Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.54 no.2 Cape Town Jun. 2016
VASCULAR SURGERY
Outcomes for cervicomediastinal vascular trauma managed by a vascular subspecialist-led vascular trauma service
J IslamI, IV; G L LaingII, IV; J L BruceII, IV; G V OosthuizenII, IV; D L ClarkeII, IV; J V RobbsIII, IV
IPietermaritzburg Metropolitan Vascular Surgery, Pietermaritzburg, South Africa
IIPietermaritzburg Metropolitan Trauma Surgery, Pietermartizburg, South Africa
IIIPrivate Practice, Entabeni Hospital, Durban, South Africa
IVNelson R Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
ABSTRACT
BACKGROUND: The management of cervicomediastinal vascular trauma is challenging. We report on our experience with the condition in a newly established vascular trauma service unit, and compare the outcomes to those reported in our parent vascular surgery department.
METHOD: The details of patients with cervicomediastinal vascular injuries from January 2012 to June 2014 were retrieved for analysis from a prospective database.
RESULTS: Ninety-three patients were identified, 84 of whom were male (90%), with an average age of 29 years. Most were penetrating injuries (89%), and 87% of these were due to stab wounds. There were 107 vascular injuries, 88 cervical and 19 mediastinal. Of these, 87 were arterial and 20 venous injuries. The most common arterial injury involved the subclavian artery (24%), followed by the common carotid artery (22%). Management was multimodal, and included conservative (8%), stenting and embolisation (8%), referral to a higher centre (8%), vascular repair (64%) and ligation (12%). Nineteen per cent required median sternotomy or thoracotomy. Eight patients died postoperatively (9%). Seven of them presented in extremis and died within 24 hours, and one died after a week from associated abdominal injuries. Postoperative complications were 9%. There was no incidence of a stroke or limb loss despite ligation of the arteries, including ligation of four internal carotids.
CONCLUSION: The development of endovascular techniques would allow for noninvasive management of a significant number of patients. Open surgery is still necessary, and associated with significant morbidity. Comparable results were reported in our newly established vascular trauma service unit to those obtained in our parent vascular surgery department in Durban.
Cervicomediastinal vascular injuries may be caused by blunt or penetrating trauma, and collectively constitute 5-10% of all reported cases of vascular trauma.1,2 The operative management of cervicomediastinal vascular trauma is challenging as surgical access is difficult, and loss of control can result in rapid exsanguination. High morbidity and the mortality rates, ranging from 14-25%, have been cited in both South African and international reports.3-7 Blunt thoracic aortic injury is immediately fatal in 80-90% of cases, and if untreated, survivors have a dismal prognosis. Thirty per cent die within six hours, 40-50% within 24 hours and 90% within four months, while overall operative mortality is approximately 28%, with a systemic complication rate of 50%.8,9 Penetrating thoracic aortic trauma is highly lethal, and the mortality rate can be as high as 80%.10
New techniques have been introduced over the last two decades with the rapid development of endovascular surgery, and offer potential solutions to complex injuries while avoiding the risk of open surgery.11 This makes decisionmaking more nuanced and complex.
Our parent vascular surgery department in Durban pioneered the concept of a dedicated metropolitan vascular trauma service over three decades ago in response to the complex nature of these injuries and their relative rarity.12,13 The spectrum and outcomes of cervicomediastinal vascular trauma in our newly established vascular trauma team are reviewed in this report, and a comparison made with those in Durban, while attempting to contextualise the new and emerging endovascular and imaging techniques with a more established approach.
Setting
The Pietermaritzburg Metropolitan Hospitals Complex consists of three hospitals. The Pietermaritzburg Metropolitan Trauma Service was initiated in 2006, and the aim is the delivery of trauma care across hospitals in Pietermaritzburg. The vascular surgery unit was initiated in January 2013, with a single full-time certified vascular surgeon. Vascular trauma management had been left up to individual surgeons prior to the development of these two services. Currently, vascular trauma cases are exclusively co-managed by the trauma and vascular surgery units. The unit functions in a closed fashion, and there is a separate vascular trauma roster to ensure that vascular trauma cases are exclusively managed by a dedicated core of vascular trauma surgeons.
Method
The details of patients with cervicomediastinal vascular injuries from January 2012 to June 2014 were retrieved for analysis from a prospectively maintained database. Cervicomediastinal vascular injuries are defined as arterial or venous injuries of the neck [carotids, subclavian (including its branches) and the proximal axillary artery], and mediastinum [ascending aorta, aortic arch (including its branches), descending aorta, the pulmonary artery and veins]. Injuries to the first part of the axillary artery were included because surgical exposure is often similar to that for the third part of the subclavian artery, and it can be difficult to distinguish between them anatomically. A supraclavicular and/or infraclavicular incision is used for subclavian and axillary artery injuries. An attempt is not made to divide the clavicle as clavicular division is associated with significant postoperative morbidity. If required, the incision can be extended up into the neck along the anterior border of the sternocleidomastoid muscle, or downwards into the chest in the form of a median sternotomy. We do not make use of lateral thoracotomy for exposure of the neck vessels.
This paper was written in full compliance with ethical standards. Pietermaritzburg Metropolitan Trauma Service personnel maintain a prospective digital trauma registry. The data from this registry were interrogated retrospectively. Ethics approval to maintain this registry was obtained from the Biomedical Research Ethics Committee (Ethics Number BE207/09 and BCA221/13) of the University of KwaZulu-Natal, Durban, South Africa; and from the Research Unit of the Department of Health (HRKM 265/13), KwaZulu-Natal, South Africa.
Results
Ninety-three patients with cervicomediastinal vascular injuries were identified over the 30-month period, 84 of whom were male (90%), with an average age of 29 years (a range of 16-54 years). The overall Injury Severity Score at presentation was 17 (a range of 4-75). The mechanisms of injury were mostly penetrating wounds (83); among them stab (72) and gunshot wounds (11), and the rest were blunt trauma (7) and iatrogenic injuries (3). Seventy-four of the patients presented within 24 hours of the injury (80%), 16 within 72 hours (17%), two after one month (2%), while one patient presented five years after the initial injury (1%).
Investigations
Preoperative computed tomography (CT) angiography was performed for 65 patients (70%).
Injuries
There were 107 vascular injuries in 93 patients. Fourteen patients had received combined arterial and venous injuries, and six isolated venous injuries. There were 74 cervical (80%) and 19 mediastinal injuries (20%). The anatomical distribution of arterial injury is shown in Table 1. Most of the patients who had experienced blunt trauma were involved in a motor vehicle collision (5) and sustained descending aortic injuries and blunt carotid injuries (2). Three patients presented with iatrogenic injuries, i.e. common carotid artery injury (1) from the insertion of a central venous line; subclavian artery injury (1), also from the insertion of a central venous line and a subclavian artery injury (1) from internal fixation of the fractured clavicle. The injuries according to body region were 88 cervical (71 arterial and 17 venous), and 19 mediastinal (16 arterial and 3 venous) vascular injuries. The anatomical distribution of venous injuries is listed in Table 2. The most common arterial injury was to the subclavian artery (24%), followed by the common carotid artery (22%). Of the venous injuries, internal jugular and axillary vein injuries comprised the highest number (6%), followed by subclavian vein injuries (5%). The most common associated injury was haemothorax or pneumothorax in 32 patients (34%), followed by brachial plexus injury in 15 (16%). The other associated injuries were cardiac injury (4), head injury (4), maxilla/mandible fracture (4), rib fracture (3), oesophageal injury (2), tracheal injury (2) and clavicle fracture (2).


Management
Fifty-six (64%) of the arterial injuries were managed by operative repair. Median sternotomy or thoracotomy was required in 18 patients (19%); 12 for mediastinal vascular injuries and six for cervical vascular injuries. Arterial exploration was undertaken in 66 patients (76%); 56 were repaired (64%) and 10 were ligated (12%). The most common arterial repairs were to the common carotid (18%) and subclavian (18%) artery, followed by the axillary artery (15%). The other arterial repairs were internal carotid (2), ascending and arch of aorta (3), descending aorta (2), innominate artery (3) and pulmonary artery (1). Primary repair was performed for all carotid and aortic injuries. Fourteen subclavian and axillary arteries underwent primary repair (48%), and 15 were repaired with interposition vein grafts (52%). Arterial ligation was performed in external carotid (3), internal carotid (4), vertebral (2) and internal mammary arteries (1). A subclavian artery injury was repaired as part of a hybrid procedure (combined endovascular and open), in which median sternotomy was avoided. Proximal subclavian artery control was obtained by an endovascularly placed temporary balloon occlusion. The artery was then approached via a supraclavicular incision and repaired.
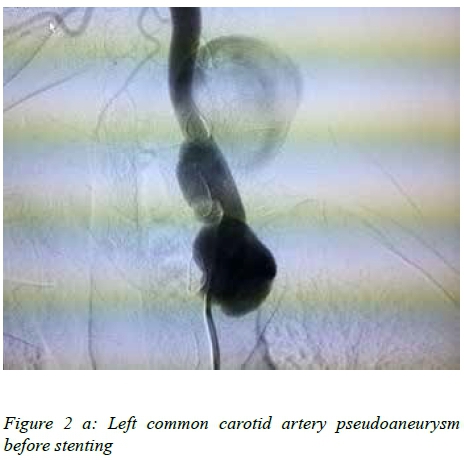
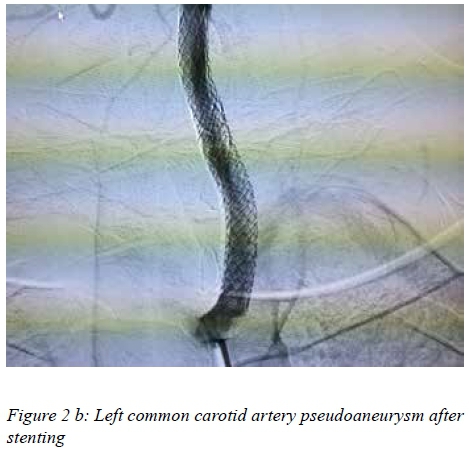
Five arterial injuries (6%) were treated with endovascular stent grafts. These included the proximal common carotid (2), the first part of the subclavian artery (1) and the second part of the subclavian artery (2). A single patient presented five years after the initial injury with a false aneurysm, and in another patient the stent graft was inserted as a bail out procedure to avoid open surgery due to lack of blood in the blood bank. Subclavian and carotid artery stenting is shown in Figure 1 a and b, and Figure 2 a and b, respectively. One of the subclavian artery stent grafts was converted to open repair after three days due to an endoleak. Two patients (2%) were treated endovascularly with coil embolisation; costocervical artery (1) and dorsal scapular artery (1). Seven patients (8%) were treated expectantly; vertebral artery (2), internal carotid artery (2) and descending aortic (3) injuries.


Seven patients (8%) were referred to the quaternary centre at Inkosi Albert Luthuli Central Hospital, Durban. The disciplines to which the patients were referred were cardiothoracic surgery (2) and vascular surgery (5). Aortic arch injuries (2) were repaired operatively with cardiopulmonary bypass, descending aortic injuries (2) were treated by stent graft, and common carotid (1) and subclavian artery injuries (2) were treated by open repair at the quaternary centre.
Of the 20 venous injuries that were managed operatively, 5 were ligated (25%) and 15 were repaired (75%) by simple lateral suture. Ligated veins included the subclavian (2) and axillary veins (3). Thrombosed vertebral arteries (2) and internal carotid arteries (2), and type I descending aortic injuries (3) were managed conservatively.
Postoperative complications were seen in 8 patients (9%); i.e. wound sepsis (2), graft thrombosis (1), graft sepsis (1), mediastinitis (1), missed injury (2) and endoleak (1). Wound sepsis and mediastinitis were treated with antibiotics with full recovery. One thrombosed graft was treated conservatively and the septic graft removed without any further complications. There was no incidence of a stroke or limb loss, despite ligation of the arteries. Eight patients died postoperatively (9%). Seven of the patients who died presented in extremis and died within 24 hours post surgery. One patient died after a week from associated abdominal injuries.
Discussion
As is typical in most trauma series, the patients in our series were young and 90% of them were male.2,14 Eighty-nine per cent of them presented with penetrating injuries, and 87% of these were due to stab wounds. This is in keeping with the literature from South Africa over the last four decades, and reflects the high rate of interpersonal violence in the country.14,15 As expected, cervical vascular injuries were more common than mediastinal vascular injuries (80% versus 20%). Arterial injuries were more common than venous injuries (81% versus 19%), and this is reflective of the fact that many venous injuries thrombosed and stopped bleeding with simple measures, such as the application of direct pressure. Patients who presented with active bleeding or haemodynamic instability were expedited to the operating room and were not investigated further. Although a policy of selective investigation of trauma patients is followed, the widespread availability of CT angiography has resulted in increased reliance on imaging.
Over 90% of all injuries were managed operatively either by open or endovascular procedures, and nearly a third of these open procedures required formal median sternotomy or thoracotomy in order for proximal control to be achieved. These are daunting injuries, and most patients presented acutely and required urgent exploration in less than optimal conditions. Appropriate decision-making in this cohort is important, and the results testify to the fact that a closed system results in very good outcomes for such patients. The fact that seven of the eight patients who demised presented in an agonal state is testament to this. Six of them had an associated venous or cardiac injury, and four of them required median sternotomy. Seven of the patients who died were managed before the inception of the vascular trauma surgery unit. Only one patient died postoperatively due to associated abdominal injuries after the inception of the vascular surgery unit.
The endovascular treatment of traumatic subclavian and axillary artery injuries continues to evolve.16 Du Toit et al.11,17 recommend that the endovascular management of penetrating carotid artery injuries is safe, and that endovascular repair should be considered the first choice of treatment in stable patients with subclavian artery injuries. We continue to have concerns about the durability of a stent graft in a young patient, and in an area with considerable movement and strain, like the subclavian artery. However, there is no doubt that an endovascular approach avoids a difficult operative approach in this instance. We have used it selectively and will continue to follow-up our cohort as best we can, hoping to further define the role of this procedure. Endovascular stent grafts helped to avoid sternotomy in three patients. Currently, endovascular stenting has replaced open surgery for the management of blunt aortic injury. This approach is associated with significantly lower morbidity and mortality in comparison to open repair, although long-term follow-up data are only beginning to emerge now.9,18 Angio-embolisation is well established in trauma, is an important weapon in the armamentarium, and is especially useful for the management of injuries to non-essential vessels.
The ligation of non-essential arteries is a useful approach, and was applied liberally in our series. However, the ligation of the internal carotid artery is controversial, and can result in a stroke in up to 18% of patients, and mortality in up to 45%.19 Four internal carotid arteries were ligated in our series, i.e. those that were thrombosed and had no back bleeding. There is a possibility that repairing the thrombosed internal carotid artery might cause haemorrhagic infarction. Neither a stroke nor mortality were associated with this. Adequate blood flow via the intact circle of Willis in young patients is the most likely explanation for the lack of strokes. Five patients were referred to the Durban vascular surgery department before the inception of the vascular surgery service at Pietermaritzburg. Other patients were not referred after that.
The management principle of cervicomediastinal venous injuries differs to that for arterial injuries. Ligation is an acceptable form of treatment of cervicomediastinal venous injuries in the presence of haemodynamic instability, or where complex methods of repair would otherwise be necessary.20 Despite the ligation of 25% of the venous injuries, there weren't any postoperative complications associated with it, and thus the ligation of complex venous injuries is advocated.
Non-operative management strategies are applicable to less than a tenth of patients with cervicomediastinal vascular trauma. Thrombosed vertebral arteries may be safely observed, and our experience with this injury supports the literature on this topic.21 Two internal carotid arteries were shown to be thrombosed following blunt neck trauma, and were treated expectantly. This also supports the literature on this topic.22 Three descending aortic injuries (type I intimal tear injury) from blunt thoracic trauma were also managed expectantly, again in accordance with evidence in the literature.23
The mortality rate of 9% in our series of complex injuries compares favourably with the rates reported from our parent unit over a decade and a half ago. The mortality rates for penetrating mediastinal arterial injuries, axillary and subclavian artery injuries and venous injuries were 17%, 12% and 16%, respectively, in their series.20,24,25 This reflects improved access to endovascular therapy, and is a testament to the success of our own newly established vascular trauma service.
Conclusion
Cervicomediastinal vascular trauma is complex and challenging. A closed system of care, delivered by a select group of specialists with an interest in vascular trauma, results in very good outcomes for patients who require an operation. The development of endovascular techniques may allow for noninvasive management of a significant number of patients. This subset of patients needs to be managed by a competent vascular and endovascular surgeon. Open surgery is still necessary, and is associated with significant morbidity. Our newly established vascular trauma service is a model which produced comparable, if not better, results, to that of our already established unit.
Declaration
There was no funding for this study.
Conflict of interest
The authors declare that there was no conflict of interest which may have inappropriately influenced them when writing this article.
REFERENCES
1. Du Toit DF, Strauss DC, Blaszczyk M, et al. Endovascular treatment of penetrating thoracic outlet arterial injuries. Eur J Vasc Endovasc Surg. 2000;19(5):489-495. [ Links ]
2. Thoma M, Navsaria PH, Edu S, Nicol AJ. Analysis of 203 patients with penetrating neck injuries. World J Surg. 2008;32(12):2716-2723. [ Links ]
3. Du Toit DF, Odendaal W, Lambrechts A, Warren BL. Surgical and endovascular management of penetrating innominate artery injuries. Eur J Vasc Endovasc Surg. 2008;36(1):56-62. [ Links ]
4. George SM Jr, Croce MA, Fabian TC, et al. Cervicothoracic arterial injuries: recommendations for diagnosis and management. World J Surg. 1991;15(1):134-149. [ Links ]
5. Demetriades D, Skalkides J, Sofianos C, et al. Carotid artery injuries: experience with 124 cases. J Trauma. 1989;29(1):91-94. [ Links ]
6. Johnston RH Jr, Wall MJ Jr, Mattox KL. Innominate artery trauma: a thirty-year experience. J Vasc Surg. 1993;17(1):134-149. [ Links ]
7. Navsaria P, Omoshoro-Jones J, Nicol A. An analysis of 32 surgically managed penetrating carotid artery injuries. Eur J Vasc Endovasc Surg. 2002;24(4):349-355. [ Links ]
8. Jamieson WRE, Janusz MT, Gudas VM, et al. Traumatic rupture of the thoracic aorta: third decade of experience. Am J Surg. 2002;183(5):571-575. [ Links ]
9. Demetriades D, Velmahos GC, Scalea TM, et al. Operative repair or endovascular stent graft in blunt traumatic thoracic aortic injuries: results of an American Association for the Surgery of Trauma Multicenter Study. J Trauma. 2008;64(3):561-571. [ Links ]
10. Demetriades D, Theodorou D, Murray J, et al. Mortality and prognostic factors in penetrating injuries of the aorta. J Trauma. 1996;40(5):761-763. [ Links ]
11. Du Toit DF, Coolen D, Lambrechts A, et al. The endovascular management of penetrating carotid artery injuries: long-term follow-up. Eur J Vasc Endovasc Surg. 2009;38(3):267-272. [ Links ]
12. Campbell FC, Robbs JV. Penetrating injuries of the neck: a prospective study of 108 patients. Br J Surg. 1980;67(8):582-586. [ Links ]
13. Robbs JV, Baker LW, Human RR, et al. Cervicomediastinal arterial injuries: a surgical challenge. Arch Surg. 1981;116(5):663-668. [ Links ]
14. Clarke DL, Quazi MA, Reddy K, Thomson SR. Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. J Thorac Cardiovasc Surg. 2011;142(3):563-568. [ Links ]
15. Sobnach S, Nicol AJ, Nathire H, et al. An analysis of 50 surgically managed penetrating subclavian artery injuries. Eur J Vasc Endovasc Surg. 2010;39(2):155-159. [ Links ]
16. Dubose JJ, Rajani R, Gilani R, et al. Endovascular management of axillo-subclavian arterial injury: a review of published experience. Injury. 2012;43(11):1785-1792. [ Links ]
17. Du Toit DF, Lambrechts AV, Stark H, Warren BL. Long-term results of stent graft treatment of subclavian artery injuries: management of choice for stable patients. J Vasc Surg. 2008;47(4):739-743. [ Links ]
18. Demetriades D, Velmahos GC, Scalea TM, et al. Diagnosis and treatment of blunt thoracic aortic injuries: changing perspectives. J Trauma. 2008;64(6):1415-1419. [ Links ]
19. Du Toit DF, Van Schalkwyk GD, Wadee SA, Warren BL. Neurological outcome after penetrating extracranial arterial trauma. J Vasc Surg. 2003;38(2):257-262. [ Links ]
20. Nair R, Robbs JV, Muckart DJ. Management of penetrating cervicomediastinal venous trauma. Eur J Vasc Endovasc Surg. 2000;19(1):65-69. [ Links ]
21. Mwipatayi BP, Jeffery P, Beningfield SJ, et al. Management of extra-cranial vertebral artery injuries. Eur J Vasc Endovasc Surg. 2004;27(2):157-162. [ Links ]
22. Biffl WL, Moore EE, Offner PJ, et al. Blunt carotid arterial injuries: implications of a new grading scale. J Trauma. 1999;47(5):845-853. [ Links ]
23. Starnes BW, Lundgren RS, Gunn M, et al. A new classification scheme for treating blunt aortic injury. J Vasc Surg. 2012;55(1):47-54. [ Links ]
24. Buchan K, Robbs JV. Surgical management of penetrating mediastinal arterial trauma. Eur J Cardiothorac Surg. 1995;9(2):90-94. [ Links ]
25. McKinley AG, Carrim ATO, Robbs JV. Management of proximal axillary and subclavian artery injuries. BJS. 2000;87(1):79-85. [ Links ]
 Correspondence:
Correspondence:
J Islam
islam@telkomsa.net














