Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.2 Cape Town Jun. 2016
PEDIATRIC SURGERY
Role of focused assessment with sonography for trauma as a screening tool for blunt abdominal trauma in young children after high energy trauma
W TummersI; J van SchuppenII; H LangeveldIII; J WildeIV; E BanderkerV; A van AsI
IDepartment of Trauma and Paediatric Surgery, Red Cross War Memorial Children's Hospital, University of Cape Town, South Africa
IIDepartment of Radiology, Academic Medical Centre, Amsterdam, The Netherlands
IIIDepartment of Paediatric Surgery, Sophia's Children Hospital/Erasmus Medical Centre, Rotterdam, The Netherlands
IVDepartment of Paediatric Surgery, Emma's Children Hospital/Academic Medical Centre, Amsterdam, The Netherlands
VDepartment of Radiology, Red Cross War Memorial Children's Hospital, University of Cape Town South Africa
ABSTRACT
BACKGROUND: The objective of the study was to review the utility of focused assessement with sonography for trauma (FAST) as a screening tool for blunt abdominal trauma (BAT) in children involved in high energy trauma (HET), and to determine whether a FAST could replace computed tomography (CT) in clinical decision-making regarding paediatric BAT.
METHOD: Children presented at the Trauma Unit of the Red Cross War Memorial Children's Hospital, Cape Town, after HET, and underwent both a physical examination and a FAST. The presence of free fluid in the abdomen and pelvis was assessed using a FAST. Sensitivity, specificity, and positive and negative predictive values (PPV and NPV) for identifying intraabdominal injury were calculated for the physical examination and the FAST, both individually and when combined.
RESULTS: Seventy-five patients were included as per the criteria for HET as follows: pedestrian motor vehicle crashes (MVCs) (n = 46), assault (n = 14), fall from a height (n = 9), MVC passenger (n = 4) and other (n = 2). The ages of the patients ranged from 3 months to 13 years. The sensitivity of the physical examination was 0.80, specificity 0.83, PPV 0.42 and NPV 0.96. The sensitivity of the FAST was 0.50, specificity 1.00, PPV 1.00 and NPV 0.93. Sensitivity increased to 0.90 when the physical examination was combined with the FAST. Nonoperative management was used in 73 patients. Two underwent an operation.
CONCLUSION: A FAST should be performed in combination with a physical examination on every paediatric patient involved in HET to detect BAT. When both are negative, nonoperative management can be implemented without fear of missing a clinically significant injury. FAST is a safe, effective and easily accessible alternative to CT, which avoids ionising radiation and aids in clinical decision-making.
Blunt abdominal trauma (BAT) is a frequent reason for emergency department admissions of children and a significant cause of death in children aged > 1 year.1 BAT accounts for 90% of childhood abdominal injuries, with falls and motor vehicle crashes (MVC) representing the most common mechanisms of injury. Injury to the abdominal organs occurs in 8% of children, can be life threatening, and a careful systematic approach is required to identify it.2 The general makeup of children's body composition places them at an increased risk of sustaining intra-abdominal injuries (IAIs) after high energy trauma (HET). The intra-abdominal organs are proportionally large, are in close proximity to one another, and the smaller size results in a greater degree of force per body surface area.
Computed tomography (CT) scanning is the gold standard for identifying BAT. However, it is associated with a number of well-known limitations, such as cost, availability and radiation exposure, especially in children. The utility of a focused assessment with sonography for trauma (FAST) in identifying free intra-abdominal fluid and guide management is well established in adults, but is less well publicised in paediatric trauma. A FAST is quick, and involves a limited examination of the abdomen at four specific locations: the right upper quandrant, left upper quadrant, suprapubic area and epigastric region of the abdominal cavity. A positive FAST in adults generally indicates a need for further imaging or immediate surgical intervention. However, in the paediatric population, nonoperative management is the standard of care for haemodynamically stable children with BAT. Thus, the outcome of the FAST does not necessarily change management.3 Furthermore, free fluid does not always develop in paediatric patients after they have sustained an abdominal solid organ injury, and these patients are at risk of unidentified injury when only a FAST is used.4 Menaker et al. recently conducted a large observational study in which a decrease in the use of abdominal CT scanning was demonstrated when FAST was performed. However, the safety of this shift in paediatric trauma care has not been reported in the recent scientific literature.5,6
Objectives
The main objectives of this study were to determine the role of a FAST as a screening tool in order to detect BAT in children who sustained HET, and whether or not it could replace CT scanning as a modality, given the limitations of the latter.
A secondary objective was to establish whether or not the combination of a FAST and a physical examination was adequate in detecting IAI.
Method
Study population
Haemodynamically stable patients aged < 13 years who presented at the trauma unit of the Red Cross War Memorial Children's Hospital, Cape Town, after HET, between 1 October 2012 and 31 January 2013, were included in the study. A level I paediatric trauma centre for children up to the age of 13 years is operational at the Red Cross War Memorial Children's Hospital.
Speed and mass determine the degree of energy transfer in a trauma victim, and hence were critical determinants in establishing whether or not a mechanism counted as HET. The following inclusion criteria were used: car crash > 35km/hour (without a seat belt), car crash > 45km/hour (with a seat belt), vehicle displacement of > 7m, child ejected from the car, fall from a height of > 3m and any pedestrian-vehicle crash.
"Haemodynamically unstable" was defined as the lack of adequate tissue perfusion, resulting in the need for the transfusion of > 20ml/kg of fluid (the standard quantity recommended for a child).7
The patients underwent a physical examination and a FAST on admission to identify BAT. A decision to provide additional CT scanning was made at the discretion of the surgical resident on call. Children involved in HET were admitted to the trauma ward for at least 24 hours of observation.
The results of the trauma mechanism, the physical examination findings and the FAST were collected and recorded prospectively on a standard data collection form specifically designed for this study.
Physical examination
The physical examination was performed by a surgical registrar on admission. Suspicion of abdominal injury was defined as abdominal tenderness, guarding, distension, lacerations or haematoma of the abdominal wall. Clinical suspicion of a pelvic fracture was defined as regional osseous tenderness or pelvic instability. Standard additional laboratory testing is not performed after trauma at the Red Cross War Memorial Children's Hospital.
Radiology method
A Lodox Statscan® (Lodox Systems, Johannesburg, South Africa) is part of the polytrauma imaging protocol at the Red Cross War Memorial Children's Hospital.8,9 It facilitates an efficient means of triage in polytrauma patients, and allows the identification of clinically unsuspected or occult bony injury.
Ultrasound method
A FAST was performed using Ultrasonix SonixOne® (BK Ultrasound, Peabody, USA) by a general surgeon or a medical student who had received specific training for this purpose. The training included a short theoretical introduction on the principles of ultrasound physics and the role of a FAST in trauma, followed by several practical sessions, led by an experienced trauma surgical consultant and radiology consultant. The practical sessions were performed on other trainees and children in the trauma ward. The trainee performed at least 20 supervised examinations using a 3-5MHz sector or curved transducer in each of the four FAST regions (i.e. the right upper quandrant, left upper quadrant, suprapubic area and epigastic region). The study focused on the detection of free intraperitoneal fluid only. An attempt was not made to identify the organ of injury.
The general surgeon or medical student interpreted the images in real time and recorded still images for the purposes of documentation. An abnormally FAST scan was defined as one that identified signs of free fluid. If signs of free fluid were present, the patient proceeded to CT scanning.
Computed tomography method
The CT scan volume included the lower chest (lung bases), entire abdomen and pelvis. The CT was performed on the 64-slice CT scanner (Philips, Eindhoven, The Netherlands) using Ultravist 300®, a non-ionic intravenous contrast (Bayer, Sunnyvale, USA) at a standard dose of 2 ml/kg, administered in bolus fashion. The slices had an increment of 0.75mm, and were reconstructed to a thickness of 1.5mm. The rendered volume was determined and three-dimensional and multiplanar reconstructions performed, as required. The CT scans were interpreted by a radiology registrar, as well as a certified paediatric radiologist proficient in paediatric trauma, and were evaluated for the absence or presence of free fluid, its location and the presence of any visceral injury.
Outcome measures
The primary outcome was the presence of one or more traumatic intra-abdominal or pelvic injuries at follow-up or at CT imaging.
An assessment was also made as to whether these injuries were expected after the physical examination or routine use of the FAST, and whether or not these findings where clinically significant.
A clinically significant injury was defined as one that resulted in an intervention other than nonoperative management, such as operative management, additional imaging or a blood transfusion.
Statistical analysis
Statistical analysis was performed using SPSS® version 18.0 for Windows®. The test characteristics were determined at the outset to evaluate the ability of the physical examination and the FAST to identify IAI, separately and in combination. Thereafter, Cohen's kappa coefficient was used to determine the agreement between the physical examination and FAST in the assessment of possible IAI.
Ethical approval
This study was approved by the Human Ethics Research Committee of the University of Cape Town (HREC/Ref: 488/2012).
Results
During the period under review, from 1 October 2012 to 31 January 2013, 75 patients were included in the study. There were 48 boys and 27 girls, ranging in age from three months to 13 years (with a mean of 5 years and 5 months). The mechanisms of injury were: MVC pedestrian (n = 46), assault (n = 14), a fall from a height (n = 9), being a MVC passenger (n = 4), a table fell on the child (n = 1) and a television fell on the child (n = 1).
To determine the added value of FAST after the physical examination, the outcomes of both examinations were analysed with respect to suspicion of BAT. During the initial survey, after the physical examination, 56 patients were not suspected of having BAT, and 19 were. Of the 19 patients in whom BAT was suspected after the physical examination, a normal FAST scan was reported for 15 (Table 1).
Four of these patients demonstrated BAT at follow-up, despite the initial normal scan. Four of the FAST scans were abnormal, and BAT was confirmed in these patients at CT scanning. One patient,who had not been suspected of having BAT after the physical examination and the FAST, presented with macroscopic haematuria on admission, but appeared to have a kidney contusion at CT. An abnormal FAST result was reported in another patient without suspicion of BAT after the physical examination, and who appeared to have splenic injury at CT (Table 2).
Clinical suspicion of BAT after the initial survey was not detected in the remainder of the patients (n = 54), who did not reveal any signs of abdominal injury on follow-up.
The abdominal FAST results were compared with the CT findings for the eight patients who received a CT scan, and with the clinical course and outcomes of the remaining 67 patients, because the costs and the risks of radiation prohibited the performance of routine CT.
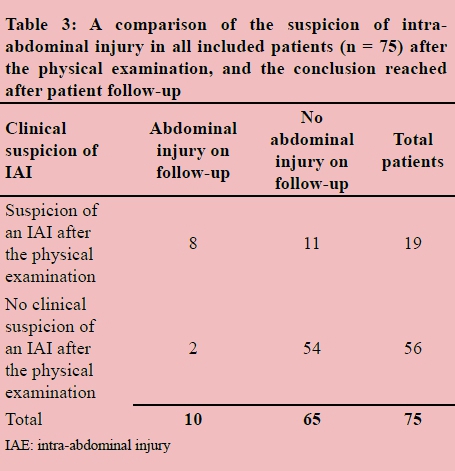
The physical examination yielded the following test characteristics for the identification of BAT (Table 3): sensitivity 0.80 [95% confidence interval CI: 0.49-0.94], specificity 0.83 [95% CI: 0.76-0.87], positive predictive value (PPV) 0.42 [95% CI: 0.20-0.64] and negative predictive value (NPV) 0.96 [95% CI: 0.88- 0.99].
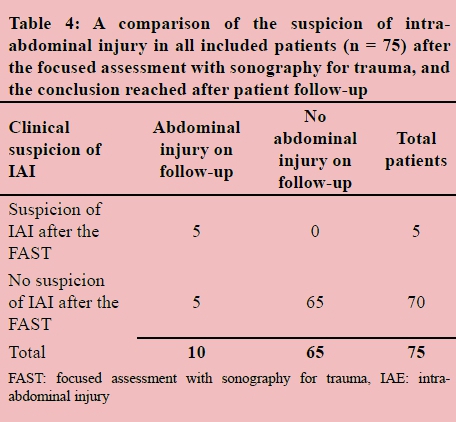
The following test characteristics were used to identify BAT with the FAST (Table 4): sensitivity 0.50 [95% CI: 0.24-0.76], specificity 1.00 [95% CI: 0.94-1.00], PPV 1.00 [95% CI: 0.57-1.00] and NPV 0.93 [95% CI: 0.84- 0.97].
Sensitivity of 0.90, specificity of 0.83, a PPV of 1.00 and a NPV of 0.45, obtained from either a positive physical examination or an abnormal FAST, were used to identify BAT. Sensitivity of 0.90, instead of 0.80, indicates the added value of the FAST, when combined with the physical examination.
According to Landis and Koch,10 and Fleiss,11 there is agreement in the range of poor to fair between the physical examination and FAST in the assessment of possible BAT with a Cohen's kappa coefficient of 0.25.
The chance of having BAT in our study was 100% when the physical examination and the FAST were both positive. The chance of having BAT was 2% when both the physical examination and FAST were negative (1 in 55 patients) in this study. This patient had a kidney contusion without free fluid.
There were no false positive outcomes when both the diagnostic tools demonstrated the same result.
Regarding the management of BAT in this research, 73 patients were treated with nonoperative management, while two patients underwent surgery, one of whom underwent surgery for an incidentally found Wilms' tumour, and not because of trauma-related injuries. Both an abnormal physical examination and a deviant FAST scan were reported for this patient. The other patient underwent an operation because of the suspicion of intra-peritoneal free air on Lodox Statscan®; found to be preperitoneal air at surgery. A deviant physical examination and a normal FAST were reported for this patient.
The protocol regarding reasons for admission beyond 24 hours was found to be ambiguous between the different doctors, and was therefore excluded from our results.
Discussion
The evaluation and management of IAI has always been subject to controversy. Since the introduction of diagnostic peritoneal lavage by Root et al. in 1965,12 the value of the physical examination in BAT has often been criticised.13,14 Nevertheless, the general opinion is that the presence of a history of significant trauma, together with a positive physical examination, are markers of possible underlying injury, requiring further investigation.15 Evidence-based guidelines, the need for cost-effective safe practice and the avoidance of unnecessary radiation exposure are important considerations in paediatric trauma care.
It was demonstrated in our study that the FAST, when used in combination with a physical examination in children with suspected BAT following HET, carried a high sensitivity for clinically significant injury, and was a potentially powerful and safe tool in paediatric trauma resuscitation.
The readily available FAST may save time by quickly directing managing clinicians to possible problem areas and obviating the need for more costly and time-consuming CT imaging with its associated radiation burden, particularly in haemodynamically stable patients.16 Having taken our findings into account, we suggest that the combination of the physical examination and the FAST was the preferred method of diagnosis for patients in the emergency department with suspicion of BAT. The role of the FAST in determining the need for ancillary imaging studies in stable paediatric trauma patients should be evaluated in further studies.
Thus, we conclude that both a negative FAST and physical examination are good indicators of the absence of clinically significant BAT. When both were negative, it was shown in the clinical follow-up that the chance of having BAT was only 2% (1:55). Nonoperative management has become the standard of care in paediatric trauma management because of its association with decreased morbidity and mortality.4 The combination of the FAST and the physical examination in our cohort of patients was found to be a good predictor of nonoperative management. Additional information was not gleaned from subsequent CT scanning that would have changed the patient management.
It could be argued that FAST has a low sensitivity in the detection of injury to solid organs requiring an operation, and therefore it is suggested that FAST is not an appropriate diagnostic tool since only one of the two patients who required surgery where identified using this tool. However, surgery in that one patient proved to be unnecessary because preperitoneal air had been misdiagnosed as intraperitoneal air. Our findings indicated that in this study, the need for an operation was correctly predicted in all patients with the use of the FAST, combined with the physical examination.
The benefits and limitations of the physical examination and ultrasound following BAT are cited in several recent articles in the paediatric trauma literature.1,3,17-26
In order to place our findings in proper perspective, it should be noted that techniques and methods vary among studies. HET diagnostic management may consist of a brief search for free fluid (the FAST) or a more complete abdominal ultrasound. The studies also differ with regard to what constitutes a positive finding for BAT.
Our results are comparable with those of Akgur et al.,17 who concluded in their prospective study in which ultrasound was used as the initial diagnostic modality, that ultrasound alone was sufficient in evaluating most children with BAT.
Schurink et al.18 concluded that a physical examination of the abdomen was beneficial in cases with an isolated abdominal injury, or lower rib cage fractures with a high negative predictive value (NPV), for normal findings.
Griedhop et al.19 identified that an abnormal physical examination was a significant risk factor for BAT. They concluded that the value of a negative physical examination without other risk factors was 100%.
Natarajan B et al.20 found a sensitivity of 43%, specificity of 99%, and PPV and NPV of 95% and 94% for identifying IAI with the FAST. Furthermore, the sensitivity of the FAST varies between 63% and 96% in the literature.21-24
Karam et al.1 suggest that only the absence of abdominal pain (NPV of 95%) as well as the absence of peritoneal irritation (NPV of 84%), are useful in assessing children with BAT.
Several other studies have shown that a physical examination is not reliable enough to rule out significant BAT 3,18,25,26
Study limitations
There were several study limitations, including the lack of prior experience with FAST scanning at the Red Cross War Memorial Children's Hospital. In addition, the doctors were not familiar with the image interpretation. This limitation is currently addressed by dedicated FAST training for all doctors working in the trauma unit at the Red Cross War Memorial Children's Hospital.
The follow-up rate for potentially missed injuries was low, albeit unlikely, given that there were no undetected clinically significant injuries.
The physical examination and the interpretation of FAST scans is operator dependent.
None of our study patients presented with serious lacerations, precluding an assessment of the FAST for this type of injury.
FAST performed in the acute phase of presentation only is less useful in slow bleeding injuries, such as mesenteric bleeds or bowel perforations, where fluid accumulates over time. Follow-up FAST, prior to discharge, should be considered in all patients.
The physical examination is often unreliable in cases of patients with polytrauma.
In spite of the aforenamed limitations, our results were in accordance with those reported in other studies,27,28 namely that the FAST can be reliably performed by non-radiologists after a fairly short and effortless period of training, with excellent results. The major advantage of the FAST is immediately shown by this. It has also been indicated in several other studies that the ability to detect free fluid using the FAST technique is equally accurate in the hands of non-radiologists and radiologists.15,29,30
Conclusion
Our research evaluated the utility of FAST as a screening tool for BAT in children involved in HET. We determined the added value of the FAST after the physical examination, to indicate or contradict the presence of BAT and its role in the direction of management. Based on our findings, we conclude that the FAST is excellent as a screening modality in children with BAT, but should be utilised in combination with the physical examination. When the physical examination and the FAST were both negative, nonoperative management could be initiated without fear of a clinically significant injury having been missed. We also demonstrated that the FAST could safely replace CT scanning in the clinical decision-making process as no significant information was added by the CT, which constitutes an unnecessary radiation burden. Finally, one of the most important advantages of the FAST is that it can be accurately performed by relatively inexperienced doctors who have received short, goal-directed training. However, the limitations of the FAST should also be recognised, and its outcomes considered, in combination with all clinical data. The FAST should be performed in combination with a physical examination on every paediatric patient, under the age of 13, who has been involved in HET and who has suspected BAT.
REFERENCES
1. Karam O. National survey on abdominal trauma practices of pediatric surgeons. Eur J Pediatric Surg. 2010;20(5):334-338. [ Links ]
2. Gaines BA, Ford HR. Abdominal and pelvic trauma in children. Crit Care Med. 2002;30(11 Suppl):S416-S423. [ Links ]
3. Coley BD, Mutabagani KH, Matin LC. Focused abdominal sonography for trauma (FAST) in children with blunt abdominal trauma. J Trauma. 2000;48(5):902-906. [ Links ]
4. Chiu WC, Cushing BM, Rodriguez A, et al. Abdominal injuries without hemoperitoneum: a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma. 1997;42(4):617-625. [ Links ]
5. Van Schuppen J, Olthof DC, Wilde J, et al. Diagnostic accuracy of a step-up imaging strategy in pediatric patients with blunt abdominal trauma. Eur J Radiol. 2014;83(1):206-211. [ Links ]
6. Menaker J, Blumberg S, Wisner DH, et al. Use of the focused assessment with sonography for trauma (FAST) examination and its impact on abdominal computed tomography use in 7. hemodynamically stable children with blunt torso trauma. J Trauma Acute Care Surg. 2014;77(3):427-432. [ Links ]
8. Kramer WLM, Ten Duis HJ, Ekkelkamp S, et al., editors. Handboek kindertraumatologie. Utrecht: De Tijdstroom, 2007. [ Links ]
9. Pitcher PD, van As Ab, Saunders V, et al. A pilot study evaluating the "STATSCAN" digital x-ray machine in paediatric polytrauma. Emerg Radiol. 2008;15(1):35-42. [ Links ]
10. Pitcher PD, Wilde JCH, Douglas TS, van As Ab. The use of the Statscan digital x-ray unit in paediatric polytrauma. Pediatr Radiol. 2009;39(5):433-437. [ Links ]
11. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. [ Links ]
12. Fleiss J L. (1971) Measuring nominal scale agreement among many raters. Psychological Bulletin. 1971;76(5):378-382. [ Links ]
13. Root HD, Hauser CW, McKinley CR, et al. Diagnostic peritoneal lavage. Surgery. 1965;57:633-637. [ Links ]
14. Bivins BA, Sachatello CR, Daugherty ME, et al. Diagnostic peritoneal lavage is superior to clinical evaluation in blunt abdominal trauma. Am J Surg. 1978;44(10):637-641. [ Links ]
15. Rodriguez A, DuPriest RW, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims: a prospective study comparing physical examination with peritoneal lavage. Am J Surg. 1982;48(9):457-459. [ Links ]
16. Williams RD, Zollinger RM. Diagnostic and prognostic factors in abdominal trauma. Am J Surg. 1959;97(5):575-578. [ Links ]
17. Thourani VH, Pettitt BJ, Schmidt JA, et al. Validation of surgeon-performed emergency abdominal ultrasonography in paediatric trauma patients. J Pediatr Surg. 1998;33(2):322-328. [ Links ]
18. Akgur FM, Aktug T, Olguner M, et al. Prospective study investigating routine usage of ultrasonography as the initial diagnostic modality for the evaluation of children sustaining blunt abdominal trauma. J Trauma. 1997;42(4):626-628. [ Links ]
19. Schurink GW, Bode PJ. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury. 1997;28(4):261-265. [ Links ]
20. Grieshop NA, Jacobsen LE, Gomez GA, et al. Selective use of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma. 1995;38(5):727-731. [ Links ]
21. Natarajan B, Gupta PK, Cemaj S. FAST scan: is it worth doing in a hemodynamically stable patient? Surgery. 2010;148(4):695-700; discussion 700-701. [ Links ]
22. Poletti PA, Wintermark M, Schnyder P, Becker CD. Traumatic injuries: the role of imaging in the management of the polytrauma victum (conservative expectation). Eur Radiol. 2002;12(5):969-978. [ Links ]
23. Forster R, Pillasch J, Zielke A, et al. Ultrasonography in blunt abdominal trauma: influence of the investigators' experience. J Trauma. 1993;34(2):264-269. [ Links ]
24. McGahan JP, Richards JR. Blunt abdominal trauma: the role of emergent sonography and a review of the literature. AJR Am J Roentgenol. 1999;172(4):897-903. [ Links ]
25. Sirlin CB, Brown MA, Andrade-Barreto OA, et al. Blunt abdominal trauma: clinical value of negative screening US scans. Radiology. 2004;230(3):661-668. [ Links ]
26. Livingston DH, Lavery RF, Passannante MR, et al. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: results of a prospective, multi-institutional trial. J Trauma. 1998;44(2):273-280. [ Links ]
27. Poletti PA, Mirvis SE, Shanmuganathan K, et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma. 2004;57(5):1072-1081. [ Links ]
28. Hsu JM, Josephy AP, Tarlinton LJ, et al. The accuracy of focused assessment with sonography in trauma (FAST) in blunt trauma patients: experience of an Australian major trauma service. Injury. 2007;38(1):71-75. [ Links ]
29. Brooks A, Davies B, Smethhurst M, Connolly J. Prospective evaluation of non-radiologist performed emergency abdominal ultrasound for haemoperitoneum. Emerg Med J. 2004;21(5):e5. [ Links ]
30. Buzzas GR, Kern SJ, Smith RS, et al. A comparison of sonographic examinations for trauma performed by surgeons and radiologists. J Trauma. 1998;44(4):604-606. [ Links ]
31. Kern SJ, Smith RS, Fry WR, et al. Sonographic examination of abdominal trauma by a senior surgical resident. Am Surg.1997;63(8):669-674. [ Links ]
 Correspondence:
Correspondence:
Willemieke Tummers
w.s.f.j.tummers@lumc.nl














