Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.2 Cape Town Jun. 2016
CASE REPORT
Solitary extramedullary plasmacytoma of the colon, rectum and anus
M MjoliI; N VorajeeI; J HowlettI; Y NaidooII; T MadibaIII, IV
IDepartment of Surgery, Pietermaritzburg Hospital Complex, Pietermaritzburg, South Africa
IINational Health Laboratory Service, Greys Hospital, Pietermaritzburg, South Africa
IIIDepartment of Surgery, University of KwaZulu Natal, Durban, South Africa
IVGastrointestinal Cancer Research Centre, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
Solitary extramedullary plasmacytoma (SEP) is a neoplastic proliferation of a single clone of plasma cells that occur outside of the bone and bone marrow. It is rare, commonly occurring in the head and neck region, followed by the gastrointestinal tract. The aetiology, risk factors, natural history and consequent treatment are not well defined. We report an unusual case of SEP of the colon in an human immunodeficiency virus (HIV)-infected patient. The patient was managed with colonic resection and made an uneventful recovery. To our knowledge, this is the first reported case of extramedullary plasmacytoma of the colon and rectum in association with HIV infection.
Solitary extramedullary plasmacytoma (SEP) is a neoplastic proliferation of a single clone of plasma cells that occur outside of the bone and bone marrow.1 It is rare, commonly occurring in the head and neck region, followed by the gastrointestinal tract.2 The aetiology, risk factors and natural history and consequent treatment are not well defined.2 We report an unusual case of SEP of the colon in an human immunodeficiency virus (HIV)-infected patient. The patient was managed with colonic resection and made an uneventful recovery. To our knowledge, this is the first reported case of extramedullary plasmacytoma of the colon and rectum in association with HIV infection.
Case report
A 42-year-old African man presented to hospital with frank rectal bleeding, preceded by a four-month history of abdominal cramps. He had human immunodeficiency virus (HIV) infection with a CD4 count of 151cells/mm3, and had been on highly active antiretroviral therapy for four years. The physical examination revealed a healthy-looking middle-aged man with no stigmata of immune deficiency. A fullness and slight tenderness in the left iliac fossa was noted. The patient's baseline blood tests were normal, and included a full blood count, urea and electrolyte analysis, liver function tests, and calcium phosphate and magnesium analysis. The abdominal ultrasound and computed tomography scan revealed a left-sided colocolic intussusception with a polyp as a lead point (Figure 1).

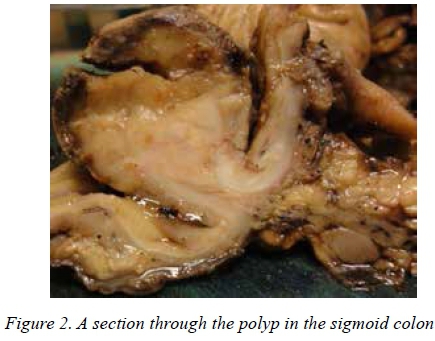
At colonoscopy, the leading part of the intussusception was visualised and confirmed to be a polyp. The intussusception could not be reduced, nor the polyp excised. Also, the colonoscope could not be advanced beyond this site. A laparotomy was undertaken, at which a sigmoid colocolic intussusception was found, with a large, 4cm polyp as a leading point (Figure 2).
A sigmoid colectomy was performed with a primary anastomosis and the patient experienced an uneventful recovery. The histology revealed the polyp to be a plasmacytoma. Immunoperoxidase staining was positive for kappa, and negative for lambda, light chains. The tumour was transmural and the lymph nodes were free from metastasis. On screening for multiple myeloma, the following observations were made:
• A slight polyclonal increase in immunoglobulin on serum protein electrophoresis, consistent with HIV infection.
• The absence of Bence-Jones protein on the urine protein electrophoresis.
• A normocellular microscopical appearance, with no plasma cell dyscrasia, was displayed on the bone marrow aspirate.
• The metastatic skeletal survey was normal.
The patient was last seen three months after the operation, at which time he had completely recovered from the surgery. He is now on a surveillance programme, in conjunction with consultations with a haematologist, for the recurrence or progression of the plasmacytoma.
Discussion
SEP is a rare condition. Only ± 25 cases have been reported in the literature to date. The upper aerodigestive tract is the most frequent location of the lesions, although it can occur in virtually any organ in the body.3 Localised or loco-regional disease is evident in most reported cases of SEP. Metastatic disease is extremely rare.3
Primary plasmacytoma of the gastrointestinal tract is even rarer, occurring in approximately 10% of cases.2 All the segments of the gastrointestinal tract may be involved. The small intestine is the most common, followed by the stomach, colon and oesophagus.2 The sigmoid colon, caecum, rectum and ascending colon are the most commonly involved colonic segments.3 Definite cause or risk factors have not been identified.2 An association was reported between SEP and various pathological conditions of the colon, namely diverticular disease, ulcerative colitis, carcinoid tumour, solid organ transplant and previous gastrointestinal plasmacytoma, but a causal relationship could not be established.1 These conditions are likely to be incidental findings, as their incidence is high in the respective populations.
An increased incidence of plasma cell tumours has been shown in HIV-positive patients, and tend to occur at unusual sites, such as the skin, soft tissues, breasts, testes and oral cavity.4 They tend to present at a young age in HIV-infected patients, and have a tendency to rapidly progress to involve multiple sites.4 It is tempting to postulate that HIV infection may be a risk factor for plasmacytoma and other plasma cell tumours. This may be explained by the stimulatory effect of HIV on the plasma cells and co-infection with oncogenic viruses, such as the Epstein Bar and human papillomaviruses.4
Clinical presentation is variable, and shows a marked male predominance. The age at presentation ranges from 15-90 years.1,3,5 The symptoms are non-specific, and include constitutional symptoms, such as anorexia and weight loss.4 Symptoms specific to the gastrointestinal tract include abdominal mass, abdominal pain and/or dyspepsia, vomiting, gastrointestinal bleeding; and complications, such as intestinal obstruction and perforation, leading to peritonitis.2-4 Specific oesophageal symptoms include dysphagia, and if the colorectum is involved, the symptoms are variable, but consistent with any colorectal or anal tumours, including a change in bowel habit.2,3
On endoscopy, gastrointestinal plasmacytoma may present as a nodular or ulcerated mass, or as a diffusely thickened mucosal fold.2 The diagnostic criteria for extramedullary plasmacytoma are an extramedullary tumour with clonal plasma cells, the absence or low levels of serum or urinary monoclonal immunoglobulin (M protein), histologically normal bone marrow and trephine, and a normal skeletal survey.3 There is an absence of related organ or tissue impairment due to plasma cell dyscrasias, such as renal failure or anaemia, and normal calcium levels.3 Satisfying these diagnostic criteria is important in order to differentiate this condition from multiple myeloma, as the treatment is different. Symptoms are not diagnostic in patients with colorectal SEP, and are similar to those for any colorectal tumour.
The best management approach to patients with SEP should be determined in a multidisciplinary setting, in order to achieve the best outcome. Surgery, or combined radiotherapy and surgery, are the optimal therapeutic options for the upper aerodigestive tract.3 Resection is the optimal management for colonic plasmacytoma.3 Treatment for rectal lesions is even more variable, including radiotherapy, endoscopic excision and rectal resection.3 Radiotherapy is an appealing option as it avoids a permanent stoma, and local control rates of 80-100% have been reported for radiotherapy to head and neck lesions.3 Treatment consists of tumoricidal radiation (40-50 Gy) and is often curative.3 If radiotherapy fails, then resection, in the form of anterior resection or abdominoperineal resection, is the next option. This management approach should be consistent with current trends in colorectal cancer treatment.3 Patients with rectal SEP, who have undergone upfront surgical resection, should only have adjuvant radiotherapy when the resection margins are positive.2 The lack of patient follow-up in the reported cases makes it impossible for us to comment on the efficacy of the different therapies.
Evidence for use of chemotherapy in plasmacytoma is lacking.5 Adjuvant chemotherapy should be considered for high-risk tumours, namely tumours > 5cm in size, high-grade histology, refractory and/or relapsed disease.2 Patients should be followed-up closely as there is a risk of local recurrence and progression to multiple myeloma.2,3 It is reasonable to suggest an approach similar to that for anal carcinoma in the absence of case reports in anal SEP.6
Conclusion
SEP is rare, and commonly affects the caecum and sigmoid colon. Rectal SEP is even rarer. Treatment should be individualised. Segmental colectomy is appropriate for colonic plasmacytoma. Surgical excision is ideal for rectal plasmacytoma, with radiotherapy as a salvage option.
REFERENCES
1. Dores GM, Landgren O, McGlynn KA, et al. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myelom: incidence and survival in the United States, 1992-2004. Br J Haematol. 2009;144(1):86-94. [ Links ]
2. Salogub G, Lokhmatova E, Sozin S. Solitary bone and extramedullary plasmacytoma. Intech Open Science [homepage on the Internet]. [ Links ] 2012. c2013. Available from: http://www.intechopen.com/books/multiple-myeloma-an-overview/plasmocytoma
3. International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haemat. 2003;121(5):749-757. [ Links ]
4. Gupta A, Kumbhalkar D, Parate S, et al. HIV seropositivity and neoplasms with plasma cell morphology: plasmablastic lymphoma and plasma cell myeloma: is it a chance Association or an increasing occurrence? Ann Pathol Lab Med. 2015;2(2):C111-C117. [ Links ]
5. Hughes M, Soutar R, Lucraft H, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone, extramedullary plasmacytoma and multiple solitary plasmacytoma: 2009 update. BloodMed.com [homepage on the Internet]. [ Links ] c2013. Available from: http://www.bloodmed.com/contentimage/guidelines/3454.pdf
6. Ntombela XH, Govender P, Sartorius B, Madiba TE. The clinicopathologic spectrum of anal cancer in KwaZulu-Natal Province, South Africa: analysis of a provincial database. Cancer Epidemiol. 2015;39(4):528-533. [ Links ]
 Correspondence:
Correspondence:
Monde Mjoli
mmjoli@yahoo.com














