
Conclusion: The BOBI score with a modified threshold value is most suitable as it fits all the required needs and is simple to use.
AUDITING SURGICAL RESIDENTS OPERATIVE ACTIVITY IN A BUSY LEVEL 1 TRAUMA UNIT IN SOUTH AFRICA
R Spence1,2, E Zargaran3, P Navsaria1,4, A Nicol14, S Sobnach1,4
1 University of Cape Town, Cape Town, South Africa
2 Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston
3 General Surgery, University of British Columbia, Vancouver, Canada
4 Trauma Surgery, Groote Schuur Hospital, Cape Town, South Africa
Introduction: In an era where surgical outcomes have been shown to differ by provider, the following study describes prospectively audited surgical activity for general surgery residents rotating through Groote Schuur Hospitals Level 1 trauma unit (GSH).
Aim: To describe the risk-adjusted surgical outcomes following major trauma surgery performed by surgical trainees.
Materials & Methods: During a 6 month period July 2014-December 2014 a prospective cohort study at GSH trauma unit was conducted. Admission, operative and discharge summaries generated on the recently implemented electronic Trauma Health Register (eTHR) as part of a multifaceted trauma quality improvement program, were reviewed. A descriptive analysis of 4 surgical trainees' and 1 rotating relief surgeons' operative activity and the outcomes thereof was performed. All major operative cases performed by one of the 4 surgical trainees or a rotating relief surgeon allocated to 'trauma cutting,' were included. Reoperations were excluded. Primary outcomes audited were in-hospital morbidity and mortality. Secondary outcomes included length of stay, admission to ICU, incidence of unplanned reoperation and readmission. Factors considered in the American College of Surgeons' Trauma Quality Improvement Program were analyzed to assess comparability between operative cohorts and risk-adjusted outcomes. The univariate relation between each predictor variable considered, including the operating surgeon, and mortality as well as morbidity is tested using χ2 or Fisher's exact tests for categorical variables and the t test or Mann-Whitney U test for continuous variables. Significance is set at p<0,05.
Results: During the 6 month period the surgical registrars performed 445 operations. After Relook laparotomies and minor procedures were excluded, 336 major trauma operations were included. The most common operation performed was exploratory laparotomy for penetrating injury to the abdomen (124 cases) followed by sub-xiphoid window to exclude penetrating cardiac injuries (51 cases). Residents were only supervised in 28.5 % of cases. Each cohort considered was comparable after reviewing patients' initial vital signs on admission, age, gender, race, transfer status, mechanism of injury, referral institution, AIS severity by individual body region and individual comorbidities. Overall in-hospital morbidity and mortality rates were 24% and 3% respectively. The operating surgeon was an independent risk factor for morbidity but not mortality.
Conclusion: Risk-adjusted surgical outcomes per surgical trainee are feasible in a busy level 1 trauma unit for benchmarking and training purposes.
IMPLEMENTATION OF A STRUCTURED SURGICAL QUALITY IMPROVEMENT PROGRAM IN A LEVEL 1 TRAUMA UNIT IN SOUTH AFRICA USING EMERGING MOBILE-HEALTH TECHNOLOGY
R Spence1,2, E Zargaran3, P Navsaria1,4, D Kahn1, A Nicol1,4, D J de Villiers1,4
1 University of Cape Town, Cape Town, South Africa
2 Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston
3 General Surgery, University of British Columbia, Vancouver, Canada
4 Trauma Surgery, Groote Schuur Hospital, Cape Town, South Africa
Introduction: The global injury burden is high in the developing world where over 90% of deaths occur. A primary source of this discrepancy is the existence of organized systems of trauma care in developed countries.
Aim: To use the newly implemented electronic trauma health registry as a stimulus for developing quality improvement initiatives in a referral trauma unit in South Africa.
Materials & Methods: In response to the Guidelines for trauma quality improvement programs by the WHO and the IATSIC, our study group hypothesized the recently implemented eTHR system is a useful tool with which to develop a trauma quality improvement program in such a setting, addressing;
• Injury surveillance, medical record keeping and trauma registry development
• Injury severity calculations
• Tracking of predefined audit filters, ICU admissions, complications and missed injuries
• Preventable death, morbidity and mortality review process.
This prospective cohort study describes the first review of the clinician-entered eTHR over a 1 year period from April 2014-March 2015 approved by the University of Cape Town's Human Ethics Research Department.
Results: The eTHR generated injury surveillance, process of care data and medical records for 12 654 patients seen over the 12 month period (22% female, 78% male). Field completion rates were significantly higher on eTHR than previous paper records. ISS, RTS, KTS and Ps scores were calculated for every patient. The majority of injuries were intentionally inflicted (53.5%) and penetrating (54.3%), most commonly sustained on the street (24.5%) and referred by ambulance directly from the scene (36.0%) with a median injury to arrival time of 4.1hrs. Orthopaedics was the most frequently consulted subspeciality (3234 consultations) with a median consultation waiting time of 29 mins. 876 Operations were performed by the general surgery residents, supervised in only 24.2% of cases. Median waiting time to theatre was 4.25hrs. Exploratory laparotomy for penetrating trauma was the most frequently performed operation (392 cases). The WHO surgical checklist was performed in 99.1% of cases. 52 Potentially-preventable deaths, 143 ICU admissions, 44 missed injuries and 466 complications captured by eTHR were discussed at monthly panel meetings.
Conclusion: A novel tablet-based tool, eTHR, provides the necessary platform for a trauma quality improvement program in middle-low resource settings.
PROPHYLACTIC ANTIBIOTICS FOR TUBE THORACOSTOMY ARE NOT INDICATED IN THE DEVELOPING WORLD SETTING
V Y Kong, D L Clarke
University of Kwa Zulu Natal, Pietermaritzburg Metropolitan Trauma Service
Introduction: Prophylactic antibiotics for tube thoracostomy (TT) for the prevention of post traumatic empyema (PTE) remain controversial. Literature specifically focusing on the developing world setting is limited.
Materials and Methods: A retrospective study was conducted over a four-year period on patients managed with TT alone in which prophylactic antibiotics is not utilised. We documented the actual incidence of PTE in high volume trauma service in a South Africa.
Results: A total of 1002 patients who had TT in the trauma room were eligible for inclusion. Ninety-one per cent (912/1002) were males and the mean age for all patients was 24 years (SD 7). Seventy-five per cent (755/1002) sustained penetrating trauma (PT), while the remaining 25% (247/1002) sustained blunt trauma (BT). Six hundred and twenty patients (62%) sustained HTXs and the remaining 382 patients (38%) had PTXs. Of the 1002 patients who underwent TT, 15 (1.5 %, 95%CI: 0.8-2.5%) developed PTE. The incidence of empyema in those with PT was 1.9% (14/755) and 0.4% (1/247) for BT. This difference was not statistically significant (p=0.135). All 15 patients who developed PTE were males, with a mean age of 31 years (SD 6). All 15 patients had HTX as the initial thoracic pathology. This difference was highly statistically significant when compared to PTX (p=0.001). The mean length of hospital stay was 11 days (SD 7). There were no mortalities in these patients.
Conclusions: In our setting where prophylactic antibiotics are not routinely used, the actual incidence of PTE in our population is extremely low. In the absence of further definitive evidence to support its use, routine prophylactic antibiotics for TT is difficult to justify in a developing world setting at present.
BLOOD ALCOHOL CONCENTRATION LEVELS CORRELATES WITH INJURY SEVERITY
A El-Shiere, M A Noorbhai, T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban
Introduction: Alcohol consumption leads to violence and poor judgement and the resultant trauma is the leading cause of emergency visits. In South Africa, alcohol related emergency visits can be as high as 57%.
Aim: The purpose of this study was to assess the prevalence of positive BAC levels in Durban, and to correlate it with injury severity and length of hospital stay.
Methods:
• Study setting: King Edward VIII Hospital, a tertiary teaching hospital in Durban.
• Study design: Blood alcohol concentration (BAC) levels were prospectively collected and analysed in consecutive trauma patients over a 3-month period (December 2014 to February 2015). Pearson chi-square test, Wilcoxon rank sum and student t-test were used to determine the significance of BAC in alcohol positive and negative patients. A p-value of <0.05 was considered statistically significant.
• Study endpoints: Blood alcohol concentration level was correlated with Injury Severity Score (ISS), mechanism of injury, length of stay, and in-hospital mortality.
• Ethical approval: BREC UKZN Ethics Approval Reference - BE254/142
Results: One hundred patients (average age 30 years) were analysed during the study period of whom 88 were male. The prevalence of positive BAC levels was 47%. The mean BAC level among the alcohol positive patients was 0.146g/dL. BAC positive patients had significantly higher ISS scores (p=0.0004). Interpersonal violence related injuries seen in 83 patients (83%) of which 42 (51%) had positive BAC levels. There was a significant difference in the length of stay between BAC positive and negative groups (p < 0.001).
Conclusion: BAC prevalence is high in the trauma population. Positive BAC levels are associated with higher ISS scores and longer length of hospital stays. BAC levels should be routinely collected at all trauma units. We recommend further reductions of the legal limit.
CLINICO-MICROBIOLOGICAL STUDY ON BACTERIAL INFECTION OF SNAKEBITE WOUNDS AT NGWELEZANA HOSPITAL, AREA 3, KWAZULU-NATAL
M Wagene, M Naidoo
Ngwelezana Hospital, KwaZulu-Natal, South Africa
Introduction: Patients can experience serious local and systemic septic complications secondary to snakebite wounds. Our aim was to determine the bacteria involved in wound infections secondary to snakebite and to determine antibiotic susceptibility of these pathogens in patients presenting to our surgery department.
Materials and Methods: A prospective audit was undertaken over a four month period in Ngwelezana Hospital. Records were analysed of patients that required surgical debridement for extensive skin and soft tissue necrosis.
At the time of debridement, tissue samples of necrotic or infected tissue were sent for bacteriological analysis as standard of care. Pathology results were analysed.
Results: A total of 164 patients were admitted to hospital for the management of a snakebite of whom 57 required surgical debridement and 42 were included in the final analysis.
Forty eight organisms were cultured from the 42 cases, 32 had a single organism cultured, 8 had 2 organisms cultured and 2 showed no growth despite there being objective wound infection. No patients had more than 2 organisms isolated.
Thirty five (73%) of the organisms were gram negative enterobacteriaceae, the most frequent being Morganella morganii and Proteus species. Thirteen (27%) were Enterococcus faecalis. No anaerobic organisms were grown.
Gram negative enterobacteriaceae showed 31% sensitivity to ampicillin; 40% sensitivity to amoxicillin-clavulanic acid; 34% sensitivity of cefuroxime; 97% sensitivity to ceftriaxone; and 100% sensitivity to ciprofloxacin, gentamycin and amikacin. Enterococcus faecalis was 92% sensitive to amoxicillin; 92% sensitive to amoxicillin-clavulanic acid, 100% sensitive to ciprofloxacin and 100% resistant to erythromycin.
Conclusion: Good surgical debridement and post operative wound care are the most important aspects of managing patients with sustantial necrosis and objective wound infection secondary to snakebite after the acute phase.
There appears to be a role for antibiotics in the managenent of these patients,however prior to this audit there was no recent local data to guide these antibiotic choices.
In order not to drive further resistance we recommend withholding antibiotics until results of approriate sensitivity testing are available.
In cases when empiric antibiotics are deemed necessary, based on this data, we would recommend ciprofloxacin as the antibiotic of choice.
THE EVENTUAL OUTCOME OF PATIENTS WHO HAD LOWER LIMB AMPUTATIONS DUE TO PERIPHERAL VASCULAR DISEASE
C de Klerk, G du Plessis, J J Fourie, A O'Neill, S J A Smit
Department of Surgery, University Free State, Bloemfontein, South Africa
Aim: Our aim was to determine the eventual outcome of persons who underwent amputations of a lower limb due to peripheral vascular disease (PVD). The purpose of the study was to test the conventional wisdom that the majority of lower limb amputees can look forward to a functional and a productive lifestyle.
Methods: Prospective data collection of a retrospective cohort study group was performed. The study period was from January 2008 to December 2011 and the data was obtained from Pelonomi Tertiary hospital in Bloemfontein. Included in the study were patients who had PVD induced lower limb amputations i.e. either below knee amputation (BKA) or above knee amputation (AKA). The target population's demographic and contact information were collected from the Meditech database. Patients with contact information were invited to a telephonic interview with either the person or surviving family members (if applicable). Mortality was also determined using the Department of Home Affairs database. Ethics Committee approval for the study was granted.
Results: Of the study population (n=224) only 119 had contact information and 49 were interviewed. Information on mortality also came from the Department of Home Affairs database. The mean age was 64 years and male representation (58%) was slightly higher. AKAs and BKAs were 47% and 53% respectively. Of the 158 people used to determine mortality, 113 patients (72%) were dead within 2 years after the amputation. Causes of death determined during the interviews (n=31) were 71% PVD related. The cumulative mortality showed that 16% demised within a month and 48% within 1 year post-amputation. Amongst the living amputees 50% became unemployed permanently, 78% were in wheelchairs, 11% were on crutches and only 11% walked with a prosthesis.
Conclusions: Losing a leg due to PVD is indicative of a very poor prognosis. According to our study, only 28% of lower limb amputees survive 2 years after the operation. The majority of them died due to pre-existing and ongoing morbid vascular disease. Amongst the living amputees, the picture is as grim. Restoration to ideal mobility was achieved in a minority of cases.
STAGE IV COLORECTAL CANCER IN RESOURCE-LIMITED SETTINGS. 12 YEAR EXPERIENCE FROM THE KWAZULU-NATAL ACADEMIC HOSPITALS
S Kader and T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban
Background: There is paucity of data on Stage IV colorectal cancer (CRC) in South Africa. Our hypothesis was that the proportion of Stage IV CRC was higher in South Africa compared to international norms.
Aim: To establish the hospital prevalence of Stage IV CRC in the KwaZulu-Natal (KZN) Province of South Africa and to document outcome in our resource-limited setting.
Methods:
• Ethical Approval: Biomedical Research Ethics Committee (UKZN): E198/04
• Setting: Colorectal Unit in a tertiary hospital
• Design: Retrospective analysis of an on-going prospectively collected CRC database. The study comprises patients with stage IV CRC enrolled between 2000 and 2012. Parameters analysed were demographics, clinical presentation, primary tumour site, site of metastasis, treatment and follow-up.
• Study endpoints: Clinicopathologic spectrum, follow-up and outcome
Results: Of 1449 patients with CRC, 322 (22%) had metastatic disease, comprising Africans (106), Indians (129), Coloureds (21)and Whites (67) which accounted for 21%, 22%, 33% and 22% of the respective CRC cohorts. Mean
age was 57.3 + 14.4 years and the median ages for Africans, Indians, Coloureds and Whites were 50, 59, 63 and 67 years respectively. There were 63 (20%), 81(25%), and 174 (54%) proximal colon, distal colon and rectal tumours respectively. Common target organs for metastases were liver (242), lung (51), peritoneum (26), omentum (15), and ovaries (10). Treatment of the primary tumour was resection in 128 patients (40%). All patients except 10 received chemotherapy. Liver resections were performed only in 9 patients and chemo-embolisation in one patient. Median follow-up was 11 months and median survival was 7 months.
Conclusions: Metastatic disease accounts for 22% in our setting. African patients tend to be younger. Site distribution of primary tumour is similar to the general cohort of patients with CRC and to general norms. Metastatic resection rate and chemo-embolisation are infrequently offered.
PREDICTORS OF OCCURRENCE OF OMENTAL DEPOSITS IN PATIENTS WITH GASTRIC ADENOCARCINOMA UNDERGOING GASTRECTOMY: A HISTOPATHOLOGICAL AUDIT
O Tobiko1,4, C Jann-Kruger1,4, J B L Kiluba1,4, M Hale2,4,5, T E Luvhengo1,3,4
1 Departments of Surgery, Charlotte Maxeke Johannesburg Academic Hospital
2 Anatomical Pathology, Charlotte Maxeke Johannesburg Academic Hospital
3 Charlotte Maxeke Johannesburg Academic Hospital
4 University of the Witwatersrand
5 National Health Laboratory Services of SA
Introduction: The aim during curative resection of gastric adenocarcinoma is to obtain R0 margin and appropriate lymphadenectomy. Greater omentectomy is added to eliminate micrometastases. Knowledge of lymphatic anatomy and lymph node count in the greater omentum is scanty. Classification of lymphadenectomy is based histopathological lymph node count which may be overinflated following greater omentectomhy. Omentum-preserving gastrectomy (OPG) does not increase the risk peritoneal relapse or decrease overall survival.
Aim: To determine if histopathologically assessment of greater omentum is performed routinely following gastrectomy for gastric adenocarcinoma; and to determine factors associated with findings of cancer deposits.
Methods: An audit of histopathology records of adult patients diagnosed with gastric malignancies at Academic Hospitals of University of the Witwatersrand Circuit. Data retrieved included patients' demography, tumour site, tumour histology and subtypes, type and indication for gastrectomy; and occurrence of omental deposits.
Results: Records of 325 patients with confirmed gastric malignancies were found. Their male to female ratio of patients was 192:133. Majority (76.6%) were adenocarcinomas 76.6% and average age was 60.2 years (range: 24-102). Twenty (8.4%) of adenocarcinoma were less than 40 years old. Gastrectomy was performed in 22.9% (57/249), 70.2 (40/57) had subtotal and 29.8% (17/57) total gastrectomy. The number of lymph node harvested ranged from x-r (average). Report on greater omentum was recorded in
14.0% (8/57) of gastrectomies of which 37.5% (3/8) had
cancer deposits. All three cases had stage IV disease either T3 or T4 diffuse type cancer.
Discussion: Early gastric carcinoma is rare and majority of the cancers are irresectable. Pathologists rarely evaluate or report on findings of greater omentum assessment. Omental deposits appear to be associated with T3 and T4 diffuse type adenocarcinoma.
PREVALENCE OF FACTORS INFLUENCING RECURRENCE AND / OR METASTASIS IN DERMATOFIBROSARCOMA PROTUBERANS
A Y Benneh1,3, P S Kay1,3, M J Hale2,3,4, J B L Kiluba1,3, T E Luvhengo1,3
1 Departments of Surgery, Charlotte Maxeke Johannesburg Academic Hospital
2 Anatomical Pathology, Charlotte Maxeke Johannesburg Academic Hospital
3 University of the Witwatersrand
4 National Health Laboratory Service
Introduction: Dermatofibrosarcoma protuberans (DFSP) is a slow growing tumour with limited metastatic potential. The fibrosarcomatous (FS) variant has increased propensity for local and distant recurrence. We conducted the study to determine the prevalence of factors influencing recurrence and/or metastasis.
Methods: A retrospective review was undertaken on records of patients with DFSPs diagnosed following core needle, incision or excision biopsy. Data retrieved included demography, tumour site, size, biopsy type, deep resection margin, CD34 stain result, mitotic count and presence of necrosis.
Results: Records of 51 patients whose male to female ratio was 22:29. All were blacks with a median age of 40.0 years of age. 66.7 percent were in the trunk and the average size was 8.1 cm (range: 1.5cm-19.5cm). Wide excision was performed in 78.4% (40/51) and resection margin was adequate in
5.7% (2/35). FS-DFSP was reported in 23.5% (12/51) and 34.3% (12/35) post excision. Around 54.8% of classical DFSPs were in males whereas 66.7% of patients diagnosed with FS-DFSP were females. Only 9.7% of classical DFSPs involved limbs whereas 33.3% of FS-DFSPs were in extremities. Mitotic count of 5 and above per 10 high power field was reported in 29.8% (8/31) of classical and 74.9% (9/12) of FS-DFSPs.
Discussion: DFSP is a disease of young adults and majority are larger than 5 cm at presentation. FS-DFSP variant of DFSP is more frequent in extremities of black female South Africans around 40 years old. Adequate deep resection margin is rarely achieved.














