Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.2 Cape Town jun. 2016
ABSTRACTS
Abstracts of the 42nd Annual Meeting Surgical Research Society of Southern Africa
Hosted by the Department of Surgery, L7, 3rd Floor Main Building, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban. 26 - 27 June 2014
Oral Presenations
COST OF TREATING PARTIAL THICKNESS BURN WOUND IN SOUTH AFRICA
A Muganza
Director Burn Unit, Chris Hani Baragwanath Academic Hospital, Wits University
Introduction: Burns in South Africa account for significant morbidity and mortality. The exact cost of treating thermal injury has never been fully explored.
Aims: The primary aim of this study was to compare the healing time and cost of partial thickness burn wound treated with skin substitutes to standard treatment.
Methods: A prospective randomised controlled study was undertaken.
Results: 96 patients were randomized of which 47 were treated by standard therapy and 49 by advanced therapy (skin Substitutes). The overall mean TBSA was 20 % (15-25) and the median age 13.0 (2 to 29). The mean cost per healed burn was higher with skin substitutes (R 85,780 versus 101,826). The length of stay was the most significant driver across all groups accounting for between 70 and 80 percent of all costs associated with management.
Conclusion: The choice of any dressing for partial thickness burns requires evidence based approach to reduce length of stay to be considered cost effective.
POST-OPERATIVE ANALGESIA FOR GENERAL SURGICAL PATIENTS AT NGWELEZANA HOSPITAL
M Wagener, T Nightingale, A Deytrikh, M Naidoo, M Fell
Ngwelezana Hospital, Kwazulunatal, South Africa
Introduction: Pain relief following operations is crucial for recovery, the prevention of post-operative complications and patient satisfaction. Prescribing adequate analgesia is difficult because the doctor has to be able to predict the amount of pain the patient will experience. Prescriptions should provide enough cover for background pain and breakthrough pain with doses that will minimalize the chance for patients to experience medication side effects.
Research Question: We aimed to examine the current prescribing pattern by doctors for surgical patients. We hoped to be able to design a useful aide de memoir to assist doctors with future prescribing.
Materials and Methods: A prospective study was undertaken over a 1-week period in the Ngwelezana Hospital operating theatres. The prescription charts for all general surgical patients receiving operations were examined immediately after their operations, before being sent to the ward. Patient demographics, type of analgesic and prescriber details were recorded. Results were compared against the post-operative pain guidelines compiled by the South African Society of Anaesthesiologists. Additionally, patients were approached 24 hours post-operatively and asked to rate the amount of pain they were experiencing on a visual analogue scale (VAS).
Results: 22 patients were operated with a mean age of 17.2 years and a wide range of pathologies and subsequent procedures. Analgesic medication was prescribed for 20 (91%) of patients. The most commonly prescribed analgesic was IM morphine in 17 (77%) patients and paracetemol was prescribed in 11 (50%) patients. Anti-emetics were never prescribed. Pain scores on the VAS scale were recorded in 17 patients with a mean score of 6.
A doctors teaching session and poster was designed to help prompt post-operative prescribed in conjunction with the national guidance and pharmaceutical advice (see Figure 1). Posters were displayed in the operating theatres and recovery areas. Examination of the prescription charts of a further 15 patients was undertaken after these changes had been implemented. Analgesia was prescribed for all 15 patients and morphine was always prescribed in conjunction with another form of analgesia with anti-emetics in 10 (66%) patients. The mean pain score on the VAS scale was 4 for the 15 patients.
Conclusions: Post-operative analgesic prescriptions for surgical patients were haphazard. Simple interventions were shown to align prescribing patterns according to national guidance. Further work should be aimed at consolidating these improvements.
HIGH-THROUGHPUT ASSAY TO IDENTIFY LEAD FRACTIONS OF SENECIO SERRATULOIDES USED TO TREAT DEEP PARTIAL THICKNESS WOUNDS
A N Gould, C B Penny1, T Snyman2, G P Candy
1 Department of Surgery, Internal Medicine, University of the Witwatersrand
2 Chemical Pathology, NHLS, Johannesburg
Introduction: The traditional remedy plant, Senecio serratuloides accelerates wound healing in deep partial thickness wounds by increasing cellular proliferation in the epidermis. The rapid healing of skin graft donor sites, deep partial thickness burns and traumatic wounds has obvious benefits. Identifying active target lead chemicals using an animal model is not feasible, given the number of compounds and possible combinations needed to be screened. A possibility is to use a tissue culture which will allow rapid and reproducible screening of active plant fractions.
Aim: To establish and screen plant fractions using a keratinocyte culture based assay to identify fractions which promote cell proliferation.
Methods: Plant material (5g each) were extracted with acidified, neutral or basic aqueous solutions for 24 hours and then sonicated for one hour. The extracts were filtered and fractionated on preconditioned hydrophobic-lipophilic solid phase extraction cartridges and eluted (4 fractions per extract) as per the cartridge manufacturer's instruction. The resultant fractions were diluted serially from 1: 80 to 1:10240. Each fraction was tested on confluent keratinocytes grown in 96 well culture plates using a resazurin dye colorimetric assay and measuring cellular proliferation by the extent of dye reduction after 4 hours. The plates were read on a UV-VIS scanning spectrophotometer with results reported as percentage of dye reduction. Controls used Epidermal Growth Factor (5ng EGF/ml) and vehicle alone (phosphate buffered saline).
Results: The 2 final elutions of the basic and neutral extracts were shown to increase the proliferative response with the percentage reductions shown in the table.
Table Reduction of dye by keratinocytes using aqueous plant extracts.
Compared to vehicle *: p<0.05; *** p<0.0001; compared to EGF : § p<0.05; §§§ p<0.0001

Conclusion: The culture based assay identified active fractions which can be further fractionated to identify lead compounds. The solid phase cartridge extraction of the active fractions can easily be reproduced and scaled up for further analysis of the active fractions.
THE UTILITY OF UPPER GASTROINTESTINAL ENDOSCOPY IN HIV POSITIVE PATIENTS D A Viljoen, S J A Smit
Department of Surgery, University of the Free State, Bloemfontein, South Africa
Introduction: The majority of studies dealing with upper gastrointestinal (GI) pathology in HIV patients are from the developed world. The utility of routine random biopsies, also remains to be determined.
Aim: We aimed to prospectively describe and analyse a cohort of HIV positive patients, with symptoms warranting referral for upper GI endoscopy, at the UFS academic hospitals. In addition, we aimed to evaluate the utility of random biopsy sampling at endoscopy.
Method: Ethical approval was obtained for a cross-sectional study. Data was collected prospectively between February and December 2012. Two random biopsies were taken in the gastric antrum and 2 in the distal oesophagus respectively. Histology and microbiology analysis was requested. Continuous data was described using medians (interquartile range). Sensitivity and specificity of symptom groups and CD4 cut off values for positive endoscopic findings, were calculated. Categorical data were compared using Fisher's exact test. Cohen's kappa coefficient was used as a measure of inter-rater agreement. A p-value of <0.05 was considered significant.
Results: 36 Patients were recruited, 27 females and 9 males (3:1). Median age was 39.5 (33.5-48.5). Median CD4 count was 193.5 (84-320). There was a trend towards more positive findings in the group with CD4 counts of <200 (p=0.06). Symptoms were categorised into oesophageal (yield 77%), upper GI bleed (yield 88%) and other (including dyspepsia) (yield 14%). Oesophageal symptoms were associated with a high yield of positive endoscopic findings, when compared to other symptoms (p=0.007, sensitivity 64%, specificity 83%). Similarly, when comparing upper GI bleed symptoms to other symptoms a positive finding was significantly more likely (p=0.0015). Gastritis was reported on histology in 22. There was no correlation between the symptom of dyspepsia and the histological finding of gastritis (κ=0.072, 95% CI -0.297 to 0.441, p=1.0). Furthermore, there was no correlation between CD4 count (cut-off value 200) and histologically reported gastritis (κ=0.172, 95% CI -0.137 to 0.482, p=0.43). The endoscopic impression of "gastritis", as reported, however correlated well with the histological finding of gastritis (κ=0.6, 95% CI 0.298 to 0.91, p=0.0014). A CD4 count of <200 was not associated with the finding of oesophageal thrush (p=0.69), but was associated with oesophageal ulcers (p=0.02). There was no difference in the occurrence of histological gastritis in patients on Highly Active Anti-retroviral Therapy (HAART), as compared to untreated patients (p=0.43).
Conclusion: While oesophageal symptoms and symptoms of upper GI haemorrhage, appear to be associated with a greater endoscopic yield, absence of oesophageal symptoms does not exclude oesophageal pathology. A CD4 count of <200 may be associated with a greater yield in symptomatic patients, but apart from a significant association with oesophageal ulcers, did not correlate well with other endoscopic or histologic findings. The endoscopic finding of "gastritis" correlated well with histology (as reported), although the finding of histological gastritis does not correlate with symptoms of dyspepsia. The high prevalence of reported gastritis, remains of uncertain significance, in the absence of a control group. We conclude that endoscopy is indicated in HIV positive patients, based on standard indications, as for HIV negative patients. We cannot currently recommend the performance of routine, random biopsies.
ACUTE APPENDICITIS IN THE PUBLIC AND PRIVATE SECTORS IN CAPE TOWN,SOUTH AFRICA
E Yang, D Kahn, C Cook
Oregon Health & Science University (USA) University of Cape Town
Background: South Africa has a low incidence of acute appendicitis, but poor outcomes compared to developed countries. There is a lack of research on appendicitis in the private sector. This study aims to compare appendicitis in public and private hospitals to fully understand the nature of appendicitis in South Africa.
Research question: How do patient characteristics, disease presentation, rupture rates, and clinical outcomes differ between public and private sector patients in Cape Town, South Africa?
Methods: A prospective cohort study was conducted among 2 public and 3 private hospitals in the Cape Town metropole, from September 2013 to March 2014. All adults undergoing appendicectomy for presumed acute appendicitis during the study period were eligible for inclusion. Enrolment continued until sufficient numbers were obtained to adequately power both arms of the study. Patients undergoing incidental appendicectomy, or those treated conservatively, were excluded. Patients were enrolled while hospitalised for appendicectomy by the principal investigator. Hospital records were reviewed, including histology results and theatre records. Interviews were held with patients during hospitalisation and again four weeks after discharge, with follow up interviews held monthly until normal function was attained. Using a level of significance (α) of 0.05, and power of 0.80, a sample size of 59 patients in each cohort was calculated using published rupture rates in South African public hospitals (47.3%) and in the US (21.7%) as estimates for the public and private sector cohorts, respectively. Statistical analysis was performed using STATA 12. Continuous variables were compared using the t-test for independent samples or Wilcoxon rank sum test for nonparametric data. Associations between categorical variables were conducted using either chi square analyses or Fisher's exact test, as appropriate. Ethics approval was obtained by the Faculty of Health Sciences Human Research Ethics Committee at the University of Cape Town (319/2013).
Results: There were 134 patients enrolled, with 73 in the public and 61 in the private sector. Education and employment were higher among private sector patients. Public sector patients had a higher rupture rate (30.6% vs 13.2%, p=0.023). Times to presentation were not statistically different between the two groups. Public sector patients had longer hospital stays (5.3 vs 2.9 days, p=0.036) and longer return to work times (23.0 vs 12.1 days, p<0.0001). Although complication rates were similar, complications in public hospitals were more severe.
Discussion: South African patients undergoing appendicectomy for acute appendicitis in the public sector have higher perforation rates, worse complications and more severe disease than patients in the private sector. This disparity likely stems from a combination of social and economic differences that characterise the patient populations that are served in each sector. Hospital stays and recovery at home are longer for public sector patients, even when controlling for disease severity and surgical approach. As a whole, patients with perforation had delayed coming to hospital longer than patients with non-perforated appendicitis, although the reasons underlying these delays are unclear.

A QUALITY OF LIFE ASSESSMENT TOOL FOR DYSPHAGIA
L Ferndale, C Aldous, S R T Thomson
University of Kwazulu-Natal
Background: Dysphagia is a common symptom of patients presenting to a surgical or gastroenterology department and quality of life is adversely affected by it. The impact of dysphagia on quality of life has been studied, but largely in the first-world setting. The quality of life tools available were largely developed and validated in developed countries. There is a need for quality of life tools developed and validated in our clinical setting to assess impact of dysphagia on QOL on our population and the effectiveness of our treatment regimens.
Methods: We compiled a dysphagia quality of life questionnaire with questions relevant to our local population and asked patients presenting with dysphagia to complete the questionnaire together with the short form 36 and dysphagia score questionnaires. The latter two are international validated questionnaires and were used in order to validate the newly designed questionnaire. In addition we collected demographic data, including age, sex and level of education. The results of the three questionnaires were then compared using Pearson's correlation.
Results: A total of 100 patients were entered into the study. There were 62males and 38 females and the average age was 59 years. The overall level of education was found to be low. Patients showed an overall poor quality of life when completing the questionnaires and this finding did not differ between the different questionnaires. There was good correlation between the newly compiled questionnaire and the two validated questionnaires. Respondents showed better compliance when completing the newly designed questionnaire compared to the international questionnaires. The results of the newly designed questionnaire were not influenced by level of education.
Conclusion: Dysphagia does impact negatively on the quality of life of individuals. The newly designed questionnaire with locally relevant questions can be used to assess the impact of dysphagia on the quality of life of affected individuals. This quality of life tool can then also be used to assess the impact of different treatment regimens on the quality of life of these patients.
FLOW VELOCITY MEASUREMENT IN HAEMO-DIALYSIS ACCESS USING 4D MRI: A PILOT STUDY OF FEASIBILITY
J Downs,S Jermy, D Kahn, E M Meintjes, T Franz
University of Cape Town
Introduction: Treatment of renal failure while awaiting transplant requires vascular access. Unfortunately, thistis access comes with both procedural complications as well as significant failure rates. In order to optimize the performance of vascular access, information about the AVF or AVG itself, as well as the haemodynamics of the flow through the access is required. Once this information is gathered, it would then be used for computer modelling techniques and computational flow dynamics. Previously, the imaging data required to perform the flow dynamic calculations has been provided by MRI using contrast, with its own set of complications. However, new MRI software that provides imaging data as well as flow in terms of time without using contrast could be used to streamline this data gathering process and provide accurate data for modelling.
Research Question: can 4D MRI be used to scan small vessels of the upper arm to give accurate flow velocities to provide adequate data for computational flow dynamics?
Methods: This was a prospective pilot study. Data (flow velocities through native vessels and grafts, as well as wall shear stresses) is collected using 4D flow MRI. 3 control cases (with no history of vascular illness or surgery of any kind to the right upper arm) were selected. They underwent contrast free MRI of the right upper arm with a Siemens Magnetom Symphony 1.5 T MRI using a variety of scan protocols, including a 2D flow sequence (axial) and 4D flow sequence(saggittal), both phase contrast Magnetic Resonance Angiography. Images were collected with cardiac gating to reflect where in the cardiac cycle information was gathered. Images were then processed using Supertool in Matlab and flow velocities at predetermined points on the brachial artery and cephalic vein were calculated. As this was a descriptive pilot study, no statistical analysis of data was performed. This fulfils the expected outcome, that the scan technique is feasible to provide the required data for further study.
Ethics: approved by the UCT Human Research Ethics Committee.
Results: mean velocity over a cardiac cycle in the distal brachial artery was measured as 8,8cm/s, 4,5cm/s and 6,2cm/s in 3 volunteers. In the same volunteers, total flow volume per cardiac cycle was 0,6ml, 1,0ml and 0,4ml respectively. Cephalic vein velocities were 4,3cm/s and 13cm/s in the volunteers.
Conclusion: this technique provides good imaging and quantitative information about small vessel haemodynamics. This technique will be used for further scanning of upper arm haemodialysis access for use in computational modelling.
DECISIONS IN 'EARLY ONSET' BLOUNT'S DISEASE D M Thompson, P M Mare and M M Barciela
Paediatric Orthopaedic unit, Greys Hospital, Pietermaritzburg
Introduction: Blount's disease (or Tibia vara) is a common condition seen in our unit. Classically it is divided into early onset (starting before 4) and late onset (starting after 8).We have carried out an audit of our patients and present all 'early onset' patients.
A tibial and fibula osteotomy has been the gold standard in treatment of 'early onset' disease, but recurrence rates of 50% are common.
We have used osteotomy alone, osteotomy in combination with growth retardation methods (eight plates and staples) and eight plates used alone, as well as the 3 in 1 procedure (medial joint elevation, lateral epiphyseodesis and osteotomy), while reserving ring external fixation methods for the severe or recurrent cases.
Research Questions:
1. What is our recurrence rate with tibia/fibula osteotomy alone?
2. What factors make recurrence likely?
3. What is the place of guided growth with eight plates?
Material: We followed up all patients with Blount's disease seen over the last 4 years. Late onset case were excluded, and in 4 cases we could not trace the initial X-rays. This left us with 100 extremities with initial X-rays and followed until the result could be seen (7 years to at least 6 months). The ages ranged from 2 to 11.
Results: We had 6 extremities treated with eight plates alone. 58 extremities treated with osteotomy alone (25 recurrences), 32 treated with osteotomy and eight plates (16 recurrences) and 5 treated with primary 3 in 1 procedures (no recurrence).
Age, obesity, high medial physeal slope (MPS), instability and lateral tibial physeal widening were important factors in determining recurrence.
We believe that eight plates do have a role in early onset Blount's.
PATIENT FOLLOW UP AFTER BURN INJURY ADMISSION TO A REGIONAL BURN SERVICE IN KWAZULU NATAL D A Links & N L Allorto
Department of Surgery Pietermaritzburg Metropolitan, University of KwaZulu Natal
Introduction: All burns which are deeper that superficial dermal heal with scarring. This may have consequences in terms of cosmesis, function, employment and quality of life for the healed burn patient. We aimed to evaluate patient scars post management of burn injuries at our institution and to assess the quality of life of this group.
Methods: This is a prospective descriptive pilot project. All patients presenting to Edendale hospital burns clinic over 3 months from January to March 2014 were reviewed. Patients included in the study were those post skin grafting or deep dermal burn wound spontaneous healing. Data collected included time post skin grafting, anatomical area grafted and the use of emollients and sunscreen. The Vancouver scar assessment scale was used to asses the extent of scarring and the EQ-5D (EuroQol Group) quality of life questionnaire was used to assess the quality of life in this group.
Results: Over the three months 120 patients were seen in the Edendale Burns Clinic. Sixteen patients (13%) were included in the study. A slight predominance of males (56%) were seen with an average age of 18 years. Fourteen patients (87.5%) were grafted and two (12.5%) by secondary healing of deep dermal burns. Clinic review occurred on average 15 weeks (range 7 - 27 weeks) post burn injury. One patient had no post burn scarring. The grafted area scored on average 5 (range 2 - 10) on the Vancouver scar scale and the donor site scored on average 2 (range 1- 7) on the same scale . Ten out of 16 patients (63%) use sunscressn and emoillients. Nine patients, six of whom where male, answered quality of life questionnaires with a general health score of 8 (range 4 - 10). Seven patients are employed and two are receiving disability grants.
Conclusion: The Vancouver scar scale is an easy tool to use in assessment of scars post burns. Donor sites teld to have better scars than the grafted burn wound. We should focus on education of patients in regards to scar management. The quality of life seems to very good in this group of burn survivors.
THE GAP BETWEEN AVAILABILITY OF REFERRAL CRITERIA FOR TRANSFER OF BURNS PATIENTS, AND THE IMPLEMENTATION OF TRANSFER
J.Govindasmy, M Naidoo, C Aldous, P Barker
Greys Hospital Complex, PMB Metropolitan and School of Clinical Medicine, UKZN; Headquarters, International Committee of the Red Cross, Geneva
Introduction: In South Africa, the burn-injury patient will present to their nearest hospital in their local area. This means that most times, it is up to the treating doctor to decide if the patient needs referral to a higher level facility. All burn units have referral criteria as guidelines for doctors, to assist them in making that decision. However, it is frequently found that patients are only transferred days or weeks after their admission, despite the fact that they meet the referral criteria. This paper looks at the reasons why patients are not transferred timeously, despite the clear guidelines for referral.
Method: A number of district hospitals in the Pietermaritzberg and Northern Kwa-zulu Natal areas, will be visited at random occasions to assess their admitted burn patients. If these patients meet the referral criteria, they will be included in the study. The study will include a minimum of 15 patients. The following categories will be examined, to ascertain the most common causes for delayed transfer:
• Awareness of the referral criteria by district doctors
• Time of discussion with referral hospital, in relation to the patient's admission
• Response of the referral hospital to the discussion
• Reason for delay in transfer
Discussion: The identification and correction of significant factors related to delayed transfer will assist in decreasing the time gap between a patient seeking medical assistance, and actually receiving the treatment that they require to ensure the best possible recovery for them. For the health-system, this will also ensure that resources are used as economically as possible. The cost of a poorly managed burn patient impacts not just that patient and the healthcare system, but spirals out to negatively impact future patients. The author hopes that by identifying the major reasons for delayed referral, despite clear referral guidelines, future interventions can be specifically focused to address those issues.
IS PLATELET DECLINE A PREDICTOR OF POOR OUTCOME IN SEVERELY BURNT PATIENTS? A FIVE YEAR RETROSPECTIVE STUDY
I Bahemia, R Moore, A Muganza,
Surgery, University of Witwatersrand and CH-Baragwanath Hospital, Johannesburg
Introduction: It is well established that thrombocytopaenia is common among ICU patients, irrespective of the nature of their illness, be it medical or surgical. Of critical importance, is the associated increased duration of stay, morbidity and mortality. The percentage decline has been shown to be a significant predictor of mortality rather than the absolute platelet counts. Minimal research has been conducted focusing on the burn patient even though a drop in platelet count among burn victims was first documented as far back as 1944 by MacDonald et al. The aim of this study is to determine if changes in platelet count after a severe burn injury can be used as a predictor of outcome.
Methodology: A retrospective descriptive study analyzing demographic, haematological (platelet count) and microbiological data of Burns ICU (Intensive Care Unit) patients admitted over a 5 year period to Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa. All Adult Patients admitted with Acute Burns to the ICU between the 1st of January of 2009 and the 31st of December 2013 were included. Exclusion criteria were 1) Patients stepped up from the general burns ward to ICU during their admission. 2) Patients that died within 4 days of admission. 3) Patients whose data were not accessible or incomplete due to clerical errors. 4) Patients admitted with thrombocytopaenia. The Percentage of Platelet decline (PPD) was calculated as follows: 100- [(platelet count on day X/platelet count on admission) x 100)]. Thrombocytopaenia was defined as a platelet count under 100 x 109/L.
Results: Out of 388 patients admitted during our time frame, 350 were included. The sample consisted of 214 males and 136 females. The mean %TBSA burn was 29.7%, the majority being from flame burns. The mortality rate was 43%. By Mid-April, only a preliminary analysis had been performed. On day 3 post admission, 29.5% of patients had thrombocytopaenia. Thrombocytopaenia was present in 40% of non-survivors and in 20.5% of survivors. The average PPD on day 3 in the sample was 38%. Among non-survivors, the PPD on day 3 was on average 47 %. In comparison, survivors had an average PPD of 28% on day 3. PPD on day 10 among non-survivors was 14% and -66% in non-survivors. A PPD of more than 50% was present in 94% of non-survivors and 77% of survivors respectively. Further analysis is currently being performed to estimate the statistical significance of the above results.
Conclusion: Thrombocytopaenia is common among severely burnt victims. The nadir of platelet count is usually between day 3 and day 4. By day 10, platelet count of survivors would have increased to above the admission value. Our data, even though still at a preliminary stage, suggest that PPD might have some prognostic value in predicting mortality in burn victims. A high PPD on day 3 should prompt the search for conditions that will lead to impending clinical deterioration such as sepsis.
ROLE OF APPLICATION OF SKIN SUBSTITUTES ON PARTIAL THICKNESS BURNS
R Sheikh, R.Moore, A Muganza
Department of Plastic and Reconstructive Surgery, and Surgery, University Of Witwatersrand and CH-Baragwanath Hospital, Johannesburg
Introduction: Skin substitutes have been used in various units for treatment of partial thickness burns with varying results. This has been done under theatre conditions thereby putting the patient under metabolic stress of a general aneasthetia and increasing cost of care of these patients. We describe a technique that allows use of skin substitutes as dressing out of theatre hence cutting cost of care of partial thickness burns in our local set up.
Aims: To assess the duration of hospital stay in patients with partial thickness burns.
Materials and Methods: A retrospective review of patients admitted with superficial partial thickness burns to Burns Unit at Chris Hani Baragwanath Academic Hospital was done between November 2013 and April 2014. Patients with partial thickness burns were included in the study. Skin substitute was applied within 72 hours of injury. This was done in the ward using standard analgesia and chlorhexidine wash. Skin substitute was secured to burn wound with Micropore Tape and Steristrips. This was dressed with Acticoat.
Exposure was done at day three and day six. If skin substitute had taken, dry dressings were continued. If wounds were still wet Acticoat dressings were continued. Any infected wounds were dressed with 0.25% acetic acid dressings.
Results: Twenty two patients were reviewed over the six month period. Mean age of 29.7 (11-55 years old). Male to female ratio 18:4. Average Total Body Surface Area of 19.1% (2-44%). Average hospital stay of 10.5 days (3-36 days). 54.5% had hot water burns, 9.1% paraffin stove burns, 1.4% flash electrical burns, 27.2% flames explosion burns and 4.1% had gas explosion burns. We had one medical related mortality. We had a 7.5% TBSA failure rate.
Conclusions: In appropriately selected cases, our use of skin substitute outside theatre set up shows healing time similar to conventional treatment methods.
ARE PREDICTIVE MORTALITY SCORES VALID IN A REGIONAL SOUTH AFRICAN BURNS SERVICE?
M T D Smith, N L Allorto, DL Clarke
University of KwaZulu-Natal
Background: Thermal injury is often devastating and large injuries have a high risk of morbidity and mortality. In order for such patients to have a chance at survival, numerous costly resources need to be utilised. Furthermore, there is a subset of patients with significant injuries, as well as inhalation injuries who will die regardless of resource availability. This is because the injury itself is not survivable. Many scores have been formulated in order to predict which injuries are survivable and which are not. These scores may be used to guide the allocation of resources to those for whom survival is more likely.
In a systematic review by Hussain et al, 45 such models were scrutinized. Only 8 of these models were based on sound methodology. These scores have not been validated in Southern Africa.
Research Question: Are existing mortality prediction models for thermal injury valid in a regional South African burns service.
Method: A retrospective chart review was done for all the admissions to the Edendale burns unit from May to July 2013. All admissions within 72 hours of thermal injury were included in the study. Delayed presentations were excluded. All patients were scored against 3 mortality predictive scores and the results tabulated in an excel spread sheet. The actual mortality rate was compared to the rate predicted by each model. No ethical approval was necessary as data was drawn from existing patient charts.
Results: 142 Patients were admitted during this time and 49 were excluded as they were admitted more than 72 hours post burn. The average age was 16 years old and the average %TBSA was 9%. The actual mortality rate was 7.5%. Each patient was scored against 3 predictive mortality scores, namely, the Abbreviated Burn Severity Index, Modified Baux Score and the Belgian Outcome of Burn Injury Score. The Modified Baux score was found to under predict mortality risk by not accounting for the presence of full thickness burns. It was however, 100% specific as a predictor of mortality.
Conclusion: The actual mortality rate was higher than that predicted by all scores (approximately 7%). This may be due to scarce resources or other independent variables. These scores need to be validated prospectively in a larger sample.
EMPIRIC ANTIMICROBIAL USE IN A REGIONAL BURN SERVICE
A Zoepke1, N L Allorto2
1 University of KwaZulu Natal
2 Department of Surgery Pietermaritzburg Metropolitan
Introduction: Sepsis remains the most common complication in burn-injured patients. Treatment includes source control and appropriate empiric antimicrobials until identification of the offending organism. Inappropriate therapy may be associated with increased mortality. Antimicrobial stewardship is important and empiric choice should be based on local pathogen susceptibility profiles. We aimed to investigate infectious complications in a single burn service and determine whether our empiric therapy is appropriate.
Methods: All patients who exhibit clinical signs of infection are screened by chest X-ray, urine and blood culture, wound swab and line is removed before commencement of systemic antimicrobials. Clinical signs, investigations done and empiric therapy commenced are documented on a sepsis form. We reviewed all patients in the burn high care unit of Edendale Hospital who had sepsis forms completed in January to March 2014 as a pilot study. Data, which included that from the sepsis form as well as microbiology results, was collated using Microsoft Excel.
Results: Twelve patients were included in this pilot. All were children with an average age of 2 years, 9 months (range 9 to 59 months). Augmentin was the empiric choice in 9 patients, addition of Gentamycin in 7, Piperacillin-tazobactam only in 2, Clindamycin only in 1 and Meropenem in 1. Positive cultures were found in nine patients (more than one organism was grown in four patients) and cultures were negative in three patients. Organisms included Acinetobacter (4), Pseudomonas Aueriginosa (3), Ecoli (2), Enterococcus faecalis (2), Staphylococcus (2) and Klebsiella pneumonia(1). Source of organism was the wound in 6, blood in 4 and intravenous catheters in 3. Empiric therapy covered the 7 out 10 organisms grown, excluding Acinetobacter.
Discussion: Empiric choice of therapy is appropriate in the majority of patients who did have systemic sepsis. Diagnosis of sepsis was incorrect in a quarter of patients and is likely to have been the inflammatory response, notoriously difficult to differentiate from sepsis in the burn patient. Acinetobacter is considered to be only a coloniser in our unit and is largely not treated. Pseudomonas aeuriginosa is our most common culprit and typically described in burn units. The burn wound is expected to be the most common source of sepsis in a burn-injured patient.
Conclusion: Tailoring empiric antibiotic therapy according to local pathogens and sensitivity patterns is an important component in burn care and we seem to be getting it right in this pilot study. We plan to expand the period of data collection for a more representative sample.
CRUSH INJURY - DOES ADMISSION CREATINE KINASE OR SERUM CREATININE LEVELS PREDICT ACUTE KIDNEY INJURY REQUIRING DIALYSIS IN PATIENTS WITH SJAMBOK INJURY? THE EXPERIENCE AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
S R Motilall, M Modisane, M Msingapantsi, N Kumar, M Z Koto
Trauma Unit, Department of Surgery, Dr George Mukhari Academic Hospital, University of Limpopo - Medunsa
Introduction: Crush Injury following assault with a sjambok is a common occurrence in the South African population. Acute kidney injury with associated multiple organ failure increases mortality and morbidity. Creatine kinase (CK) has been suggested to be a predictor of acute kidney injury with a paucity of data on an elevated serum creatinine (sCr) as a predictor of acute kidney injury in crush injury.
Aim: To determine the role of an abnormal creatine kinase in the first 24 hours of admission or abnormal serum creatinine on admission in predicting acute kidney injury requiring dialysis at an academic hospital.
Methods: Retrospective review of data collected from March 2013 to February 2014 in all patients with a clinical suspicion of crush injury. Patients were resuscitated according to ATLS principles. Fluid diuresis predominantly with normal saline was initiated. CK, urea and electrolytes (U&E) were part of initial blood screen. The U&E was repeated within 24 hours and repeated again if deranged. If the initial CK was < 1000 IU/L it was repeated within 24 hours. Crush injury was defined as a CK > 1000 IU/L within 24 hours of admission. sCr > 104umol/l was defined as abnormal. Dialysis was instituted as per standard protocols. Data collected included age, gender, CK, volume of fluid infused, urine output (U/O), dialysis and ICU admission. P values < 0.05 were significant.
Results: Sixty one patients presented with a clinical suspicion of crush injury. Seven patients were excluded because of incomplete data. Three patients were excluded as the CK remained below 1000. The remaining 51 patients were all male. Average age was 27 years (range 17 - 64 years). Average CK over the first 24 hours was 2889 (range 1149 - 9417 IU/L). Average crystalloid administered in 24 hours was 5500ml and urine output over the first 24 hours averaged 3240 ml. Fourteen patients had an abnormal creatinine with an average of 134 (range 105 -176umol/l). Two patients (3%) required dialysis. They also developed pulmonary oedema requiring ICU admission. In these patients CK and sCr were 1997/149 umol/l and 4024/176 umol/l respectively. Only 2/14 (14%) patients with abnormal sCr on admission progressed to dialysis. None of the patients with a normal admission sCr required dialysis.
Conclusion: Elevated CK within the first 24 hours in a patient with crush injury cannot be used as a reliable predictor of patients who would proceed to acute kidney injury requiring dialysis. Of those patients diagnosed with a crush injury, an elevated sCr on admission is also unable to predict the need for dialysis. However we can comment that patients with a normal sCr on admission with appropriate resuscitation will not require dialysis for crush injury.
CLINICAL AUDIT OF FIFTY CASES OF PENETRATING CHEST TRAUMA PRESENTING TO A DISTRICT LEVEL HOSPITAL REQUIRING OPERATIVE INTERVENTION
J H Klopper, A van der Walt, H Molabe, J J Venter
Background: GF Jooste District Hospital (GFJDH) was situated in the heart of the Cape Flats, an area notorious for gang warfare and a high rate of interpersonal violence. This research looked into the operative findings of 50 cases of penetrating chest trauma requiring operative intervention in an eight months period in 2011.
Methods: Fifty consecutive cases where identified from the hospital theatre records and these files were retrospectively audited for a range of parameters pertaining to these patients.
Results: Patients arrived at the hospital by both ambulance and private transport. The patient group comprised 48 male and only two female patients, all fairly young adults. Eighteen patients underwent midline sternotomies, with 19 left and eight right-sided thoracotomies. Six concomitant laparotomies were performed. A total of 12 subxiphoid windows were created, six of which were converted to a midline sternotomy. The majority of cardiac injuries were to the left ventricle, comprising 13 cases. Five patients had three major injuries. A single patient died.
Discussion: GFJDH served a valuable role in the acute management of penetrating cardiac injuries and results of the impact of the closure of the hospital is awaited. A variety of injuries presented to the hospital.
IS THERE A ROLL FOR TRANEXAMIC ACID AT GROOTE SCHUUR HOSPITAL TRAUMA CENTER IN MASSIVELY HEMORRHAGING PATIENTS? A FEASIBILITY STUDY
B. Thurston, S Chowdhury, A J Nicol, S Edu, P H Navsaria
Trauma Center, Groote Schuur Hospital and University of Cape Town
Background: The CRASH-2 trial demonstrated that early administration of tranexamic acid can reduce mortality from trauma associated bleeding by up to 32%. This finding is particularly pertinent in countries where access to blood products that ameliorate coagulopathy are not widely available. Tranexamic acid needs to be administered as early as possible, ideally within one hour of injury and certainly within three hours as beyond this it increases mortality.
Aim: This study explored whether, in our trauma network based in a middle income country, patients arrived in hospital soon enough after injury for tranexamic acid administration to be effective and safe.
Methods: SRC approved audit. We undertook a prospective cohort study of 50 consecutive patients admitted to our trauma unit. Inclusion criteria were as for the CRASH-2 study: BP<90 and/or HR >110 and injuries suggestive of a risk of haemorrhage. Patients with isolated head injuries were excluded. The mechanisms of injury, time since injury and any reason for delay were recorded.
Results: Thirteen (26%) patients presented soon enough for tranexamic acid treatment to be safe. Of these, only 3 presented within the first hour. Eleven (22%) patients had a documented time of injury greater than 3 hours. We were unsure of the time of injury of 26 patients, but based on local referral patterns were assumed to be > 4 hours.
Conclusions: The majority of our bleeding trauma patients do not present within a time frame that administering tranexamic therapy is appropriate. Of those that do, most would benefit from even earlier commencement of therapy. This study suggests that rather than incorporation into in-hospital protocols, tranexamic acid should be added to the pre-hospital arena if maximum benefit is to be obtained.
A RETROSPECTIVE INVESTIGATION OF THE ADMISSION INR LEVELS AND ASSOCIATED OUTCOMES AT THE INKOSI ALBERT LUTHULI CENTRAL HOSPITAL LEVEL 1 TRAUMA UNIT A Noorbhai, MH Cassimjee, D J J Muckart
Background: Haemorrhagic shock is a leading cause of early traumatic deaths. Acute coagulopathy can occur on admission to trauma unit and is said to be associated with worse outcomes. Haemorrhagic shock is a leading cause of early death after trauma. This relationship to early mortality that is ascribed to haemorrhage remains consistent regardless of mechanism of injury. Haemorrhage and haemorrhagic shock are increasingly amenable to interventions that result in reductions in morbidity and mortality.
Aim/Research question: The study aims to assess the incidence of the Coagulopathy of Trauma at the Inkosi Albert Luthuli Central Hospital (IALCH) level 1 trauma unit, and further correlate it with outcome. The admission INR levels are correlated with Injury Severity Scores (ISS), lactate, PT, PTT and in-hospital mortality.
Methodology: Post graduate and BioMedical Research Ethics approval was obtained. A retrospective analysis of all patients admitted to the Level 1 trauma unit during the period 2007 - 2011 was performed. The variables obtained were: INR, Coagulation profile, lactate, base deficit, clinical parameters and in-hospital mortality. The data was analysed using the SPSS statistics program.
Results: There were 1000 patients of whom 752 were male. The number of patients admitted directly from the accident scene was 261 (26%), whilst the remaining 74% where inhospital transfers. The mechanism of injury varied with 60.5% due to motor vehicle collisions, 10.3% due to blunt trauma and 26.6% due to penetrating trauma The INR levels were obtained in 939 patients; 772 were alive. The median INR value among live patients was 1.18 and 1.35 among dead patients. The mean INR value among live patients was 1.33 and 1.92 among dead patients. There was an increased mortality amongst patients with abnormal INR levels which was statistically significant (p value < 0.001). The mortality rate of patients with abnormal INR levels directly from scene was 41% versus 25% of in-hospital transfers.
Conclusion: Raised admission INR levels are associated with worse outcomes. There is a direct correlation between INR and ISS levels. Acute coagulopathy of trauma has been shown to occur before the onset of therapeutic interventions. Early recognition of acute coagulopathy will help reduce patient morbidity and mortality.
ASSOCIATION OF ORGAN INJURY WITH EVISCERATION IN STAB WOUNDS OF THE ANTERIOR ABDOMEN: THE CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL EXPERIENCE
M. Mauser, BI Monzon, R. Pretorius, F. Plani
Trauma Directorate, Chris Hani Baragwanath Academic Hospital
Department of Surgery, University of the Witwatersrand, Johannesburg
Background: Both routine laparotomy and clinical observation by serial abdominal examination are used in the treatment of patients with anterior abdominal stab wounds with bowel or omental evisceration. There is an ongoing debate about the safety of non-operative management of patients with evisceration and anterior stab wounds. The objective was to determine incidence of associated injuries requiring surgical repair in patients with omental and/or visceral evisceration.
Method: A retrospective audit of prospectively collected data of the operative findings of 65 patients who presented with bowel or omental evisceration and were treated at Chris Hani Baragwanath Academic Hospital (CHBAH) between April 2010 and March 2013. All patients on record were analysed. Variables included the organ eviscerated, location of the evisceration and the intra-abdominal injuries that were found during the exploratory laparotomy. Injury severity was categorized using the penetrating abdominal trauma index (PATI). The main objective was to determine incidence of organ injury and the need for surgical repair related to omental or visceral evisceration. A results were considered significant when p < 0.5.
Results: A total of 44,655 patients were treated in the study period, of those 8,687 were major trauma cases and 685 underwent exploratory laparotomy. Of those, 65 patients were treated with an exploratory laparotomy for an anterior abdominal stab wound with omental or organ evisceration. Thirty-eight patients (58%) had eviscerated organs, twenty-seven patients (42%) had eviscerated omentum. Overall 58 patients (89,2%) had a therapeutic laparotomy with intraabdominal injury that required repair. There was only one non- therapeutic laparotomy in the group of patients with bowel evisceration and 6 non-therapeutic/negative laparotomies in the group of omental evisceration.
Conclusion: 97,4% of the patients with organ evisceration and 77,8 % of patients with omental evisceration had intra-abdominal injuries that required surgical repair. It is our opinion that any form of evisceration should prompt operative intervention.
AN AUDIT OF THE IMPACT OF THE WORKLOAD ON ACUTE CARE SURGICAL SERVICES AT GROOTE SCHUUR HOSPITAL FOLLOWING THE CLOSURE OF A LOCAL REFERRING COMMUNITY HOSPITAL
Q Moodie, J Klopper, C Kloppers, P Navsaria, D Kahn
Department of Surgery, Groote Schuur Hospital and University of Cape Town
Background: Groote Schuur Hospital (GSH) has a 40 bed dedicated Acute Care Surgical Unit (ACSU) that functions in a tertiary environment. Acute trauma care is excluded, thus making it a unique concept. GF Jooste Community Hospital (GFJ) closed during September 2013. The patient workload was meant to be shared between a new district hospital and acute care surgical services at GSH. We reviewed the number of referrals 2-months before closure and 3-months after closure to calculate the true impact of the closure.
Materials and Methods: A prospective, HREC approved audit was conducted over a 5 month period. The primary end point was to see if the closure of GFJ had any influence on the on the workload of the ACSU. The surgical profile of the patients seen was also reviewed. Categorical groups of data was analysed using the Chi Square test. p < 0.05 was considered significant.
Results: On average, the two months pre-GFJ closure recorded 125 multi-centre referrals per month, compared with 166 referrals post-closure, thus showing a statistical significance in overall direct referrals to the ACSU following the closure of GFJ [p < 0.0044]. Total number of patients admitted over the 5 month study period was 646, with 518 surgical procedures being performed. The top 5 surgeries performed were: amputations (n=87), hernias (n=78), exploratory laparotomies (n=67), appendicectomies (n=64), and cholecystectomies (n=44). All cases were operated on the emergency list except for 56 hernias and 37 cholecystectomies that were electively done.
Conclusion: The closure of the nearby GFJ showed a significant increase in the multi-centre direct referrals. The new district hospital by inference is not functioning as planned. The ACSU in GSH is a new and unique concept in the South African surgical setting offering purely non-trauma emergency surgery care.
VERSATILITY OF "NO VERTICAL SCAR" MAMMOPLASTY - EXPERIENCE IN MALIGNANT / BENIGN BREAST DISEASE AND BREAST TRAUMA
Y.Brakovsky , I.Buccimazza
Dept. of Plastic & Reconstructive Surgery and Breast Unit I.A.L.C.H. Durban KZN Dept. of Surgery and Breast Unit I.A.L.C.H. Durban UKZN
Background: Commonly used Reduction Mammoplasty incisions (i e. "Wise pattern" ,Vertical scar, "Batwing" etc.) can result in conspicuous , potentially stigmatizing scars especially in African / Asian patients. The "No vertical scar "approach ,although not popular seems to be preferred by patients (as suggested by recent prospective, multi-centric research).
Research Questions: We aimed to assess the suitability of "No vertical scar" technique in surgical treatment of different breast conditions, namely -malignant breast tumours, benign breast tumours and trauma to the breast.
Materials and Methods: Retrospective chart review of 78 patients, treated at I.A.L.C.H. Breast Unit Durban between June 2012 - April 2014.These were consecutive patients assessed by multidisciplinary team as suitable for either: 1)Mastectomy with Contralateral Breast Reduction due to Hypermastia 2) Mastectomy with Breast Reduction Pattern 3) Breast Conserving Surgery - Therapeutic Mammoplasty + symmetrising Breast Reduction. ( In this group 2 patients were excluded due to potentially compromised oncological safety - tumours in zone III and VIII) 4) Mammoplasty for removal of Benign Breast Disease 5) Mammoplasty for treatment of deformity resulting from Trauma to the breast.
The surgical excision margins were measured on Histology where applicable (in group3). The rates/types of complications (major, minor, surgical, aesthetic) were recorded as well as the overall aesthetic results (judged by the panel of observers-photographic results, and the patients themselves- actual results).
Results: There were 18 patients in group1, 1 in group 2, 44 in group 3, 14 in group 4, and 1 in group 5.
There were no major complications in either group.
In group 1 there were 2 minor surgical complications (wound dehiscence /delayed healing)- all healed on dressings only. There were 4 aesthetic complications : 2 too lateral positions of neo-NAC (Nipple-Areola Complex) , 1 under-reduction and 1 - residual lateral fullness.
In group 2 there were 2 minor wound dehiscences, 4 aesthetic complications: 1 too lateral position of NAC,1 "bottoming -out", 2 - residual lateral fullness.
In group 3 there was 1 aesthetic complication of long / visible medial aspect of horizontal scar.Majority of patients were pleased with their aesthetic outcomes (detailed results to follow).
Conclusions: "No Vertical Scar" technique seems to be safe and suitable for use in the surgical treatment of several breast conditions. The "operated on" appearance is avoided resulting in high patients satisfaction.
THE EFFECT OF HIV ON THE MANAGEMENT OF BREAST CANCER
B P Phakathi; V O L Karusseit, S Olorunju,
Introduction: HIV/AIDS and breast cancer have become the two pressing issues in women's health in the 21st century. Women in their reproductive age face a greater risk of HIV infection with approximately 17% in South Africa. HIV infection predisposes patients to the development of neoplasia by depressing their immune system. However, paradoxically some studies have shown that immunosuppression may offer protection against breast cancer, as evidenced by a low incidence of breast cancer in HIV infected patients. Furthermore, the choice of treatment poses a challenge as these patients are prone to both local and systemic complications related to surgery, due to their immunosuppressed status. Moreover, drug interactions between cytotoxic chemotherapeutic agent and anti-retroviral agents further complicates the decision making. The effect of HIV on the management of breast cancer hasn't been studied. This study, therefore aims at determining the effect of HIV in the management outcome in breast cancer.
Method: The study is a prospective, cohort study based at the Steve Biko Academic Hospital, Pretoria- South Africa. All patients diagnosed with breast cancer were asked to participate in the study and were tested for HIV. The patients were divided into three groups: HIV positive patients with CD4 > 200, HIV positive patients with CD 4 < 200 and HIV negative patients. The local and systemic complications related to surgery were compared in these 3 groups. The patients' tolerance to the effect of adjuvant therapy (chemotherapy & radiotherapy) was also compared.
Results: One hundred and fifty nine patients were treated surgically, of whom one hundred and twenty six were HIV negative. Five patients were HIV positive with CD 4 count < 200, of whom four were on ARVs. Twenty four patients were HIV positive with CD 4 count > 200. Local complications occurred in twenty two patients: 14 wound sepsis, 4 seroma, 2 wound hematoma and 2 lymphoedema. All patients with complications were HIV negative. There were no systemic complications related to surgery. One hundred and forty one patients were referred for chemotherapy, of which one hundred and twenty seven had completed the course. Ten patients did not complete chemotherapy due to the effect of chemotherapeutic agents: two of these patients were HIV positive, on ARVs and had developed severe neutropenia while on chemotherapy, which had to be stopped. Twenty-two patients did not receive chemotherapy for various reasons.
Fifty two patients were treated with radiotherapy. Two patients could not complete radiotherapy course: One defaulted, had progression of disease and died before radiotherapy course could be completed. This patient was HIV positive on ARVs. One other patient was HIV negative and had progression of disease.
Conclusion: There was no increase in the rate of complications and the rate of default in the HIV positive group compared to the HIV negative group. We therefore suggest that breast cancer in HIV positive patients be treated according to standard guideline.
DETERMINING THE RELATIONSHIP BETWEEN AGE AND PSYCHOSOCIAL CONCERNS IN BREAST CANCER IN URBAN SOUTH AFRICA
S Rayne1,2,3, D Kruger3, K Wright3 and C A Benn1,2,3
1 Helen Joseph Breast Care Clinic
2 Netcare Breast Care Centre, Milpark Hospital, Johannesburg
3 Health Sciences, University of the Witwatersrand, Johannesburg
Background: In Sub-Saharan Africa there is a considerable lack of understanding of how patients' race, age, culture and beliefs affect their help-seeking behaviour in breast cancer care. This study is part of ongoing research designed to prospectively gather information from women of very differing socioeconomic and racial groups and determine the influence of these variables on psychosocial concerns and delay to presentation in breast cancer. Initially the effect of age is considered.
Aim: To determine the influence of age on psychosocial concerns in breast cancer patients.
Methods and Materials: This was part of a pilot prospective, descriptive study using a questionnaire answered by participants diagnosed with breast cancer and attending currently undergoing active management at either of two centres (government and private) in Johannesburg. Questions determined demographics; socioeconomic and educational background; religious beliefs; time to diagnosis; fears concerning facets of breast cancer diagnosis and treatment; and finally rated their agreement with statements embodying preconceptions surrounding breast cancer.
Results: 158 patients completed the questionnaire and response rate was 100%. 11 patients (9%) failed to complete it adequately and were excluded from analysis beyond demographics.
The age of patients ranged from 23 to 79 years with a mean of 52 years. 31 patients (19.6%) were 40 years or under. 89% of patients spoke English as a first or second language and most patients had completed basic education (74.4%). Patients leaving school early were more likely to be older and of black race (p<0.001).
Younger patients were more likely to be fearful about undergoing surgery both before their treatment (p=0.04) and during their treatment (p=0.01). They also showed a very strong fear at the loss of a breast (p=0.01) and the loss of hair during chemotherapy (p=0.03) although not to the potential of other chemotherapy side-effects. Younger patients were far more likely to be very strongly fearful of dying (p>0.001).
There was also no significant relationship of age with the beliefs of patients surrounding breast cancer: age did not affect whether patients believed in alternative methods of cancer management, whether they believed they would survive nor determine their understanding of who gets breast cancer and why.
Conclusion: Young patients face a unique set of fears when considering a breast cancer diagnosis. This may affect their willingness to undergo treatment and also highlights an important group that may benefit from more intensive counselling and psychosocial support.
THE IMMUNE-MEDIATED CYTOKINE PROFILE OF HORMONE-DEPENDENT AND HORMONE-INDEPENDENT BREAST CANCER CELL LINES IN A 3D IN VITRO SYSTEM
T N Augustine1, R Duarte2, G P Candy3
1 Anatomical Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
2 Internal Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
3 Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
Introduction: Cytokines mediate the complex interactions between immune, and tumour cells within the breast tumour microenvironment. In advanced cancer, an excess of regulatory T (TREG) lymphocyte and lack of natural killer (NK) cells, in tumour infiltrating lymphocyte populations may reflect a shift to adaptive immune mechanisms to promote cancer survival. We established 3-dimensional models of the tumour microenvironment to determine the profile of induced cytokine product.
Methods: NK cells and CD4+CD25+ TREG lymphocytes were co-cultured with luminal phenotype MCF-7 or basal phenotype MDA-MB-231 cell lines in growth factor reduced Matrigel. Cytokine production was measured using a multiplex cytokine assay. Multivariate analyses were used to determine significant differences in cytokine production, and to explore associations and relationships between cytokines.
Results: CCL2, CCL4 and CXCL8 levels were significantly elevated in the MCF-7 culture model reflecting the importance of NK cells whereas increased proinflammatory IL-1B, IL-6, TNF-α, CCL4 and CXCL8 was measured in the MDA-MB-231 culture with both TREG and NK cells. NK cells
alone induced a significant increase in only IL-12 and CCL2. Cluster analysis and principal component analysis implicated IL-6 in the induction of a chemokine cascade.
Conclusions: From the cytokine profiles, we propose that weakly invasive breast tumours may increase their metastatic potential by ameliorating NK cell involvement in the cancer microenvironment. In contrast, proinflammatory TREG cell-mediated cytokine secretion in the basal phenotype model, implicate TREG cells in the maintenance of tumour progression. Further, the data suggests a role for IL-6 in promoting such immune evasion and tissue invasion.
MEDICAL STUDENT STUDY RESOURCES AND ATTITUDE TOWARDS VARIOUS TEACHING METHODS
J H Klopper, L Kuttschreuter
Department of Surgery and the Students Surgical Society, University of Cape Town
Background: Technology has brought about opportunities to improve education. Despite these opportunities, many medical schools still rely on formal lectures and tutorials, requiring students to meet teachers at specific, and often once-off, times and places. We investigate the resources used by modern-day medical stduents and their attitude towards traditional and more modern forms of instruction.
Method: An electronic questionnaire was designed to investigate both the resources that medical students use and their attitude to both traditional and more modern forms of education. The questionnaire was distributed in electronic format to members of the University of Cape Town Surgical Society. The student-led Society comprises students across all years of study and has more than 500 active members.
Results: In all, 110 responses were received, with a good spread over all six years of study. Printed textbooks and formal lecture notes were most often used as study resources, with 29% indicating that they never use more modern online video or audio lectures.
Almost half (45%) of students found formal lectures boring. In accordance with known literature many (51%) noted that they soon forget what was said during lectures and tutorials. Sixty-four percent indicated that they did not prepare for lectures, calling into serious question the effectiveness of traditional forms of teaching.
Another alarming trend was towards the use of regular large search engine inquiries to find study resources, trailing more academically-oriented search engines such as Google Scholar. Even fewer students indicated the use of formal medical database searches, such as Medline. Wikipedia was used by 53% of students on a daily basis.
Discussion: The traditional form of medical education requires formal teaching during lectures and tutorials and self-study by formal texts and departmental lecture notes. This might not be the optimum format as very few students actually prepare for lectures and soon forget what was said during these lectures. Although formal lecture notes are most often used, an alarming number of students indicated that they use Wikipedia and regular Google search on a daily basis. These resources are not peer reviewed and serious thought must be given to educating students on proper resources. Eighty-eight percent of students indicated that they would prefer recorded online lectures that they could view and review at their convenience and efforts to make these available should be a priority.
Conclusion: Findings are in keeping with investigations in other academic fields. The time has come for fundamental changes in medical education to keep up with the needs of the modern student.
THE DEVELOPMENT OF A COMPUTERISED SURGICAL DATABASE AT KING EDWARD VIII HOSPITAL IN DURBAN, SOUTH AFRICA
B Singh, S Ebrahim, A Noorbhai, S S Ramklass
Background: King Edward VIII (KEH) hospital is a large hospital in Durban, providing regional and tertiary services to the entire region of KwaZulu-Natal (KZN) and the Eastern Cape. It is a teaching hospital for the University of KwaZulu-Natal's Nelson R Mandela School of Medicine. In developing countries such as South Africa, with a high burden of disease due to trauma, HIV and other infectious diseases, the design and implementation of a surgical database forms a vital component of a modern surgical care system. At present, there is no system for electronic collection and record of patient information for surgical patients admitted to hospitals in the greater Durban metropolitan area. The development of such a database will facilitate clinical audits and improve the quality of care that surgical patients receive. We aim to design and implement an electronic surgical database for the prospective collection of patient information at KEH.
Methods: Ethical approval was obtained from the Biomedical Research Ethics Committee (BREC) at UKZN. A Relational Database Management System (RDBMS) in the form of Microsoft Access 2013 was used to develop and create a browser-based database application i.e. The King Edward General Surgery Database program. To ensure patient privacy protection, a study number will be created and linked to each patient record. Data will be stored onto a secure server using password-protected access systems. All subsequent secondary data analysis will be performed on de-identified data only. In order to provide consistency and comparability of reporting of medical information, the International Statistical Classification of Diseases and Health Related Problems (ICD) classification was built into the programme. Consultants, registrars, medical officers and interns involved in the clinical care of patients will be trained on data entry and capture and the system will be piloted and tested prior to roll-out. Patient information will be captured on admission as well as the following: demographic data, clinical data, investigations (serology and imaging), management (operative and non-operative) and follow up plans. Each variable is recorded on the database on field-based table. Various tables have been designed to incorporate the vast array of information recorded from each patient. Upon analysing the data, these tables can be cross-referenced to allow specific searches and areas of research. The database will allow the users to enter the data via the front-end (forms only) whilst the back-end will store the data at a secure location with administrator access only. This will allow data integrity and non-manipulation of stored data from non-administrator users.
Results: The prospective information collected will serve as a repository for specific data that can be evaluated, trended, and linked to outcomes. It will act as an ideal information system for performance improvement and quality assurance processes. Additionally it may allow for accurate audits and comparison of outcomes between KEH and other regional and tertiary hospitals in KZN. Other advantages include that it can be used by administrative personnel in cost accounting and by management for the planning of service facilities.
Conclusion: Databases have been described as the "engine of change in today's healthcare environment". A surgical database acts as a source for data which may be used for evaluation, quality control and planning. It has the potential to be a powerful tool for clinical research and the advancement of knowledge in General Surgery. It is envisaged that this endeavour will be successfully implemented at all major hospitals in the greater Durban area as well as major clinical departments in the near future.
GAMIFICATION IN SURGICAL EDUCATION
J H Klopper
Department of Surgery, University of Cape Town
Introduction: Contemporary medical education offers many challenges to both the student and clinician-educator. The setting is unique amongst the fields of higher education, as the teaching requires incorporation into a setting of professional service delivery. Many new tools are made available by the digital age and together with this the modern era of educational research has brought a myriad of new teaching opportunities. Amongst these is the implementation of a strategy of gamification in the clinical setting, aimed at improving certain shortcomings in training by the use of elements of gameplay and reward in a non-game context.
Method: A pilot program of gamification was implemented during a six-week period comprising the rotation of three groups of final year medical students through the Acute Care Surgery Unit at an academic hospital. The strategy aimed at improving three key elements of clinical teaching in the unit, namely active participation in patient consultation and presentation on ward rounds, assistance during surgical procedures, and learning by consulting published literature. Participation was voluntary and managed by subscription to a closed online forum allowing monitoring of participation. Rewards were structured around a points based leaderboard, published daily on the forum.
Results: A total of 21 students took part in the program, resulting a total of 211 posts. Post categories included short descriptions of case presentations and findings during surgical procedures. A total of 24 online reports were submitted after literature searches, all directed towards clinical questions posed to students during patient presentation. The remainder of posts constituted direct discussions amongst students about the content of the aforementioned categorical posts. Direct verbal feedback from students were positive and participation by students in operative cases were subjectively reported as greatly improved by surgeons involved.
Discussion: Gamification involves the implementation of game-play and its inherent psychological motivators to encourage participants in reaching set goals. The pilot program showed that such a strategy can be implemented in the clinical teaching setting augmenting the aims of such teaching.
A MATHEMATICAL MODEL TO PREDICT THE IMPACT ON WAITING LISTS BY IMPROVEMENT IN OPERATING ROOMS WAITING TIMES
J H Klopper
Department of Surgery, University of Cape Town
Background: The operating room environment contributes a large proportion to the efficiency of any surgical department. The number of cases performed has a direct impact on patient throughput and waiting list times. One method of increasing efficiency in theatre is the shortening of time spent between cases. Various methods can be employed to shorten this wasted time period, but can be very costly. A mathematical model can be constructed to look at the impact of any changes. Results of changes calculated by this model can help in planning and cost management of any improvement plan.
Methods: Time periods between elective cases for a specific unit in an academic hospital were calculated from operative records. These times were divided into three groups at cut-off times equating to the first and third quartiles. The proportion of cases in these three groups constituted an initial state matrix. A transitional matrix was constructed, with values that could be changed to accommodate various improvement plans. A Markov chain constructed from these two matrices allowed for the calculation of a steady state matrix from which changes in patient throughput could be reconstituted from the group waiting time averages. The calculated increased patient throughput can be used in a differential equation with constrained growth, which can be used to look at the impact of waiting times and time to approach the maximum.
Results: Constraining the transitional matrix to applicable improvement plans resulted in implementation times spanning 18 to 30 months. The final state matrix showed a clear calculated value as far as patient throughput was concerned, with the effects clearly impacting on both waiting times and time to reach maximum capacity.
Conclusion: The costs involved in improving operating room capacity are prohibitive. A mathematical model that can be used to predict the impact of any changes made is of great value and can save time and money. The mathematical model used here shows very clearly the impact on patient waiting times and can be used in management decisions.
INCIDENCE OF AMPUTATION AMONG PATIENTS WITH DIABETIC FOOT ULCERS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
M L Phakula, M Z Koto, R R Makinita
Department of General Surgery, School of Medicine, Faculty of Health Sciences
University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Background: The Dr George Mukhari Academic Hospital is a tertiary health care facility that serves a large population of patients with diabetes. Without a dedicated diabetic foot clinic, a significant majority of these patients end up with diabetic foot ulcers. Some of these patients eventually end-up with an amputation. A study was undertaken to document the extent of the problem.
Method: A prospective cohort study was done at Dr George Mukhari Academic Hospital between 01/10/2012 and 30/11/2013. Results: 48 patients were included in the study. There were 26(54%) males and 22(46%) females. The mean age at admission was 60.21 ±11.28 years. The mean duration of diabetes was 12.5 ± 10.89 years. 77% had type 2 diabetes mellitus, 56% had hypertension as the only co-morbidity, and 33% of the patients had Wagner 3 ulcers at presentation. The amputation rate was 85% with 63% below knee amputations. The mean hospital stay was 33.9 ± 22.34 days. The inpatient mortality rate was 13%.
Conclusion: An approach which will address issues of patient education, diabetic foot care, early identification of diabetic foot complications, and infection control is needed to reduce the morbidity associated with this problem.
THE EFFECTIVENESS OF THE MAIN ANTIBACTERIAL SUBSTANCES IN PRE-OPERATIVE HAND CLEANSING USED BY SURGEONS IN BLOEMFONTEIN
M. Jonker, R. Kleinhans, I. Reyneke, B van Niekerk, S M le Grange
UFS, Bloemfontein
Introduction: Wound infections remain an ever-present problem in our surgical wards. Since the most commonly cultured organisms originate from the skin, we asked ourselves how effective the cleansing mechanisms of both the patient's skin, as well as the surgeons' hands are. We then recognised the absence of trials comparing the effectiveness of the different hand scrubbing substances commonly used in the Bloemfontein hospitals.
Aim: The aim of our study was to investigate chlorhexidine gluconate (HibiScrubR), povidine-iodine (BetadineR), chlorhexidine+isopropyl (BioscrubR) and SurgisoapR used by surgeons in the major hospitals in Bloemfontein, with the intent to determine the most effective substance in removing pathogenic organisms. By undertaking to compare these substances, we saw an opportunity to improve the health care system in Bloemfontein, even if only by a small margin.
Method: A prospective, cross-over controlled study was done in the theatre complex of Universitas Academic Hospital, Bloemfontein. Approval was obtained from the Ethics Committee of the Faculty of Health Sciences, UFS. Registrars and consultants from different surgical disciplines were identified who, after signing informed consent, took part in the study. Each of the substances was tested on separate days. A pre-wash swab was taken on three specific areas of the hand, after which the surgeons scrubbed for exactly three minutes. The hands were then dried with a sterile towel. A post-wash swab was then taken on the same areas as the pre-wash swab. These swabs were then cultured to determine colonial growth counts.
Results: The results showed that BioscrubR had the highest clearance percentage (99%) of S. epidermidis, followed by Betadine (91%). HibiscrubR had a clearance percentage of 90%, while SurgisoapR obtained a 73,8% clearance rate.

Conclusion: Although we aimed to identify the most effective hand scrubbing substance, we found the most ineffective hand scrubbing substance. According to our results, there was no significant difference in the effectiveness of BioscrubR, HibiscrubR and BetadineR. However, in our particular study, SurgisoapR underperformed relative to the other three substances.
EARLY RECOVERY AFTER SURGERY (ERAS) IN TRAUMA SURGERY: A PROSPECTIVE SINGLECENTER PILOT STUDY
R Moydien (Registrar), R Oodit, AJ Nicol, S Edu, J Klopper, PH Navsaria
Trauma Center, Groote Schuur Hospital and University of Cape Town
Introduction: ERAS programmes conducted in elective colorectal, vascular, urologic and orthopaedic surgery has provided strong evidence for decreased lengths of hospital stay without increase in postoperative complications. Aim: The aim of this study was to explore the role and benefits, if any, of ERAS / ERP (early recovery programmes) implemented in patients undergoing emergency laparotomy for trauma at a level 1 trauma center.
Methods: Institutional UCT-HREC approved study. A prospective cohort of 38 consecutive patients with isolated penetrating abdominal trauma undergoing emergency laparotomy were included in the study. The ERP included: early feeding, early u-catheter removal, early mobilisation/ physiotherapy, early intravenous line removal and early optimal oral analgesia. This group was compared to a historical control group of 40 consecutive patients undergoing emergency laparotomy for penetrating abdominal trauma, prior to introduction of ERP. Demographics, mechanism of injury and injury severity scores (ISS and PATI) were determined for both groups. The primary end-points were the length of hospital stay and incidence of complications (Clavien-Dindo classification) in the 2 groups. The difference in means was tested using the t-test assuming unequal variances. Statistical significance was defined as p less than 0.05.
Results: The two groups were comparable with regards to age, gender, mechanism of injury and ISS and PATI scores. The mean time to solid diet, catheter removal and NGT removal was (non ERAS) 3.6 and (ERAS) 2.8 days [p < 0.035], (non ERAS) 3.3 and (ERAS) 1.9 days [p <0.00003], (nonERAS) 2.1 and (ERAS) 1.2 days [p < 0.0042], respectively. There was no difference in time from admission, to time of laparotomy [(non ERAS) 313 vs. (ERAS) 358] min (p < 0.07). There were 11 and 12 complications in the control and study group, respectively. When graded as per the Clavien-Dindo classification there was no significant difference in the 2 groups (p < 0.59). Hospital stay was significantly shorter in the ERAS group: 5.5 (SD 1.8) days vs. 8.4 (SD 4.2) days [p < 0.00021].
Conclusion: This small pilot study shows that ERPs can be successfully implemented with significant shorter hospital stays without any increase in postoperative complications in trauma patients undergoing emergency laparotomy for penetrating abdominal trauma. Furthermore, the study shows that ERP can also be applied to patients undergoing emergency surgery.
SELECTIVE NONOPERATIVE MANAGEMENT IN 1106 PATIENTS WITH ABDOMINAL GUNSHOT WOUNDS: CONCLUSIONS ON SAFETY, EFFICACY, AND THE ROLE OF SELECTIVE CT IMAGING IN A PROSPECTIVE SINGLE-CENTER STUDY
P H Navsaria, A J Nicol, S Edu, R Gandhi, C G Ball
Trauma Center, Groote Schuur Hospital and University of Cape Town
Background: Nonoperative management (NOM) of abdominal gunshot wounds (AGSW) remains controversial.
Objective: The primary aim of this study was to delineate the role of computed tomography (CT) in patients undergoing NOM for AGSW.
Methods: This prospective, HREC approved study, included all patients with abdominal gunshot injuries admitted to our trauma centre from 01 April 2004 to 30 September 2009. Exclusion criteria included patients with peritonitis, hemodynamic instability, unreliable physical examination, head and spinal cord injury with an AGSW underwent immediate laparotomy. The remaining patients were selected for nonoperative management. Nonperitonitic stable patients with right-sided thoracoabdominal (RTA) / right upper quadrant (RUQ) gunshots and/or haematuria underwent mandatory computed tomography (CT) with intravenous contrast. CT to delineate missile trajectory was optional. The primary outcome measure was failure of NOM. Secondary outcomes were unnecessary laparotomy rates and mortality.
Results: A total of 1106 patients with abdominal gunshot injuries were admitted. Of these, 834 (75.4%) underwent immediate laparotomy, while 272 (24.6%) were selected for NOM. In the former group, there were 56 (6.7%) deaths and 29 (3.5%) unnecessary laparotomies, while in the latter NOM group, 82 (30.1%) patients were managed by serial clinical examination alone, while 190 (69.9%) patients underwent abdominal CT scan, in addition to serial clinical examination. The overall NOM success rate was 95.2%. Of the 13 patients undergoing delayed laparotomy, there were 10 therapeutic, 2 non-therapeutic and one negative laparotomy.
Conclusion: The NOM of appropriately selected patients with AGSW with selective use of CT scanning is feasible, safe and effective, but largely based on findings from serial clinical examinations.
AN AUTOPSY STUDY OF SPLENIC INJURIES SEEN IN PATIENTS WITH BLUNT ABDOMINAL TRAUMA AT PARIRENYATWA GROUP OF HOSPITALS IN HARARE: PREVALENCE OF MISSED SPLENIC INJURIES
N R Zulu, G I Muguti
Dept of Surgery, University of Harare, Zimbabwe
Background: The spleen is one of the most commonly injured organs following blunt abdominal trauma. In low resource centres, absent management protocols and the lack of expertise and equipment, have resulted in a significant number of splenic injuries being missed.
Objectives: To determine the frequency of missed splenic injuries related to blunt abdominal trauma at the Parirenyatwa Group of Hospitals at autopsy.
• To evaluate the initial diagnostic modalities being utilised in screening for splenic injuries.
• To identify other injuries associated with missed splenic injuries at autopsy.
Study Design: Retrospective Descriptive autopsy study.
Materials and Methods: Records of autopsies done over the period January 2008-December 2011 were analysed in conjunction with those from casualty at the Parirenyatwa Group of Hospitals. All autopsies performed for blunt trauma were included in the study. Analysis was done using Stata version 10.0.Permission to undertake the study was obtained from the Joint Parirenyatwa and College of Health Sciences Research and Ethics Committee.
Results: A total of 2171 autopsies were conducted for blunt trauma during the period January 2008 and December 2011. Of these, 136 cases were identified as having a missed splenic injury, giving a prevalence of 6% (p=0.001). In 83% of cases, the initial attending clinician was the casualty officer.Sixty per cent of cases presented with a Glasgow Coma Scale of 3-8. Head injuries were the most common association in 46% of cases. None of the cases had an ultrasound scan done.
Conclusion: The study confirms that a significant number of splenic injuries were missed by the attending clinician. A low Glasgow Coma Scale and the presence of serious injuries were the commonest associations. The lack of training in ATLS®, absence of protocols of managing trauma patients and inadequate diagnostic equipment and expertise were the other contributory factors associated with the missed splenic injuries. Early detection and appropriate management of these cases could significantly reduce the mortality of these poly-trauma patients.
THE PREVALENCE OF PRIMARY HEPATIC SPACE OCCUPYING LESIONS IN PATIENTS WHO DIE FROM UNNATURAL CAUSES AT PARIRENYATWA GROUP OF HOSPITALS AND HARARE CENTRAL HOSPITAL, ZIMBABWE
A A Munyika, R Makunike-Mutasa, G Muguti
Department of Surgery, Parirenyatwa Group of Hospitals, Harare, Zimbabwe
Introduction: Parirenyatwa Group of Hospitals and Harare Central Hospital are the main University Teaching Hospitals in Zimbabwe. In this study we selected a sample population of subjects who died from unnatural causes at the two hospitals, i.e. Road Traffic Accidents (RTAs), suicide, gunshot wounds, stab wounds, drowning, burns, maternal deaths, poisoning, and studied their livers to identify primary hepatic space occupying lesions (PHSOLs). There have been no postmortem studies done in Zimbabwe to look at the prevalence of PHSOLs.
Objectives: Major objectives:
1. Identify the prevalence of tumor-like, benign and malignant PHSOLs in subjects who die from unnatural causes.
Minor objectives:
1. Identifying the commonest benign liver lesions at post mortem
2. Calculate the prevalence and identify the commonest primary malignant tumor in subjects who died from unnatural causes
3. Identify the epidemiological distribution of PHSOLs at post-mortem in subjects who died from unnatural causes.
Design and Site: This was a descriptive prospective postmortem cross sectional study which took place at Parirenyatwa Group of Hospitals and Harare Central Hospital in Zimbabwe.
Materials and Methods: A total of 150 cases were studied over a period of 6 months. The study focused on primary space occupying liver lesions and their distribution in terms of age, sex and race. The lesions identified were described and their final diagnosis confirmed at histology. All specimens were analyzed in the department of histopathology at Parirenyatwa Group of Hospitals.
Results: The mean age in this study was 34 years, IQR (Q1=26, Q3=44). There were 103 males and 47 females (M: F, 2:1). The total prevalence of hepatic space occupying lesions was 15.3% (n=22). The only benign PHSOLs found was cavernous haemangioma (5.3%, n=8). There were more male subjects with cavernous haemangioma than females (6 vs. 2). There were no malignant PHSOLs found.
Conclusion: The prevalence of cavernous haemangioma (5.3%) is the same as that reported by other authors from developed countries. We ascribed the absence of other PHSOLs to the relatively small sample size.
NONOPERATIVE MANAGEMENT OF PENETRATING LIVE TRAUMA
P H Navsaria, M Hommes, A J Nicol, S Edu, J E Krige
Background: Nonoperative management (NOM) of penetrating liver injuries is infrequently practised. The aim of this study was to assess the safety of selective NOM of penetrating liver injuries.
Patients and Methods: A prospective, protocol-driven, HREC approved study, which included patients with penetrating liver injuries admitted to a level I trauma center, was conducted over a 52- month period (Sept 2008 - Dec 2012). Patients with right-side thoracoabdominal, and right upper quadrant (RUQ) penetrating wounds with or without localized RUQ tenderness underwent contrasted abdominal CT scan evaluation to detect the presence of a liver injury. Patients with confirmed liver injuries were observed with serial clinical examinations. Outcome parameters included need for delayed laparotomy, complications, length of hospital stay and survival.
Results: During the study period, 95 patients (54 gunshot and 41stabbed liver injuries), were selected for nonoperative management. The mean injury severity and PATI scores were 20 (range 4-50) and 7(range 4-20), respectively. Simple liver injuries (Grades I and II) occurred in 49 (51.6%) patients and complex liver injuries occurred in 46 (48.4%) patients. Associated injuries included 23 (24.2%) kidney, 69 (72.6%) diaphragm, 23 (24.2 %) lung contusion, 42 (66.7%) hemo/pneuomothorax, and 28 (29.5%) rib fractures. Two patients required delayed laparotomy resulting in successful nonoperative management rate of 97.9%. Complications included: liver abscess (1), biliary fistula (9), retained hemothorax (3), and nosocomial pneumonia (4). The overall median hospital stay was 6 IQR: [4-11] days, with no mortality.
Conclusion: The nonoperative management of appropriately selected patients with penetrating liver injuries is safe and associated with minimal morbidity.
TRAUMATIC DIAPHRAGMATIC INJURY: CONTEMPORARY MANAGEMENT AT EDENDALE HOSPITAL
N D'Souza, G Laing, D Clarke
Edendale Hospital
Introduction: The range of traumatic diaphragmatic injuries begins with the occult, isolated small defect and extends to the diaphragmatic rupture with multiple associated injuries. Laparoscopy has emerged over the last 20 years as a diagnostic and therapeutic tool to manage the occult diaphragmatic injury.
This series looks at the spectrum and management of traumatic diaphragmatic injury at Edendale Hospital in the contemporary era.
Methods: The prospective trauma registry of Pietermaritzburg metropolitan complex has been maintained since January 1st 2012.
Results: A total of 51 patients with diaphragmatic injury were treated in this period under review. The mechanism of injury was penetrating trauma in 48 patients (94%) and blunt trauma in 3 patients (6%). 38 patients had injuries found at laparotomy or thoracotomy and13 patients had occult diaphragmatic injury found at laparoscopy.
At laparotomy, 31 patients had lacerations to the diaphragm, 2 had acute herniation of visceral organs, and 5 patients presented with chronic diaphragmatic injuries. 27 of 33 acute patients at laparotomy +/- thoracotomy had associated intra-abdominal or cardio-pulmonary injuries (82%).
77 patients underwent diagnostic laparoscopy for left thoraco-abdominal injuries, 13 of whom had diaphragmatic injuries (17%). 9 of the 13 defects (69%) were repaired laparoscopically. 3 patients with diaphragmatic injuries (23%) had additional intra-abdominal injuries seen at laparoscopy, 1 of which required intervention through laparotomy.
Conclusion: Diaphragmatic injuries are often diagnosed intra-operatively in association with multiple associated injuries. Isolated diaphragmatic injuries can be detected and repaired at laparoscopy.
We believe that the detection rate of diaphragmatic injury in our series of 17%, and high rate of successful minimally invasive repair justifies our practice of routine diagnostic laparoscopy in thoraco-abdominal injury.
MANAGEMENT OF COLONIC TRAUMA IN THE DAMAGE CONTROL ERA IN THE PIETERMARITZ-BURG METROPOLITAN TRAUMA SERVICE
B Shazi, D L Clarke, G Laing, J L Bruce
Background to the study: Trauma remains a major problem in South Africa. In the Pietermaritzburg Metropolitan Trauma Service our spectrum of trauma is different to that of the developed world. We have a high burden of penetrating trauma and colonic trauma is a common sequelae. We generally experience long delays from time of injury to definitive care. The management of colonic trauma has undergone a number of changes over the last seventy years.
Aim of the Study: Audit our experience in the PMTS regarding management of colonic trauma.
Methodology: This study is a descriptive, retrospective audit of a prospectively maintained regsitry. The PMTS maintains a digital trauma registry, which captures data at both Edendale and Greys hospitals. Ethics approval to maintain this registry has been obtained from the Biomedical Research Ethics Committee (BCA221/13 BREC) of the University of KwaZulu-Natal and from the Research Unit of the Department of Health. We were able to retrieve all the data on colonic trauma over a three year period: 2012 - 2014.
Results: Out of the 118 patients with colonic trauma who presented at the PMTS over the 3 year period, only 2 were children, 7 were females, and 109 were males. Four percent and 96% of colonic injuries were due to blunt and penetrating trauma, respectively. Sixty percent of the penetrating trauma was the result of stab wounds, whereas 40% is from gunshot wounds. Most of the patients presented with other associated abdominal injuries. About 15% of patients had colostomies as part of damage control surgery, due to delayed presentation or because of 2 missed colonic injuries and 1 patient needed a colostomy because of breakdown of colonic repair. Most of the colonic injuries were repaired primarily. Transverse colon was the most commonly injured part of the colon, followed by descending and sigmoid colon, ascending and splenic flexure, caecum, and hepatic flexure. Only 5 patients died, and this was mostly due to delayed presentation and associated multi-organ failure.
Conclusion: Our management of colonic trauma is in line with current evidence in the literature. Our challenge remains the delay in the presentation of some of our patients. The results of our study provide a solution to this challenge. That solution is to avoid performing a primary repair or an anastomosis in the setting of damage control surgery but rather bring a colostomy.
LAPARASCOPIC GRAHAM PATCH FOR PERFORATED PEPTIC ULCER AT DR GEORGE MUKHARI ACADEMIC MUKHARI HOSPITAL
M N Latakgomo, M Z Koto, M L Phakula
Department of General Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus Dr George Mukhari Academic Hospital
Introduction: Perforated peptic ulcer is a relatively common acute surgical condition. It remains a challenge for a treating surgeon especially in patients with high Boey score and those with giant ulcers. Minimally invasive surgery has become integral part of management of this condition.
Aim: To update on our initial experience with laparascopic Graham patch for perforated peptic ulcer.
Methods: This is a retrospective review of prospectively collected data on patients who presented with perforated peptic ulcer between 01 November 2011 to December 2013. Exclusion criteria include those who were offered open surgery. The patients' demographics, clinical condition, operative procedure and outcome were all collected. All patients were resuscitated fully and offered laparascopic Graham patch. A three port technique was used for most cases and additional port was inserted when necessary.
Results: During this period 53 patients were seen, (47 males and 6 females) their mean age 44years (19-71). Average Boey score 2. The average operative time was 90 min, the mean hospital stay was 4days. One patient spent 2days in ICU because she had associated comorbidity preoperatively and one patient had superficial wound sepsis.
Conclusion: Laparascopic Graham patch is safe and feasible in our setting. Patient with a high Boey score did better than expected.
LAPAROSCOPY AT SEBOKENG HOSPITAL
I Bombil, A Maraj, W S Lunda, J Thompson, B Puttergill
Department of Surgery, Sebokeng Hospital and the Faculty of Health Sciences
University of Witwatersrand, Johannesburg, South Africa
Background: Advances in minimal access surgery has revolutionised the practice of surgery over the past two decade. In some cases, laparoscopy has become the standard of care for example cholecystectomy. But trauma laparoscopy seems to be trailing behind supposedly because of fear of missed injury in an unpredictable trauma setting. There are reports in the literature about the benefit of laparoscopy in trauma, but we do not have local data. We therefore endeavour to assess the place of laparoscopy in trauma through the audit of our laparoscopy practice at Sebokeng Hospital, South Africa.
Methods:
• Study design: A retrospective study of prospectively collected data
• Setting: Sebokeng Hospital, Vaal , South Africa
• Inclusion criteria: All laparoscopic procedures performed between November 2011 and October 2012 with available data were included
• Objective: Overview of practice of laparoscopy at Sebokeng Hospital with special emphasis on trauma to identify the indications of laparoscopy in the management of selected injuries. The aim is to answer the question: is there any role for laparoscopy in trauma?
• Statistical analysis: Descriptive study using proportion by ratio or percentage
• Ethics: Ethic approval has been obtained from the Wits Human Research Ethic Committee (M121111)
Results: A total of 390 laparoscopic procedures were performed. Majority were emergency 77.9% (304/390) topped by appendicectomy 54.9% (167/304) whilst trauma represented 13.8% (42/304) of all emergencies. Cholecystectomy was the most common elective procedure 74.4% (64/86). Of the trauma cases, 40 were available for analysis; they were predominantly male (36/40) and stable penetrating trauma was the most common indication (34/40). Laparoscopy was successfully completed in 65% (26/40) of the patients. The remaining cases benefited from conversion 17.5% (7/40), laparoscopy assisted mini-laparotomy 15% (6/40) and laparoscopy guided referral to tertiary Hospital 2.5% (1/40).
Conclusion: Laparoscopy is applicable in trauma in carefully selected cases obviating the need for unnecessary laparotomy with its related early and long term complications.
DIAGNOSTIC AND THERAPEUTIC LAPAROSCOPY IN PATIENTS WITH PENETRATING ABDOMINAL TRAUMA: A TWO YEAR EXPERIENCE
M Z Koto, O Y Matsevych, S Motilall, N Kumar
Surgery, Dr George Mukhari Academic Hospital, Health Sciences, University of Limpopo, Pretoria
Introduction: Diagnostic and therapeutic laparoscopy is well established approach in managing patients with penetrating abdominal trauma. However, multiple controversies exist on indications, contraindications and its appropriateness.
Research Question: What were indications and contraindications for diagnostic and therapeutic laparoscopy in patients with penetrating abdominal trauma at Dr George Mukhari Academic Hospital during 2012-2013 years.
Materials and Methods: This is a retrospective, observational study. All retrieved cases of patients with penetrating abdominal trauma managed by diagnostic and therapeutic laparoscopy during 2012 -2013 were included into the study. The patients cases recorded as converted from laparoscopy to laparotomy were also included into the study. Exclusion criteria: patients under age of 12 year old, patients with blunt abdominal trauma, patients treated non-operatively or with primary laparotomy, patients whose records were missing or incomplete.The recorded indications and contraindications were looked into. The critical review of appropriateness of laparoscopy in terms of adverse outcome (complication, reoperations and mortality) were done.
Data Analysis: Demographic details were summarised descriptively by mean, minimum and maximum values for continuous variables, and frequency count and percentage calculations for categorical variables. The prevalence of diagnostic laparoscopy was compared with the prevalence of therapeutic laparoscopy for gunshot wounds (GSW), stab wounds and overall. Clinical outcomes following laparoscopic surgery were described descriptively. The Fisher exact test was used for comparisons of frequency counts/percentage. The p-values < 0,05 was considered significant.
Ethical Considerations: The ethical clearance was obtained from the Medunsa Research and Ethics Committee (MREC) and the permission to conduct the research was granted by the authorities of Dr George Mukhari Academic Hospital.
Results: Out of 114 patients, who met inclusion criteria, stab injuries were sustained by 81 (71%) patients and 33 (29%) patients sustained GSW to the abdomen. The conversion rate was 7%. The operation was completed laparoscopically in 106 patients (79 with stab wounds (74.5%) and 27 with GSW (25.5%)). The diagnostic laparoscopy was performed on 44 (41.5%) patients and therapeutic on 62 (58.5%) patients. The fully laparoscopic therapeutic procedures were performed on 39 (36.8%) patients and laparoscopic-assisted on 23 (21.7%) patients. The most common therapeutic procedure was the diaphragm repair followed by the repair of the stomach, small bowel and colon. In total 13 (12%) patients required re-intervention and two patients died (1.9%). All complications were not specific to laparoscopic approach. No missed injuries were reported in the study.
Conclusion: The diagnostic and therapeutic laparoscopy in patients with penetrating abdominal trauma is appropriate in haemodynamically stable or responsive to initial resuscitation patients. The location of injuries is not a limiting factor but affecting ports placement. The conversion is not a complication but a correct way of completing the operation in an appropriate situation and should be considered in patients with intraoperative extensive bleeding indicating possibility of significant vessel injury, significant deterioration of the haemodynamic status and complexity of the injuries requiring prolong laparoscopic procedure.
HAND-ASSISTED LAPAROSCOPIC LIVING DONOR NEPHRECTOMY: A COMPARISON OF RECIPIENT OUTCOME WITH AN EQUIVALENT OPEN NEPHRECTOMY GROUP
M Schamm, B Jugmohan, C Joseph, J R Botha, J F Botha, R Britz, J Loveland
Transplant Division, Department of General Surgery, University of the Witwatersrand
Objective/Background: Laparoscopic donor nephrectomy has become the procedure of choice for living donor kidney transplantation in many centres. We report our experience with hand-assisted laparoscopic donor nephrectomy (HALDN), concentrating on graft function and postoperative surgical complications in the recipient population, comparing outcomes to a similar group who had received kidneys procured by open living-donor nephrectomy (OLDN).
Materials and Methods: After institutional approval, files of all patients transplanted between September 2008 and June 2011 were reviewed. 100 patients with end-stage renal disease received kidney transplantations from living donors. OLDN was performed in 65 donors, and 35 underwent HALDN. Delayed graft function and post-operative complications were recorded.
Results: Six adverse events were reported, of which 5 presented with delayed graft function (DGF). One DGF was reported in the HALDN group and 4 in the OLDN group. The morbidity in the HALDN group (1/35, 2.9%) was a graft rupture secondary to acute rejection that required exploration and transplant nephrectomy. Five patients in the OLDN group (5/65, 7.7%) required re-operation. This amounts to an overall morbidity of 6 percent, with no mortalities.
Conclusion: As previously documented, HALDN is safe and not inferior to OLDN for the donor. It is not associated with either an increased incidence of DGF or a higher complication rate in the transplant recipient, when compared to the cohort that received a kidney harvested by the OLDN technique.
YOUNG AGE IS NOT ASSOCIATED TO ADVERSE TUMOUR BIOLOGY IN A SOUTH AFRICAN POPULATION
S Rayne1,2, E Cloete2 and C A Benn1,2
1 Helen Joseph Breast Care Clinic, Johannesburg
2 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Background: Age is reported to be an independent risk-factor for prognosis in breast cancer with young patients having adverse molecular sub-types and later stage disease. In Sub-Saharan Africa where later presentation is common in all patients, less in known about the effect young age has on tumour biology and advanced disease.
Research Question: To determine the relationship between tumour biology, stage and young age at presentation in a government hospital.
Material and Methods: This was a one-year period retrospective review of consecutive uninsured patients diagnosed with a breast malignancy. Tumour characteristics and stage at presentation were compared, particularly with reference to young patients (40 years and under). Data was analysed using simple descriptive and statistical analysis. A p-value of <0.05 was determined significant.
Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee.
Results: A new breast malignancy was found in 334 patients including 292 invasive ductal carcinomas,17 lobular and other sub-types and 13 patients with DCIS. 12 patients had other malignancies and were excluded. The median age at diagnosis was 55, with 57 (17.7%) 40 years or under.
64.0% (206) of patients presenting with a breast cancer were black. Although more young patients were of black race than non-black, this was not significant (p=0.23).There was no significant difference in the incidence of grade 3 tumours and triple negative tumours between younger and older patients (p=0.49 and p=0.15 respectively). Although not significant, HER2 overexpression was found more commonly in the older patients (22.4% vs 17.3%, p=0.12).
The median tumour size was 39mm in young patients and 20mm in older patients (p=0.03). Despite the difference in tumour size, as is common in our practice, most patients in both young and older groups presented with nodal disease, and in equal numbers (75.5% and 74.8%, p=0.91).
Conclusion: Young patients had significantly larger tumours but with no change in nodal status probably due to the high level of nodal involvement in all patients. This may reflect a delay in presentation or diagnosis but is not related to adverse tumour biology, with none of the three surrogate markers of aggression significantly more common in our younger South African patients.
PRESERVED AREOLAR SKIN AFTER SKIN-SPARING MASTECTOMY PROVIDES INCREASED SENSATION IN THE RECONSTRUCTED NIPPLE AREOLAR COMPLEX
I do Vale1, S Rayne1,2, C A Benn1,2, J Slabbert2, C Serrurier2
1 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
2 Netcare Breast Care Centre, Milpark Hospital, Johannesburg
Background: Nipple areolar complex reconstruction (NACR) is the final stage of breast reconstruction that transforms the surgically created breast mound into a more natural-looking breast facsimile, using local or distant tissue. Its aim is only to restore aesthetic integrity and sensation is usually impaired which disappoints many patients. A new technique of sparing areolar skin at the time of skin-sparing mastectomy (SSM) can be used with this areolar tissue used then to reconstruct the nipple. The benefit to nipple sensation of this technique is unknown. of NACR.
Research Question: To determine the effect of areolar skin preservation on nipple sensation after Areolar-skin Preserved NACR (A-PNACR) compared to traditional methods.
Material and Methods: This was a prospective study of patients who underwent NACR between 2009 and 2013 in one unit. The study groups comprised patients who had undergone bilateral NACR using preserved areolar skin and full-thickness skin graft (FTSG), following SSM with areolar-skin preservation. The control group comprised patients with NACR from chest wall skin and FTSG after mastectomy and expander-prostheses reconstruction.
Skin sensation was determined by light touch using a cotton swab and sensation using a Semmes-Weinstein monofilament kit exerting between 0.07g and 300g pressure. Sensation was tested in four quadrants of each nipple and each areolar (8 patient test-areas (PTA) per patient) using the suprasternal notch as control. Minimum grams of pressure resulting in sensation were recorded for each area.
Data was analysed using simple descriptive and statistical analysis. A p-value of <0.05 was determined significant. Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee.
Results: 29 patients were recruited, 18 in study group (A-PNACR) and 11 as control. The groups were well-matched for age and time since final surgery. Nipple reconstruction used either a Maltese cross (8 study, 11 control) or double opposing tab (10 study, 0 control; p=0.002).
Pressure sensation was highly significantly increased in patients with A-P NACR with sensitivity to 0.07g found in 12 PTA and to 0.4g in17 PTA. No sensitivity to 0.07g or 0.4g was found in the control group (p<0.00001). Far fewer A-PNACR patients had very poor (300g) or absent nipple sensation (50 PTA vs 74 PTA; p<0.0001). Light touch was diminished in both groups although better in A-P NACR (11.1% vs 4.8%; NS).
Conclusion: This study confirms that an areolar-skin preserved NACR confers significantly better nipple sensation for patients post-operatively than conventional techniques of NACR.
TREATMENT OUTCOMES OF BREAST CARCINOMA IN A RESOURCE-LIMITED ENVIRONMENT
M du Plessis & J P Apffelstaedt
Surgery; University of Stellenbosch; Tygerberg Hospital
Introduction: Carcinoma of the breast is the second most common malignancy among South African women and its incidence is rising and the mortality rate is significantly higher than in the developed world.
Offering quality treatment in a resource-limited environment with poor patient socioeconomic circumstances are ongoing challenges. Frail health as well as lack of support for the event of severe toxicity and finally the lack of availability of advanced pharmaceuticals, taxane regimens and biologicals, limits treatment options for chemotherapy.
Methods: Records of 250 consecutive female patients newly diagnosed with breast cancer from January 2008, were retrieved and analysed. Staging at diagnosis, demographic data, histopathology, treatment given, compliance and outcomes were recorded retrospectively.
Results: Average follow-up time was 36.2 months. The mean age was 56 years. 205 patients underwent surgery. 84.4% of patients were fully compliant with therapy. Stage II survival was 73.4% and stage IV survival 21%. Stage III survival was 29.6%, significantly lower to survival figures in the developed world. A large proportion of patients with stage II and III breast cancer in our series did not receive chemotherapy. For stage III patients not a single pathologically complete response was recorded; in stage II complete response rate was 10%. 41 out of 51 patients (80.3%) with node negative tumours larger than 2cm and only 3 out of 14 patients (21.4%) with 1-2cm node negative tumours received adjuvant chemotherapy.
83.8% node positive stage II and 88% stage III patients received adjuvant radiotherapy. 90.7% of the oestrogen receptor positive tumours received hormonal therapy and 64% of these were still taking treatment at time of last follow-up.
Conclusion: Stage III survival in this series was considerably lower than developed world figures.
Adjuvant radiotherapy and hormonal therapy were well applied where indicated. The option of adjuvant chemotherapy was underutilised in this series. Moreover tumours showed poor response to chemotherapy regimens administered. The emphasis on the expansion of the services to women with breast cancer should concentrate on the extension of medical oncological services to improve outcomes. Biologicals as well as advanced chemotherapeutic options including taxane regimens should be made available.
USE OF THE LOCAL PERFORATOR FLAPS IN SURGICAL MANAGEMENT OF BREAST CANCER
Y. Brakovsky, I. Buccimazza.
Dept. of Plastic & Reconstructive Surgery and Breast Unit I.A.L.C.H. Durban KZN
Dept. of Surgery and Breast Unit I.A.L.C.H. Durban UKZN
Background: Local perforator flaps constitute an additional option in Breast Conserving Surgery in patients not suitable for Parenchymal Flaps or Therapeutic Mammoplasty, this option is also minimally invasive as it preserves the underlying muscles.
Research Question: Assessment of the long-term results with the use of these flaps.
Materials and Methods: Retrospective chart review of all breast cancer patients in whom local perforator flaps were used between May 2008 and April 2014.This included follow-up visits and photographic follow-up. The following were assessed:
• Oncological outcomes ( local recurrence rate)
• Surgical complications ( Flap loss ,fat necrosis ) .
• DXT- related complications (Hyperpigmentation, flap atrophy)
Overall aesthetic outcomes (as judged by the panel of independent observers and patients themselves -questionnaire) and their change with time.
Results:
• 44 patients ( 42 females, 2 males)
• 39 patients underwent immediate reconstruction of partial mastectomy defects.
• 3 patients underwent reconstruction of chest wall / male breast defects.
• 2 patients underwent augmentation of the breast opposite to reconstructed total mastectomy defect.
• 42 patients received adjuvant Radiotherapy.
• 39 L-ICAP flaps, 2 TDAP flaps, 2 LaTP flaps, 2 IMAP flaps and1 A- ICAP flap were used.
• All flaps were totally islanded, Propeller - type flaps.
• There were no local recurrences, 1 total flap loss, 2 partial flap losses,3 cases of fat necrosis.
• Hyperpigmentation in 2 patients. Most aesthetic results were judged as good ( details to follow.)
Conclusions: In long term follow up local perforator flaps appear safe and reliable. Aesthetic results appear to be stable or improve with time. Patients satisfaction is high.
THE LEFT CORONARY ARTERY AND ITS BRANCHES: THEIR ANATOMICAL BASE FOR SURGICAL INTERVENTION
N O Ajayi1, L Lazarus1, E A Vanker2, K S Satyapall
1 Clinical Anatomy, Laboratory Medicine and Medical Sciences, College of Health Sciences, University of KwaZulu-Natal, Westville Campus, Durban
2 Specialist Cardio-Thoracic Surgeon, St. Augustine's Hospital, Chelmsford Medical Centre, Durban, KwaZulu-Natal
Introduction: The left coronary artery (LCA) extends from its origin at the aortic sinus to its division into its terminal branches viz. the left circumflex (LCx) and left anterior descending (LAD) arteries. Several morphological and morphometric factors influence the disease process and surgical intervention used in the management of coronary artery disease. Some of the morphologic variations include the absence of the LCA and bridging of the LAD.
Aims: The study aimed to document the parameters of the LCA and LAD that may influence coronary arterial disease process and its management.
Materials and methods: The study comprised of two subsets viz: (a) Angiographic subset: A total of 170 coronary angiograms obtained from cardiac catheterization laboratories in the eThekwini Metropolitan Area, KwaZulu-Natal, South Africa. (b) Surgical notes: A review of 1 349 surgical reports of consecutive CABGs performed over a period of 23 years. (a) After exclusion of the angiograms with absence of the LCA (n=19), the morphometry of the LCA in the remaining angiograms (n=151) was determined in relation to the atherosclerotic distribution in its branches (b) The prevalence of the intramyocardial (IM) course of the LAD and surgical methods employed in their grafting was documented. All analyses were performed by a single observer and used the statistical package for Social Sciences (SPSS); a p value < 0.05 was considered significant. Ethical clearance (Ethics no. BE 103/11) was obtained from the relevant institutional committee.
Results: (a) Angiographic subset: The mean length, diameter and angle of division of the LCA were as follows: Total angiograms: 10.4mm, 3.8mm and 86.2o; normal group: 10.5mm, 3.9mm and 85.7o, Coronary artery disease (CAD) group: 10.2 mm, 3.7mm and 86.3o; proximal sub-group: 10.9mm, 3.7mm and 91.6o, mixed sub-group - 9.8 mm, 3.7mm and 85o and distal sub-group - 9.1mm, 3.8mm and 79.4o, respectively. There was a positive correlation between the length and the angle of division of the LCA, with the longest LCAs having the largest angle of division.
(b) Surgical notes: An IMLAD artery was present in 293 patients (21.7%). The prevalence was 20.2% (51/253) in females and 22.1% (242/1 096) in males. The IMLAD arteries extended into the interventricular septum in 3.8% (11/293) of the patients.
Discussion and Conclusion: The LCA with distally located lesions in its branches were recorded to have shorter lengths and smaller angles of division than vessels with proximal lesions. Morphometric parameters of the LCA may be predictive of a coronary arterial arrangement that may favour the progression of proximally located lesions. An IM course of the LAD artery is relatively common in patients undergoing CABG and poses a challenge in bypass grafting. Techniques used to address this anatomical variation at surgery are described.
THE STUDY OF INNATE LYMPHOID CELLS IN HIV INFECTED TISSUE
H N Kleverpris1,2, A Noorbhai4, W Kuhn5, M C Yadon1, D Ramsuran1, S Nhamoyebonde1, J Mjosberg3 and A Leslie1
1 KwaZulu-Natal Research Institute for Tuberculosis and HIV, K-RITH. Durban, South Africa
2 Dept. of Int. Health, Immunology and Microbiology, University of Copenhagen, Denmark
3 Center for Infectious Medicine, Karolinska Institute, Stockholm, Sweden
4 Department of General Surgery, King Edward Hospital, University of KwaZulu-Natal, Durban, South Africa
5 ENT department, University of KwaZulu Natal, Durban, South Africa
Innate Lymphoid Cells (ILCs) lack rearranged antigen receptors but share functional and developmental characteristics with lymphocytes and can be subdivided into three main groups according to their production of TH1, -TH2 and -TH17 cell-associated cytokines named ILC1, ILC2 and ILC3s, respectively. Recent reports demonstrate that ILCs play a crucial role in tissue homeostasis and repair in both non-infectious and infectious diseases. HIV-1 pathology involves lymphoid tissue destruction, particularly of the gut mucosa, leading to microbial translocation, immune activation and disease progression in most individuals, and limiting immune reconstitution of those taking antiretroviral drugs. We therefore hypothesized that, as ILCs play an import role in maintaining lymphoid tissue, this pathology may result from impairment of ILC function in HIV infected subjects.
Initial work in peripheral blood shows that ILCs are rapidly lost in early HIV infection, and that the level of ILC depletion in the chronic phase directly correlates with disease progression. We therefore next investigated the effect of HIV infection on tissue resident ILC populations. Using lymphoid tissue samples obtained from subjects undergoing routine gut biopsy and tonsillectomy we are able to isolate and characterize the main ILC populations. Preliminary data show overall reduction of ILCs in lymphoid tissue and, in the gut, skewing towards a natural cytotoxicity receptor positive ILC3 population. These findings are preliminary, but suggestive of a role for ILC modulation in HIV induced destruction of lymphoid tissue. Improved understanding of this crucial disease process will present new opportunities for therapeutic intervention to restore the function of the gut barrier and other lymphoid organs in HIV infected individuals. This work is ongoing and highlights the value of establishing long-term collaborations between surgical practitioners and bench scientists.
PIG MUCINS AND THE INHIBITION OF HIV-1
S Pillay1, A S Mall1, J R Dorfman2 And D Kahn
1 Division of General Surgery, University of Cape Town, South Africa
2 ICGEB Division of Immunology, University of Cape Town, South Africa
Sub-Saharan Africa is the world's worst HIV-AIDS affected region. More interventions to manage this pandemic are urgently required. This project sought to further describe findings that crude pig saliva and its purified mucins inhibit HIV-1 using an in vitro pseudoviral assay.
Pig saliva and gastric mucus were used in this experiment. Mucus was extracted in 6M guanidinium hydrochloride or in 0.02%NaN3+0.2M NaCl, and a cocktail of protease inhibitors, pH 6.5. Sepharose 4B gel filtration was used to separate salivary mucins into V0 (Muc5b + Muc19) and Vi (Muc7). Gastric mucins were purified by density-gradient ultra-centrifugation in caesium chloride. Dot blotting determined the purity and identity of the mucins. The inhibitory activity of crude and purified mucins was tested by their incubation with DU422 (Durban) subtype C HIV-1 pseudovirus and infection of susceptible epithelial tumour cells (genetically modified TZM-BL cells).
To date, only the pig saliva and gastric samples have been run on the pseudoviral assay. Crude and purified pig saliva as well as purified pig gastric mucus (Muc5ac+Muc6) inhibited HIV-1 in the above assay. Our current data shows purified pig saliva having the best inhibition of HIV-1, the IC50 of which, are comparable to our human salivary data. The neutralisation capability of Muc5b+Muc19 appears to be greater than the other mucins we have investigated.
In conclusion, pig salivary and gastric mucins inhibited HIV-1 in an in vitro pseudoviral assay, the best inhibition came from purified pig salivary mucins Muc5b+Muc19.
AN INVESTIGATION OF THE DEVELOPMENT OF A BIOCHEMICAL AND CLINICAL MARKER FOR GASTRIC DISEASE
R Chivaura1, E Panieri1, D Govender2, B Ndimba3, D Kahn1, and A Mall1
1 Division of General Surgery, University of Cape Town and Proteomics Group
2 Anatomical Pathology, University of Cape Town and Proteomics Group
3 Department of Surgery, Department of Medical Biochemistry, University of Cape Town, South Africa
Introduction: Gastric cancer is prevalent in the Western Cape region of South Africa and there is no suitable biochemical marker for pre-malignant disease. Previous work from our laboratory showed that a 55-65kDa glycoprotein associated with albumin, reproducibly fractionated with mucins from crude gastric mucus scrapings and gastric juice subjected to ultra-centrifugation in a caesium chloride density gradient. This protein was identified as α-1-acid glycoprotein (AGP) by its protein spots on 2D-SDS-PAGE staining with
Coomassie Blue. We sought to confirm the identification of the glycoprotein PAS spot and determine if AGP could be used as a clinical marker for pre-malignant gastric disease. We also determined the levels of MUC1, MUC4, MUC5AC and MUC6 in blood plasma and in gastric tissue (including MUC1c and MUC2), to ascertain if there was any correlation with the levels of AGP.
Methods: Human gastric mucus scrapings were collected after total or partial gastrectomy from Groote Schuur Hospital. Briefly the mucus scrapes were collected into 5.0ml of 6M guanidinium chloride containing 10mM EDTA, 5mM NEM and 1mM PMSF pH 6.5. After mucus purification by caesium chloride density gradient ultracentrifugation, glycoprotein identification was performed by Western blotting and staining with PAS. Samples which identified positive for glycoprotein were run on a 2D SDS-PAGE gel, stained with Coomassie Brilliant Blue then the spots of interest excised and run on a MALDI-TOF-TOF for identification.
Blood samples were collected from patients 3 days after the gastrectomy (n=14). Normal blood was collected from volunteers (n=15). The concentration of AGP was determined with a human ELISA kit using the provided protocol. The levels of MUC1, MUC4, MUC5AC and MUC6 in the plasma were determined using a sandwich ELISA. Gastric tissue blocks were retrieved from the archives of the Division of Anatomical Pathology, National Health Laboratory Service, Groote Schuur Hospital. The expression of AGP and mucins, MUC1, MUC1core, MUC2, MUC4, MUC5AC and MUC6 were determined in the gastric tissue by immunohistochemistry techniques.
Results: The PAS positive protein on both 1 and 2-D gels was identified as AGP. Levels of AGP in blood plasma were lower
in cancer patients (336μg/ml) than that of healthy controls (547μg/ml) (p-value=0.00006). This was also observed in the adenocarcinoma tissue where the AGP expression was lower than normal gastric tissue. Cancer plasma levels were lower than controls for MUC1 (p=0.00017) and MUC5AC (p-value=0.02308). No difference was observed in MUC4 (p-value=0.343) and MUC6 (p-value=0.379) plasma levels between the two groups. Tissue staining of MUC1 and MUC4 did not correlate with ELISA findings but a correlation was observed with MUC5AC and MUC6. De novo MUC2 expression was observed in adenocarcinoma and intestinal metaplasia tissue.
Summary: The lower levels of AGP-MUC1 combination in the blood of cancer patients would have potential as a marker for early gastric disease.
BURN SURGEONS IN SOUTH AFRICA: A RARE SPECIES
S Zoepke1, N Allorto2
1 University of Pretoria
2 Department of Surgery Pietermaritzburg Metropolitan, University of KwaZulu-Natal
Introduction: There is a high burden of burn injury in South Africa, which requires skilled surgeons, however there are few dedicated burn surgeons and few properly equipped units or centres in which to manage burns. The purpose of this study was to investigate the involvement of surgeons in burn care in South African hospitals and the deterrents that affect pursuing burn care as a career.
Methods: This is a prospective qualitative study. Voluntary and anonymous questionnaires were handed out to doctors at the South African Burn Society Congress in September 2013. The data was collated into a Microsoft Excel spread sheet.
Results: There was a 72% response rate (34 out of 47). Nineteen (63%) of the respondents were male and the majority (36%) were between 30 and 39 years. Post-graduate training in burn care was only received by 68% whereas 84% had learnt through hospital experience. Asked why they would become involved in burn care in South Africa, 54% said early exposure to burn surgery affected involvement, 46% mentor influence during training and 65% because burns is a rewarding field. By contrast, a deterrent to working in the burn field was predominantly the emotional stress (83%).
Discussion: The majority of doctors working in the field of burns are young. Although 40% are specialist surgeons, involvement in burns is part time. It is evident that there is insufficient training in burns in junior years with majority of respondents having gained their knowledge in burns by experience rather than formal training. Less than half are training interns in their current involvement in burns. The emotional stress is by far the biggest deterrent to working in burns and in contrast, the reasons why respondents work in burns is due to early exposure and influence by a mentor.
Conclusion: Increased focus should be placed on exposure and training of interns in the field of burns.
NEUROENDOCRINE TUMOURS: ARE CURRENT MANAGEMENT GUIDELINES PRACTICABLE IN DEVELOPING COUNTRIES?
P N Mthethwa & T E Madiba
Department of General Surgery, University of KwaZulu-Natal, Durban, South Africa
Background: Neuroendocrine tumours (NETs) represent a heterogeneous group of tumours. Although rare they are increasingly being diagnosed in our setting.
Aim: To evaluate hospital prevalence and clinicopathologic characteristics of NETs and to establish if our management approaches compare to international norms.
Methods:
• Ethical Approval: Biomedical Research Ethics Committee (UKZN): BE229/1
• Setting: Colorectal Unit in a tertiary hospital
• Design: Retrospective analysis of an on-going prospectively collected NET database into which all patients with NETs from the KwaZulu-Natal (KZN) Province of South Africa are enrolled. Patients are discussed at the Multidisciplinary clinic where treatment decisions are made. Data extracted included demographics, clinical presentation, disease distribution, staging, grading, treatment and follow-up.
• Endpoints: Long term follow-up, survival.
Results: Thirty patients have been enrolled over 13 years, including Africans (12, 40%), Indians (12, 40%), Whites (4, 13%) and Coloured (2, 6.7%). Thirteen were male and median age was 53.5 years. Change of bowel habit was the predominant presenting feature. Median duration of symptoms was 6.5 months. Four patients presented with tumour complications. The sites were foregut (11), midgut (6), hindgut (12) and unknown primary (1). The common specific sites were the rectum (8) and pancreas (6). Seventeen patients presented with metastatic disease with the liver being the most common target organ. The WHO grading was I (3), II (1) and III (27). Seventeen patients underwent resection resulting in R-0, R-1 and R-2 resection in 14, 2, 1 patients respectively. Patients received somatostatin or its analogues (11), chemotherapy (9) or no treatment (10). Median follow-up was 13 months. Four patients have developed new metastases during treatment, two of which were successfully treated with resection. Ten patients (33%) have been confirmed to have died.
Conclusion: Neuroendocrine tumours are an established disease which affects all population groups in KZN Province. Carcinoma is the most common histology. Foregut and hindgut tumours are more common. Late presentation is a problem. One third present with metastatic disease. Treatment approach and outcome is comparable to international trends.
COLORECTAL CANCER: DOES THE CLINICO-PATHOLOGIC TREND SEEN IN STATE HOSPITALS REFLECT THE GENERAL POPULATION IN KWAZULU-NATAL?
X H Ntombela, T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban
Introduction: Colorectal cancer is considered rare in some population groups in South Africa. A previous local study has suggested a varied population-based clinicopatologic pattern in state hospitals.
Purpose: To establish if the trends observed in the state hospital sector translates to the general population in the KwaZulu-Natal (KZN) Province.
Methods:
• Ethical Approval: Biomedical Research Ethics Committee (UKZN): E198/04
• Setting: Colorectal Unit in a tertiary hospital
• Design: Retrospective analysis of a prospectively collected KZN Colorectal cancer database which started in 2000. The 2009 cohort included both state and private patients and forms the basis of this study. Data collected included patient demographics, clinical presentation, site distribution, and staging.
• Outcomes: Demographics, pathological findings
Results: The study comprises 481 patients of whom 253 were male. The mean age was 62.7 ± 14.9 years. There were 88 Africans, 98 Indians, 47 Coloureds and 248 Whites of median ages 49, 60, 64, and 68 years respectively. Seven present presented at < 40 years (Africans 26%, Indians 2%, Coloureds 2%, and Whites 2%). The most common presenting symptoms were cChange in bowel habit (68), PR Bleeding (50), weight loss (47), abdominal pain (38) and abdominal mass (17). Median duration of symptoms was 5.5 months. The site distribution was proximal colon (107, 22%), distal colon (121 25%), and rectum (179, 37%). Ten per cent, 35%, 40% and 15% of patients had stage I, II, III and IV tumours respectively. Differentiation was moderate (296), poor (47), well (12), carcinoma-in-situ (6), mucinous (4) and undifferentiated (2). Staging, site distribution and tumour differentiation were similar in all population groups. Surgical resection was undertaken in in 311 patients.
Conclusion: Colorectal cancer affects all population groups. African patients tended to be younger at presentation with the highest proportion of those < 40 years of age. Late presentation is a problem. Staging, tumour differentiation and site distribution are similar in all population groups and reflect that in the state sector with some differences from that seen in the world literature.
RISK FACTORS FOR PEPTIC ULCER REBLEEDING L Kuttschreuter, J Klopper
Study Design: Case-Control study.
Aims & Objectives: Peptic Ulcer Disease (PUD) is common and rebleeding is expensive to both patients and the health care system. Current risk factors for rebleeding include age, shock, ulcer characteristics and ulcer lack of proton pump inhibitor (PPI) use. This project aimed to elicit the prevalence and risk factors for rebleeding peptic ulcers following initial endoscopic evaluation with/without medical management at a tertiary level academic hospital in South Africa.
Methods: Patients included presented with clinical or endoscopic evidence of upper gastro-intestinal bleeding, as well as identified peptic/gastric ulcer disease on endoscopy. Subdivision took place into 'non-bleeds' and 'rebleeds', with rebleed criteria being: new clinical or endoscopic features of bleeding, or a haemoglobin drop, following initial management. Two-group comparison was done to identify differences in patient-, disease-, or management-related variables.
Results: 84 patients were sampled (66 non-bleeds, 18 rebleeds) with a 21.4% incidence of rebleeds. Differences were found between the groups in age, history of smoking, alcohol use, NSAID use, admission systolic blood pressure, heart rate, formal haemoglobin, platelet count, endoscopic peptic ulcer appearance, time taken to PPI administration, route of administration, type of fluid given for resuscitation, use of and time to blood product administration (all p-values <0.05).
Conclusions: Patient- and disease-related factors can be used to identify at-risk individuals for peptic ulcer rebleeding. Management-related factors need to be avoided by modification of practices or development of treatment guidelines.
UNDERSTANDING OF MEDICAL ABBREVIATIONS ACROSS DIFFERENT MEDICAL DEPARTMENTS AT AN ACADEMIC HOSPITAL COMPLEX IN BLOEMFONTEIN
H E Rae, H Ally, W Mahomed, R Schanknecht, S Sealanyane.
School of Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
Introduction: Doctors need to communicate with colleagues from other medical departments in order to optimise patient care. Medical abbreviations are used to save time but they can be misinterpreted and lead to treatment errors.
Research Question: This study aimed at evaluating the understanding of common medical abbreviations in the Departments of Oncology, Surgery, Gynaecology, Paediatrics and Internal Medicine at the Universitas Academic Hospital, and the factors that may influence doctors' understanding of abbreviations.
Methods: In this prospective cross-sectional study, questionnaires were distributed for voluntary completion to all doctors at all levels of qualification currently working in the five Departments being sampled. It consisted of questions regarding graduation year, place of study, 35 medical abbreviations (seven from each department provided by the Heads of Departments), and doctors' experiences of abbreviation usage affecting patient care. Statistical analysis was done by the Department of Biostatistics at the University of the Free State. The study was approved by the Ethics Committee of the Faculty of Health Sciences at the University of the Free State. All participants received an information leaflet in English and Afrikaans, before participating in the study. All results were collected anonymously.
Results: The total mean score was 61.2%. Oncology abbreviations were least understood (29.1%) while Internal Medicine abbreviations were well known (74.4%). There were significant differences between performances of doctors from different departments with Oncology doctors scoring highest (71.6%) and Internal Medicine and Paediatric doctors scoring lowest (56% and 55.4%, respectively). Interns (63.2%) performed significantly better than specialists (57.2%). Non-standard medical abbreviations were poorly understood (40.2%) compared to standard medical abbreviations (70.8%).
Conclusion: There is sub-optimal understanding of medical abbreviations across medical departments. Use of abbreviations in multilingual environments may contribute to poor patient care and may be considered as negligence. We recommend that medical terms be written in full, the use of non-standard medical abbreviations be actively discouraged, and abbreviations only be used when they are widely understood and are accepted as standard terms.
THE SURGICAL OUTCOME OF CLEFT LIP AND PALATE REPAIR IN MADAGASCAR
M Fell, E Farley
Operation Smile South Africa
Introduction: Operation Smile is an organisation providing free surgeries to repair cleft lip, cleft palate and other facial deformities for children around the globe. Operation Smile aims to deliver life changing treatment to patients in some of the poorest areas of the world. A follow-up system has been designed to recognise and manage post-operative complications, therefore demonstrating their commitment to high standards of care.
Research Question: This study aimed to assess the surgical outcome of the operation smile model when a large number of patients were treated in a resource poor setting.
Materials and Methods: A prospective study was performed when a surgical mission was organised in Antananarivo, Madagascar, April 2014 with Operation Smile South Africa. Patients with cleft lip and/or palate (CLP) were initially invited for screening then nominated for surgical treatment which was delivered over a five day period. All operated patients were asked to attend follow-up one week after their surgery and assessed by a surgeon and an anaesthetist. Incidences of post-operative complications were recorded. Results were analysed via non-parametric Chi Squared test using Stats Direct.
Results: 782 patients came for screening over a two day period and of these, 151 with CLP received surgical treatment.151 patients were operated over five days, 90 were male and the mean age was 2.5 years. All operations were primary closures comprising 116 cleft lips (86 unilateral and 30 bilateral) and 35 cleft palates. During the operating period, one patient was returned to theatre for post-operative bleeding from a primary palate repair. At 1 week follow up, 140 out of 151 patients attended. There was one case of wound dehiscence in a cleft lip repair and 4 cases of fistula formation in the palate repairs. The relative risk of a complication in a palate repair was 13.3 compared to a lip repair at one week (p=0.012, 95% CI 1.47-355.84).
Conclusions: The considerable demand and need for the provision of care for patient with CLP was evident in Madagascar. The large number of patients who presented for screening, were operated and attended follow-up demonstrated that that the organisational model was working effectively. The overall complication rate was low. Whilst the lip repair has fewer complications than the palate repair it can be argued that both operations should be offered to this patient cohort. Further work should be aimed at improving the outcome of palate repair in this setting.
IMPROVING RATES OF NEGATIVE LAPAROTOMY IN PLACES OF LIMITED INVESTIGATIVE RELIABILITY
S Bola, J Cronje, I Dash
Ngwelezane Hospital, KwaZulu-Natal
Aims: Penetrating abdominal trauma can impose a difficult decision in balancing the risks of negative laparotomy and missing an intra-abdominal injury. In the west, negative laparotomy rates for penetrating trauma can vary from 1-24% with considerable morbidity rates. In rural South Africa, where trauma rates are high and resources low, we investigate the role of selective conservatism in managing penetrating abdominal injury.
Methods: Penetrating abdominal trauma was triaged in 2013 for patients that could undergo serial examinations and resuscitation. A prospective six-month audit of laparotomy findings for penetrating abdominal trauma was collated. Cases were only included if the peritoneum was breached. This was compared to findings listed in the theatre logbooks from 2010 and 2012.
Results: 87 laparotomies were performed in 2010 and 87 in 2012, of which the majority were positive-67% and 72% respectively. 81 laparotomies were performed in 2013, of which 78% were positive. There was availability of investigative resources (C.T and ultrasound) but not always the expertise to interpret findings. A notable increase in senior staff numbers within the department over the study period resulted in more clinical input on a Consultant level.
Conclusions: Clinical examination by a senior surgeon is a powerful indicator of intra-abdominal injury. It is important for institutions to invest in surgical expertise to be able to select appropriate cases for exploratory laparotomy and therefore reduce patient morbidity. The advent of trauma laparoscopy in this region can further avoid patients undergoing a negative laparotomy and reduce hospital stays.
OPERATION SURGICAL RESUS: IMPROVING RESUSCITATION IN NGWELEZANA
S Johnson, Y Squire, J Hickman, M Naidoo, M Fell
Ngwelezana Hospital, Kwazulunatal, South Africa
Introduction: Patients admitted to a tertiary level surgical trauma centre have a tendency to be critically unwell. An operation is often a crucial component of the management of these patients but the majority of care occurs in clinical areas outside of the operating theatre. Effective resuscitation of the critically ill surgical patient relies on having available equipment and relevant expertise.
Research Question: We determined the availability of resuscitation equipment for surgical inpatients and then use this information to improve awareness, understanding and execution of resuscitation in the acute setting.
Materials and Methods: A prospective study was undertaken to assess the resuscitation equipment available in surgical areas (wards, recovery, burns unit) at Ngwelezana Hospital. The Resuscitation Trolley Equipment Guideline produced by the Emergency Medicine Society of South Africa was used as the gold standard by which to make comparison. Teaching sessions were designed to question health staff about resuscitation and educate them in order to enhance their understanding and skill.
Results: Resuscitation trolleys in surgical areas were poorly stocked and the equipment that was present was often in poor working condition. The most commonly absent items were oxygen delivery devices (80%), portable oxygen cylinders (62%), suction devices (49%) and blood glucose testing kits (45%). Items that were consistently present but in variable conditions of operation included the defibrillator.
A list of missing items and an explanation of their importance was provided to the sectional operation managers. Additionally a checklist was created in accordance with the national guidance. Furthermore, a teaching session was designed for doctors and nursing staff. The doctors teaching session involved practical examples of resuscitation scenarios in the ward using the available equipment. The nurses teaching session focused on stocking and access to essential resuscitation equipment. The role of the nursing staff in the recognition of the critically ill patient and initiation of resuscitation before the doctors arrived was emphasised.
Conclusions: Resuscitation of surgical patients was hampered by a lack of available equipment and an inadequate knowledge of how to use the equipment. Raising awareness amongst staff via checklists and teaching sessions helped to improve care for the critically ill.
REVIEWING THE PRACTICE OF RELAPAROTOMY IN A DEVELOPING WORLD TERTIARY SURGICAL SERVICE: BENCHMARKING THE EXISTING PRACTICE AND OUTCOMES
M Scriba, G Laing, D L Clarke
Introduction/Background: The need for relaparotomy following abdominal surgery is associated with high rates of morbidity and mortality. Published research on the need for relaparotomy and the outcome practices in the developing world is scarce and there is not much consensus on the indications for relaparotomy. This audit reviews the spectrum and outcome of relaparotomy in a single tertiary centre in South Africa.
Materials and Methods: This study retrospectively reviewed data of all patients prospectively entered into an electronic registry over a 15 month period at Greys Hospital, Pietermaritzburg. All patients entered on the registry during the study period who had required an index laparotomy were entered into the study and used as the denominator to compare with all those requiring one or more relaparotomies. Simple statistical analyses were done using commercially available software. This study received full ethics approval from the Biomedical Ethics Research Committee of the University of KwaZulu-Natal (BE047/14).
Results: During the 15 month study period, 1294 patients required a laparotomy. Of these 106 patients required at least one relaparotomy, with a total of 163 relaparotomies, giving a relaparotomy rate of 12.59%. In patients needing relaparotomy, 98 (92.45%) had an emergency index laparotomy and 16 (15.09%) had a non-emergency index laparotomy. Of the relaparotomies, 45 (27.61%) were general surgical, 34 (20.85%) were paediatric surgical and 27 (16.56%) were trauma relaparotomies. Seventy two (67.92%) patients had only one relaparotomy, and 34 (32.08%) needed multiple relaparotomies. Seventy one (43.56%) were planned relaparotomies and 92 (56.44) were unplanned or "on-demand" relaparotomies. Overall mortality rate was 13.21% and 63.21% of patients needing relaparotomy had a significant morbidity. Of patients requiring only one relaparotomy, 52.78% had a significant morbidity and the mortality rate was 6.94 %, while those requiring multiple relaparotomies had a morbidity rate of 85.29% and a mortality rate of 26.47%. This equates to a 1.62 times greater rate of morbidity and 3.81 times greater rate of mortality when more than one relaparotomy is needed.
Conclusion: This study showed a high incidence of relaparotomies in the study population. The need for relaparotomy is associated with patients requiring emergency index laparotomies and is associated with significant rates of morbidity and mortality, with patients requiring multiple relaparotomies being the highest risk group.
THE USE OF GRADUAL CORRECTION WITH THE TLHEX EXTERNAL FIXATOR IN BLOUNT'S DISEASE
P Maré, D Thompson & M Barciela
Background: Recurrent or late presenting Tibia Vara is a complex clinical problem. In addition to the multiplanar deformity the disorder is often accompanied by obesity. Simple re-alignment osteotomy with acute correction is effective early in the disease. Its use in recurrent or severe deformities is limited by geometric constraints (mechanical axis translation), difficult fixation and the risk of compartment syndrome. Gradual correction with external fixation devices is a well-accepted technique in these cases. It has been shown to obtain accurate correction and provides stable fixation. This allows early weight bearing which facilitate consolidation and rehabilitation. Hexapod fixators are technically less demanding than standard Ilizarov techniques. The TLHex is a relatively new hexapod fixator available in South Africa. This is the first report on its use in Blount's disease.
Purpose: Evaluation of the result of gradual correction with the TLHex external fixator in Blount's disease in terms accuracy of correction, union and complications. Illustration of key hardware and software features.
Methods: A retrospective chart and X-ray review of 7 patients (9 legs) treated by gradual correction with the TLHex external fixator. Degree of correction of varus and procurvatum was assessed on pre-operative and post-correction X-rays. Internal rotation deformity correction was assessed clinically. Complications such as neurovascular compromise, minor and major pin tract infection and hardware complications were documented. The pre-operative planning, surgical technique and post-operative treatment protocol is reviewed.
Results: Mean varus was corrected from 21° (17° to 45°) to 1°(-2° to 4°). Mean procurvatum was corrected from 8° (0° to 25°) to 0° (0° to 8°). Internal rotation was corrected to between 5° to 10° of external rotation in all patients. Three patients needed one additional program to correct residual deformity (one over-corrected coronal aligment, one under-corrected saggital alignment and one rotational over-correction). The mean time in frame was 112 days. Three patients required oral antibiotics for minor pin tract infection. One patient required intravenous antibiotics and wire removal for major pin tract infection. One patient required frame adjustment after correction for soft tissue impingement. One strut loosened after consolidation prior to frame removal.
Frame pre-assembly allows easier mounting on a limb with complex deformity. The software allows for non-orthogonal mounting, which simplifies frame-mounting assessment. Double telescoping struts allow greater strut excursion and the outside mounting of struts on the ring increases mounting options for fixation elements.
Conclusion: Gradual correction of Tibia Vara with the TLHex external fixator is a safe and effective treatment method.
SHOULD APR BE CONSIDERED WHEN A DEFUNCTIONING STOMA IS REQUIRED FOR ANAL CANCER?
J C Kloppers; E D T Coetzee
Department of Surgery - UCT & Groote Schuur hospital
Introduction: Combined modality treatment (CMT) is the preferred treatment for anal squamous cancer, but a small subgroup needs a defunctioning colostomy with temporary intent.
Aim: The aim of this study is to evaluate the functional outcome and stoma closure rate of patients who needed defunctioning colostomies prior to CMT for anal squamous carcinoma (SCC) at Groote Schuur Hospital (GSH). The key objective being to assess whether abdomino-perineal resection (APR) is a suitable primary treatment modality for the subgroup of patients needing a defunctioning stoma prior to CMT.
Method: A retrospective chart review of all patients treated at the Combined Colorectal Clinic (CRC) at Groote Schuur Hospital with histological diagnoses of anal squamous carcinoma between 1995 and 2012. Patients who required defunctioning colostomies prior to CMT will be analysed in terms of demographics, indication for stoma, response to treatment and stoma closure rate.
Results: 125 patients were treated for anal SCC. Fifty eight were males and 67 females with a median age of 56 years. Thirty nine of these were deemed to require a defunctioning stoma prior to CMT. Thirty of these were treated with curative intent (22 males and 8 females). Indications for these stomas were obstruction (n=14); incontinence (n=8); pain (n=4); fistula (n=3) and sepsis (n=1). Three of the 30 patients' stomas were successfully reversed. Disease progression (n=15) was the leading reason for non-reversal of defunctioning stomas. Thirteen of the 30 patients who needed a stoma prior to CMT were clearly not resectable, while 6 were evaluated on the pre-treatment examination under anaesthesia (EUA) as resectable.
Conclusion: A defunctioning stoma prior to CMT is likely to be permanent. APR might be an alternative in cases where the tumour is resectable.
THE INCIDENCE OF RECURRENCE AFTER DELORME'S PROCEDURE FOR FULL THICKNESS RECTAL PROLAPSE - A RETROSPECTIVE PRIVATE-PUBLIC COHORT STUDY
J J Plaskett, R J Baigrie, P A Goldberg, D Kahn
Department of General Surgery, Groote Schuur Hospital, University of Cape Town
Background: Delorme's perineal repair has remained a procedure reserved for the surgical management of full-thickness rectal prolapse in the elderly and comorbid patient group due to its low operative morbidity and postoperative complication rates. Reported recurrence rates are higher than the abdominal approach.
Aim: This study attempted to assess the long-term clinical outcomes after Delorme's procedure with respect to recurrence rate and postoperative bowel function and compare these outcomes in a multi-surgeon public hospital and a single surgeon series in the private sector.
Patients and Methods: Retrospective cohort study which included all patients who underwent a Delorme's procedure for full-thickness rectal prolapse between February 2001 and March 2014 at either of the two primary study sites: Groote Schuur Hospital and Kingsbury Hospital (representing the public and private sector respectively). Patient data was collected from electronic records/database (Kingsbury Hospital) and paper folders/op notes (Groote Schuur Hospital). Primary outcome was absence of recurrence of full-thickness rectal prolapse after Delorme's procedure. Secondary outcomes included postoperative mortality, 30-day postoperative complication rate, postoperative bowel function (specifically with regard to faecal incontinence and constipation), and length of hospital stay. Short-term follow-up data was obtained from routine postoperative follow-up notes, and long-term follow-up data was obtained by means of a telephonic interview with patient/family member/primary caregiver.
Results: During the study period, 70 patients underwent a Delorme's procedure: 37 of these patients were operated on in a private hospital and 33 were operated on in a public hospital. The mean age was 71 years. There were 10 (14%) recurrences of rectal prolapse: 4 in the private cohort and 6 in the public cohort. Mean time to recurrence was 52 months: 53 months in private cohort and 6 months in public cohort. There were 6 minor (PR pain, PR bleeding not requiring reoperation or transfusion, urinary retention, confusion, hyponatraemia) and 6 major (PR bleeding requiring transfusion or reoperation, bowel obstruction, pneumonia, MI) complications and 2 postoperative deaths (pneumonia, MI). The mean postoperative hospital stay was 4 days.
Conclusion: Short-term follow-up results show the recurrence rate after Delorme's procedure for full-thickness rectal prolapse to be 14%, major and minor complication rate 8,6% respectively, and mortality rate 2,9%. This figure is lower than many published series.
ETHNIC DIFFERENCES IN CROHN'S DISEASE IN CENTRAL SOUTH AFRICA
O C Buchel1, W M Simmonds2
1 Surgery, University of the Free State, Bloemfontein
2 Medicine, University of the Free State, Bloemfontein
Introduction: Crohn's disease remains rare in black South Africans. Differences, if any, in disease characteristics, risk factors and outcomes in comparison to white patients have therefore not been studied.
Aim: To compare black and white patients within a cohort with Crohn's disease, followed up at the Academic Hospitals of the University of the Free State.
Method: Ethical approval: ECUFS 51/2012. Black and white patients with Crohn's disease, followed up since 2004 where included in this retrospective cohort study. Data were collated from patient records. Ethnicity, obtained from the patient registration system, was the independent variable. The Montreal classification was used. Continuous data were expressed as medians and compared using the Mann-Whitney test. Categorical data were compared using Fisher's exact test +/- the Freeman-Halton extension, as appropriate. Event rates where compared by calculation of the Poisson probability. A p-value of < 0.05 was considered significant.
Results: 38 patients (25 female, 13 male, ratio 1.9:1) with median age at diagnosis 34.5 years. Median follow-up was 8 years. There were 23(60.5 %) whites and 15(39.5%) blacks. Whites were diagnosed from 1973 to 2013 (41 years) and blacks from 2002 to 2013 (11 years). Gender distribution was: 17/23 (74%) white females and 6/23(26%) white males (ratio 2.8:1) vs. 8/15(53%) black females and 7/15 (47%) black males (ratio 1.1:1) (p=0.3). Median age at diagnosis was 34 for whites vs. 35 for blacks (p=1.0). Age at diagnosis, A1, A2 and A3 respectively, was 1/23 (4%), 14/23 (61%) and 8/23 (35%) for whites and 2/15 (13%), 9/15 (60%) and 4/15 (27%) for blacks (p=0.68). 16 (69.5%) whites and 5 (33%) blacks were active smokers at diagnosis (p=0.046). Disease location data were complete for 22/23 white patients and all black patients. Isolated small-bowel (L1), ileo-colonic (L3), and isolated colonic (L2) disease occurred in 8/22 (36%), 9/22 (41%), and 5/22(23%) white patients respectively and in 3/15 (20%), 7/15 (47%) and 5/15 (33%) black patients respectively (p=0.58). Median follow-up was 12 years for whites and 3 years for blacks (p=0.02). Whites had a cumulative follow-up of 335 patient years and blacks of 67 patient years. No white patient developed PSC in the follow-up period, but 2 (13%) black patients were diagnosed with PSC (rate 1/33.5 patient years; p<0.001).13/23 (57%) whites and 10/15 (67%) blacks had required a bowel resection (rate1/26 patient years for whites vs. 1/7 patient years for blacks; p<0.001). 1/23 (4%) white patient had died in the follow-up period and 2/15 (13%) black patients (mortality rate 1/335 patient years for whites vs. 1/33.5 patient years for blacks; p=0.018). The single death in the white cohort was post-operative. Both black patients who died had PSC. On excluding PSC from the analysis no difference in mortality rate could be shown (p=1.0). With PSC as the independent variable, the mortality rate was 1/8 patient years for patients with PSC vs. 1/386 patient years for the remainder of the cohort (p=0.001). Categorical comparison of deaths in PSC patients (2/2; 100%) to deaths in patients without PSC (1/35; 2.8%) confirmed a significant difference (p=0.004).
Conclusion: Age at diagnosis, gender distribution and disease location in Crohn's disease, appear to be similar between ethnic groups in our cohort. Black patients are less likely to be active smokers at the time of diagnosis and PSC developed exclusively in black patients. While the rate of bowel resection was 3.8 fold higher in black patients, the 10 fold increased mortality rate amongst blacks may be confounded by PSC. The shorter cumulative follow-up and period over which blacks were diagnosed, may indicate recently improved case ascertainment, true emergence of the disease in blacks or simple loss-to-follow-up of earlier cases. This requires further study.
CLINICOPATHOLOGIC SPECTRUM OF COMPLICATED COLORECTAL CANCER IN THE KWAZULU -NATAL TEACHING HOSPITALS
S J Mothae and T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban
Background: Up to 30% of patients present with complications, the most common being obstruction and perforation. Data on complicated CRC is lacking in South Africa.
Aim: To establish the prevalence of complicated CRC among patients presenting to the KwaZulu-Natal (KZN) Teaching Hospitals and to establish trends in presentation.
Methods:
• Ethical Approval: Biomedical Research Ethics Committee (UKZN): E198/04
• Setting: Colorectal Unit in a tertiary hospital
• Design: Retrospective analysis of a prospectively collected data from an on-going CRC database of all patients in the KwaZulu-Natal State Hospitals. Data on all patients with malignant perforation were extracted from the database and analysed, including demographics, presentation and treatment, outcome and follow-up.
• Endpoints: treatment outcome, mortality, follow-up and survival
Results: Out of 1479 patients with CRC enrolled from 2000 to 2013, 306 had complicated CRC (21%), of whom 175 were male. The patient profile is shown in Table I.

There were 4%, 37%, 23% and 37% stage I, II, III and IV tumours. Management of the complications was resection (233), Diversion (72), Stent (39) and conservative (1). Median follow up was 2 (1-108) months. Forty one patients are confirmed to have died (13%). Median survival 2 (1-108) months.
Conclusion: Complicated colorectal cancer accounts for 21% in our setting. Site distribution differs from that in the general CRC cohort but reflects international norms. Complicated CRC has a higher proportion of higher stage tumours and is associated with an appreciable mortality.
THE SIGNIFICANCE OF PRE-TREATMENT CARCINO-EMBRYONIC ANTIGEN MEASUREMENT IN COLORECTAL CANCER
Z Moolla, T E Madiba
Department of Surgery, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal
Background: The tumour marker carcino-embryonic antigen (CEA) is routinely measured prior to treatment in patients with colorectal cancer (CRC). Unlike diagnostic investigations it is widely available in South Africa. The usefulness of pre-treatment CEA measurement has not been investigated locally.
Aim: The aim of this study was to determine whether increased serum levels of CEA correlate with the presence of primary CRC, and its activity based on tumour site and metastatic status.
Methods: Patients referred to Inkosi Albert Luthuli Central Hospital between 2007 and 2013 with CRC and a pre-treatment serum CEA measurement were identified from a prospectively collected CRC database. Patient demographic data, site of tumour, metastatic status and baseline CEA activity captured. Serum CEA >5ng/ml was considered increased. Ethical clearance was obtained from the Biomedical Research Ethics
Committee (E198/04).
Results: One hundred and twenty of 201 patients had an increased CEA with an overall sensitivity of 60%. The mean patient age in the cohort was 56 years (SD ± 15). Serum CEA sensitivity increased in younger age groups with a sensitivity of 70% calculated in patients less than 40 years old. No significant difference in CEA sensitivity was found between African, Indian, White and Coloured race groups (p>0.05). Sixty seven patients (33.33%) had metastatic disease at time of CEA analysis. The median CEA increase in metastatic disease and locally advanced tumours were 27.51ng/ml (0.5 - 2678.17ng/ml) and 5.15 ng/ml (0.08 - 4908ng/ml) respectively [p<0.001]. Rectal tumours had higher median CEA levels than colonic tumours [12.04 ng/ml (0.08 - 1677.70ng/ml) versus 7.78ng/ml (0.50 - 2678.67 ng/ml); p<0.001].
Conclusion: The use of serum CEA level has not proven to be sufficiently sensitive to accurately correlate with primary CRC among all age and race groups. Significantly higher CEA activity was present in patients with rectal tumours and metastatic disease. Referral of patients with suspected CRC irrespective of CEA activity for endoscopic evaluation remains the definitive option.
ACUTE APPENDICITIS IN SOUTH AFRICA: A SYSTEMATIC REVIEW
E Yang1, D Kahn1, C Cook1,2
1 University of Cape Town
2 Oregon Health & Science University (USA)
Background: Acute appendicitis is one of the commonest surgical emergencies in the West, with a large body of research investigating risk factors for disease and perforation. As South Africa has a social environment, health system structure, and population demography unique from developed nations, findings may not be generalisable to this setting. A systematic review has not been performed for appendicitis research in South Africa.
Objective: This review systematically examines the literature on appendicitis in South Africa.
Methods: MEDLINE and EBM Reviews were searched for published literature on appendicitis and appendicectomy in South Africa up to March 2014. The reference lists of identified studies were searched further to identify relevant studies. Articles which were published in Afrikaans were translated into English for review. For all searches, the following specific search terms were used:
1. "Appendicitis AND South Africa"
2. "Appendectomy AND South Africa"
3. "Appendicectomy AND South Africa"
All peer-reviewed, published, original research studies addressing appendicitis in South Africa were eligible for inclusion in this review. For appendicitis and appendicectomy audits, inclusion criteria and methodology for defining appendicitis were used in determining inclusion in analysis. Recurring themes and observations by researchers were compiled and assessed. Racial categories were included to highlight research in differential determinants of disease and outcomes.
Research themes were analysed in the literature. Perforation rates, mortality, negative appendicectomy rates, and gender differences were analysed from audits for patients undergoing appendicectomy for acute appendicitis. Chi-square and Fisher's exact tests were used to compare categorical variables. There was no required institutional board review for this study.
Results: Ten audits were included in the quantitative analysis, with some being excluded in subgroup analyses. Negative appendicectomies occurred at a rate of 17.29% (580/3354). Women were more likely to have a negative appendicectomy than men (27.92% vs 9.46%, p<0.01). The perforation rate for appendicectomy patients was 36.1% (970/2688), and mortality rate was 1.22% (36/2946). Research efforts focused on investigating differential incidence and outcomes between racial groups within the country.
Conclusions: Appendicitis trends in South Africa are consistent with those in developing regions. However, there is a lack of research from the private sector. The findings in this review, along with some notable gaps in the literature, express the need for further research investigating appendicitis in the private sector, understanding why delays in care occur, estimating the prevalence and outcomes of laparoscopic surgery, and strengthening surgical services at the district hospital.
NEGATIVE APPENDICECTOMY: EVALUATION OF ULTRASONOGRAPHY AND ALVARADO SCORE
S G Mungazi, I Kundiona, O B Chihaka, G I Muguti
Surgery, University of Zimbabwe, Harare, Zimbabwe
Background: High negative appendicectomy rates are no longer acceptable with improvements in imaging techniques and clinical prediction rules. The use of ultrasound and CT scan in addition to clinical assessment and blood investigations has greatly reduced the negative appendicectomy rate to less than 10%. The aim of this study was to assess the negative appendicectomy rate at the two University Teaching Hospitals in Harare.
Objectives: The aim of the study was to determine the negative appendicectomy rate at the two major teaching hospitals in Harare and to evaluate the accuracy of the Alvarado score and ultrasound scan in diagnosing acute appendicitis.
Design: Prospective observational, cross sectional study.
Setting: Parirenyatwa Group of Hospitals and Harare Central Hospital, in Zimbabwe.
Materials and Methods: A total of 206 patients undergoing appendicectomy at the two major teaching hospitals in Harare were included in this study between June 2012 and May 2013. Information recorded included: age, sex, clinical features, investigations and treatment. Alvarado score was calculated from the data in the case notes and ultrasound scan results were also captured. All appendices removed at operation were sent for histopathological examination. Appendicitis was confirmed at histology. The positive predictive value of Alvarado score and sensitivity and specificity of ultrasound scan were calculated. The following patients were excluded from the study: children under 5 years, incidental appendicectomy, patients undergoing interval appendicectomy and patients with a mass in the right iliac fossa. Data was analyzed using Epi-info v3.5.3. Approval was sought from the Joint Research and Ethical Committee.
Results: The overall negative appendicectomy rate was 16.5%. The negative appendicectomy rate for men was 13.3% and that for females was 29.9%. The negative appendicectomy rate for Parirenyatwa Group of Hospitals was 19.0% and that for Harare Central Hospital was 12.1%. The mean age for the study was 28 years (SD 12.8). Appendicitis was diagnosed commonly in the second and third decades of life. Sensitivity of ultrasound scan in diagnosing acute appendicitis was 89.5% with a positive predictive value of 77.2%. Females were 2.6 times more likely to have an ultrasound scan done to diagnose appendicitis than males. Alvarado score had a sensitivity of 95.3% with a positive predictive value of 90.3%.
Conclusion: Negative appendicectomy rate (16.5%) at the two University Teaching Hospitals in Harare is relatively high when compared with modern trends. Alvarado score had a high sensitivity (95.3%) and predictive value (90.3%). Ultrasound scan had a high sensitivity (89.5%) and a relatively low predictive value (77.2%) in diagnosing acute appendicitis. Regular use of these assessment modalities should contribute substantially to reduction in the negative appendicectomy rate in our practice.
SERUM LIPASE SHOULD BE THE LABORATORY TEST OF CHOICE FOR SUSPECTED ACUTE PANCREATITIS
S Hofmeyr1, C Meyer2, B L Warren1
1 Division of General Surgery, National Health Laboratory Service, Stellenbosch University and Tygerberg Academic Hospital; Stellenbosch
2 Division of Chemical Pathology, National Health Laboratory Service, Stellenbosch University and Tygerberg Academic Hospital; Stellenbosch
Background: Serum lipase and amylase are adjuncts used to establish the diagnosis of acute pancreatitis. Despite lipase being shown internationally to be a more sensitive and specific test, amylase remains a popular first-line test. To provide a local basis for the recommendation of the best first-line laboratory test, an assessment of their performance in our local setting was undertaken.
Methods: A prospective database was kept on patients presenting with acute abdominal pain and raised serum lipase and/or amylase values. The sensitivity and specificity of serum lipase, amylase and their combination for the diagnosis of acute pancreatitis, as defined by the Atlanta classification, were calculated for the diagnostic threshold of three times the upper limit of normal.
Results: During the study period, 476 patients presented with acute upper or generalised abdominal pain and raised serum amylase and/or lipase values. The median age of included patients was 43 years (range 14-85), with 58% male and 42% female patients. 322 (68%) presented with abdominal conditions other than acute pancreatitis. 154 (32%) had acute pancreatitis. Ethanol abuse and gallstones accounted for 55% and 23% of acute pancreatitis patients respectively. Lipase displayed a sensitivity of 91% for acute pancreatitis, against 62% for amylase. Specificity was 92% for lipase and 93% for amylase. Dual testing with lipase and amylase had a sensitivity of 93%.
Conclusions: Lipase is a more sensitive test than amylase when utilising cut-off levels to diagnose acute pancreatitis. Lipase should replace amylase as the first-line laboratory investigation for suspected acute pancreatitis.
ROUX-EN-Y GASTRIC BYPASS VERSUS SLEEVE GASTRECTOMY - A META-ANALYSIS
S Nietz, M Brand
Surgery, University of the Witwatersrand, Johannesburg
Introduction: Bariatric surgery is an effective long-term treatment modality for morbid obesity and its associated comorbidities. Roux-en-Y gastric bypass (RYGB) is considered the gold standard in bariatric surgery. Despite a paucity of evidence sleeve gastrectomy (SG) has gained popularity even though currently there is no evidence proving superiority of SG over RYGB.
Research Question: The purpose of this meta-analysis was to determine whether SG is as effective as RYGB.
Materials and Methods: Randomized controlled trials (RCTs) comparing adults undergoing laparoscopic RYGB or SG for treatment of morbid obesity were compared in a fixed-effect model meta-analysis. The two review authors independently performed the selection of trials, assessment of risk of bias, and data extraction. Outcomes included measures of weight loss, improvement of comorbidities, procedure-related morbidity and mortality, and changes in gut hormone levels. We analysed dichotomous outcomes using risk ratios (RR) and heterogeneity was assessed using the I2 test. Ethical clearance was approved by the Human Research Ethics Committee of the University of the Witwatersrand.
Results: We included eight RCTs with 520 participants. No mortalities were reported. SG had lower rates of morbidity, re-operation and re-hospitalization, but this was not statistically significant. There was no significant difference between SG and RYGB for parameters of weight loss and diabetes resolution after 12 months follow-up. RYGB significantly improved dyslipidaemia and lowered leptin levels. SG lowered fasting ghrelin levels.There was no difference in PYY levels.
Conclusions: SG and RYGB are equivalent in procedural morbidity and mortality, weight loss and parameters of diabetes resolution after 12 months follow-up. RYGB has a superior resolution of dyslipidaemia.
STAGE IV COLORECTAL CANCER IN RESOURCE-LIMITED SETTINGS. 12 YEAR EXPERIENCE FROM THE KWAZULU-NATAL ACADEMIC HOSPITALS
S Kader and T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban
Ethical Approval: Biomedical Research Ethics Committee (UKZN): E198/04
Background: There is paucity of data on Stage IV colorectal cancer (CRC) in South Africa. Our hypothesis was that the proportion of Stage IV CRC was higher in South Africa compared to international norms.
Aim: To establish the hospital prevalence of Stage IV CRC in the KwaZulu-Natal (KZN) Province of South Africa and to document outcome in our resource-limited setting.
Methods: Setting: Colorectal Unit in a tertiary hospital Design: Retrospective analysis of an on-going prospectively collected CRC database. The study comprises patients with stage IV CRC enrolled between 2000 and 2012. Parameters analysed were demographics, clinical presentation, primary tumour site, site of metastasis, treatment and follow-up. Study endpoints: Clinicopathologic spectrum, follow-up and outcome
Results: Of 1449 patients with CRC, 322 (22%) had metastatic disease, comprising Africans (106), Indians (129), Coloureds (21)and Whites (67) which accounted for 21%, 22%, 33% and 22% of the respective CRC cohorts. Mean
age was 57.3 + 14.4 years and the median ages for Africans, Indians, Coloureds and Whites were 50, 59, 63 and 67 years respectively. There were 63 (20%), 81 (25%), and 174 (54%) proximal colon, distal colon and rectal tumours respectively. Common target organs for metastases were liver (242), lung (51), peritoneum (26), omentum (15), and ovaries (10). Treatment of the primary tumour was resection in 128 patients (40%). All patients except 10 received chemotherapy. Liver resections were performed only in 9 patients and chemo-embolisation in one patient. Median follow-up was 11 months and median survival was 7 months.
Conclusions: Metastatic disease accounts for 22% in our setting. African patients tend to be younger. Site distribution of primary tumour is similar to the general cohort of patients with CRC and to general norms. Metastatic resection rate and chemo-embolisation are infrequently offered.
WHAT IS THE CLINICOPATHOLOGIC SPECTRUM AND TREATMENT OUTCOME OF PATIENTS WITH LOCALLY ADVANCED COLORECTAL CANCER IN
KWAZULU-NATAL? N Manzini, T E Madiba
Department of Surgery, University of KwaZulu-Natal, Durban, South Africa
Introduction: Colorectal cancer is locally advanced if it is not possible to resect following the natural visceral fascial layer. There is paucity of data on this disease category in our setting.
Aim: To determine the clinicopathologic pattern, management and treatment outcome for locally advanced colorectal cancer.
Methods:
• Setting: Colorectal Unit in a tertiary hospital Biomedical Research Ethics Committee (UKZN): E198/04
• Design: The data extracted from an on-going colorectal cancer database forms the basis of this study and included demographics, clinical presentation, staging, management and outcome.
• Endpoints: Long term follow-up, survival
Results: Of 1449 patients with colorectal cancer in the KwaZulu-Natal (KZN) Province, 693 patients (48%) had locally advanced colorectal cancer (48%, 49%, 44%, and 47% for Africans, Indians, Coloureds and whites respectively). Mean age was 57.96 + 15.25 years. Median ages for Africans, Indians, Coloureds and Whites were 50, 62, 62.5 and 67 years respectively. Fifteen per cent presented at < 40 years (Africans 21%, Indians 7%, Coloureds 7% and Whites 3%). Colonic cancer occurred in 126 patients; 44 and 82 had cancers involving the proximal and distal colon respectively. Treatment was resection (89) no resection (36) and bypass (1). Twelve patients have been confirmed dead. Rectal cancer was seen in 567 patients. Resection was followed by adjuvant therapy in 126 patients; 238 patients received neo-adjuvant therapy prior to surgery; 41 patients received no onco-therapy. Palliative therapy was offered to 73 patients. A total of 328 patients underwent resection and there was no resection in 240 patients. Eighty five patients have been confirmed dead. Median follow-up for all patients was 71.5 months.
Conclusion: Locally advanced colorectal cancer accounted for 48% and is similar in all population groups. Site distribution is similar to the main colorectal cohort in KZN. Twenty-nine per cent of patients with colonic cancer and just under half with rectal cancer do not undergo resection.
A STUDY OF THE EFFICACY OF PORCINE DERMAL COLLAGEN (PERMACOL) INJECTION FOR PASSIVE FECAL INCONTINENCE IN THE COLORECTAL UNIT (CRU) AT THE WITS DONALD GORDON MEDICAL CENTRE (WDGMC)
N Harran, J Herold, B Bebington, D Lutrin
Donald Gordon Medical Center and the University of the Witwatersrand
The aim of this study is determine objectively if our patients with sphincter intact fecal incontinence (FI) or passive FI have an improvement in their symptoms post Permacol injection and if so, for how long does the effect last. As this is the only surgical option other than a permanent stoma available to these patients this is an important assessment.
In the phase 1 arm patients were assessed retrospectively from the 1st of January 2012 to 31st of December 2013. They were asked to complete a self-administered Wexner and FI QoL score based on their symptoms pre operatively and a second self-administered Wexner and FI QoL score post operatively. These were then assessed to determine the degree of benefit, if any.
In the phase 2 arm patients will be enrolled prospectively and recruitment will commence 1 April 2014. Recruitment will be closed on the 31st of December 2015. Patients will be asked to complete self-administered Wexner and FI QoL scores pre operatively and at the time, 1, 3, 6, 12, and 18 months to assess duration of response. Both phase 1 and phase 2 have been approved by HREC.
The results from phase 1 will be available for presentation. Phase 2 will only be available in 2016. As there have been no local studies to assess the efficacy of Permacol it will be interpreting to see if our findings equal the few international trials on this subject.
Poster Presentations
AN AUDIT OF TRAUMA SURGERY AT A LEVEL 1 TRAUMA CENTRE IN SOUTH AFRICA S Chowdhury, A J Nicol, P H Navsaria, S Edu, D Kahn
Trauma Center, Groote Schuur Hospital and University of Cape Town
Background: Groote Schuur Hospital Trauma Centre (GSHTC) in Cape Town has a role to play in the prevention and mitigation of trauma through the propagation of quality treatment and fulfilling the aim of the World Health Organization (WHO) declaration on emergency care for the injured.
Aim: An examination of the trauma care services at a level-1 Trauma Centre using best care principles as a means of accessing and improving the current trauma system in GSH.
Methods: A retrospective review of prospectively collected data of a cohort of patients admitted to the trauma surgery ward over a 3-month period (01Dec 2011 to 28 Feb 2012). All patients above 13 years of age acutely admitted to the trauma surgery ward following blunt or penetrating chest, abdomen, neck and peripheral vascular trauma were included. Surgical cases were categorised according to the Groote Schuur Hospital Emergency Surgical Case Categorization Chart (ESCCC) and complications were measured according to the Clavien-Dindo classification of surgical complications.
Results: A total of 300 patients were admitted. The mechanism of trauma was stab wounds in 204 (68%), 73 with GSW's (24.3%), and 23 (7.7%) blunt injuries. Two-hundred and seventy-nine (93%) patients were transported by the Emergency Medical Services (EMS). The ISS was >15 in 49%. The median delay for arrival at GSH from scene, Community Health Clinic (CHC), and secondary hospital were 1.5, 5 and 5.8 hours respectively (P < 0.001). Of 106 theatre cases 6, 47, 40 and 13 cases were booked as Red, Orange, Yellow and Green and the median delay for operation was 0.8, 2.0, 3.5 and 1.8 hours respectively. The delay from injury to theatre was a significant factor in the development of complications (P=0.02). Seventy-two cases (60%) of abdominal trauma were managed non-operatively (P <0.001). Of 33 GSW abdomen 24 (72.7%), and of 18 blunt abdominal trauma only 3 (16.7%) patients required surgery. The median stay was 3 days and 12 days for patients that developed complications (P<0.001). Only two patients died (0.7%).
Conclusion: Penetrating trauma continues to be a major burden on the resources of a Trauma Centre. There are delays in the transport of patients from the smaller hospitals and the direct trauma referral system needs to be strengthened. Non-operative management of abdominal trauma is a very important component of trauma surgical care and is decreasing the operative load on the theatres.
ANALYSIS OF 79 NECK EXPLORATIONS IN A MAJOR SOUTH AFRICAN TRAUMA CENTER
B I Monzon, M Mauser, R Pretorius, F Plani, A Mushtaq, V Jennings
Trauma Directorate, Chris Hani Baragwanath Academic Hospital
Department of Surgery, University of the Witwatersrand, Johannesburg
Background: Cervical trauma poses a great challenge to trauma surgeons; airway obstruction and exsanguinating haemorrhage are the most important immediate risk to life. The policy of mandatory exploration for penetrating neck trauma was introduced during the Second World War; however in the 1980s investigators observed that while operative mortality was declining with mandatory operation, the number of negative and non-therapeutic explorations was on the increase. This assertion radically challenged the old approach and lead to the introduction of the concept of selective non-operative management, the current "gold standard" of management of penetrating cervical trauma which while identifying early what patient requires surgical intervention also reduces the number of non-therapeutic and unnecessary interventions.
Methodology: A retrospective review of data from Unit's Medibank (www.medibank.co.za) Trauma Registry, spanning 42 months (1st January 2010 to 30th June 2013) A registry search using the key words: neck trauma, penetrating neck trauma and neck exploration was conducted; all patients who fit the search criteria were included except those declared dead on arrival. Data is presented raw; no tests of statistical significance have been applied.
Aim of Study: To analyse the clinical findings and final outcome (survival) in patients subjected to neck exploration at the Chris Hani Baragwanath Academic Hospital Trauma Unit.
Results: During the study period 10 500 major trauma cases were entered in the registry, of those 497 fitted the search criteria: 340 penetrating (302 stab wounds, 38 gunshot wounds) and 157 blunt injuries. Of the total only 79 (16%) underwent neck exploration, the rest (418) were treated using the Unit's protocol of selective non-operative management (SNOM) and are not discussed here.
Sixty-nine (87.3%) were operated for stab/incised wounds, 5 for GSW (6.3%), 3 for combined penetrating cervical-thoracic trauma and 2 for a blunt mechanism (impalement). Twenty-one comma six percent of patients were operated due to abnormal haemodynamia, 55,7% due to hard signs of vascular injury, 26,6% due to hard signs of aero-digestive trauma and 30,3% based on radiology reports of injuries (66,6% true positive). Near all (68/79 - 86%) were therapeutic interventions. There was only one mortality not related to the surgical procedure
Conclusions: There is a clear reduction of non-therapeutic interventions when a policy of SNOM is employed in patients with neck trauma.
PHYSIOLOGY CHARACTERISATION AND OUTCOMES OF PATIENTS AFTER EMERGENCY ROOM THORACOTOMY (ERT)
B I Monzon, J Goosen, M S Moeng
Department of Surgery, University of the Witwatersrand, Johannesburg
Introduction: An Emergency Room Thoracotomy is a resource intensive, high-risk procedure where rapid decision-making is essential.
Aim of Study: To analyse the outcomes of patients who underwent ERT to identify which group of patients achieved the most benefits from the procedure.
Methodology: A retrospective review of data collected of patients who underwent ERT, between 1st September 2005 and 31st December 2010 at a major trauma unit. Variables included: mechanism of injury, cavity involved, degree of physiological and metabolic derangement present at time of ERT, revised trauma score (RTS), injury severity score (ISS), and outcome (mortality). Patients declared dead on arrival were excluded. Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS), IBM Co.
USA. Results were considered significant when p < 0.5. the study was approved by the Human Research Ethics Board of the University of the Witwatersrand.
Results: Eighty-six (0,65 %) of the 13,279 major trauma cases managed at the Charlotte Maxeke Johannesburg Academic Trauma Unit (TU) during the study period, underwent ERT. Mortality was high [80.2%]. Patients with cardiac and or chest trauma fared better (survival 32.6%) compared to those with combined thoraco-abdominal or sub-diaphragmatic trauma, irrespective of mechanism. The majority of patients exhibited severe metabolic and physiological derangement on arrival.
Conclusions: The results of the series support the idea that ERT should be reserved for patients with a potential cardiac or pulmonary injury. Further studies may offer a better insight into this issue.
CLINICAL PRESENTATION, DIAGNOSIS AND SURGICAL MANAGEMENT OF PATIENTS PRESENTING WITH DCIS AT A SINGLE TERTIARY CENTRE
M Mutebi1, L Cairncross1, H Simonds2, E Panieri1
1 Endocrine and Surgical Oncology, Groote Schuur Hospital, Western Cape
2 Department of Radiation Oncology, Groote Schuur Hospital, Western Cape
Background: In situ carcinomas of the breast may constitute between 25-30% of all screen detected tumors in countries that practice routine screening 1. Of the in situ tumors, at least 80% are ductal carcinomas in situ (DCIS). In a local South African series conducted in the private health sector where some breast cancer screening is practiced, Mannell found a DCIS rate of 11.5% over 12 years with 165 patients undergoing breast conservation surgery. Similar findings were reflected by Edge and colleagues who demonstrated an overall DCIS rate of 13 % of all breast cancers seen in a series of 730 breast cancer patients. There is however, limited data on isolated DCIS in the public health sector in South Africa. In our clinical setting, mammography is diagnostic or done as opportunistic screening in breast or surgical clinics. This may account for a different presentation and incidence of DCIS diagnosed in our hospital.
Aim: To determine the clinical presentation of patients presenting with isolated DCIS at a single tertiary centre in the Western Cape. To review the diagnostic techniques most commonly used and the primary surgery performed for these patients.
Methods: This study was a retrospective chart review of patients presenting with DCIS from Jan 2005 to Dec 2012. Patients were identified from the oncology breast cancer database, the NHLS laboratory histological record and surgical operative notes.
Results: 42 patients with isolated DCIS were identified. DCIS comprised less than 1% (42/3768) of all breast malignancies managed in this period. There were 41 females and 1 male. The average age was 58 years. Most patients presented with a breast lump (23/42). 6 patients presented with nipple ulceration and 5 patients with a nipple discharge. 8 patients had their lesions picked on mammography. The diagnosis was made on core biopsy in 14 patients while 8 patients required excision of the palpable lump to make the diagnosis. 6 patients had a punch biopsy, 4 patients underwent a microductectomy and 8 patients required a stereotactic biopsy. 2 patients had a diagnostic ROLL performed.
In terms of primary surgical management, 23 patients underwent a primary mastectomy, 6 patients had a WLE and 6 patients had a ROLL with therapeutic intent. 3 patient declined surgery and 1 was transferred to a different unit. 3 patients were poor surgical candidates and were placed on tamoxifen only. In terms of axillary management, 9 patients had a concurrent axillary clearance and 9 patients had a sentinel lymph node biopsy. Of the 12 patients who had initial BCT (either ROLL or WLE), half required mastectomy for close or involved margins and two patients required re-excision of margins. Two patients had an immediate reconstruction and two underwent a delayed reconstruction. All the axillary node clearances and sentinel lymph nodes were negative for metastatic disease.
In terms of histology, the majority of patients had high grade DCIS (17/42). A Van Nuys score was determined for 10 out of the 12 BCT patients and came to a median score of 8/12.16 out of 31 patients were ER/PR positive.
Conclusions: Our incidence of isolated DCIS is much lower than that reported in other series. This could be explained by the late clinical presentation of our patients and lack of access to screening and diagnostic mammography. The commonest clinical presentation for DCIS was a breast lump which also differs from the experience in other parts of the world. The inappropriately high axillary clearance rate for our patients could be explained by diagnostic concerns over concurrent invasive disease and the previously limited availability of sentinel lymph node biopsy facilities.
DETERMINING THE ROLE OF SURGERY IN THE MANAGEMENT OF T4 BREAST TUMOURS
P Mapunda1, C A Benn1,2 and S Rayne1,2
1 Helen Joseph Breast Care Clinic
2 Health Sciences, University of the Witwatersrand, Johannesburg
Background: Locally advanced breast cancer at initial presentation is a common entity in South Africa. Historically almost all patients with T4 breast cancer were categorized as inoperable but current recommendations for developing countries suggest a multimodal approach to management, with surgery as a fundamental component normally after neo-adjuvant chemotherapy. The impact and success of surgery on this disease is still poorly described.
Aim: To determine the role of surgery in the management of patients presenting with T4 breast cancer.
Material and Methods: This was a retrospective records review over a three-year period of consecutive patients diagnosed with breast cancer at a government hospital treating an uninsured population.
Patient medical records were reviewed to collect demographics, including age and race. All patients with a histologically confirmed invasive breast cancer of any subtype presenting with the clinical stage T4NxMx were included (nodal status and metastases are not in the recruitment criteria). Radiology, histology and treatment plans were recorded. Follow up including recurrence and survival was also assessed. Data was analysed using simple descriptive and statistical analysis. A p-value of <0.05 was determined significant.
Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee.
Results: 87 patients were included with T4NxMx diagnosis. 65 (74.7%) were black, 13 (14.9%) were white and the remaining were either Indian or coloured (10.2%). Median age at presentation was 62 (range: 31-103 years). Young patients (<40 years) comprised 10% of the study population.
Treatment plans were recorded for 70 (80.5%) of patients. 91.4% received neoadjuvant chemotherapy, 4.3% had surgery first and 2.8% had radiation first. One patient refused all treatment. Surgery was carried out in 36 (51.4%) patients, and local recurrence occurred in 9 (25%). Patients with N2/3 nodal disease at presentation were significantly more likely to recur (p= 0.022) however this became less significant when alterations in treatment regimen were controlled for, as more patients with early nodal disease recurred. There was no significant difference in adjuvant radiation rates or biological sub-type between those who recurred and did not.
Conclusion: Patients with T4 tumours are not a homogenous group. Some patients will benefit from surgery as part of a multi-modal treatment regimen but a significant rate of recurrence (one quarter in this study) should be expected. This is increased by nodal disease and non-adherence to conventional multi-modal therapy. Recurrence is least likely to occur when neo-adjuvant chemotherapy is followed by surgery and then radiation in patients with a low burden of nodal disease.
EMPIRIC ANTIBIOTIC THERAPY FOR COMMUNITY ACQUIRED COMPLICATED INTRA-ABDOMINAL SEPSIS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL (DGMAH). ARE WE APPROPRIATE?
S R Motilall, N Kumar, M N Latakgomo, K Motilall, M Z Koto
Trauma Unit, Surgery, Dr George Mukhari Academic Hospital and the University of Limpopo - Medunsa
Introduction: The pillars of management of complicated intra-abdominal infections are a combination of source control and appropriate early empiric antibiotic therapy. In the era of increasing antibiotic resistance appropriately directed empiric antibiotic therapy would improve outcome as well as decrease antibiotic resistance.
Aim: In the department of General Surgery at DGMAH the combination of Cefuroxime and Metronidazole are the empiric antibiotics of choice for community acquired intra-abdominal infection (CAIAI). To assess its appropriateness we compared the antibiotic sensitivity profile of the most common organism involved in CAIAI to our chosen empiric antibiotic regime.
Methods: Retrospectively collected data of all patients who presented with CAIAI (i.e. perforated duodenal ulcer, appendicular abscess, or perforated appendix with free intra-peritoneal pus) from January 2012 to February 2014. Microbiological data was collected from the National Health Laboratory Service (NHLS) data bank. All patients were commenced on empiric antibiotics in the emergency department. All procedures were performed laparoscopically. At surgery intra-peritoneal fluid was collected and sent for microscopy, culture and sensitivity testing. Data collected included age, gender, procedure performed, bacteria cultured and their respective sensitivities. P-values <0.05 were considered to be statistically significant.
Results: Over the study period there were 145 patients who presented with CAIAI. Eighty patients were excluded as the data was incomplete. Of the remaining 65 patients, 51 (78%) were male. The average age was 28 years (range 7 years -74 years). All 12 (18.5 %) patients with perforated duodenal ulcers had Graham Patch repairs. Appendiceal abscesses (28 patients, 43.1%) were drained and appendectomies were performed. The perforated appendices (25 patients, 38.5%) all had appendectomies performed with peritoneal lavage. Thirty two (49.2%) patients had no growth on their cultures. In the remaining 33 (50.8%) patients the most commonly identified organisms were E.coli in 21 (64%) patients, Klebsiella in 5 (15%) patients and Pseudomonas in 2 patients (6%). E.Coli was sensitive to Cefuroxime in 14/21 (67%), Gentamycin in 14/21 (67%) and Amoxycillin-Clavulanate in 10/21 (48%) patients. Klebsiella and Pseudomonas were resistant to the above antibiotics but still broadly sensitive to most carbapenems.
Conclusion: The combination of Cefuroxime and Metronidazole as empiric antibiotics in our sub group of patients remains a reasonable option for CAIAI demonstrating a significant sensitivity for the most common organism namely E.coli. In the era of increasing carbapenem resistance it is reassuring to know that community acquired Klebsiella and Pseudomonas remain sensitive to most carbapenems. We hope this study will guide antibiotic stewardship at the DGMAH.
KI-67 A SURROGATE MARKER OF TUMOR DOUBLING TIME IN BREAST CANCER. A PILOT STUDY
D H Mokone, J H R Becker
Multidisciplinary breast clinic, Department of Surgery, Faculty of Health Sciences, School of Medicine Sefako Makgatho Health Sciences University, Dr. George Mukhari Academic Hospital
Introduction: The assessment of tumor cell proliferation and the calculation of tumor growth in vivo are at best flawed because of the inability to have access at cellular level. Mitotic index and grading does reflect -post hoc- to a degree on aggressiveness of growth. Ki-67 could be a "real-time" indicator of tumor growth.
Research Question: can the proliferation marker Ki-67 be used to measure the rate of cell division: tumor doubling time?
Method: A "biopsy" of 100 consecutive patients from the multidisciplinary breast clinic records will be analysed; and Ki-67 will be plotted against: age, stage, histological grading and receptor status. Trends will be observed and the feasibility of a prospective study.
Results: Stage 3+4, 81% (51+30 respectively), Infiltrating ductal carcinoma 73%, Grade 2+3, 88% (46+42 respectively), ER pos. 68%, PR neg. 55%, Her. Neg. 77%, Ki-67 53%>20, 38% (1-20)
Conclusion: Our patients are younger than reported in Western literature, are at more advanced stages, more have higher grades, with a high incidence of PR+HER negativity. More than 50% have a Ki-67 > 20%. The indications are that we are dealing with a subgroup of patients where the tumor doubling time is higher than the norm, <130 days. This finding needs to be further investigated, especially in our younger patients.
REFERENCES:
1. Specific Growth Rate versus Doubling time for Quantitative Characterization of Tumor Growth Rate .Esmaeil M, Et al, Cancer Research, April 15, 2007, 67; 3970.
2. Ki-67 is a prognostic parameter in breast cancer patients: results of a large population-based cohort of cancer registry. Inwald EC. Et al. Breast Cancer Research and Treatment. June 2013; 139(2): 539-52.
3. Estimates of breast cancer growth rate sojourn time from screening Database information. Michaelson J. et al. Journal of woman's imaging; 2003, 5, 1: 11-19.
LAPARASCOPIC INGUINAL HERNIA REPAIR: THE INEXPENSIVE WAYAPARA
M N Latakgomo, M Z Koto, O Y Matsevych
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus Dr George Mukhari Academic Hospital, Pretoria, South Africa
Introduction: Laparascopic repair is increasingly becoming popular method of addressing groin hernia problem. It allows widest coverage of myopectineal orifice, resulting in lowest recurrence rate in experienced hands. Associated with less operative pain; best and quick patient recovery; early return to work and normal activities.
Aim: To present our cost-effective laparoscopic approach.
Methods: Inclusion: Patients presenting with diagnosis of inguinal hernia, Informed consent. Exclusion: Hernia with complications ie strangulations, Incarceration, peritonitis; contraindication to general anaesthesia. We used re-useable instruments with no commercial balloon to create space. Total extraperitoneal approach using a 3D mesh, fixed using a protractor.
Data was prospectively collected using standard forms that were completed at end of surgery. Patients followed up at clinic after discharge; 2 weeks; 1 month; then on demand; to be recalled at 1 year.
Determination of secondary outcome: Complications, conversion to another procedure.
Organisation: Surgery was performed by/in the presence of consultant surgeon.
Results:
Data from January 2009 to date.
• 137 Patients (130 Males,7 Females). 129 Patients underwent Total Extraperitoneal Approach (TEP).
• 8 Patients were converted to Transabdominal Preperitoneal Approach (TAPP) due to technical difficulties
• Hernia type: (Direct n=58, Indirect n=79). Position: (Left n=56; Right n=66; Bilateral n=15). Recurrent: 12
• TAPP conversions: 2 early recurrences due to mesh migration/poor placement.
• 6 Patients had torn peritoneum with large air leaks.
• Recurrences: 2 early recurrences detected before discharge (following day). Patients underwent TAPP repair and recovered uneventfully.
• Mesh operative time: 90 minutes.
• Average hospital stay: 1,5 days.
• Complication: Penile/Scrotal haematoma: 6(8%): managed conservatively.
• Seroma: 11(16%):aspirated and resolved.
• Bowel injury: 1(1,5%):
• Mortality (Post operation MI):1(1,5%)
• 2 WEEKS: No recurrence. 1 MONTH: No recurrence
Conclusion: Laparascopic repair is a safe procedure in good, well trained hands.
TEP has lowest recurrence rate and least associated with complications. TEP highly feasible using low cost instrumentation
LOWER EXTREMITY AMPUTATION AMONG BLACK POPULATION OF THE EASTERN CAPE: GENDER AND AGE DISTRIBUTION
S Z Molaoa, L Mtimba
Nelson Mandela Academic Hospital and Walter Sisulu University
Background: Lower limb amputation is one of the oldest surgical procedures. It is the surgical procedure of choice in various surgical conditions, such as unreconstructible chronic peripheral arterial disease, advanced extremity malignancy, severe trauma and sepsis.
Level of amputation and the age of the amputee have impact on rehabilitation potential of the amputee. Above the knee amputees expend more energy on walking with prosthesis than their below the knee counterparts.
Prevalence of Peripheral arterial disease; as determined with Ankle brachial index of < 0.9, among asymptomatic Black patients seen at Mthatha General Hospital, was estimated at 29.3%. It was postulated that a significant number of these would probably end up with a major amputation (Paul, AK; Mash, B and Rupesinghe (2007).
Objectives: To determine age and gender distribution of the amputees.
Materials and method: This is the retrospective review of theatre record of emergency amputation from January, 2012 to December, 2013. Data on gender, age, and level of amputation was extracted. Records were grouped into below 50, 50-69, and 70 and above year age categories. Proportions and level of amputation by age and gender was determined.
Results: 201amputations from the emergency register were reviewed. There were 125 (62%) men and 76 (38%) females, with mean age of59 (+/- 14.8 years). Female amputees were slightly older than their male counterparts (mean age: 61.8 +/- 13.5 years, versus 57.6 +/- 15.4 years), which was statistically significant (p-value=0.0477). Men were more likely to undergo amputation (62 %, 95 CI = 55- 69%) than females (38%; 95% CI = 31- 45%).
Of 201 amputees, 188 (93.5 %) were major amputations (ABK or AKA) and there were 13 (6.5%) minor amputations (TMA or digital).
Men were more likely to undergo major amputation than their female counterparts. 120 (64%) were males of whom 38(32%) were AKA, and 82 (68%) were BKA, whereas, 68 (36%) of female major amputees, 17(25%) were AKA, and 51(75%) were BKA. Female major amputees were more likely to have BKA than their male counterparts, OR: 1.39.
More major amputations were seen in the 50-69 year age category (52%) in comparison to under 50, and 70 and above (23% and 25%, respectively). Males predominated both AKA and BKA in all categories.
Conclusion and recommendations: Men are more likely to undergo major amputations at an early age than females, and are more likely to undergo both AKA and BKA than females. Determination of ABI in at-risk groups and timely institution of secondary preventive measures may be worthwhile.
MORTALITY IN PAEDIATRIC BURNS VICTIMS: A RETROSPECTIVE REVIEW FROM 2009 - 2012 IN A SINGLE CENTRE
B Jugmohan, J Loveland, L Doedens, R Moore, C Westgarth-Taylor
Department of Paediatric Surgery and Paediatric Critical Care, Chris Hani Baragwanath Academic Hospital, University of the Witwatersrand, Johannesburg,
Background: Childhood mortality is high in the developing world. Burns is one of the 5 leading causes of childhood mortality in South Africa. Whilst there is an abundance of literature on burns in the developed world, there is a paucity of publications dealing with childhood mortality related to burns in Africa, and South Africa in particular. We describe the mortality of children admitted to a dedicated paediatric burns unit.
Methods: A retrospective review was performed of patients admitted to the Johnson and Johnson Paediatric Burns Unit, Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa, between May 2009 and April 2012.
Results: 1372 patients between the ages of 0 to 10 years were admitted to the unit during the study period. There were 1089 admissions to the general ward and 283 admissions to the intensive care unit. There were 109 deaths (mortality7.9%). 50.4% of deaths occurred in children less than 3 years old. 90.8% of deaths occurred in children aged 5 or younger. No child with a burn injury > 60% total body surface area survived.
Conclusions: Our overall mortality rate is lower than the national childhood burns mortality rate (7.9% vs 14.1%). Our mortality rate is lower than that quoted in countries in Africa and the East Mediterranean. The majority of mortalities occurred in children less than 5 years old. The mortality rate has declined since the introduction of paediatric intensive care specialists into the unit. Massive burns (total body surface area > 60%) are uniformly fatal in our unit.
AN AUDIT OF TRAUMA MORTALITY IN THE PIETERMARITZBURG METROPOLITAN COMPLEX
N B Moodley, C Aldous, D L Clarke
Department of Surgery, Nelson R Mandela School of Medicine, University of Kwazulu-Natal
Introduction: The trauma epidemic in South Africa has been well documented over the years and we have learnt a great deal from the literature that has been generated. Due to poor record keeping, hospital based mortality data has not capture the actual mortality rate, as many corpses are taken directly to the state mortuary. This has resulted in a significant under reporting of trauma related mortality rates.
Research Question: This study presents a comprehensive overview of the forensic mortality data for trauma in an urban metropolitan complex.
Materials and methods: This study took the form of a retrospective audit for a two year period by accessing State Medico-legal Mortuary records of all trauma-related deaths in the Pietermaritzburg Metropolitan area. All self-inflicted deaths and burn victims were excluded from this study. Ethical approval from the local Biomedical Research and Ethics Committee was obtained prior to commencing the study.
Results: There were 1105 trauma victims who demised during the January 2010 to December 2011 period, 471 of whom survived long enough to be admitted to a medical facility. There were 930 (84%) male deaths and 175 (16%) female trauma related deaths. The mortuary group consisted of (56%) blunt trauma and (44%) penetrating trauma victims. Of the blunt trauma related deaths 153 (25%) were secondary to assault and 462 (75%) secondary to a road traffic collisions (RTC). Of the penetrating trauma victims there were 181 (37%) GSW victims and 309 (63%) stab victims. The three leading causes of trauma-related deaths were head injuries (33%), polytrauma (30%) and chest injuries (27%). The scene of the deaths was as follows: On scene (n=584~53%),Edendalehospital(n=259~24%), GreysHospital (n=144 ~ 13 %), Northdale Hospital (n=68 ~ 6%) and primary health care clinics and private hospitals in Pietermaritzburg (n=50 ~ 4.5%).
Conclusion: Pietermaritzburg metropolitan complex has a very high rate of trauma related mortality, which is in keeping with high rates of interpersonal violence and RTC's. The trauma system in the city is immature and this results in a significant number of second phase deaths, which are potentially salvageable. The ongoing distribution of severely injured trauma patients to inappropriate facilities is a cause for concern and needs to be addressed by the enforcement of referral protocols.

PREDICTIVE VALUE OF A PERSISTENT TACHYCARDIA TO INDICATE IMPENDING PERFORATION IN NECROTIZING ENTEROCOLITIS
F van der Schyff1, J H R Becker2
1 Department of Surgery, Faculty of Health Sciences, School of Medicine, University of Pretoria
2 Department of Surgery, Faculty of Health Sciences, School of Medicine, University of Limpopo (Medunsa Campus)
Background: Necrotizing enterocolitis (NEC) is a devastating disease of infancy. The disease not only affects preterm but also term infants to various degrees. Mortality rates range from 40 - 100% in infants with fulminant NEC, bowel perforation and soiling. Surgical intervention is often the only option to prevent mortality. The timing of this surgical intervention is of critical importance. It has been shown that the best time to operate on these infants is after gangrene of the bowel has set in, but prior to perforation. Identifying infants at risk of disease progression and possible bowel perforation will allow pre-emptive management1. Infants compensate for metabolic stress with a tachycardia, they have an inability to increase cardiac stroke volume.
Research questions:
1. To determine whether a persistent tachycardia in a fully resuscitated infant with proven NEC is indicative of disease progression, full thickness bowel wall necrosis and therefore impending perforation. This will allow the clinician to use the clinical sign of tachycardia to determine the optimal time to operate on these infants in a timely fashion.
2. Which other risk factors may further guide the clinician in identifying those infants at risk of progressing to fullblown disease and may require surgical intervention sooner.
Methods and Materials: This retrospective study is being conducted in the Neonatal Intensive Care Units of Steve Biko Academic Hospital and will in future include data from the Royal Hospital for Sick Children in Glasgow. All neonates with proven NEC in these institutions will be included in the study. Data is being collected from the relevant ICU files from the time of admission to the date of discharge. Should the child go to surgery, operative notes are studied to determine whether the surgeon found perforation of the bowel present. A relationship between a persistent tachycardia in infants with NEC and impending perforation are sought as well as the presence of possible other risk factors. Ethical approval for this study has been granted by the Ethics Department of the University of Pretoria.
Results: Thus far the ICU data of 50 children diagnosed with NEC has been studied and 22 were suitable. Children were divided into two groups: those who progressed to full thickness bowel necrosis,16/22 and those that resolved on conservative treatment, 6/22. It was found that in terms of gender, mode of delivery, HIV exposure, maternal age and special investigations e.g. pH, lactate, platelet count etc. no difference was shown between the two groups. For both groups, the following parameters were similar: average gestational age, 31/52, birth weight 1.2kg. Head circumference and body length and Apgar scores. On admission, 25% of the children in the progression group were already haemodynamically compromised, and 50% had free air on abdominal X-rays. Time of presentation in the progression group was day 11 and in the non-progressive group was day 17. A persistent tachycardia 72 hours prior to surgery was observed in the progression group. The pulse rate in the non-progressive group remained variable around a baseline.
Conclusion: This study conclusively demonstrated that a persistent tachycardia is an important indicator of pathological progression to full thickness bowel wall necrosis and perforation. An additional observation was that the children in the progressive group presented 6 days earlier with no significant differences between the two groups in terms of traditional parameters.
REFERENCES:
1. Banieghbal M.B. et. al., "Surgical indications and strategies for necrotising enterocolitis in low income countries". World J.Surg. 2002; 26,444-447.
PRESENTATION OF PROSTATE CANCER AT A REGIONAL HOSPITAL IN KWAZULU-NATAL H A le Roux, R J Urry
University of KwaZulu-Natal, Greys Hospital, Pietermaritzburg
Introduction: We have observed that patients diagnosed with prostate cancer at Edendale Hospital are more likely to present with advanced or aggressive disease. These patients are all Black men from rural and peri-urban populations.
Aim or Objective: To investigate the demographics and serum PSA values of patients diagnosed with prostate cancer at Edendale hospital, and to assess the clinical stage and histological grade of their cancers.
Method: All patients diagnosed with prostate cancer at the Edendale Hospital between 1 March 2012 and 31 March 2014, are included in a retrospective chart review. A clinic database of patients with prostate cancer was used to obtain the study patients.
Results: Preliminary results of the first 46 patients reviewed revealed mean age of presentation of 67.6 years (range 56 to 91 years). The median PSA was 172.5ng/ml (range 5.7 to 11084ng/ml). On diagnosis, 61% of patients already had metastatic disease, 24% had high-risk or locally advanced disease and only 15% had low- or intermediate-risk organ-confined disease.
Conclusion: The majority of patients diagnosed with prostate cancer at Edendale hospital already have metastatic disease on presentation. These patients have no potential for curative treatment and have a worse prognosis than patients diagnosed with organ confined disease.
THE INCIDENCE OF AN ELEVATED ADMISSION SERUM POTASSIUM IN CRUSH INJURY PATIENTS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
S R Motilall, N Dube, N Kumar, A Kirpichnikov, M Z Koto
Trauma Unit, Department of Surgery, Dr George Mukhari Academic Hospital and University of Limpopo - Medunsa
Introduction: Hyperkalaemia is a significant concern in crush injury patients. This concern determines the choice of the initial resuscitation fluid i.e. a non-potassium containing fluid which is usually normal saline.
Aim: The aim of this study was to determine the incidence of an elevated serum potassium (sK) on admission in patients with crush injury at the Dr George Mukhari Academic Hospita.l
Methods: Retrospective review of data collected from March 2013 - February 2014 in all patients who had a clinical suspicion of a crush injury. Patients were resuscitated as per ATLS principles. Fluid diuresis was predominantly with normal saline, however Balsol or Ringers Lactate were also used. Creatine Kinase (CK), urea and electrolytes (U&E) were part of the initial blood screen. The U&E was repeated within 24 hours and repeated again if deranged. Crush injury was defined as a CK > 1000 U/L within 24 hours of admission. Normal sK was defined as (3.5 - 5.1mmol/l). Data collected included age, gender, CK, sK on admission. P values < 0.05 were considered clinically significant.
Results: Sixty one patients presented with a clinical suspicion of crush injury. Twelve patients were excluded because of incomplete data. In 3 patients CK remained below 1000 IU/L and they were excluded. The remaining 46 patients were all male. Average age was 27 years (range 17 - 64 years. Average CK over the first 24 hours was 2889 (range 1149 - 9417 IU/L). Only 1 (2.2%) patient had an elevated sK (6.2mmol/L) on admission and his sK normalised within 24 hours. His CK was only 2523 IU/L. The remaining 45 (97.8%) patients had no hyperkalaemia on admission with 6 (13%) patients actually having hypokalaemia (range 2.9 - 3.4mmol/L). In the 2 (4.3 %) patients requiring dialysis for oliguria, pulmonary edema and acidosis the sK remained normal (3 days) up to the initiation of dialysis. Interestingly in 7/46 (15.2%) patients, Ringers Lactate (6 patients) or Balsol (1 patient) was used as the primary resuscitation fluid. Repeat sK in these 7 patients remained normal.
Conclusion: These results demonstrate that hyperkalaemia on admission in patients with crush injury has a very low incidence. The argument of using non-potassium containing resuscitation fluids in crush injury patients for this same reason may not be valid. In the few patients in whom a potassium containing fluid was used, hyperkalaemia was not a problem through the entire admission.
THE COSTS OF DELAYED TREATMENT IN BURNS -A COMPARATIVE CASE STUDY
J Govindasmy1, G Oosthuizen1, C Aldous1; P Barker2
1 University of KwaZulu-Natal, South Africa
2 Headquarters, International Committee of the Red Cross, Geneva
Introduction: It is widely accepted that burn-injury recovery is significantly improved when treated actively and rapidly in the acute phase of the injury with early resuscitation, early surgical debridement, appropriate wound care and cover.
However, the reality is that many patients are not afforded this approach. This paper looks at the costs involved in delayed treatment for acute burn injury.
Method: The case comparison is between 2 children burned with hot water, both with similar distribution and % burn-TBSA. One patient was admitted directly to the regional burns unit. The 2nd patient was managed at the district hospital for 6 weeks before transfer to the regional burns unit.
Results: Some of the comparative costs incurred at the regional burns unit at Edendale Hospital Burns Unit (EDH BU), are tabulated below:
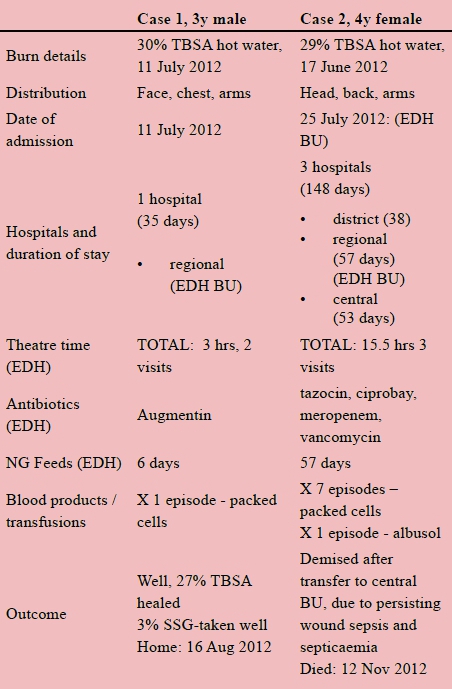
This case comparison is done to demonstrate the range of costs incurred when a burn-injury patient is not actively and appropriately managed. It highlights that the costs are not just monetary, but includes time, labor, blood products, antimicrobial use, dressing resources, and more. Appropriate burn-care is not just a key for survival but perhaps more importantly, a sword to protect the quality and dignity of the lives in our care, as healthcare professionals.














