Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.2 Cape Town jun. 2016
ABSTRACTS
Abstracts of the 41st Annual Meeting Surgical Research Society of Southern Africa
Hosted by the Department of Surgery, University of Limpopo, Medunsa Campus. Held at Roodevallei Conference Venue, Kameeldrift East, Zeekoegat, Pretoria. July 4 & 5 2013
Oral Presenations
MICROBIOLOGY AND ANTIBIOTIC RESISTANCE IN SEVERE BURNS : A 5 YEAR RETROSPECTIVE REVIEW IN A SPECIALIST ADULT BURNS UNIT
I Bahemia, R Moore, A Magunza
Burns Unit, CH-Baragwanath Hospital, Soweto, Johannesburg
Introduction: In the ICU setting, the highest rates of primary bloodstream infection in patients with central venous catheters is found in Burn Intensive Care Units (BICU). A knowledge of the spectrum, incidence and antimicrobial sensitivities of the micro-organisms causing septicaemia within each institution's BICU is important as it informs and directs empiric antibiotic therapy for the septic patient. It also allows for more effective infection control measures.
Methods: This is a retrospective study of patients admitted to the Adult BICU, Chris Hani Baragwanath Academic Hospital (CHBAH BICU) from 1 January 2008 - 31 December 2012. Patient files and National Health Laboratory Service (NHLS) records were accessed to obtain the relevant data.
Results: 58% of patients admitted to CHBAH BICU in the 5 year analysis period had positive microbiological cultures. The mortality rate during this time was 36%. Methicillin resistant Staphylococcus areus (MRSA) and Acinetobacterbaumannii are the two most prevalent organisms in the CHBAH BICU. Antiobiogram to follow.
Conclusion: The microbiology profile in CHBAH BICU is similar to that described in several overseas BICUs. Interestingly, the profile is closest to that of the "tropical" Singapore BICU. The antibiogram will allow us to assess the appropriateness of our current empiric antibiotic protocol for patients who develop sepsis.
BLOOD TRANSFUSIONS IN BURN PATIENTS IN A REGIONAL BURN SERVICE
N L Allorto, M D T Smith, C Aldous
*Department of Surgery, Pietermaritzburg Metropolitan Complex, University of Kwa-Zulu Natal
Introduction: Bleeding during burn excision is substantial. Blood is a scarce and costly resource in our setting. Literature suggests that a more restrictive strategy is acceptable. We aimed to obtain a quantitative idea of actual blood consumption in burn surgery as well as doctor's opinions on transfusion triggers. No protocol currently governs practice.
Methods: Ward, theatre and blood card records of patients admitted with a burn injury were scrutinized for a 12-month period in Edendale Hospital. All patients requiring burn surgery were included. Age and weight of the patient, percentage surface area burn operated on, day post burn and total blood received were recorded. A questionnaire was given to anaesthetists and surgeons at Edendale Hospital.
Results: Seventy peri-operative transfusions were given. These included 22 children and 23 adults. An average TBSA of 23 percent (range 2.5 - 35%) was operated on which included debridement and or skin graft, done on average day 23 post burn (range 1 - 102 days). A total of 24.6 litres of red cells were transfused which is 1.2 mls/kg/% TBSA. Average haemoglobin pre operatively was 9.6g/dL and 9.9 g/dL post operatively. Sixty percent of anaesthetists and 70 percent of surgeons preferred a higher pre-operative haemoglobin for burn surgery compared to other procedures.
Conclusion: Burn wound excision consumes a significant amount of blood. Clinicians favour higher transfusion triggers for burns patients despite the significant risks of transfusion and evidence for a restrictive strategy. We need to address our approach to such a limited and valuable resource.
CHEMICAL BURNS: A SINGLE-CENTRE EXPERIENCE
D den Hollander
Burns Centre, Inkosi Albert Luthuli Central Hospital, Durban
Introduction: An increase in the number of chemical injuries since January of this year prompted us to review our experience with chemical burns
Methods: A chart review was undertaken of all burn injuries managed at the Burns Centre at IALCH was done. Information extracted was: age, gender, mechanism of injury, size and depth of burn, length of stay, complications and mortality.
Results: Between March 2007 and May 2013, 23 patients were admitted with chemical burns. Three were children under the age of 2, and one was a child of 9. The average age of the remaining patients was 32 years. Male: female ratio was 17: 6. Ten burns were non-accidental (9 assaults and 1 parasuicide), and 11, amongst which were all pediatric cases, were accidental. Of the 9 assaults 5 were seen since January 2013. Accidental cases occurred most commonly at home. Only 2 burns were the result of an IOD. Average TBSA burnt was 16% (range 3-35%). Patients underwent an average of 2.5 surgical procedures. Average LOS was 30.6 days. Five patients suffered loss of vision, 3 developed early contractures and 2 patients died.
Conclusion: Chemical burns are an uncommon injury in the Public Sector in South Africa, and are usually accidental in nature. However, as has been reported elsewhere in the world, assaults with chemical agents reveal an increasing trend.
THE BURDEN OF BURNS CARE AT A REGIONAL HOSPITAL IN REGION 4, KWAZULU-NATAL
M Naidoo, N Panday, T E Madiba, D L Clarke, C Aldous
Department of Surgery, University of KwaZulu-Natal and Ngwelezana Hospital
Background: Burns injury is a serious cause of morbidity and mortality in rural Kwazulu-Natal. Fire is often the only source of energy and warmth in rural areas where there is no household electricity.
Aim: To carry out a situational analysis of the current state of burns care in Region 4, in order to inform further planning of burns services. We aimed to identify problems pertaining to delayed transfers, resuscitation and burns dressing.
Methodology: Daily ward round lists and intake reports for the Ngwelezana burns unit were analysed from 1 January 2013 until 31 March 2013. Data collected included epidemiological information, surgery performed and morbidity and mortality.
Results: A total of 189 patients were admitted into the Ngwelezana burns service. 42 (21.5%) were adult male, 42 (21.5%) adult female and 107 (56%) paediatric. 61% were referred from the local drainage area,. 67% sustained 10% or less burns, 9% 10-15% TBSA , 1% between 15-25% TBSA and only 2% over 35% TBSA. There were a significant number of problems with the transfer protocol. The commonest being the inaccurate initial assessment of the burn surface area (incorrect in 55% of cases). Mortality was 15 (7.9%).
Conclusion: Children are prone to predominantly hot water burns (85%) and open flame burns (13%). These are largely preventable burns. Patients transported vast distances (Average = 172km) are frequently inaccurately assessed. In Adults, epilepsy is a significant contributing factor to burn injury (8%).
Burns care assessment and treatment is poor in the Burns service referral hospitals. Intervention by way of training of district hospital doctors will help to improve adherence to the transfer protocol. Burns care may be improved significantly with a number of simple measures.
THE EMERGING ROLE OF THE SPEECH-LANGUAGE THERAPIST IN IHE MANAGEMENT OF ADULT BURNS PATIENTS: A 3 YEAR RETROSPECTIVE ANALYSIS IN A SPECIALIST BURNS UNIT
G Jones, R Moore, A Magunza
Burns Unit, CH-Baragwanath Hospital, Soweto, Johannesburg
Introduction: Although Burns Units worldwide have a strong multi-disciplinary team tradition, the role of Speech-Language Therapy has not been fully understood or well-utilized. In addition there is very little literature focussing on this area of rehabilitation for a burns patient. According to data published in 2003, 3.2% of South Africa's population will suffer a burn injury of some description. Approximately 10% of these will be admitted to a Burns Unit. With an estimated population of 50 million people, this translates to a significant number of potential interventions by the speech-language therapist.
Methods: This is a retrospective study of patients admitted to the Adult Burns Unit, Chris Hani Baragwanath Academic Hospital (CHBAH ABU) from 1 January 2010 - 31 December 2012. Patient files and Speech-Language Therapy records were accessed to obtain the relevant data.
Results: 595 patients were admitted to the CHBAH ABU during the 3 year analysis period. 51 of these patients were referred to Speech-Language Therapy. Of these patients, 55% presented with dysphagia; 14% with voice disorder; and the remaining 41% with a variety of other speech, language or communication difficulties.
Conclusion: There is a need for increased awareness of the role of the speech-language therapist in the multi-disciplinary team management of burns patients. This in turn will necessitate the development of guidelines and protocols addressing the indications for referral to Speech-Language Therapy.
IS EARLY ENTERAL FEEDING SAFE FOR ADULT PATIENTS WITH SEVERE BURNS? - A 2 YEAR RETROSPECTIVE REVIEW IN A BURNS INTENSIVE CARE UNIT
S Steffen, R Moore, A Magunza
Burns Unit, CH-Baragwanath Hospital, Soweto, Johannesburg
Introduction: Early enteral feeding of severe burns patients is widely advocated, however many authors maintain that feeds should only be commenced after the initial 24 hour resuscitation phase has been completed. Our practice in the Adult Burns Intensive Care Unit, Chris Hani Baragwanath Academic Hospital (CHBAH BICU) is to commence feeds as part of the initial resuscitation phase i.e. on the day that the patient arrives in the unit.
Methods: This is a retrospective study of patients admitted to the CHBAH BICU from 1 May 2011 - 30April 2012. Patient files and Dietetics records were accessed to obtain the relevant data.
Results: All patients tolerated early enteral feeding initially. Those patients that did not tolerate enteral feeds developed intolerance later in their ICU stay, with these being due to ileus as a result of systemic sepsis.
Conclusion: We recommend that all patients with severe burns that are admitted to a BICU should have enteral feeds commenced on the day that they arrive in the Unit. Regular measurement of residual gastric content is essential to monitor absorption of enteral feeds. This is especially important in patients who have developed systemic sepsis.
SAFETY AND EFFICACY OF CONTINUOUS STROKE VOLUME VARIANCE (SVV) AS THE ENDPOINT IN HAEMORRHAGIC SHOCK
J Goosen, G P Candy, G A Richards, K D Boffard
Trauma Unit, CM-Johannesburg Academic Hospital, Johannesburg
Introduction: Time to achieve the endpoint of serum lactate levels <2mmol/l is a predictor of mortality and morbidity in resuscitation from haemorrhagic shock. We determined whether times to reducing the Stroke Volume Variability (SVV) could be used as an alternative endpoint.
Method: Prospective study comparing the safety and efficacy of continuously measured SVV endpoint vs. lactate (LACT) and clinical parameters (CLIN) (Systolic blood pressure (SBp), pulse rate, urine volume/ hour). All patients admitted with haemorrhagic shock (SBp < 90mmHg, BE >- 4mmol/L, serum lactate > 4 mmol/l) were included in the study. Patients with non-survivable injury, or those transferred from another hospital were excluded. Patients were resuscitated with blood component therapy, surgical control of haemorrhage and monitoring with Edwards Vigileo® minimally invasive cardiac output monitoring system as soon as possible after admission. Resuscitation was guided to achieve the earliest of: SVV (<13,) or LACT <2mmo/l, or BE < 4mmol/L from 2 consecutive readings > 2 hours apart.
Results: Actual mortality was 21.7% (10/46) vs. Predicted (MTOS USA) of 43.6%. Mean time to endpoints was: CLIN 12h, SVV 16h, BE 17h, LACT 23h. There were no serious adverse events due to the use of SVV.
Conclusion: Time to SVV <13 provides a real-time, safe and reliable endpoint for resuscitation for haemorrhagic shock.
PROCEDURAL COMPLICATIONS OF CHEST DRAIN INSERTION IN A REGIONAL TRAUMA UNIT IN SOUTH AFRICA
V Y Kong, C Keene, G V Oosthuizen, C Aldous, D L Clarke
Department of General Surgery, Pietermaritzburg Metropolitan Hospitals Complex and the Nelson Mandela School of Medicine, University of Kwazulu Natal, Pietermaritzburg
Introduction: Chest drain (ICD) insertion is a common procedure that is associated with appreciable morbidity. It is often left to the juniors whom knowledge, training and supervision may be limited.
Methods: Over a period of 12 months (January 2011 to January 2012), all patients presented to our trauma unit with clear indication of ICD were included. The indications, drain size, operator training level, insertion location and immediate complications were reviewed.
Results: A total of 540 ICD were inserted. Male: 89%, Female: 11%. Mean age: 27 yrs. Mechanism: 89% penetrating injuries, 21% blunt injuries. 10% of all drains were inserted outside the defined safe triangle. 11% (55/540) were incorrectly placed: Breast tissue (4), subcutaneous tissue (3), Liver (2), Diaphragm (3), drain hole outside thoracic cavity (27), drain kinked (16). 79% were inserted by interns, 21% by registrars. 27% (15/55) of all error occur when placed by registrars, compared with 73% by interns. There was no morality as a direct result of ICD insertion in this series.
Conclusions: Procedural complications remain high, with a significant proportion inserted outside the recommend safe triangle. The majority were inserted by junior doctors, which was associated with significant complications. Urgent effort must be made in improving supervision and training for junior doctors in order reduce the associated adverse outcomes.
A MULTI FACETED QUALITY IMPROVEMENT PROGRAM RESULTS IN IMPROVED OUTCOMES FOR THE SELECTIVE NON-OPERATIVE MANAGEMENT OF PENETRATING ABDOMINAL TRAUMA IN A DEVELOPING WORLD TRAUMA CENTRE
G L Laing, C Jones, J L Bruce, D L Skinner, C Aldous, G V Oosthuizen, D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan Complex and the University of Kwa-Zulu Natal
Introduction: The selective non-operative management (SNOM) of penetrating abdominal trauma (PAT) is well established in our environment. In light of quality improvement initiatives and the introduction of new imaging modalities, we have reviewed our current experience with the management of PAT.
Methodology: A prospectively maintained digital registry was retrospectively interrogated and all patients with PAT treated by our service from January 2012 to March 2013 were included in this study.
Results: A total of 325 patients sustained PAT during the fourteen-month study period. This included 238 SWs, 80 GSWs and 7 impalement injuries. Eleven patients had eviscerated bowel, and twelve had eviscerated omentum. A total of 123 patients (38 %) were selected for a trial of SNOM. This included 103 SWs, 15 GSWs and 5 impalement injuries. Emergency laparotomy was performed on 182 patients (115 SWs, 65 GSWs and 2 impalement injuries) and 21 patients with left sided thoraco-abdominal SWs underwent definitive diagnostic laparoscopy. SNOM was successful in 122 cases (99 %) and unsuccessful in one case (1 %). In the laparotomy group 161 (88 %) patients underwent a therapeutic procedure, in 12 cases (7 %) the laparotomy was non-therapeutic and in 9 cases (5 %) the laparotomy was negative. In the laparoscopy group (24), two patients required conversion for colonic injuries and one for equipment failure. Seven laparoscopies were therapeutic with the identification and intra-corporeal repair of seven left hemi-diaphragm injuries.
Conclusion: We have improved our results with the SNOM of PAT and we have also managed to safely and successfully extend the role of SNOM to abdominal GSWs. We have selectively adopted newer modalities such as laparoscopy to assess stable patients with left thoraco-abdominal SWs and abdominal CT scan for the SNOM of abdominal GSWs.
ANALYSIS OF THE BODY REGION AND SEVERITY OF INJURIES SUSTAINED BY CHILDREN INVOLVED IN PEDESTRIAN VEHICLE ACCIDENTS E. Brits, SM le Grange
Trauma Unit, Pelonomi Hospital and the University of the Free State
Introduction: Injuries to children involved in pedestrian vehicle accidents (PVA) contribute significantly to morbidity, as well as mortality in South Africa.
Aim: To analyse the body regions most likely to be injured, as well as the severity of injuries sustained by different pediatric age groups involved in PVA's. This could assist in the planning of facilities in our province.
Method: After obtaining permission from the Ethics Committee and approval from the various managers, we did a retrospective study on children involved in PVA's between the ages of 1 and 12 years who were managed in the Trauma Unit in Pelonomi Hospital between April 2007 and February 2010. 249 patients were enrolled and divided in four groups: 1 - 3 years, 4 - 6 years, 7 - 9 years and 10 - 12 years, loosely having their height in common. The Chi-square test was used for comparison of variables of multiple groups.
Results: External injuries were by far the most common. The incidence of Head and Neck-injuries were higher in the younger age groups (p=0,0075). The incidence of Lower Limb-injuries were higher in the older age groups (p=0,0067). There was no difference between the groups regarding the severity of injury. A difference was found between the different groups regarding outcome, where the youngest group did worst. (p=0,0412).
Discussion/conclusion: A large proportion of patients involved in PVA's fall in the pediatric population. A certain trend as to what kind of injuries prevail in a certain height/ age group exists and should be considered in the management of these patients. Attention should be paid to the resuscitation skills of the pediatric population in the Trauma Unit.
A RETROSPECTIVE INVESTIGATION OF THE ADMISSION INR LEVELS AND ASSOCIATED OUTCOMES AT THE INKOSI ALBERT LUTHULI CENTRAL HOSPITAL LEVEL 1 TRAUMA UNIT M A Noorbhai, M H Cassimjee
Department of General Surgery, Nelson R Mandela School of Medicine, University of Kwa-Zulu Natal, Durban
Background: Haemorrhagic shock is a leading cause of early traumatic deaths. Acute coagulopathy can occur on admission to trauma units. Acute Coagulopathy of Trauma is said to be associated with worse outcomes.
Aim: The study aims to assess the incidence of the Coagulopathy of Trauma at the IALCH level 1 trauma unit, and further correlate it with outcome.
Methodology: A retrospective analysis of all patients admitted to the Level 1 trauma unit during the period 2007 - 2009 was performed. The variables obtained were: INR, Coagulation profile, lactate, base deficit, clinical parameters and in-hospital mortality. The data was analyzed using the SPSS statistics program.
Results: There were 651 patients of whom 480 were male. The INR levels were obtained in 620 patients; 483 were alive while 137 died. The median INR value among live patients was 1.19 and 1.28 among dead patients. There was an increased mortality amongst patients with abnormal INR levels which was statistically significant (p value 0.12). As the ISS scores increased, the percentage of patients with abnormal INR levels also increases.
Conclusion: Raised admission INR levels are associated with worse outcomes. There is a direct correlation between INR and ISS levels. Early recognition of Acute Coagulopathy will reduce patient morbidity and mortality.
ONE HUNDRED AND FORTY PAN CT'S FOR BLUNT TRAUMA
G V Oosthuizen, H Palmer, J Bruce, G L Laing, W Bekker, D L Clarke
Pietermaritzburg Metropolitan Trauma Service, University of KwaZulu Natal
Background: Pan CT is infinitely helpful in the management of blunt polytrauma patients, but a rising concern about radiation risk is necessitating a rethink as to how pan CT protocols should be applied.
Aim: We aimed to perform an audit of our experience with pan CT's and to see if we could identify a subset of patients that could safely be spared pan CT in future.
Methodology: We performed a retrospective audit of all pan CT's done on blunt polytrauma patients in the Pietermaritzburg public sector in 2012. Indications for pan scan included injury on both sides of the diaphragm, significant mechanism of injury, depressed level of consciousness with unknown mechanism. CT findings were analyzed to ascertain how the use of this investigation impacted patient management and to see if we could have safely omitted some of the scans in hindsight.
Results: We performed 140 pan scans in 2012. Of these, 108 scans were done on males, 32 on females. The average age was 24 (2-62) and the mechanism of injury vehicle-related in the majority of cases (119). Of the 140 pan scans, 5 (4%) were totally negative, while all the rest showed some findings, major or minor. There were 108 scans (77%) that changed our initial management (brain 62 [44%], cervical spine 16 [11%], chest 50 [36%], abdomen 31 [22%]). Of the 32 (23%) scans that did not change our initial management, 26 (19%) were regarded as helpful in terms of ruling out injury in patients that could not be reliably clinically assessed (depressed level of consciousness or distracting injury present). Only 6 (4%) pan scans were done for patients who were fully conscious and with no distracting injury, and could probably safely have been omitted and replaced with a combination of clinical observation and the use of other modalities such as ultrasound and x-rays.
Conclusion: With the mentioned indications, the yield of pan CT can be expected to be high in terms of findings that change initial management. "Negative" scans too are useful in patients who cannot be reliably clinically assessed. Pan CT may be omitted in patients that are fully alert and with no distracting injuries, in favour of clinical observation and other screening modalities.
NEURO-NAVIGATION ASSISTED ENDOSCOPIC TREATMENT OF MULTILOCULATED HYDROCEPHALUS IN PAEDIATRIC PATIENTS
B Enicker1, T E Madiba2, A Landers1, R Harrichandparsad1
1 Department of Neurosurgery, University of KwaZulu-Natal and Inkosi Albert Luthuli Central Hospital, Durban
2 Department of General Surgery, University of KwaZulu-Natal and Inkosi Albert Luthuli Central Hospital, Durban
Background: Multiloculated hydrocephalus is common in our setting. Current treatment is ventriculo-peritoneal (VP) shunt. Combination neuro-endoscopy and neuro-navigation provides an alternative treatment for this condition.
Aim: We tested this treatment by comparing its effectiveness to VP shunt procedure only. The outcome measures were control of hydrocephalus and time to shunt malfunction.
Methodology: Twenty-seven children were prospectively randomized over 15 months into navigated endoscopic treatment and VP shunt (Group A, n=14) and VP shunt only (Group B, n=13). Diagnosis was made using CT/ MR neuro-imaging utilising neuro-navigation sequence for Group A. Rigid neuro-endoscopy was used to connect the loculations within the ventricular system. Patient profiles and responses to treatment were analysed.
Results: Causes of hydrocephalus were meningitis (59%), shunt sepsis (7%) and intraventricular haemorrhage (7%). All children had delayed milestones and 18 had seizures. Mean hospital stay was 17± 9.1 and 9 ± 3.9 days for group A and B respectively. Five and seven children in groups A and B experienced shunt blockage after 5 ± 3.2 and 4.8 ± 3.1 months respectively. Mean follow up was 9 months and mean head circumference was 52.8 ± 3.4 and 53 ± 5.6cms for group A and B respectively. One child died and no children attained normal milestones.
Conclusion: Neuro-navigation-assisted endoscopic treatment of multiloculated hydrocephalus leads to fewer shunt blockages, over a longer period compared to the old treatment method.
USE OF THE GLOBAL ARGININE BIOAVAILABILITY RATIO AS A MEASURE OF DIMINISHED ARGININE AVAILABILITY IN PATIENTS OF AFRICAN ANCESTRY
G P Candy1, M Nel1, C Naidoo1, A D Cromarty2
1 Surgery, University of the Witwatersrand, Johannesburg
2 Pharmacology, University of Pretoria, Pretoria
Background: Traditional risk factors do not fully explain cardiovascular risk in patients of African ancestry. We have previously shown arginine, the precursor of the vasodilator nitric oxide, to be unexpectedly raised in hypertension as arginine supplementation reduces blood pressure. The Global Arginine Bioavailability Ratio (GABR, arginine/ (citrulline+ornithine)) has been reported to be a better measure of arginine availability in relation to cardiovascular risk. To test this we determined GABR in subjects without, and in patients with elevated blood pressures.
Methods: Amino acid profiles were determined in new diagnosed patients with hypertension and in matched control subjects using HPLC/MS. The GABR was determined and subjects dichotomized by the median value. Blood pressure was measured over 24 hours by ambulatory BP monitoring (Spacelabs). Demographic and other measures were compared by an ANOVA using SAS V9.2.
Results:

Conclusion: In contrast to the literature for coronary heart disease, our data suggests an elevated GABR is associated with higher BP, lower ornithine and not elevated citrulline concentrations. This may be a reflection of the different cardiovascular disease group or population group in whom coronary artery disease is unusual.
ARE SURGICAL REGISTRARS ADEQUATELY EXPOSED TO KEY PROCEDURES?
D Kruger, M G Veller
Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand
Introduction: The registrar logbooks submitted to the College of Surgeons (CS) of the CMSA, are used by surgical trainees to log procedural experience in 25 categories. In addition the procedural exposure is specified as unsupervised (US), supervised (S) or assisted surgeon (A). We retrospectively assessed recent surgical trainee exposure to key procedures during their training period.
Methods: 82 recent logbooks submitted to the CS for the past 6 final examinations and considered to be 'satisfactorily' were included in this study. The consolidated logged experience of registrars was analysed according to exposure (US, S or A), operation category, key procedures and University. Logbooks were available from 5 of the 8 South African medical schools.
Results: The number of procedures is expressed as mean (range) and Universities referred to as U1 - U5. 118 409 operations were logged as 60% US, 18.5% S and 21.5% A.
The key findings are indicated in the table below.
Logged data show limited experience in Liver, Neck and Paediatric procedures.
Conclusions: Surgical trainees log a large number of procedures performed during their surgical training. The number of surgical procedures appears to be adequate in some of the procedural categories, but not in others (including varicose veins, burns, oesophagus, rectum and anus, liver and neck). Inter-university procedural exposure varies substantially, particularly in regard to endoscopic, intensive care, oesophagus and stomach & duodenum procedures.
THE ROLE OF BILE AFTER ROUX-EN-Y GASTRIC BYPASS IN PROMOTING WEIGHT LOSS AND IMPROVING GLYCAEMIC CONTROL
D J Pournaras, C Glicksman, R P Vincent, S Kuganolipava, J Alaghband-Zadeh, D Mahon, J H R Becker, M A Ghatei, S R Bloom, J R F Walters, R Welbourn, and C W le Roux
Department of Investigative Medicine, Imperial Weight Centre, Imperial College London, United Kingdom Department of Bariatric Surgery, Musgrove Park Hospital, Tauton, United Kingdom
Department of Clinical Biochemistry, King S College Hospital, London, United Kingdom
Department of Gastroenterology, Imperial College London, United Kingdom
Department of Surgery, University of Pretoria, Pretoria,South Africa
Experimental Pathology, Conway Institute, School of Medicine and Medical Sciences, University College Dublin, Ireland
Introduction: Bile acids signal through the cell-membrane G protein-coupled receptor (TGR5) and stimulate the gut hormones, including peptide YY (PYY) and glucagon-like peptide-1 (GLP-1) which in turn promotes satiety and stimulates β-cells in the pancreas to release insulin. Bile acids increase Fibroblast growth Factor-19 (FGF-19) that regulates glycogen metabolism in an insulin-independent manner.
Hypothesis: The altered bile flow of the Roux-en-Y bypass (RYGB) partly explains the beneficial metabolic outcomes of the operation.
Materials and Methods: The following models were studied: Gastric bypass, Gastric banding, Canine and rodent models
with altered bile flow. Blood tests: FGF 19, plasma bile acids, GLP-1, PYY.
Results: FGF 19 and total plasma bile acids increased after gastric bypass with no change after banding. In the Canine model, GLP-1 and PYY increased significantly when food and bile is combined compared to when only food or bile is given separately.
In the rodent model drainage of endogenous bile into the distal ileum was associated with enhanced PYY responses, reduction in food intake and weight loss.
Conclusion: Altered bile flow after RYGB leads to increased plasma levels of bile acids, FGF 19, incretin and satiety gut hormones, and possibly explains the remission of type 2
diabetes after RYGB.
REFERENCE
1. Endocrinology, August 2012, 153(8);3613-3619
EVALUATION OF THE PAEDIATRIC MAXILLARY NERVE BLOCK
L Prigge1,2, M C Bosman2, A N Van Schoor2,
1 Department of Anatomy, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Garankuwa, South Africa
2 Department of Anatomy, School of Medicine, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa
Background: Regional anaesthetic procedures are being performed more regularly on paediatric patients. This is despite a gap in the knowledge of understanding the exact position, course and/or relationships of the structures used in paediatric nerve blocks. Maxillary nerve blocks are also gaining prevalence in peri-operative analgesia of cleft palate repair in infants. However, the best method for blocking the maxillary nerve in paediatric patients has yet to be established.
Design: Three maxillary nerve block techniques were simulated and compared on 24 dried paediatric skulls as well as 30 dissected paediatric cadavers. The depth and angles, at which the needle travels to block the maxillary nerve, as it exits the skull at the foramen rotundum within the pterygopalatine fossa, was measured and compared. Two age groups were constructed: group 1 consisted of skulls and cadavers from neonates (0-28 days after birth), and group 2 consisted of the skulls and cadavers less than one year of age.
Results & Discussion: No statistical significance difference (p>0.05) was found between the left and right side of each skull or cadaver. Only method B, the suprazygomatic approach from the frontozygomatic angle towards the pterygopalatine fossa, exhibited no statistical significance (p>0.05) when comparing any of the measurements between the skulls and cadavers. Method A, a suprazygomatic approach from the midpoint on the lateral border of the orbit, as well as method C, an infrazygomatic approach with an entry at the site of a vertical line extending along the lateral orbit wall, showed statistical significance when comparing measurements of the skulls and cadavers.
Conclusion: It can therefore be concluded that method B produces the most consistent data for age group 1 and 2, and should be tested in a clinical setting.
OESOPHAGEAL CANCER : REASONS FOR DELAY IN PRESENTATION - A PATIENT PERSPECTIVE M Govender
Department of Surgery, Grey's Hospital, Pietermaritzburg, KwaZulu-Natal
Background: In our setting, most patients with oesophageal cancer have a delayed presentation, with long-standing symptoms and inoperable disease.
Objective: This study was undertaken to establish reasons for this delay in seeking medical attention and identify ways to encourage earlier presentation.
Patients and Methods: It was a prospective study of patients with oesophageal cancer seen at Greys Hospital in Pietermaritzburg between June and November 2012. Data was collected by means of patient interviews.
Results: Forty-six patients were interviewed. All experienced dysphagia but 83 %(38 patients) were prompted to seek help only after weight loss. The duration of symptoms prior to first clinic/hospital attendance was 0 - 12 months (average 3 months).
Reasons for the delay included the following:
• 41 % of patients didn't consider dysphagia a significant symptom
• 24 % had no money
• 19 % sought the help of traditional healers first
• 15 % said the hospital was too far away
Conclusion: Patients with oesophageal cancer defer seeking medical attention for numerous reasons. The most significant are lack of knowledge about oesophageal cancer symptoms and limited access to healthcare. Patient education and improved referral systems are vital in encouraging earlier presentation.
AEROBIC CRUSH SYNDROME. DOES VENOUS BICARBONATE RISK STRATIFICATION CORRELATE WITH THE RIFLE SCORING SYSTEM?
G L Laing, J L Bruce, D L Skinner, J Wang, C Aldous, G V Oosthuizen, D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan Complex, and the University of Kwa-Zulu Natal
Introduction: Professor D.J Muckart previously published on the use of venous bicarbonate levels as a predictor for the development of acute renal failure in aerobic crush syndrome. This study aimed to identify if venous bicarbonate levels < 17mmol/l, provided a robust predictor for the development of acute renal failure according to the more recent RIFLE classification of acute kidney injury.
Methods: This study included both the retrospective and prospective collection of data of 235 patients admitted within the Pietermaritzburg Metropolitan Trauma Service, with suspected aerobic crush syndrome. Patients were classified into non-AKI, Risk and Injury, and Failure groups (according to the RIFLE criteria). The admission venous bicarbonate, base deficit and serum creatinine kinase levels were analysed between these three groups.
Results: In the non-AKI group, the mean venous bicarbonate was 21.5 mmol/L (SD 3.6), base excess was - 4.2 (SD 4.8) and serum creatinine kinase was 2814IU/L (SD 2808). In the Risk and Injury group, the mean venous bicarbonate was 18.8mmol/L (SD 4.9), base excess was - 7.7 (SD 6.4) and serum creatinine kinase was 4433 IU/L (SD 4388). In the Failure group, the mean venous bicarbonate was 16.4mmol/L (SD 5.3), base excess was - 10.8 (SD 7.9) and serum creatinine kinase was 5015IU/L (SD 4997). The p values for venous bicarbonate, base excess and creatinine kinase were <0.0001, <0.0001 and 0.003 respectively.
Conclusion: Admission venous bicarbonate levels of < 17mmol/L remains a robust predictor for the risk of development of acute renal failure according to the RIFLE criteria, in cases of aerobic crush syndrome.
WHAT IS THE ROLE OF AN AXILLARY ULTRASOUND IN DECREASING THE RATE OF NEGATIVE SENTINEL LYMPH NODE BIOPSIES?
I Cassimjee1, C Benn2, G Candy3
1 Helen Joseph Breast Care Clinic
2 Netcare Breast Care Centre of Excellence, Milpark Hospital
3 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
Background: In early breast cancer, a sentinel lymph node biopsy (SLNB) is performed in order to assess a clinically node-negative axilla. Sentinel lymph node biopsies are less invasive than level two axillary dissections, however they still have associated complications. Seventy percent of SLNBs are negative and thus potentially avoidable. Is an axillary ultrasound an appropriate non-invasive means of accurately evaluating an axilla?
Methods: We retrospectively reviewed 151 patients ultrasound reports and correlated them with their SLNB histology findings. In addition, we examined the following patient and tumour characteristics in an effort to identify a pattern of nodal spread which could be used in conjunction with the ultrasound findings in order to decrease the rate of negative SLNBs. These were age, sex, T-stage, location, histological subtype, lymhovascular invasion, oestrogen, progesterone and Her-2 status, and the ultrasonographer.
Results: The ultrasound reports varied in their consistency and quality, and there was no uniform standard of reporting. An ultrasound was able to predict a pathologically negative axilla in 71.6% of patients. Exclusion of micrometastasis increased this result to 82.8%. Ultrasound also ruled out metastasis if the number of involved nodes was less than three. Nodal metastasis could not be predicted based on tumour characteristics (ER/PR/Her2-neu, LVI, Grade, Location) gained from the initial biopsy specimen.
Conclusion: Our results show that an ultrasound cannot currently replace a SLNB as an accurate means of evaluating an axilla. A clear limitation is the inability to detect micrometastasis, however the role of micrometastasis in axillary staging is diminishing and in one study axilla's with less than three nodes involved had similar outcomes to those that are negative. Ultrasonographic evaluation of the axilla is currently reported in a non-standardised manner. Classification systems do exist, and if applied to current reporting will increase the negative predictive value of ultrasonography. The evolving management of micrometastasis and small volume metastasis in the axilla will in the future be combined with improved reporting of axillary ultrasounds in an effort to reduce the rate of negative SLNB's.
BREAST CANCER CHARACTERISTICS AMONG ETHNIC GROUPS IN THE PUBLIC SECTOR OF AREA 2 KWAZULU NATAL
S R Čačala , M Faurie
Grey's Hospital, Department of Surgery, University of KwaZulu-Natal, Pietermaritzburg
Introduction: Breast cancer characteristics in various ethnic groups were evaluated in Area 2 KZN which comprises a largely rural, poorer population, with a lower female life expectancy than the national average.
Methods: Cases of breast cancer were identified retrospectively, for a 5 year period (2002- 2007), from Grey's hospital pathology reports and oncology registration cards.
Results: 872 breast cancers identified in 861 patients; Black 76%, Indian 14.5%, White 7.5% ,Coloured 2%, unknown -2 patients.
Age range : 22-93 years. Mean age Blacks (54.5 years) versus Whites ( 61 years): p=0.0004; and Indian ( 55.7 years) versus Whites: p=0.008.
More Blacks diagnosed < 40 years age compared with Whites (15.6% versus 6.3%).
High grade cancers (52%), commoner in Black women
Oestrogen receptor positive cancers in 63%. Black women more likely to be Oestrogen and Progesterone receptor negative compared with other ethnicities.
Only 76% of patients seen in Oncology; 48% for neoadjuvant treatment for advanced and metastatic cancer. Only 35 % of patients completing neoadjuvant therapy underwent surgery.
Initial surgery in 339 women showed tumour size of 1-20 cms. Blacks had significantly larger cancers (5.6cm) than other ethnicities (mean 3.1- 3.3cm).
Nodes were positive in 69% of patients. Black women were more likely to be node positive (76%).
Conclusion: Distinct differences exist in the prognostic and predictive markers in various ethnic groups. Black women present with larger, more high grade and node positive, ER-breast cancers compared to other ethnicities. This may be implicated in the poorer outcomes in Black women with breast cancer. The younger age at presentation may be a reflection of the life expectancy. Education is paramount to improve breast cancer prognosis in Black women.
FACTORS INFLUENCING DECISION-MAKING FOR NIPPLE AREOLAR COMPLEX RECONSTRUCTION
B Puttergill2, S Rayne1,2, L C J Serrurier1, M Venter1,2, J Slabbert1 and C A Benn1,2
1 Netcare Breast Care Centre of Excellence, Milpark Hospital
2 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
Introduction: Nipple Areolar Complex reconstruction (NACR) is the final surgical procedure undergone as part of onco-reconstructive surgery for breast cancer. The reconstructed nipple operates as a non-functional facsimile of the native NAC and its aim is to restore further aesthetic integrity to the operated female breast. The motivations guiding this reconstruction decision in our patients is poorly understood and this study aims to explore some of these reasons.
Methods: This was a prospective quantitative questionnaire-based study of patients at the Netcare Breast Care Centre. 50 female patients were randomly assigned for recruitment from a cohort of patients who had undergone bilateral mastectomy for a unilateral cancer from 2001-2011.Following an introductory phone call and verbal consent by the participant, a short quantitative questionnaire was completed. The questionnaire was designed with multi-disciplinary input of the specialist breast surgeon, reconstructive plastic surgeon and clinical oncopsychologist. The themes included are: demographics and relationship status; media, surgery, anaesthetic concerns, personal perception and sexuality.
Results: Of the 50 randomly selected patients 11 (22%) were excluded without contact (2 had no breast reconstruction, 1 patient died and 8 were not contactable), and 17 (34%) failed to complete the questionnaire during the study time. 22 questionnaires were analysed. The median age of patients at diagnosis was 50years for NACR and 56 years without NACR (38-67 years). 20% did not have NACR; 75% underwent NACR within 3 procedures in less than 6 months, and 100% within one year.
Cost was important to some degree in 67% undergoing NACR and 50% without NACR. Opinion of a partner was a consideration in only 22% of the patients undergoing NACR; and despite the NAC being important to sexual intimacy before surgery to 90% of all patients, 60% reported a change to their sexual function with a reconstructed nipple and none in the no NACR group. 22% of all noticed a change to their clothing choices furthermore only 25% of patients with NACR and 4% of patients without NACR are comfortable naked. 50% of patients without NACR reported a fear of anaesthesia or surgery affected their choice. No patient would have changed their decision to have or not to have NACR.
Conclusion: The decision to complete reconstructive surgery with NACR or not; is a multi-factorial expression of each individual. It appears unreconstructed patients are influenced by the cost and risk of the procedure whilst reconstructed patients align more closely with their self image and sexual function; the impact if the partner is not significant in either group. NACR does restore confidence and aesthetic pleasure to selected patients undergoing the procedure; but not having NACR can be as satisfactory.
PERCEPTION OF DISEASE AND EMOTIONAL STRESSORS IN MALE BREAST CANCER PATIENTS IN JOHANNESBURG, SOUTH AFRICA
J Thomson1,3, S Rayne12,3, J Reid1 and C A Benn1,2,3
1 Helen Joseph Breast Care Clinic
2 Netcare Breast Care Centre of Excellence, Milpark Hospital
3 Faculty of Health Sciences, University of the Witwatersrand,
Johannesburg
Background: More than 99% of breast cancer occurs in female. It is associated strongly with the feminine persona and fundraising and activism is allied with female colours and themes. Male Breast Cancer (MBC) is a rare disease. There is a paucity of evidence surrounding the personal perceptions and psychological stressors associated with MBC survivors with high levels of cancer-specific distress alterations in body image reported in the USA. There is no experience of how MBC survivors in South Africa experience their disease and psychological sequelae and this study aims to determine this.
Methods: A prospective study was carried out using a short quantitative questionnaire. The primary focus of the questionnaire was MBC patients' perception and experience of their disease. The themes explored included the effect of MBC physically, emotionally and particularly whether having MBC has affected their perception of their masculinity and their personal and sexual relationships.
All male patients presenting to either the Helen Joseph Breast Care Clinic (government hospital) or Netcare Breast Care Centre (private institution) within the study period of May 2007 to May 2012 were identified. Inclusion criteria were a new diagnosis of invasive or in-situ breast cancer and male gender. An exclusion criterion was failure to complete questionnaire. Following verbal consent the questionnaire was administered with the aid of a translator where necessary.
Results: 23 male breast cancer patients were identified. 5 were excluded due to unavailability. 18 questionnaires were completed. Only 6 patients were aware of male breast cancer prior to their diagnosis. The median time of first noticing a breast lump to seeking medical attention was 6 months, with a range of 1 to 36 months.
27% of patients agreed that their perception of their masculinity was negatively affected after being diagnosed with breast cancer. A single patient felt that having breast cancer adversely affected his sexual relationships and only 3 patients felt embarrassed to remove their shirts in public places following their surgery. Neither patient's race or relationship status had a direct correlation to their perception of their masculinity or reluctancy to remove their shirts in public. 94% of patients disclosed their diagnosis with their families and friends.
Conclusion: Despite the rarity of MBC and the poor level of awareness of the disease, patients are freely willing to disclose their diagnosis to friends and family. A quarter of patients diagnosed have a emasculated perception of themselves as a result of breast cancer. Although these patients feel less masculine, their personal and sexual relationships have not been negatively affected or influenced by this.
LAPAROSCOPIC VERSUS OPEN PROCEDURE FOR COMPLICATED APPENDICITIS: A RANDOMIZED CONTROL TRIAL (PROOF OF CONCEPT)
J Thomson, D Kruger, C Jann-Kruger, O Jones, A Kiss, T Luvhengo, M Brand
Department of Surgery, Chris Hani Baragwanath Academic Hospital, R68 Old Potchefstroom Road, Johannesburg
Background: To date no randomized control trials have been performed comparing open appendectomies (OA) to laparoscopic appendectomies (LA) in complicated appendicitis. A Systematic Review and Meta-analysis by Markides (2010) concluded LA is advantages to OA with less surgical site sepsis, however the level of evidence is very poor (level 3a).
Objectives: The primary objective of the study was to determine whether LA is safe in the treatment of complicated appendicitis. Secondary objectives include the intra-operative duration, the rates of wound sepsis, the rates of relook, the length of hospital stay and the rates of re-admissions between the OA and LA groups.
Methods: One hundred and fourteen patients where randomized prospectively to either OA or LA using a computer-generated blind method. Patients who were either less than twelve years of age, had previous abdominal surgery or were pregnant were not considered for randomization. A team of senior surgeons capable of doing both OA and LA performed all procedures.
Results: OA group had a greater risk of developing wound sepsis than the LA group (P < 0.47). Furthermore, in the OA group presenting within 72 hours from the onset of symptoms, the risk of developing wounds sepsis was significantly greater
Conclusion: Laparoscopic appendectomy is safe in complicated appendicitis
ALVARADO FOR AFRICA: ACCURACY OF THE ALVARADO SCORE FOR PREDICTING ACUTE APPENDICITIS IN THE AFRICAN POPULATION
V Y Kong, S van der Linde, C Aldous, J J I Handley, D I Clarke
Department of General Surgery and Anaesthetics1, Pietermaritzburg Metropolitan Hospitals Complex Nelson Mandela School of Medicine, University of Kwazulu Natal, Pietermaritzburg
Introduction: Acute appendicitis continues to pose significant diagnostic challenges. The Alvarado score has been shown to be accurate and is widely used. There is a paucity of literature focusing on the applicability to the South African population. The majority of our patients present with atypical features or advanced pathologies, often causing much confusion, leading to inappropriate management. This prospective study reviews the accuracy of such scoring system in our setting.
Methodology: Over a 3 year period (September 2009 to September 2012), 1000 patients with intra-operatively confirmed acute appendicitis were reviewed. The Alvarado score was assigned with each patient. Scoring was a follows: 1-4 (low likelihood), 5-6(intermediate likelihood), 7-10 (high likelihood).
Results: Male: 54.1%, Female: 45.9%, Mean age: 20.8 yrs. 40.5% had uncomplicated appendicitis, and 59.5% complicated. Alvarado scores: 20.9% had a score of 1-4, 35.7% (5-6), 43.4% (7-10). 69.4% of those with uncomplicated inflamed appendices had a score of 7-10, and 25.7% in complicated cases.
Conclusions: The majority of patients presented with atypical presentation. If such score was to be applied, over one-fifth of patients would have been considered low likelihood and be discharged or delayed to surgery. We recommended exercising extreme caution in applying the Alvarado score to the South African population, and the decision to operate should continue to be based on overall clinical suspicion.
FACTORS ASSOCIATED WITH DELAYS TO EMERGENCY SURGICAL SERVICES FOR ACUTE APPENDICITIS
V Y Kong, S van der Linde, C Aldous, J J I Handley, D I Clarke
Department Of General Surgery and Anaesthetics, Pietermaritzburg Metropolitan Hospitals Complex, Nelson Mandela School of Medicine, University of Kwazulu Natal, Pietermaritzburg
Introduction: Late presentation of acute appendicitis is associated with significant morbidity and mortality in the developing world. Currently, there is a paucity of data in relation to the actual factors involved. This prospective study aimed to address this issue.
Methodology: A prospective database of all acute appendicitis from Sep 2011 to Sep 2012 were reviewed. A delay > 24hrs at any point from the onset of illness to reaching the surgical service is considered significant.
Results: 72% (361/500) had significant delay that contributed to late presentation and associated advanced pathology. Reasons for delay were: Health seeking behaviour (98%, 353/500), Assessment error from hospital doctors (41%, 149/500) and Logistic issues (42%, 151/500), related to ambulance waiting time. 40.7% had 1 factor involved, 35% had 2 and 32% had all 3. Specific risk factor that contributed to assessment error were: referral from rural areas, female gender, and age > 60.
Conclusions: Multiple factors contributed significantly to late presentation of appendicitis. Whilst health seeking behaviour is difficult to change, effort must be made in addressing issues related to assessment and logistic issues in order to improve patients' outcome.
OUTCOME OF URBAN VERSUS RURAL PATIENTS PRESENTING WITH ACUTE APPENDICITIS
V Y Kong, S van der Linde, C Aldous, J J I Handley, D I Clarke
Department Of General Surgery and Anaesthetics1, Pietermaritzburg Metropolitan Hospitals Complex, Nelson Mandela School of Medicine, University of Kwazulu Natal, Pietermaritzburg.
Introduction: Acute appendicitis is common. Patients from rural areas often experience significant delay in presentation and are associated with worse outcome. This prospective study aimed to review the outcome of patients who present from either rural or the urban setting.
Methodology: A prospective database was maintained and all cases of acute appendicitis from Sep 2011 to Sep 2012 were reviewed. Any patients from the Pietermaritzburg district were considered urban. All patients from outside the district (including the peripheral hospitals referrals) were considered rural.
Results: A total of 500 cases were reviewed, 60% (300) were from the urban region and 40% (200) from the rural region. Those from the rural group had a significantly longer duration of illness prior to presentation (6 vs. 3 days, p<0.001). Simple non perforated appendicitis is more common in urban than rural patients (52.3% vs. 21%, p<0.001). Those from the rural group were also associated with higher perforation rate with 4 quadrant sepsis (60.5% vs. 21%, p<0.001) and the need for intensive care admission (23% vs. 2.3%). The length of hospital stay was also longer (8 vs. 4 days). There was no significant difference in overall mortality.
Conclusions: A significant proportion of patients from the rural areas present with a protract course of illness and were associated with significantly higher adverse outcome. Effort must be focused in addressing improvement in access to appropriate surgical services.
THE SPECTRUM OF APPENDICEAL POSITIONS IN THE BLACK SOUTH AFRICAN POPULATION IN KWAZULU NATAL
V Y Kong, G V Oosthuizen, C M Keene, C Aldous, C D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan Trauma Service, University of KwaZulu Natal, Pietermaritzburg
Introduction: Appendiceal position is known to be highly variable and has been well described in the western anatomical literatures. It has direct implication on clinical presentation and operative manoeuvres required for successful surgical management. There is a paucity of literature in this area specifically relating to the Black South African Zulu population in KwaZulu Natal. The aim of this study was to describe the spectrum of anatomical position in this population.
Methods: A prospect study was conducted at Edendale Hospital from September 2010 to September 2012. All patients with acute appendicitis who required operative interventions were included. A single surgeon (VK) performed all of the operations. The position, other associated intra-operative findings were recorded.
Results: A total of 100 cases were included. Mean age: 22.9, Male: 70%, Female: 30%. Positions: Retrocaecal: 69%, Pelvic: 9%, Subcaecal 8%, Preileal: 6%, Postileal: 3%, Unknown: 5% (perforation with associated caecal destruction). 57% of all appendices were perforated (with associated intrabdominal contamination). Laparotomy was required in 64%, with remaining 36% via local incisions.
Conclusions: The majority of cases had retrocaecal position, with a similar distribution amongst the remaining groups. The overwhelmingly high perforation rate caused identification difficulties in a small number of cases. A more liberal use of laparotomy in face of perforation and difficult in accessing a retrocaecal appendix may be required in some cases.
CLINICAL PRESENTATION OF ACUTE APPENDICITIS IN ADULTS AT THE CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL
R Nshuti, D Kruger, T E Luvhengo
Department of Surgery, Chris Hani Baragwanath Academic Hospital, Soweto, Johannesburg
Background: Acute appendicitis is the commonest surgical abdominal emergency. Delayed treatment increases incidence of complications. The aim of this study was to investigate presentation, incidence and predictors of complications, prevalence of HIV infection, and histological findings in adult patients with clinical diagnosis of acute appendicitis.
Methods: The study was prospective observational study. Patients above 11 years old diagnosed with acute appendicitis were included in the study. Collected were demographic data, clinical presentation including HIV status, duration of symptoms and reasons for delay, diagnostic investigations results, operative findings, length of hospital stay and ICU stay, and outcome and histology results.
Results: A total of 146 patients were admitted. The male to female ratio was 1.6:1. Their mean age was 26 years. Predominant presenting symptoms were Right iliac fossa (RIF) pain (95%), nausea (80%) and vomiting (73%); and 63% presented after 2 days. Fever was present in 15% and only 30.9% of patients gave classic history of acute appendicitis. The negative predictive value of WCC and CRP were 28% and 50%, respectively. Sensitivity of ultrasound was 60% with NPV of 31%. Twenty five per cent of patients who were tested were found to be HIV positive. In 30% the disease was complicated. Around 11% of histology results showed normal appendix. The 30-day mortality rate was 1.4%.
Conclusion: Patients with acute appendicitis rarely present with a typical history of vague peri-umbilical pain. Leukocyte count is not reliable in the diagnosis of acute appendicitis. Most of our patients present late with complicated disease and the commonest explanations for delay presentation are lack of access (proper information, health facilities) and prior treatment by general practitioners. Complications were higher in males, the elderly and longer hospital stay in HIV positive patients.
A RETROSPECTIVE AUDIT OF APPENDECTOMIES DONE AT UNIVERSITAS HOSPITAL COMPLEX FROM 2005 TO 2009.
P J Oosthuizen, N E Pearce
Dept Surgery, Faculty of Health Sciences, University of the Free State, Bloemfontein
Background: Appendectomy remains one of the most common emergency surgical procedures performed in the world. With improvements in diagnostic techniques, the efficiency of diagnosis pre-operatively has increased over the years (now approaching a negative rate of <10%), although a 10-25% rate is still considered acceptable1. However, the entity of negative appendectomies still poses a dilemma because they are associated with unnecessary morbidity, mortality and cost. This study was conducted to show recent trends in negative appendectomy rates at our institution taking into account age, gender and ethnicity.
Methods: A retrospective analysis was conducted using data from the Universitas Hospital Complex (Universitas and Pelonomi Hospitals, Bloemfontein) from 2005 to 2009. All patients who had undergone surgery for clinically suspected acute appendicitis at the Pelonomi and Universitas Hospitals from 2005 to 2009 were included. Patients with incidental appendectomy were excluded, while those with other appendiceal pathologies, like Carcinoid and Tuberculosis, who had presented as acute appendicitis, were also included. The patients were then stratified according to age, gender and ethnicity.
Results: Between 2005 and 2009, there were 708 cases of appendectomy. Seven hundred and four (n=704) of them were included in our study. Of these, 163 were negative appendectomies (23.3%). The age range of the 704 cases was 4 to 84 years, with a median age of 20 (25th percentile 14 years and 75th percentile 29 years). The male:female ratio was 1.4:1. The percentage of misdiagnosis was greater amongst women than men (32% vs. 16.7%; p<0.0001). The number of patients with negative appendices was higher in the childbearing age group (between 13 and 50) than in children (27.0% vs. 7.3%). The average rate of perforation was 32.8% (231 of all patients). Ethnic distribution in our setting was 69.3% Black patients, 11.2% Caucasian, 19.1% coloured and 0.4% other ethnic groups. When comparing misdiagnosis among patients by ethnicity, a statistically significant difference were found in the incidence between Black and Caucasian groups (18.4% vs. 39.2%; p<0.0001). Other appendicular histology was found in 0.9% of cases, with an incidence of 0.14% of Carcinoid of the appendix in our study population.
Conclusion: Despite efforts to reduce negative appendectomies they still occur. It does appear however, that careful clinical assessment of these patients still remains one of the main modes of reducing the incidence of negative appendectomies. Specialized diagnostic tools might be more important in females of child bearing age.
COMPARISON OF CONVENTIONAL INSULIN SLIDING SCALE VERSUS MODIFIED SLIDING SCALE IN SURGICAL DIABETIC PATIENTS AT DR GEORGE MUKHARI HOSPITAL
F O Ghoor, S Ndlovu
Department of Surgery, University of Limpopo, Medunsa Campus
Introduction: Diabetic patients have a high morbidity when the diabetes is poorly controlled.(1) The mainstay of glucose control in surgical wards has been the "insulin sliding" scale. However, numerous studies have shown it to be ineffective, but it is still extensively used due to its simplicity.(2,3) The effectiveness of the modified physiologic sliding scale has been proven in various studies, but numerous variables in calculating the exact dosages are required which has dampened its adoption.(4) Aim and Objective. To compare the effectiveness of glucose control with the conventional sliding scale, to a simplified version of the modified physiologic insulin sliding scale (BNC: Basal/Nutritional/ Correctional sliding scale) in surgical patients at Dr George Mukhari Hospital.
Methods: Review of prospectively collected data over a 6 week period from 01 April 2013 to 15 May 2013. Diabetic surgical patients in Wards 4 and 8 (conventional) were compared with Wards 3 and 7 (modified) who were diagnosed with diabetes. Quality of glucose control, sepsis (absent /mild/ severe), age, gender and DM type were recorded. All diabetic surgical patients in Wards 3 and 7 were included on the BNC sliding scale except those on diet control or on a single oral agent. The BNC is calculated according to the formula: Basal dose = ½ (Weight (kg) x 0,4) units Actraphane given at 06:00. The nutritional dose is designed to provide insulin during meals, 4 units Actrapid sc 30 minutes before meals. NPO patients get no insulin. The haemoglucotest is done before meals and at night and a correctional dose of Actrapid administered according to the conventional sliding scale.
Results: Logged data show limited experience in Liver, Neck and Paediatric procedures.

Conclusions: Surgical trainees log a large number of procedures performed during their surgical training. The number of surgical procedures appears to be adequate in some of the procedural categories, but not in others (including varicose veins, burns, oesophagus, rectum and anus, liver and neck). Inter-university procedural exposure varies substantially, particularly in regard to endoscopic, intensive care, oesophagus and stomach & duodenum procedures.
SARS (UK) Patey Prize Winning Presentation
MICROEMBOLI ARE VISIBLE IN THE RIGHT HEART DURING ENDOTHERMAL ABLATION OF VARICOSE VEINS
H M Moore1, V Sounderajah1, A Thapar1, T Ra Lane1, K Fox2, I J Franklin1, A H Davies1
1 Academic Section of Vascular Surgery, Department of Surgery & Cancer, Imperial College School of Medicine
2 Imperial College Healthcare NHS Trust, Charing Cross Hospital
Background: Cerebrovascular events have been reported after foam sclerotherapy. The cause is unknown, but one hypothesis is migration of microbubbles to the brain. The aim of this study was to identify whether microemboli are found in the right side of the heart during radiofrequency ablation of varicose veins, as neurological events are not reported during these procedures.
Methods: Transthoracic echocardiography was performed during local anaesthetic radiofrequency ablation of the great saphenous vein in 14 patients. Views were captured at the start of the procedure, during each heating cycle and one minute post-treatment, and read by an independent cardiologist. The presence of microemboli was classified as: 0=absent, 1=occasional microemboli, 2=stream of microemboli, 3=complete opacification.
Results: Loops were diagnostic quality in 79% patients. Microemboli were seen in the right heart in 5/11 (45%) patients, classified as grade 1 in 4 patients and grade 2 in 1 patient. No microemboli were seen in the left heart. No neurological symptoms were reported.
Conclusion: Microemboli in the right heart are a common finding during radiofrequency ablation. More neurological events might be expected if these particles were responsible for these events. Further work is required to elicit the mechanisms underlying neurological complications following sclerotherapy.
IMPROVING THE MORBIDITY AND MORTALITY PROCESS AT A RURAL REGIONAL HOSPITAL IN SOUTH AFRICA
B Shazi, D Clarke, M Naidoo, C Aldous
Ngwelezana Hospital, Northern KwaZulu Natal
Background: Ngwelezana Hospital is a Regional hospital located in Northern KwaZulu Natal. One of the methods we use to assess our standards of surgical care is through weekly Morbidity & Mortality meetings. Exhaustive discussions around all patient incidents contribute to quality control. However, gathering the data for M&M meetings has been unreliable and there has been a discrepancy between the cases reported at the M&M meetings with mortuary and other data.
Aim: We aimed to identify the gaps in the system where cases or morbidity and mortality escaped the weekly discussion.
Methodology: This was a retrospective, descriptive study. We compared the numbers of cases presented at the M&M meetings from January to March 2013 to the number of deaths noted in the mortuary book, admission and mortality registers of the surgical wards, ICU and EMU(emergency medicine unit).
Results: Out of 122 surgical deaths in the first 3 months of 2013, 71 (58.2%) were not presented at the M and M meetings. Twenty-three deaths (23.4%) and 3 (0.42%) of the 71 that were not presented, were from EMU and ICU, respectively. Fifty-five of these deaths (75%) occurred in the surgical wards.
Conclusion: We need to have morbidity and mortality meetings for quality control and to improvement our surgical service. This is an age old traditional way things are done all over the world in the discipline of surgery. To be effective, every single M&M case should be discussed in the M&M meeting. None should be omitted at all. However, with the poor resources we have for record keeping in our setting, more than half the mortalities escape the discussion at the forum. Thus we are not really doing very good quality control and not learning as much as we should. We must develop a system that allows no case is omitted. We should:
1. Have a person responsible for ensuring that all morbidities and mortalities are reported including those that occur in ICU and EMU.
2. Have M&M registers in all surgical wards and theatre
3. Involve the nursing staff in data collection.
THE QUALITY OF OPERATIVE NOTES IN A BUSY REGIONAL METROPOLITAN SURGICAL SERVICE: DO COMPUTERS IMPROVE QUALITY?
P H Grabe, G L Laing, V Y Kong, C M Keene, C Aldous, D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan Hospitals, University of KWAZulu-Natal, Pietermaritzburg
Introduction: The quality of operative notes varies significantly between different hospitals. There is currently no standardisation for quality assessment nationally or between and within hospital groups. The Pietermaritzburg metropolitan Complex consists of two hospitals with different systems for making operative notes. Greys - the tertiary hospital has adopted from Addington Hospital a computer based system, whereas Edendale - the regional hospital uses traditional free text notes.
We aimed to measure the difference between these two methods in regard of completeness and quality of the notes.
Methods: We retrospectively reviewed 100 operative notes for emergency laparotomy from each hospital between over a three month period against the standard WHO criteria.
Results: Total completion rate for computerised notes (CN) was 76.3% and 60.2% for handwritten notes (HN). Completion rate for each items (CN vs. HN): Patient demographics: 100% vs. 99%, Surgeon's Name: 76.6% vs. 68%, Consultants: 44% vs. 31%. Operative indications: 98% vs. 82%. Operative Diagnosis: 100% vs. 31%. Procedure: 100% vs. 95% Incision (61% vs. 74%), Findings: 87% vs. 43%. Post-operative plan: 58.3 vs. 40.6%. Legibility score analysis of all notes in the HN group scored 2/5 (scale of 1-5).
Conclusion: There is significant deficiency in the quality of the hand written operative notes . The computerised cohort was of better quality because of the template format. Further development of the computer bases system may result in further quality improvements.
TOO WELL FOR ICU, TOO SICK FOR THE WARD - DEVELOPING AN ACUTE PHYSIOLOGICAL SUPPORT SERVICE FOR SURGICAL PATIENTS AS PART OF A MULTIFACETED QUALITY IMPROVEMENT STRATEGY AT A BUSY REGIONAL HOSPITAL IN SOUTH AFRICA
V Y Kong, L C Naidoo, C M Keene, C Aldous, E D L Clark
Department of Surgery, Pietermaritzburg Metropolitan Hospitals, University of kwaZulu-Natal, Peitermaritzburg
Introduction: Previous audits have revealed deficits in the process of care of acute surgical patients at our institution. In response, the Acute Physiological Support Team (APST) was created directed at improving the care for those not meeting the criteria for ICU admission, but were felt to be of significant risk to warrant more intensive support than the general surgical ward care.
Methods: During the period November 2012 to January 2013, all cases referred to the APST were eligible, all were followed up until discharge from the team (or death).
Results: A total of 101 patients were admitted. Mean age: 40, Female: 36, Male: 65. 65 non-trauma, 35 trauma cases. Mean length of stay: 4 days. 11 were haemodynamically unstable on presentation and 12 were clinically septic. Reasons for referral: Sepsis (4), respiratory distress (3), AKI (38), post-operative monitoring (26), pancreatitis (3), ICU down-referral (7), hypoxia (5), low GCS (1), coagulopathy (1). Mortality rate was 13%. Interventions initiated: IV fluids (101), antibiotics (9), management of neutropaenic sepsis (1), central line insertion (3), optimisation of oxygen therapy (7), correction of electrolyte abnormality (8), correction of coagulopathy (2). A total of 36 cases experienced one or more errors: Drug related (4), fluid related (16), indwelling device related (5), surgical decision related (2) and failure to review special investigations (2).
Conclusion: The introduction of APST had a significant positive impact on patient care improvement in these high risk surgical patients. There is a high intervention rate as well as error detection rate, and is effective in improving the care for these high risk patients not deemed suitable for ICU.
THE ECONOMIC IMPACT OF ELECTRONIC GATE-KEEPING AT DR GEORGE MUKHARI: DOES IT REALLY LOWER LABORATORY INVESTIGATION COST?
T Sumbana, M Z Koto
Department of Surgery, Faculty of Health Sciences, School of Medicine, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Background: The electronic gate keeping is software introduced to block repetition and unauthorised ordering of blood investigations the aim is to reduce unnecessary cost. The NHLS can automatically reject blood investigations if repeated within a specific time period with exception made for high care and ICU. The decision can be over-ruled by a senior clinician if he/she is of the opinion that the test is necessary. The software was first introduced in the Western Cape Province were the cost savings were way above 5%. This has been adopted by the Gauteng province targeting overall 5% cost saving. It was implemented at Dr George Mukhari hospital as part of the provincial policy.
Objectives: The main aim is to look at the cost effectiveness of electronic gate keeping software and also its clinical implication whether it can be done without compromising patient care.
Methods: The year on year analysis of the cost(monthly bill) and the quantity(number of tests requested) before the electronic gate keeping was introduced of year 2011-2012 were compared with those after the introduction of electronic gate keeping year 2012-2013 on a monthly basis. End points being reduction in the number of blood tests requested with associated cost reduction, the target being 30% and any adverse effect on patient care (a death/delayed treatment because blood test couldn't be repeated or done) to be reported to a senior clinician/clinical manager.
Outcome: Our experience at DGMH is a cost reduction of 23% per month 7% short of our target. But this is much higher than the 0, 9% at the provincial level which is way below the 5% target. In terms of adverse events on patient care we have a case of hyperkalaemia where patient results couldn't be processed ending with a mortality. On another occasion half the slate was cancelled because the gate keeping couldn't be reversed on time.
Conclusion: Electronic gate keeping is a safe strategy to reduce cost, but its impact in patient care, if not managed well can be devastating.
EMERGENCY SURGICAL ADMISSIONS IN A REGIONAL HOSPITAL IN NORTHERN COASTAL KWAZULU-NATAL (REGION 4)
I Dash1, S Bola1, D Clarke2, C Aldous3, M Naidoo1
1 General Surgery Department, Ngwelezana Hospital
2 General Surgery Department, Metropolitan Trauma Service Pietermaritzburg
3 School of Clinical Medicine, University of KwaZulu-Natal
Introduction: Our hospital is currently responsible for a regional General Surgery service provision for the region 4 of Northern Kwazulu-Natal, The hospital is under-resourced with overcrowding of wards and overspill onto medical wards, resulting in poor quality of care. We set out to assess the true emergency workload of our general surgery department.
Methods: We analysed daily emergency surgery intake reports to collate information regarding the admissions between 1st January 2013 and 31st March 2013.
Results: Over three months we admitted a total of 911 patients. Trauma accounted for 37% of these patients, sepsis (diabetic foot sepsis, abscesses etc) accounted for 20% of these admissions. Admissions with an acute abdomen accounted for 140 patients (15%). Of the trauma patients, interpersonal violence accounts for 38%, snakebites account for 19%, burns for 16% and road traffic accidents account for only 11%.
Conclusion: Currently, our high intake of emergency general surgical admissions is placing significant stresses on our department, with a high turnover of patients and wards overflowing resulting in patients being placed on stretchers or in wards where nurses are not accustomed to looking after surgical patients. Combine this with a third of our admissions resulting from trauma, where the patients often have complex multi-factorial injuries, there is a concern that this could potentially cause a significant impact on the hospital's already stretched resources. As many of our patients are of employment age, this also may cause a wider social problem due to indirect costs due to loss of earnings and workforce.
GENERAL SURGICAL OPERATING THEATRE: DO WE MAKE THE BEST USE OF TIME?
I D Smith
Dept of Surgery, Ngwelezane Hospital, KZN
Background: Operating theatre time is an expensive resource in any surgical unit and it needs to be used as efficiently as possible. We conducted an audit to examine exactly how our theatre time was used over a two-month period. In particular, what proportion of the day was spent operating and how that time might be maximised in the future was the key purpose of the study.
Aim: We aimed to quantify the allocation of time to various activities within the theatre space.
Methodology: Theatre activity was recorded over nine daytime theatre slates in our main general surgery OT in the months of September and October 2012 at Ngwelezane Hospital. There were several surgeons involved with elective (23) and emergency (5) cases. Timing of theatre activities began when either the surgeon or anaesthetist arrived and ended when the last patient left the OT if their surgery had commenced between 3 and 5pm - a typical day. The times when the patient arrived in OT, when anaesthesia was induced, when surgery commenced and ended and finally when the patient left OT were recorded for each patient.
The data was recorded and analysed in a Microsoft Excel spreadsheet. Each time period was allocated to either the anaesthetist or surgeon or neither if the theatre was empty. The time between induction of anaesthesia and the operation commencing was split equally between surgeon and anaesthetist because it might involve either an anaesthetic adjunct (eg. caudal block) or surgical positioning and draping.
Results: An average of 3.2 cases were operated on each day. The average day lasted 8 hours with the first operation commencing at 8:59AM. 53% of that day surgery was being performed, 27% anaesthetic induction and recovery and the theatre was empty on average 20% of the time. Two-thirds of the cases were major elective surgery with an average operating time of 70 minutes.
Conclusions: The time split between surgery and anaesthesia is debatable in a public sector Teaching hospital but 20% of the time we found our theatre lay empty. In our unit a larger pre-op holding area and a more coordinated, earlier start should help reduce this inefficiency. Previously most of the day's elective patients were brought down at the start of the day to a large room adjacent to theatre - this shortened transfer times and allowed our anaesthetic colleagues to review patients while OT continued to function. Patients now tend to be collected in a serial fashion from the wards.
OESOPHAGEAL CANCER IN PIETERMARITZBURG: THE SHOCKING TIMELINE TO DIAGNOSIS AND DEFINITIVE MANAGEMENT
M Govender
Department of Surgery, Grey's Hospital, Pietermaritzburg, KwaZulu-Natal
Background: Despite advances in its management, oesophageal cancer remains a disease with dismal outcomes. Most patients present with advanced lesions amenable only to palliation.
Objective: This study was undertaken to quantify the oesophageal cancer timeline, from first symptom to definitive management, and to identify undue delays and points of potential impact.
Patients and Methods: This was an audit of patients seen with oesophageal cancer at Greys Hospital in Pietermaritzburg from January to November 2012. Patients were identified from records at Oncology and Surgical clinics and the GI unit. A retrospective analysis of charts was performed and a timeline plotted. It included duration of symptoms prior to first presentation, time to diagnosis and to definitive management.
Results: 113 patient charts were reviewed. The time to first visit ranged from immediate presentation to a 12 month delay with the average symptom duration being five months. Establishing a diagnosis took an average of one month from first presentation but varied from zero to eight months. Once diagnosed, definitive management was instituted on-average one month later (range zero to seven months). The overall timeline from first symptom to definitive management was 2-14 months with a mean of seven months.
Conclusion: There are unacceptably long delays in the presentation, diagnosis and management of oesophageal cancer in our environment. The problem is multi-faceted. Patient education and improved referral systems may result in earlier presentation. The use of protocols and a multi-disciplinary team may facilitate rapid diagnosis and management. Only by significantly reducing delays can we hope to impact on outcomes.
LAPARASCOPIC GRAHAM PATCH FOR PERFORATED PEPTIC ULCER AT DR GEORGE ACADEMIC MUKHARI HOSPITAL
M N Latakgomo, M D Ntsoane, M Z Koto
Department of General Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Introduction: Perforated peptic ulcer is a relatively common acute abdominal condition. It remains a challenge for a treating surgeon especially in patients with high Boey score and those with giant ulcers. Minimally invasive surgery has become integral part of management of perforated peptic ulcer.
Aim: To update on our initial experience with laparascopic Graham patch for perforated peptic ulcer.
Methods: Prospective data from patients who presented with acute abdomen as a result of perforated peptic ulcer was collected between November 2011 to April 2013. Those who had open surgery were excluded from the study. We looked at patient's demographics, clinical condition, operative procedure, and outcome. All patients had full resuscitation on admission and were operated under general anesthesia. A three port technique was used for most cases and additional port was inserted when necessary. The peritoneal lavage was done with superabundant amount of warm saline and the ulcer closed with Graham patch.
Results: During this period 35 patients were seen, (31 males and 4 females) their mean age 44years (19-71). Average Boey score 2. The average operative time was 100 min, the mean hospital stay was 4days. One patient spent 2days in ICU because she had associated comorbidity preoperatively and one patient had superficial wound sepsis.
Conclusion: Laparascopic Graham patch is safe and feasible in our setting, and it is even better in patients with high Boey score.
TRENDS IN DEMOGRAPHICS AND MANAGEMENT OF OBSTRUCTING COLORECTAL CANCERS IN KWAZULU-NATAL
Z Moolla, T E Madiba
Department of Surgery, Nelson R. Mandela School of Medicine,University of KwaZulu- Natal, Durban
Introduction: Patients who develop obstruction early in the course of colorectal cancer seem to have more aggressive tumors, higher operative complications and a poorer prognosis. There is a paucity of local studies investigating obstructing colorectal cancers. The aim of this study is to describe our experience at a tertiary hospital and compare it with international standards.
Patients and Methods: Data of patients referred to Inkosi Albert Luthuli Hospital with colorectal cancer between 2000 and 2012 was prospectively collected. Demographic information and management of patients with obstructing tumors were analyzed.
Results: Colorectal cancer was diagnosed in 1478 patients. Malignant obstruction occurred in 206 patients (13.9%) and was more common in males (118). The mean age at presentation was 59 years with African patients presenting significantly younger. The most common sites of obstruction were the sigmoid and rectum. Twelve patients presented with associated perforation, 5 with fistulation and 2 with intussusception. Fifty eight patients (28%) presented with concomitant metastatic disease. One hundred and twenty eight patients (62%) were managed by resection, 40 (20%) were managed by stenting, 35 (17%) by defunctioning colostomy, 3 (1%) by colonic bypass. Stenting was unsuccessful in 5 patients and used as a bridge to surgery in 6 patients.
Conclusion: The high percentage of patients presenting with obstruction as well as the younger age in African patients highlights the need to diagnose colorectal cancer before obstruction. Stenting remains a reliable management option.
INTERPERSONAL VIOLENCE: THE BURDEN OF KWAZULU-NATAL, SOUTH AFRICA
S Bola, I Dash, M Naidoo, D Clarke, C Aldous
Ngwelezane Hospital, KwaZulu-Natal
Introduction: Interpersonal violence is an under-reported and expensive burden on our health and social resources. It costs a substantial proportion of the gross domestic product in developed countries and the economic effects are likely to be more significant in lower socio-economic countries. The workload and stress on hospital resources is known but difficult to quantify. We set out to identify the impact that interpersonal violence, a largely preventable admission, has on the General Surgical department in Northern Coastal Kwazulu-Natal.
Methods: Emergency admission reports were reviewed between the period 1st January 2013 and 31st March 2013. All admission data was recorded in a database and interpersonal violence admissions were identified. Case files were examined for further information such as details of inpatient stay, need for surgical intervention and the use of hospital resources. We utilised cost analysis research from neighbouring hospitals to estimate hospital expenditure.
Results: There were 911 acute surgical admissions. Trauma made up 37% of patients intake of which 45% was secondary to interpersonal violence. The average inpatient stay was 10 days and the majority of these patients needed high care beds on admission. One third required an emergency operation and of these, 12 patients went to ICU for post-op care. There was high level of CT scan and blood product usage in these patients.
Conclusion: The prevalence of interpersonal violence in this population is obvious. Patients are often severely injured and require a high level of surgical care, costing the hospital considerable usage of precious resources. This further impacts on other emergency patients, for what is ultimately a preventable admission causing delays in surgery, diagnosis and treatment. Community intervention and education is crucial in reducing this burden in Kwazulu-Natal.
A FAVOURABLE OUTCOME OF COMPOUND SKULL FRACTURES CAUSED BY ASSAULT WITH A MACHETE
B Enicker1, T E Madiba2
Department of Neurosurgery and General Surgery, University of KwaZulu-Natal Inkosi Albert Luthuli Central Hospital ,Durban
Background: Machetes are agricultural slashers used across South Africa which are also used in interpersonal violence.
Aim: To profile cranial injuries caused by machetes over a 10-year period.
Methodology: Retrospective analysis of patients with compound skull fractures following assault with a machete , admitted for emergency neurosurgical intervention, from 2003 to 2012 was performed. Medical records were analysed for demographics, clinical presentation, neuroimaging findings, neurosurgical treatment and outcomes.
Results: A total of 135 patients were treated of whom 123 were male (M:F = 10:1). Mean age was 31 ± 12.1 years. Mean GCS on admission was 13 ± 2.4. 25 patients presented with oozing brain matter and 63 presented with focal neurological deficits whilst 14 patients presented with post traumatic seizures. Forty patients had machete injuries in other parts of the body. There were 116 depressed skull fractures (86 %). Associated intracranial findings on neuroimaging were intracerebral (92), extradural (19) and subdural (9) haematomas. Pneumocephalus was present in 53 cases and 51 cases had cerebral swelling . Nineteen cases presented with septic wounds. One hundred and five (85%) cases were treated surgically and all patient received antibiotics. Average hospital stay was 13 ± 18.5 days and mean GCS at discharge was 14 ± 3.1 . All patients who presented with focal neurological deficits had residual deficits on discharge and 10 (7.4%) died.
Conclusion: Machetes cause devastating cranial wounds. A favourable outcome is possible with timeous intervention and good surgical principles.
THINGS CAN ONLY GET BETTER... COMPARATIVE LEVELS OF INTERPERSONAL VIOLENCE INJURIES AND THEIR MANAGEMENT OVER FIVE YEARS IN JOHANNESBURG, SOUTH AFRICA
S L Rayne2, D L Gersun2, C Sofianos2, M S Moeng1,2, J Goosen1,2, K D Boffard1,2
1 Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit
2 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
Introduction: Johannesburg is still characterized as a city with a large burden of intentional injury and violence. This study compares the changing patterns of injury resulting from interpersonal violence (IPV) between 2007 and 2012.
Method: All patients attending the Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit with evidence of IPV injury over the same period five years apart (2007 and 2012) were studied prospectively. The patterns of mechanism, injury and management were compared.
Results: Overall, there were a similar amount of patients seen during the two study periods of 2007 and 2012 (n=1304 and 1334 respectively) but a marked decrease in the rate of IPV cases. Changes in the patterns of weapon use and management of patients are summarised in the Table.

Conclusion: There has been a change in the pattern of IPV in Johannesburg over the last five years with less firearms violence and more blunt common assault evident. There has also been a change in the practice of trauma care, with less operative management, significantly more investigations and a more conservative approach to trauma management.
INTIMATE PARTNER VIOLENCE AT A TERTIARY INSTITUTION
K Spencer, G P Candy and M Haffejee
Department of Urology and 1General Surgery, University of the Witwatersrand, Johannesburg
Introduction: The World Report on Violence and Health 2002 defined interpersonal violence (IPV) as violence between individuals, subdivided into family and intimate partner violence and community violence. This study was to ascertain the prevalence of intimate partner violence within a South African tertiary institution population with a diverse demographic profile.
Methods: Ethical clearance from the University Research Ethics Committee and permission was obtained from Dean of Students (Health Sciences Faculty) as well as from Head of Social Sciences. Undergraduate medical students from the Medical School and Social Sciences were asked to complete an anonymous questionnaire which was derived from similar international studies. Students were made aware of psychological counselling services that were available to them, if they experienced discomfort from the survey process. Data obtained included demographic and data on sexuality, the extent of intimate partner violence, whether participants were victims or even perpetrators of IPV. Data was recorded in an EXCEL spreadsheet and analysed using Statistica & SAS V9.1 using a Chi-squared test with correction as appropriate.
Results: Responses were obtained from 1351 of 1593 students (68% female; 45.9% African; 32.7% Caucasian; 14.7% Eastern ancestry). Most questions had more than 1300 responses (minimum 1202) and appeared to have been answered consistently. Respondents indicated that 94% were only heterosexual, 47% were in a relationship with 57% indicating that they were sexually active. 77% were HIV negative, with 21% indicating they did not know their status. 35% of respondents admitted to have been emotionally abused, 19% physically abused, and 9% sexually abused (2.5% of males and 12.6% of females) with 16.8% of African female students indicating they had been sexually abused. Of the total victims of sexual abuse victims, 45% were able to negotiate at least protected sex. 13% of respondents admitted they had physically hurt someone close to them, without gender difference (p=0.55), with differences between ethnic groupings. Only 3 perpetrators of sexual abuse had been sexually abused. Only 59% of respondents knew where to get help.
Conclusions: The extent of emotional, physical and sexual abuse amongst University medical and social science students is unacceptably high. The survey should be undertaken at other centres of higher learning to determine possible region differences.
IMPACT OF INSTABILITY ON OUTCOMES IN PENETRATING NECK TRAUMA
M S Moeng, E Chikwendu, S R Motilall, S Gyebi, R Jacks, D Mogabe, J Goosen
Trauma Unit, CM-Johannesburg Academic Hospital and the University of the Witwatersrand, Johannesburg
Introduction: Penetrating neck trauma may be associated with significant bleeding and haemodynamic instability(HD). Due to close proximity of vascular and aero-digestive tract, potential multiple injuries are likely. Failure to promptly control bleeding or establish a definitive airway may result in loss of life.
Aim: Evaluate the impact of HD instability on outcomes in patients presenting with penetrating neck trauma at a single Trauma centre Method All patients who sustained penetrating neck trauma at the CMJAH from 01/04/2005 to 28/04/ 2008 were recruited for the study. Haemodynamic instability was defined as BP less than or equal to 90 in the emergency department. Demographic data, mechanism of injury, physiological parameters, ISS, anatomical organ injury, CT scan findings, procedures done and outcomes were recorded. Data was recorded on an excel spreadsheet. Statistica V8 was used as a tool for statistical analysis. P value <0.05 was considered statistically significant.
Results: Of the 466 patients recruited, 35 were excluded due to insufficient data. Twenty nine of the 431 had haemodynamic instability (6.7%). The HD unstable group had a higher median ISS (17 v/s 5), higher ISS>25 (38% v/s 6.7%), higher incidence of major vascular injury (44.8% v/s 15%) and higher mortality (24.1% v/s 3.23%). All deaths in HD unstable patients were in Emergency department or on table in theatre. Clinical improvement with resuscitation allowed for CT scan investigation in only 34% of HD unstable patients compared to 50.7% of the HD stable. Surgery was only required in 48.2% in those initially presenting with HD instability v/s 22.9% of the HD stable group.
Conclusion: Haemodynamic instability in penetrating neck trauma is associated with more severe trauma and carries a high mortality. Only a third of the HD unstable group improved enough to allow for a CT investigation.
Poster Presenations
COST EFFECTIVE LAPAROSCOPIC APPENDICEC-TOMY: SEBOKENG HOSPITAL
I Bombil, T A T Mosia, S W Lunda, R Isakov
Department of Surgery, Sebokeng Hospital and the University of Witwatersrand, Johannesburg, South Africa
Introduction: Appendectomy is the most commonly performed emergency procedure in general surgery. Therefore it is likely to impact the most on the budget. Cost effectiveness is vital to reduce expenses. In our situation, laparoscopy is perceived to be expensive due to the consumables. Hence the aim of our study is to evaluate the cost of consumables in performing laparoscopic appendectomy in a level II regional hospital with limited resources.
The main objective is to prove that consumables used in laparoscopic appendectomy as performed in Sebokeng Hospital is cheaper than in ideal circumstance( private or the first world hospital).
Ethic approval has been obtained from the Wits Human research ethic committee (M121110)
Methods: Retrospective review of prospectively collected data from November 2011 to October 2012. A total of 167 laparoscopic appendectomy were performed.
Parameters analysed were:
Cost of consumables in ideal circumstances vs. the cost in our Hospital:
1. Endo-stapler vs. Diathermy
2. Endo-pouch vs. Vacoliter
3. Endo-loop vs. Homemade Endo-loop.
4. Trocar, grasper, scissors, hook, dissectors: Disposable vs. Re-usable
5. Gas (Co2): Carbon dioxide.
Results: Table. Price comparison: Sebokeng Hospital vs. Ideal circumstance.
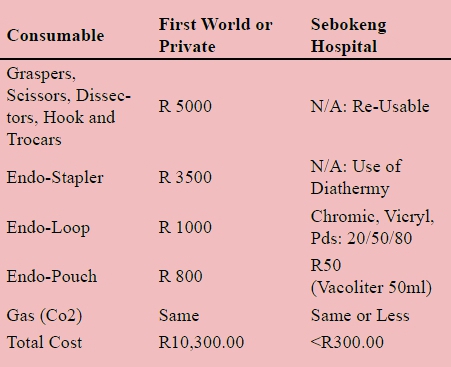
Conclusion: Laparoscopic appendectomy as performed in Sebokeng Hospital is by far (34 times) cheaper than in private or first world countries in term of consumables.
SURGICAL MANAGEMENT OF RECURRENT PERIDUCTAL MASTITIS AT GROOTE SCHUUR HOSPITAL
M Mutebi, L Cairncross, E Panieri
Endocrine and Surgical Oncology Department, Groote Schuur Hospital, UCT
Introduction: Periductal mastitis is an inflammatory condition of the breast in which the sub-areolar ducts are progressively damaged and become infected. Patients may present initially with sub-areolar inflammation (with or without an associated mass) or with abscesses and may progress to fistula formation and nipple changes.1 Surgical excision of the retroareolar ductal tissue is indicated for patients with multiple relapses or chronic mammary fistulas.
Methods: A retrospective review of all patients who underwent definitive surgery for periductal mastitis at Groote Schuur Hospital between March 2005 and March 2013 was conducted.
Results: A total of 25 patients had definitive surgery during this time period. Mean age at presentation was 36 years. Majority of patients presented with recurrent peri-areolar abscesses (96%) and fistulae (92%). An Adair's procedure was performed in 92% of patients. 8% of patients underwent excision of the nipple-areola complex. All patients were identified as smokers, and a median of 10 pack years was established. Patients had a mean of 14 clinical visits and a mean of 3 courses of antibiotics before definitive surgical intervention was offered. Positive cultures isolated Staphylococcus Aureus. Histology revealed plasma cell inflammation in 84% of patients. 2 patients developed recurrent fistulas on subsequent follow up.
Conclusion: Periductal mastitis remains a significant cause of long term breast morbidity. Our findings are in keeping with world literature, which demonstrate a younger patient profile and a strong association between severe periductal mastitis and cigarette smoking2. Behavioral modification may aid in ameliorating its clinical course.
REFERENCES
1. Dixon, J. M., et al. Treatment of Breast Infection. BMJ. 2011;342:d396
2. Almasad, J. K. (2006), Mammary duct fistulae: Classification and management. ANZ Journal of Surgery, 76(2006): 149-152.
IDIOPATHIC MOTILITY DISORDER OF THE BOWEL
I Bombil, A Kiss, M Tun, M Govender, S Mulira
Department of Surgery , Chris Hani Baragwanath Academic Hospital and the University of Witwatersrand, Johannesburg, South Africa
Introduction: Motility disorder of the bowel is rare and complex. Advanced in diagnostic modalities does not necessarily translate into improved patient care. Often patient spend years on laxatives before surgical option is considered. For the sake of simplicity; this condition is divided in two:
• Motility disorder of the bowel: colonic inertia.
• Functional pelvic outlet obstruction. Or combination of the two.
which further subdivide into congenital and acquired.
Our aim is to discuss the management plan of this rare but incapacitating condition.
To alert the health professionals on this condition for early referral.
Methods: Retrospective review of 6 cases treated at Chris Hani Baragwanath Academic Hospital (Unit 3) from 2007 to 2010. Parameters studied: demography, clinical presentation, time of onset, management, investigations and outcome.
Result: 6 cases of chronic constipation. All of black African origin. Mean age of 18 years (11-32), predominantly male with a 5:1 ratio. They all presented with severe constipation (1 stool per month) since birth in 83.3% (5/6) and one acquired (16.7%); their mainstay of treatment has been chronic laxatives with insignificant benefit. 5 patients had total colectomy (of which one as an emergency) and one had segmental resection. All patients improved except the only one in the acquired limb who relapsed and the condition progressed proximally in the small bowel. In the congenital limb, 4 patients are off laxatives and one had partial response and remains laxative dependent. There was no evidence of any pathology on histology.
Conclusion: Rare condition with unknown aetiology and challenging management. Surgery offers satisfactory result in selected cases.
PERCUTANEOUS ENDOSCOPIC GASTROSTOMY (PEG): THE MEDUNSA EXPERIENCE A Mokhtari, S R Ndlovu
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo
Medunsa Campus, Dr George Mokhari Academic Hospital, Ga Rankuwa Hospital, South Africa
Background: PEG Tubes are the preferred route for gastrostomy feeding in many different clinical contexts. This study set out to analyse the experience of the Surgical Department of a single academic institution over a period of 10 years looking at changing trends in the trusted method.
Design: A retrospective analysis of the databank of the Endoscopy Unit was conducted over a period of 10 years (2002 - 2013).
Results & Discussion: The data of a total of 246 patients were collected and analysed with regards to:
• Demographics
• Referral patterns from different clinical departments within the same institution looking at indications for the procedure
• Success of the procedure with regards to immediate commencement of gastrostomy feeding.
The major departments referring patients for PEG-tube insertion were our ENT (Ear, Nose and Throat) Department in the context of Head & Neck Cancers and our Neurosurgery Department.
It was found that even advanced Head & Neck Cancer patients can be successfully managed with
A PEG-Tube provided the Endoscopist conducts a thorough inspection of the oropharynx under sedation. Even the problem of trismus can be overcome by the usage of the "Syringe Technique" used routinely at Medunsa in this context.
The open gastrostomy insertion in theatre under General Anaesthetic with the added risk in sick patients could therefore be avoided in most patients. The PEG tube offers a longer lasting solution for patients requiring gastrostomy feeding compared with the open inserted gastrostomy tube.
Conclusion: Attention to detail can allow the Endoscopist to successfully insert PEG-tubes in most patients, even those with trismus and advanced Head & Neck Cancers
AN EPIDEMIOLOGICAL SURVEY OF INTERPERSONAL VIOLENCE AT A MAJOR TRAUMA CENTRE IN JOHANNESBURG, SOUTH AFRICA
S L Rayne2, C Sofianos2, D L Gersun2, M S Moeng1,2, J I Goosen2, K D I Boffard1,2
1 Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit
2 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
Introduction: Trauma and intentional injury form a major burden of disease in South Africa. We aim to describe the current pattern of interpersonal violence (IPV) occurring in Johannesburg, as experienced by a Level 1 trauma unit serving the area.
Methods: All patients attending the Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit were identified from records and those with a mechanism or injuries consistent with IPV selected. During the study period, attending medical and nursing personal were asked to record site of injuries, weapons used as described by the patient, and all initial investigations and management (within 24 hours). Exclusion criteria were non-intentional trauma and age under 16 years.
Results: 1334 patients attended the trauma unit within the forty day study period. 372 (27.9%) were due to IPV and 962 (72.1%) excluded as non-intentional injury. IPV affected 315 males (average 29.1 years) and 57 females (average 30.8 years). Only 35 patients (9.4%) were over 40 years. No weapon was used in one quarter of events (n=92, 24.7%). Weapons used included bottles (n=88, 23.7%), knife-like weapons (n=92, 24.7%) and blunt-type weapons (n=35, 9.4%). Only 30 patients (8.0%) sustained gunshot injuries. 137 (36.8%) patients required admission. This was more likely if the patient was male, over 40 years or had received a penetrating injury.
Conclusion: The trauma unit sees a large volume of trauma with a significant proportion of IPV. As is typical of interpersonal violence, most patients (and protagonists) are young, male and show a high level of weapon carriage.
LAPARASCOPIC HELLER MYOTOMY FOR ACHALASIA: OUR INITIAL EXPERIENCE
M Z Koto, T A Mosia
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Introduction and Aim: Laparoscopic Heller myotomy for achalasia has become the standard of care for patients with achalasia
The often cited advantages of minimally invasive surgery are better visualization, minimal morbidity and early recovery. We document our initial experience with this procedure.
Methods: The records of all patients with documented achalasia who underwent laparoscopic Heller's myotomy with antireflux procedure were prospectively collected between Jan 2005 and May 2013. The demographic data, clinical presentation, investigations, surgical procedure and outcome were recorded.
Results: There were 19 patients (11males and 8 females) with a mean age of 32yrs (23-45YRS)
The presenting symptoms were dysphagia and chest pain predominantly. All patients had gastroscopy and barium swallow and some of the patients had manometry done, laparoscopic Heller myotomy with antireflux procedure was done in all of the patients. All the patients reported significant improvement in swallowing ability afterwards except one patient who initially reported minimal improvement but improved over time. There was no conversion
Two perforations were noted and one was a redo patient. No mortality was reported.
Conclusion: Laparoscopic Heller myotomy is feasible and effective way of treating achalasia.
LAPAROSCOPIC INGUINAL HERNIA REPAIR: EXAMINING THE LEARNING CURVE
M Z Koto, T Monareng, S Nkosi
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr Georg Mukhari Academic Hospital
Introduction: Laparoscopic inguinal hernia repair has become a well-established treatment strategy that has been shown to be superior to open procedure. Despite all of this only 20% of groin hernias are repaired using this technique. The often sited reason is the perceived long learning curve. We embarked on an aggressive strategy since Nov 2011 to offer all our patients minimally invasive surgery for groin hernias.
Aim: We present our initial results using minimally invasive technique to repair inguinal hernia and compare this with results over a similar period in an established laparoscopic unit
Method: Records of all patients with groin hernia who underwent laparoscopic repair at Dr George Mukhari Academic Hospital (DGMAH) between November 2011 and May 2012 were looked at. We excluded all patients that were offered open operation because of incarceration or strangulation. We also looked at the records of patients done at SEBOKENG hospital between January 2009 and November 2009. We looked at the demographics, operating time, complications, conversion rate and recurrence between the two groups
Results: Total number of patients seen at DGMAH was 58(52 males; 6 females). Mean age 40, 3(15-81yrs). Average operating time was 90min. Complications: early recurrence =1. Conversion to open =4, conversion to TAPP= 6, hematomas =5(8%), seromas=7(12%) MORTALITY= 0 RIGHT SIDE= 43 LEFT SIDE= 8 BILATERAL= 7. At SEBOKENG Hospital Total number of patients 67(65 males 2 females) mean age = 45yrs. Mean operating time = 60min; complications: penile scrotal hematoma = 6(8%)seroma = 11(16%)bowel injury=1(1,5%) early recurrence =2 ( both patients offered TAPP) ; conversion to open = 0 conversion to TAPP = 2 (Large air leaks) average hospital stay = 1.5 d, mortality = 1 (MI). LIH = 20, RIH = 26, BILATERAL = 9, RECURRENT = 12, Most of the patients were seen at the clinic and had no recurrence at one month. The outcomes of the two groups were comparable
Conclusion: Laparoscopic inguinal hernia repair can be done safely with a short learning curve.
LAPAROSCOPIC ADHESIOLYSIS FOR ADHESIVE BOWEL OBSTRUCTION : THE INITIAL DR. GEORGE MUKHARI ACADEMIC HOSPITAL EXPERIENCE
K P Legodi, F O Ghoor; M Z Koto
Department of Surgery, Faculty of Health Sciences, School of Medicine, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Background: Adhesions are the almost unavoidable sequelae of abdominal surgery. The extent and frequency of these adhesions increase with the extent of the operation performed. About 6 % of all patients treated with laparotomy will undergo reoperation for adhesion - related complications. Release of these adhesions by laparotomy might exarcebate the adhesions leading to multiple hospital admissions and repeated laparotomies. Laparoscopic adhesiolysis might reduce the formation of new adhesions due to less operative trauma and might be a suitable alternative in the management of adhesions.
Objective: The aim of the study was to report on the initial experience of laparoscopic adhesiolysis at the Dr. George Mukhari Academic Hospital over an initial period of 18 months.
Methods: This is a retrospective study of patients who underwent laparoscopic adhesiolysis from November 2011 to April 2013. Patients were either operated on an emergency basis upon presentation or after failed conservative management.
Results: A total of 7 patients were included, 4 females and 3 males. All had an abdominal surgical scar, 4 midline, 1 appendicectomy scar, 1 bilateral tubal ligation scar and 1 trocar scar. 1 had an emergency laparoscopic assisted adhesiolysis (gangrenous small bowel) and 6 had delayed surgery (failed conservative management). There was 1 conversion to open laparotomy (dense adhesions),1 iatrogenic perforation and 1 mortality. There were no recurrences. Average hospital stay was 4,06 days.
Conclusion: Laparoscopic adhesiolysis is feasible but can be technically challenging when the adhesions are dense. It offers the benefits of minimally invasive surgery (decreased length of hospital stay, early return to normal activities and decreased morbidity). In our study, our results compared relatively well to already reported series.
LAPAROSCOPY IN TRAUMA, OUR EXPERIENCE
E V Ndlovu, M D Ntsoane, M Z Koto
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Introduction: There has been a huge skepticism about the use of laparoscopy in trauma patients; this has been attributed to the data released in the early nineties where laparoscopy was associated with high missed rate of small bowel injuries.
Aim: To collect data in all trauma patients treated with laparoscopy in our institution
Methods: We prospectively collected the records of all patients treated at our institution using minimally invasive surgery. We included all patients who were offered diagnostic laparoscopy for trauma (penetrating & blunt). The patients' demographic data, operative findings, procedure and outcomes were looked at, between NOV 2011 and MAY 2012. We excluded all patients who were haemodynamically unstable and patients who were offered open operation.
Results: All patients treated using this modality were hemodynamically stable. 95 patients were included in our series (90 males & 5 females), age ranges from 9- 52 years, mean age 32, operative findings included: small bowel perforations 47, colonic perforations 27, stomach perforations 7, gallbladder perforations 5, inferior vena cava injuries 1, diaphragmatic injuries 36, non-remedial 6, conversion to open 1.
Mean operating time 167 minutes, range 35 minutes-385min, hospital stay, range 2days- 50 days mean 10 days.
Conclusion: Laparoscopy in trauma patients is certainly a safe modality in the haemodynamically stable patient and it should be done under supervision.
TOTAL THYROIDECTOMY AT DR GEORGE MUKHARI ACADEMIC HOSPITAL
M Bondo
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Background: Total thyroidectomy is the treatment of choice for malignant thyroid diseases. In an endocrine unit it is the preferred therapy for benign disease. However it still a debate as a first choice treatment for benign diseases. The objective of this study, was to evaluate whether total thyroidectomy can safely be done by general surgeons for both malignant and benign diseases of the thyroid.
Methods: 22 patients underwent total thyroidectomy at DGMAH, from November 2011 till 30 April 2013. Indication for surgery were:
• Malignant diseases
• Multinodular goitre
• Failure of medical treatment for Grave's disease Parameters Analysed:
• Gender, age, post-operative complications and final pathology.
Results: 22 total thyroidectomies were performed.
• 15 multinodular goitres
• 4 malignancies
• 3 Grave's disease
21 Female patients and one male patient. Age ranged from 33 years to 69 years. Final pathology:
• 7 Colloid goitres
• 8 multinodular goitres
• 4 malignancies - 3 papillary
• 1 follicular
• 3 Grave's disease
One patient had temporary laryngeal nerve palsy. One patient had permanent laryngeal nerve damage. No hypoparathyroidism.
Conclusion: Total thyroidectomy is done at DGMAH which is not a big volume centre and does not have an endocrine unit. We had one patient out of 22 patients with nerve damage.
When performed by an experienced general surgeon, total thyroidectomy is a safe procedure, and can reduce significantly the rate of re-operation for recurrent disease.
ISOLATED MYCOBACTERIUM TUBERCULOSIS OF THE THYROID GLAND IN A HIV NEGATIVE PATIENT. A CASE REPORT AND REVIEW OF LITERATURE
A Maraj, A Kiss, T Luvhengo
Chris Hani Baragwanath Hospital, Soweto and University of the Witwatersrand, Johannesburg
Background: Thyroid abscesses caused by tuberculosis (TB) are rare, even more so in patients who are HIV negative. Usually the main causative organism is Staphylococcus aureus. Only a few cases of TB abscess of the thyroid have been reported. We present a case of Mycobacterium TB of the thyroid gland in a HIV negative patient. Reasons pertaining to why infections of the thyroid are rare include the antibacterial properties of colloid; high blood flow in thyroid and the presence of high iodine content concentrated in the thyroid.
Aim: This report describes a case of thyroid tuberculosis abscess in a HIV negative patient.
Methodology: This is a case report of a 63 year old HIV negative female who presented with a one year history of an anterior neck mass. She complained of pain and compressive symptoms, i.e. difficulty breathing, stridor, hoarseness and dysphagia. Fine needle aspiration cytology was performed and Acid Fast Bacilli were observed.
Results: The patient was successfully treated with antituberculosis drugs.
Conclusion: In our local setting, thyroid TB should be suspected in a HIV negative patient who presents with a painful goitre. FNAC should be performed to exclude malignancy as patients may have features similar to thyroid malignancy. The mainstay of management of thyroid TB is anti-TB treatment as patients respond well to this.
SALMONELLA THYROIDITIS- A CASE REPORT AND REVIEW OF LITERATURE
A Maraj, A Kiss, T Luvhengo
Chris Hani Baragwanath Hospital, Soweto, and University of the Witwatersrand, Johannesburg
Background: Thyroid abscesses caused by Salmonella are rare. Usually the main causative organism is Staphylococcus aureus. HIV infection has reached endemic proportions in South Africa. Patients with HIV may present with rare conditions such as Cytomegalovirus intestinal perforations or upper gastrointestinal tract bleed secondary to Kaposi sarcoma. Salmonella infection typically involves the hepatobiliary system, bones, joints and soft tissue. Infection of the thyroid is rare and when it occurs in immuno-compromised patients it is associated with high mortality. We present a case of Salmonella thyroiditis in a HIV positive patient who was successfully treated with antibiotics and incision and drainage. Such rare conditions should be considered when managing HIV positive patients.
Infective thyroiditis is rare and reasons include the following: (1) thyroid colloid material contains anti-bacterial properties; (2) thyroid gland receives a high blood flow; (3) storage of excess iodine in the thyroid is protective against infections; (4) in hyperthyroid states phagocytes have an increased physiological ability to destroy bacteria; and (5) thyroid hormones have antibacterial roles.
Aim: This report describes a case of Salmonella thyroiditis in a HIV positive patient.
Method: This is a case report of a 48 year old HIV positive female on Highly Active Anti-Retroviral Treatment who presented with a one year history of an anterior neck mass with marked enlargement over the past three months. She also complained of pain, compressive symptoms (including difficulty in breathing, stridor, hoarseness, dysphagia), palpitations, sweating and loss of weight. Fine needle aspiration cytology was performed and Salmonella species cultured.
Results: The patient was successfully treated with antibiotics and incision and drainage.
Conclusion: Even though thyroid abscesses are rare, they need to be considered in a HIV positive patient presenting with a painful anterior neck mass. As these patients may have features suggestive of thyroid malignancy FNAC should be done. The mainstay of treatment for salmonella thyroid abscess is antibiotics and incision and drainage.
ELEPHANTIASIS OF THE SCROTUM AND PENIS
I Bombil, A Kiss, K G Panda, E Tshimpaka
Department of Surgery , Chris Hani Baragwanath Academic Hospital and the University of Witwatersrand, Johannesburg, South Africa
Introduction: Elephantiasis of the scrotum and penis is a chronic condition caused by obstruction of lymphatic drainage due to various causes: parasite (filariosis), bacterial infection (lymphangitis), iatrogenic and idiopathic.
It is characterised by inflammation and blockade of the lymphatic circulation resulting in hypertrophy of the skin and subcutaneous tissue (lymphoedema). Its management is challenging both for the general surgeon and surgical specialities (plastic and urology). Our asim is:
1. To present these cases and highlight the psychosocial impact of this condition to the individual affected.
2. To create awareness of this rare condition to the health professionals in order to channel the patient to the right speciality for management.
Methods: Presentation of two cases treated at Chris Hani Baragwanath Academic Hospital and review of the literature.
Results: Two African male patients aged 49 and 61 years presented with elephantiasis of the scrotum and penis evolving over 11 and 8 years respectively. They both had diverting colostomy +inadequate incision and drainage of perianal sepsis prior to presentation. There was evidence of long standing perineal hydradenitis suppurativa poorly treated. Degloving of the penis and scrotum was offered followed a week later by a split skin graft with successful cosmetic outcome. Erection is preserved but the patients are still reluctant to resume sexual activity due to shame of colostomy.
Conclusion: Elephantiasis of the penis and scrotum is uncommon and challenging to the patient. Lack of awareness result in marked delay in referral and management. Surgical treatment is satisfactory both cosmetically and sexually.
QUALITY OF VITAL SIGN RECORDINGS AND ASSESSMENT OF THE MODIFIED EARLY WARNING SCORE TO DETECT AND INTERVENE ON PHYSIOLOGICAL DERANGEMENTS
C M Keene, V Y Kong, C Aldous, D L Clarke
Department of Surgery, Edendale Hospital, Pietermaritzburg Metropolitan Hospital Complex, UKZN
Introduction: Conscientious monitoring of vital signs is necessary to determine the requirement for early medical intervention. The Modified Early Warning (MEW) Score assesses the need to intervene based on vital signs alone. This study audited the recording of vital signs and assessed the need for intervention based on MEW scores.
Methodology: Over 6 weeks the details of all patients in the Acute Care surgical wards at Edendale Hospital were collected, noting the vital signs recorded in the chart and those measured by the investigator. The MEW score was retrospectively calculated for both sets of data.
Results: Details of 181 patients were collected. Vitals recordings had completion rates of 81% for heart rate, 98% for blood pressure, 88% for respiratory rate, 92% for temperature and 40% for the Glascow Coma Scale. Recorded vitals underestimated the MEW score in 60% of patients. 80% had a MEW score requiring 4 hourly vitals checks - carried out in 2% of these patients. 86% had a MEW score not necessitating escalation of care - of these 33% had an investigator MEW score that required escalation.
Conclusions: Vital sign recording was incomplete and measurement was of poor quality: recorded values underestimated the severity of physiological derangements so necessary interventions were not implemented. The MEW score may be an effective method to improve the detection of physiological deterioration and provide a framework to act on it. The correct application requires education to improve vitals measurement and recording, coupled with administrative change in charts to enable completion.
QUALITY OF FLUID BALANCE RECORDING IN PATIENTS WITH PHYSIOLOGICAL DERANGEMENTS IN AN ACUTE REGIONAL SURGICAL UNIT
C M Keene, V Y Kong, C Aldous, D L Clarke
Department of Surgery, Edendale Hospital, Pietermaritzburg Metropolitan Hospital Complex, UKZN
Introduction: At Edendale Hospital sicker surgical patients requiring acute physiological support are monitored in the Acute Care ward. Fluid balance is an important component of management, necessitating strict monitoring. This prospective study audited the recording of fluid balance to assess a baseline of quality in this ward.
Methodology: Over 6 weeks, details of all patients were collected, noting whether doctors completed the prescription, the correct fluid and rate were recorded and charts were complete. IV fluid input, per os input and output were recorded, noting whether the totals were added, the balance was calculated and whether the calculation was correct.
Results: 164 of the 181 patients had fluid charts prescribed. Doctors gave fluid directions in 98%. 79% recorded the correct fluid. 58% recorded the correct amount and rate. 66% of charts were complete. IV intake was recorded in 91% with 37% totalled. 18% recorded per os fluid and 26% of these were added. Output was completed in 75%, and totalled in 37%. The fluid balance was calculated in 29% and was correct 72% of the time.
Conclusions: Fluid balance recording is of poor quality, with high rates of qualitative and quantitative error in fluid administration. This compromises management of already physiologically challenged patients. Few charts had calculated balances and only a proportion were correct - a potential second hit that might not be tolerated by unstable patients. Education may improve the accuracy and completeness of fluid balance recording, but a systems intervention could be more appropriate and have more lasting effects.
REDCap FOR THE MANAGEMENT OF CLINICAL DATA
M Klipin, I A Maré
Department of Surgery, University of the Witwatersrand, Johannesburg
REDCap (Research Electronic Data Capture) is a web-based database application developed by the Bioinformatics Core at Vanderbilt University. REDCap licenses are given to Consortium Partners free of charge, provided REDCap is used in a non-commercial or academic setting. The user interface is intuitive and easy to use, making project design quick and effortless. Data entry is expedited by a variety of instruments like checkboxes, radio buttons, date/time pickers and visual analogue scales. Workflow can be further improved by using calculated fields and branching logic. REDCap is also mobile device friendly, allowing users to log in with smartphones or tablets. Wits Faculty of Health Sciences brought their REDCap server online in August 2012, and already has a user base of around 100, with more than 60 actively involved in approximately 50 projects. Future objectives for the Faculty include the establishment of a Medical Bioinformatics division and the creation of a central data repository for Healthcare and Medical research.
AN AUDIT OF HEPATOBILIARY TRAUMA WITHIN THE PIETERMARITZBURG METROPOLITAN TRAUMA SERVICE
C Jones, J L Bruce, G L Laing, C Aldous, G V Oosthuizen, D L Clarke
Department of Surgery, Pietermaritzburg Metropolitan Complex, University of Kwa-Zulu Natal
Introduction: Complex management algorithims have been proposed for these injuries. Our university pioneered a selctive conservative approach. We reviewed our management of these injuries.
Methods: Since 2012 a prospective electronic database was kept in the Metro from which data on patients with hepato-biliary injuries were retrieved.
Results: Hepato-biliary trauma accounted for 94 acute admissions. Forty-three were blunt and 50 penetrating. One patient had a combined injury. The most common blunt injury was motor vehicle accidents, 21 cases, followed by eight pedestrian vehicle accidents, five assaults, and four falls. The average age of these patients was 29yrs (1-70) with a male predominance: 31 vs 13 and mean injury severity score (ISS) of 17 (4-34). Most blunt trauma were polyregional, with isolated abdominal injuries accounting for 10 cases, thoracic injuries the most common association present in 26 cases. Nineteen patients required a total of 26 operations, with five deaths. Nineteen patients needed Intensive Care and one High Care. Penetrating trauma included 21 gunshots and 30 stabs. The demographics were similar to the blunt trauma group, with lower mean injury severity score (ISS) of 12 for both groups. Two deaths were recorded in the gunshot group. Forty-three patients required 70 operations prior to discharge, with 17 needing Intensive Care and a further three High Care support.
Conclusion: Hepato-biliary trauma, challenging to manage, often requires extensive resources and operative care for a successful outcome. Appropriate application of selective conservatism is key.
PENETRATING CARDIAC INJURIES: A COMPARISON BETWEEN GSW AND STAB INJURIES AT A SINGLE CENTRE IN JOHANNESBURG
M S Moeng, A N Chaane, S R Motilall, S Gyebi, R Jacks, M Morna, J Goosen
Trauma Unit, CH-Johannesburg Academic Hospital, Johannesburg
Introduction: The higher energy in Gunshot injuries (GSW) is likely to result in complex injuries that may result in death at the scene. As a result, fewer GSW to the heart survive to arrive alive at the emergency department, compared to the stab cardiac injuries. Management of all cardiac injuries may be complicated by physiological changes over and above the anatomical injuries sustained. A comparison between these two mechanisms may help us understand these injuries better.
Aim: Evaluate injury patterns and outcomes in patients presenting with cardiac GSW compared to cardiac stab wound at a single Trauma centre.
Method: All penetrating injuries presenting at CMJAH between 01/04/2005 and 30/03/2012.Demographic data, anatomical injuries sustained, physiological scores, haemodynamic status, preferred surgical incision, surgical findings, outcomes, post-mortem findings were noted. Data was recorded on an excel spreadsheet, and Statistica V8 was used as a tool for statistical analysis. P value<0.05 was considered statistically significant.
Results: Eighty six (n=86) patients were recruited for the study. GSW cardiac injuries were in 11 patients all of whom were male. Only 9 of the 75 stab injuries were in female patients. Median age was 29.5yrs in GSW compared to 27.5yrs, and the median ISS of 29 v/s 25 in stab injuries. Forty-five percent (45%) of GSW were unstable on arrival compared to 31% of stab wounds. Emergency room thoracotomy was required in about a third in each group due to worsening haemodynamic status. Sternotomy was the most common incision in theatre for stab injuries. Right and left ventricles were commonly involved injuries in both mechanisms. The left atrium was the least involved chamber. Mortality rate from GSW were double those in stab injuries.
Conclusion: Cardiac stab injuries are seen more frequently than GSW. Overall mortality was high, with GSW mortality rate double that of stab injuries.
UNDERSTANDING THE BURDEN OF TRAUMA TO THE JOHANNESBURG TRAUMA UNIT IN THE PAST EIGHT YEARS: A PARADIGM SHIFT
M S Moeng, S R Motilall, S Gyebi, R Jacks, S Max, J Goosen, K D Boffard
Trauma Unit, CH-Johannesburg Academic Hospital, Johannesburg
Introduction: Trauma remains a major pandemic in RSA. Unfortunately we still do not have a comprehensive National Trauma registry that can allow us to evaluate the extent of the Trauma disease burden. The emphasis on mortality figures as a measure of this disease is only a tip of the iceberg.
The Charlotte Maxeke Johannesburg Hospital Trauma unit (Johannesburg Trauma unit) participated in the development and implementation of the Medibank: an electronic Trauma data collection system. This was implemented since January 2005, initially capturing only priority 1 (severe trauma patients).
Aim: Evaluate epidemiological data of severe trauma patients (P1) entered into the Medibank at Johannesburg Trauma unit.
Method: All severe patients who presented to the Johannesburg Trauma unit and were entered in the Medibank from Jan 2005 till December 2012 were included in the study. The demographics (age, sex, mechanism of injury), injury patterns, ISS , NISS, and mortality outcomes were evaluated. Comparisons were made between the different years to observe any trends. Statistical analysis was performed and a p value of <0.05 was considered significant.
Results: The 21-45 year old's were the most affected by trauma than any other age group. Overall, blunt trauma accounted for 50.28% of injuries, penetrating trauma 48.64% of the cases and burns 1.08%. Though stab injuries were the highest isolated cause of injury. The highest average ISS score was noted in burns group, followed by blunt trauma, with the lowest ISS score noted in the stab injuries. Blunt Trauma had the highest NISS score and again stabs had the lowest score. Predicted mortality was worst in blunt trauma group.
Conclusion: Blunt trauma is the most common mechanism, and is also associated with the high mortality. Medibank simplifies analysis of patterns of injury, which adds value in unpacking challenges to the health system. More effort is required to reduce the burden of Trauma disease. A national Trauma data system is urgently required to optimize our prevention strategy.
PENETRATING CARDIAC INJURY: IS PELONOMI TRAUMA UNIT UP TO STANDARD?
P Taylor, E Arko-Cobbah
Dept of Surgery, Pelonomi Trauma Unit, Univ of the Free State, Bloemfontein
Background: Penetrating Cardiac Injuries (PCI) are seen as one of the most lethal injuries with only 6% of patient surviving the pre-hospital phase. Although initially fatal, the mortality rate decreases dramatically if the patient survives until the hospital phase. Recent international data indicates a mortality rate ranging from 3,66 to 32,9% over the last 13 years. Pelonomi Trauma unit is the only public trauma unit in the Free State province and manages about 900 patients per month. The purpose of this study is to establish the outcome of PCI at Pelonomi Trauma unit and to compare the outcome with the world literature.
Method: A retrospective case series was performed of all patients presenting with PCI to Pelonomi Trauma Unit from 2008 - 2012.
Results: Forty-one patients were included in the series. One patient had incomplete data, therefore only 40 patients' data were used. All the patients had penetrating stab injuries. Thirty-nine (95,12%) were male patients with only two (4,88%) female patients. The median age was 26 years (range 13 - 61). Twenty-two (55%) patients were hemodinamically shocked at presentation with 19 (47,5%) patients receiving more than 2 ℓ of resuscitation fluid prior to surgery. Twenty (50%) patients were stabbed in the precordial area. The diagnosis of penetrating cardiac injury was confirmed by ultrasonography on 29 (72,5%) patients prior to surgery. In 19 (47,5%) patients the time from first being seen until anaesthesia given was longer than 2 hours.
Sternotomies were performed in 36 (87,8%) with 19 (47,5%) of patients having right ventricular injuries. Seven patients died, giving an overall mortality of 17,07%. In 4 patients front room thoracotomies were done with only one mortality (25%). The mean hospital stay was 9 days.
Conclusion: Pelonomi Trauma Unit is up to standard and has acceptable results regarding mortality rate in PCI. By improving the resuscitation protocol in hemodynamic unstable patients and by reducing time spent before surgery the outcome could still be improved for even better results.
LAPAROSCOPIC GASTRECTOMY. THE DR GEORGE MUKHARI EXPERIENCE
M L Phakula, M Z Koto
Department of General Surgery, School of Medicine, Faculty of Health Sciences, , University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Background: Laparoscopic gastrectomy is a well recognised management for benign gastric pathology. Since the introduction of laparoscopic gastrectomy, the indications have been extended to include early gastric cancer and palliative resection. High volume centres have reported good outcomes with this form of management.
Aim: To report our initial experience with laparoscopic gastrectomy for both benign and malignant disease at our institution.
Method: we did a retrospective analysis of all the laparoscopic gastrectomies done at The Dr George Mukhari Academic Hospital from November 2011 to April 2013. All patients had a laparoscopic gastrectomy, both emergency and elective were included. Those who had open surgery were excluded from the study.
Results: Between November 2011 and April 2013, a total 11 laparoscopic gastrectomies were done. There were 4 males and 6 females with an average age of 46y (20-75). 4 gastrectomies were done for benign disease and 7 for malignancies. Total gastrectomies were done on 3 patients. The average operating time was 262 min. There was one patient converted (Hostile Abdomen). One patient had a duodenal stump leak and another developed acalculus cholecystitis. Only 1 mortality reported.
Conclusion: Even though the numbers are still small, our results show that laparoscopic gastrectomy is feasible with acceptable morbidity and mortality.
THE CHARLES OPERATION REVISITED : THE SURGICAL MANAGEMENT OF CHRONIC LYMPHOEDEMA - A CASE REPORT
A Mokhtari, D H Mokone
Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital
Introduction: Chronic Lymphoedema of the lower legs is an incurable and debilitating disease causing mayor functional impairment, anxiety and depression. The disease causes at its advanced stages fibrosis and skin thickening leading to a vicious cycle of recurrent lymphangitis and cellulitis. Conservative treatment modalities can help to reduce the suffering. Microsurgical techniques are often contraindicated in advanced stages of the disease.This leaves the surgeon often with a final option to consider debulking procedures. Those operations come, however, with a bad reputation due to their unacceptably high morbidity.
Objective: We report on the surgical management of a young adult with chronic lymphoedema of the leg looking at two unique scenarios:
• We were able to harvest and bank the patients' own skin prior to the debulking procedure leaving us with a large amount of transplantable skin.
• Modern wound management material was made available thanks to the generous support of Smith and Nephews allowing us to use modern Silver dressings and Negative Pressure Vacuum Pumps.
Material and Methods: Case Report on a single patient, demographics with surgical history and details of surgical procedure conducted in three stages.
Results: Successful management of chronic lymphoedema based on a telephonic interview 6 months after the operation with full return to employment as documented in a series of photographs.
Conclusion: A modification of the Charles Procedure can lead to acceptable longterm results in advanced stages of chronic lymphoedema provided the surgeon provides meticulous surgical care and applies modern tools of wound management.
A CADAVERIC STUDY OF THE ARTERIAL SUPPLY OF THE SIGMOID COLON WITH SPECIAL ATTENTION TO THE PRESENCE OF A SIGMOID MEGACOLON LOOP
P Humphries1, L Prigge1, A Mokthari2, H R Human1
1 Department of Anatomy, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Garankuwa, South Africa
2 Department of Surgery, School of Medicine, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Dr George Mukhari Academic Hospital, Garankuwa, South Africa.
Background: An increase in the prevalence of sigmoid volvulus has been observed, especially in younger patients at Dr George Mukhari Hospital. Therefore, a new minimally invasive procedure for the resection of the elongated sigmoid colon associated with sigmoid volvulus is being developed. However, before any clinical trials can be performed, in depth knowledge related to the specific blood supply of the sigmoid colon is required, and the Anatomy department at Medunsa was approached by the Surgical Department at the Dr George Mukhari Hospital. A cadaveric study was suggested to investigate the exact blood supply of the sigmoid colon as it pertains to resection of sigmoid volvulus.
Design: A descriptive quantitative study was undertaken to investigate the blood supply of the sigmoid colon of the total cadaveric sample, pre-dissected by second year medical students and dentistry students. A total of 45 abdominal cavities and gastro-intestinal tracts were dissected under the supervision of the anatomy demonstrators to ensure accurate and meticulous precision during the exposure of the arteries contained within the mesentery of the colon. Three cadavers were excluded due to incomplete dissection. All the arteries supplying the sigmoid colon were noted and photographed.
Results and Discussion: In the cases where sigmoidal elongation was observed, the quantity of sigmoidal arteries arising from the inferior mesenteric artery, correlated to the known values of two to five sigmoidal arteries. However, the occurrences of several arterial trunks that branch again into two to three branches were observed. These branches often united to form several arcades prior to supplying the sigmoid colon. Therefore four to eight branches ultimately supply the sigmoid colon, making it extremely vascular. The point for arterial ligation is known as Sudeck's critical point, described in literature as the important landmark for resections of sigmoid volvulus. This landmark is found at a point on the inferior mesenteric artery just proximal to the origin of last sigmoidal artery. Thus ligation of any artery should be done at Sudeck's point to ensure sufficient arterial supply to colon & rectum.
Conclusion: Knowledge of the deviations in arterial distribution will ultimately assist in decreasing the possible complications surgeons might encounter while attempting resection of an elongated sigmoid colon, ensuring sufficient blood supply to viable bowl while attempting resection of the elongated sigmoid colon to prevent future twists in the sigmoid colon.
VARIATION IN THE COURSE OF THE SUPERIOR SAGITTAL SINUS AT THE CONFLUENCE OF SINUSES - AN INVESTIGATION OF SKULL SPECIMENS IN A SOUTH AFRICAN POPULATION GROUP.
G Venter, B L Viljoen
Department of Anatomy, School of Pathology and Pre-clinical Sciences, Faculty of Health Sciences, University of Limpopo (Medunsa Campus), South Africa.
Background: The confluence of sinuses is defined as "the dilated posterior end of the superior sagittal sinus, situated to one side of the internal occipital protuberance, where it turns to become a transverse sinus. It also connects with the occipital sinus and contralateral transverse sinus. The size and degree of communication is variable". So the question arises: Why is it important to study the variations found at the confluence of sinuses? Variations within this area of the confluence of sinuses might be a potential problem for a neurosurgeon planning an interventional procedure such as an occipital craniotomy or repair of an arterio-venous fistula. Thus this study focuses on the variations found within the confluence of sinuses as to better prepare the neurosurgeon for a potential procedure. The aim of this study is threefold. Firstly, to investigate the variations found in the joining of the dural venous sinuses in the area of the confluence of sinuses in a sample of South African adult skull specimens, then to compare results found in this study with those of other population studies and lastly, to investigate whether the variations found in this area are linked to gender (male or female).
Design: A total of 300 South African skull specimens were used to determine the variations found in the area of the confluence of sinuses. The sample consisted of 240 males and 60 females. Digital photographs were taken and the sex of the specimens was documented.
Results and discussion: The variations in the region of the confluence of sinuses were divided into four categories: Type A: Confluence; Type B: Bifurcation; Type C: Right dominant and Type D: Left dominant. Type A was found in 12%, Type B in 15.7%, Type C in 56.3% and Type D in 16% of the specimens. The most common drainage type in the current study was Type C or the right-dominant type for both males (45.3%) and females (11%).
Conclusion: In comparison to other studies, it is shown that the variation found in the region of the confluence of sinuses is diverse and might not necessarily be the same for different population groups. Although there is a difference in the pattern of drainage between males and females, it is not statistically significant different in the current study as well as that reported in the literature.
WHITHER MUCIN RESEARCH IN CAPE TOWN?
Anwar Suleman Mall, Santhoshan Pillay, Julia Peacocke, Jeffery Dorfmann and Delawir Kahn
Division of General Surgery and Medicine, UCT, ICGEB and UCT Division of Immunology, South Africa
Introduction: Sub-Saharan Africa is the world's worst HIV-AIDS affected region. More interventions to manage this pandemic are urgently required. Transmission of the virus through an exchange of saliva is rarely known to occur. This project sought to further describe findings that crude saliva and its purified mucins inhibit HIV-1 using an in vitro pseudoviral assay.
Methods: Mucus was extracted in 4M guanidinium hydrochloride, and a cocktail of protease inhibitors, pH 6.5. Sepharose 4B gel filtration was used to separate MUC5B and MUC7 in saliva and mucins were purified by density-gradient ultra-centrifugation in caesium chloride. SDS-PAGE analysis and Western blotting determined the size, purity and identity of the mucins. The inhibitory activity of crude saliva and purified MUC5B and MUC7, from HIV-negative (n=20) and HIV-positive (n=20) donors, was tested by their incubation with subtype A and C HIV-1 pseudovirus and infection of susceptible epithelial tumour cells (genetically modified TZM-BL cells).
Results: Crude HIV-negative and HIV-positive saliva inhibited HIV-1 in an in vitro pseudoviral assay in a dose-response nature. Salivary MUC5B neutralises HIV-1 pseudoviruses CAP45 (KZN) and DU422 (Durban) of subtype C AND Q168a.2 (Kenya) of subtype A, when purified from HIV-negative and HIV-positive individuals. The neutralisation capability of MUC5B IC50 15.40ug/ml appears greater than MUC7 IC50 26.78ug/ml for the HIV-negative group.
Conclusion: Crude saliva and its purified mucins from both uninfected controls and HIV positive individuals inhibited HIV-1 in an in vitro pseudoviral assay. The different inhibitory capabilities are postulated to be due to altered glycosylation of the mucins.
DOES TIME OF THE WEEK AND MONTH, AND SEASONAL CHANGE, INFLUENCE THE NUMBER OF PATIENTS SEEN IN A MATURE TERTIARY TRAUMA CENTRE?
KL Milford, PH Navsaria, AJ Nicol, D van Breda
Trauma Centre, Groote Schuur Hospital Trauma Centre, University of Cape Town
Introduction: Patient volumes in trauma units fluctuate dramatically, and popular belief holds that these fluctuations are influenced by time of week and month, and season. The aim of this study was to determine whether or not such fluctuations truly exist in an urban trauma unit.
Methods: Patient registers at the Groote Schuur Hospital trauma unit were evaluated, and data collected for a period of 17 months. Patients were divided into three presentation categories: vehicle-related accidents; interpersonal assault; and non-vehicle-related accidents. Shifts were classified as 'weekday' or 'weekend'. 'Mid-month' and 'month-end' weekends were isolated, as was one summer and one winter season within the data period. The mean number of patients presenting with each trauma type within each time division was calculated and compared, and this comparison assessed for statistical significance using a heteroscedastic or homoscedastic t-test, depending on variances.
Results: Weekends show significant increase in all trauma types. This is particularly marked in the interpersonal violence category. Month-end weekends show a slight but statistically significant increase in total patients volumes compared to mid-month weekends. The interpersonal violence category again shows the most marked difference. Similarly, patient numbers are slightly increased in summer compared to winter, but this difference is only statistically significant in the interpersonal violence category.
Conclusion: Weekends are markedly busier at this trauma unit than weekdays, but time of month and season show less variation. This has potential impact on staffing strategies in this and other similar units.
VIOLENCE AND SUBSTANCE ABUSE AT GROOTE SCHUUR HOSPITAL TRAUMA CENTRE
A Nicol, P Navsaria, C Ward
SAVI Group of Investigators(UCT) Trauma Center, Groote Schuur Hospital and University of Cape Town
Introduction: Violence and the associated injuries are the second leading cause of death in South Africa. South Africa also has one of the highest levels of alcohol consumption per capita in the world. Alcohol and drugs are a major risk factor for high trauma rates. Concerted action is needed by the health care system in South Africa to address linkages between alcohol and other drug use and trauma, but accurate and current data is urgently required prior to implementation of interventions.
Aim: To determine the relationship between alcohol, drugs, and interpersonal violence in patients presenting to a South African Trauma Centre.
Method: Prospective study on patients presenting to the Groote Schuur Hospital Trauma Centre as a result of interpersonal violence over an idiolised month (2-weeks). Adult patients over the age of 18-years were screened with a breath alcohol analyser (passive and active). Urine was obtained for analysis of metamphetamines, cannabis, cocaine, opiates, benzodiazepines and mandrax.
Results: One-hundred-and twenty-two patients (16 females), mean age 30-years (range 18-73) were included in the study. Fifty-eight tested (47.5%) tested positive for alcohol. Cannabis was present in 41%, metamphetamines in 33%, mandrax in 25%, opiates in 14%, cocaine in 0.8% and benzodiazepines in a single patient.
Conclusion: Alcohol continues to show a major link with violence. There is an extremely high incidence of metamphetamines (33%) and mandrax (25%) abuse. Violence prevention strategies will have to address this trend and routine screening must be introduced in all hospitals dealing with injuries sustained from interpersonal violence.
NONOPERATIVE MANAGEMENT OF PENETRATING LIVER INJURIES
P Navsaria, M Hommes, G Valstar, S Edu, J Krige, A Nicol
Trauma Center, Groote Schuur Hospital, University of Cape Town
Background: Nonoperative management (NOM) of penetrating liver injuries is yet to gain universal acceptance. The aim of this study was to assess the feasibility and safety of selective nonoperative management of such injuries.
Patients and Methods: Prospective, protocol-driven study, which included all penetrating liver injuries admitted to a level I-type trauma center, over a 4-year period. Patients who were hemodynamically stable and had no signs of generalised peritonitis with either a missile trajectory traversing right upper quadrant and/or localised RUQ tenderness underwent CT scan evaluation to detect the presence of a liver injury. In the absence of CT scan findings suggestive of hollow a viscus injury, the patients were observed with serial clinical examinations. Outcome parameters included survival, complications, need for delayed laparotomy, and length of hospital stay.
Results: During the study period, there were 225 patients with penetrating injuries to the liver: 149 (66.2%) patients met the criteria for immediate operation and 76 (33.8%) [42 gunshots and 34 stab wounds] patients were selected for nonoperative management of their liver injury. The mean injury severity score was 16 (range 5-26). The liver injury grading was: grade I-10, grade II-26, grade III-28, grade IV-11(40.3%) and grade V-1. Associated injuries related to the same missile causing the liver injury were: kidney (12), diaphragm (49), lung contusion (16), haemo/pneumothorax (65) and rib fractures (15). Complications included: failed abdomen observation (2), liver abscess (1), biliary fistula (3), retained haemothorax (3), and nosocomial pneumonia (4). The mean hospital stay was 9 (range 3-57) days. There was no mortality.
Conclusion: The nonoperative management of appropriately selected patients with penetrating liver injuries is highly feasible, safe and effective.














