Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.1 Cape Town Mar. 2016
INTENSIVE CARE
Positron emission tomography/computed tomography scanning for the diagnosis of occult sepsis in the critically injured
D MuckartI; T HardcastleI; F PeerII
IDepartment of Surgery, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIDepartment of Nuclear Medicine, Inkosi Albert Luthuli Central Hospital, Durban, South Africa
ABSTRACT
BACKGROUND: Although the site of nosocomial sepsis in the critically ill ventilated patient is usually identifiable, it may remain occult, despite numerous investigations. The rapid results and precise anatomical location of the septic source using positron emission tomography (PET) scanning, in combination with computed tomography (CT), has promoted this modality as the diagnostic tool of choice for pyrexias of unknown origin.
METHODS: The objective of this study was to report our experience using PET/CT scanning for the localisation of a septic focus in critically injured patients in whom no source could be identified using conventional investigations.
RESULTS: Two patients with gunshot wounds and two who had sustained multiple fractures following motor vehicle collisions developed pyrexias of unknown origin during their stay in the trauma intensive care unit. Routine screening for a septic focus was unrewarding, and 18F-fluorodeoxyglucose PET/CT scanning was used to identify the possible source. PET/CT scanning identified the septic focus in all patients. Abscesses were drained successfully in those with penetrating trauma and in one with blunt polytrauma. Pulmonary tuberculosis, not apparent on initial radiology, was identified using PET/CT in one patient with blunt thoracic trauma.
CONCLUSION: PET/CT scanning appears to both confirm and localise the source of sepsis in a variety of pathologies in critically ill patients who develop pyrexias for which no source can be identified by conventional screening techniques.
Pyrexia is a physiological event within the first 48 hours of major injury as a result of the systematic inflammatory response syndrome and the metabolic response to trauma. Thereafter, new-onset fever is pathological, and most commonly arises as a consequence of nosocomial sepsis. Ventilator-associated pneumonia (VAP), vascular catheter-related bloodstream infections, and surgical site infections account for the vast majority, and the source of sepsis is readily identifiable in association with a clinical examination and microbiological cultures. However, on occasion, recurrent episodes of pyrexia occur, and despite repeated cultures of suspected sites, the source of sepsis cannot be found. The activated inflammatory cells accumulate 18F-fluorodeoxyglucose (18F-FDG),1,2 making positron emission tomography (PET) an attractive alternative for the diagnosis of occult sepsis. The combination of PET with computed tomography (CT) scanning produces both morphological and anatomical imaging, thereby confirming and localising a potential source.2 Used extensively to image malignant disease, this technique has been gaining wide acceptance outside of that field, especially for the diagnosis of non-infective inflammatory disorders, orthopaedic and vascular implant sepsis, osteomyelitis and fever of unknown origin.3,4,5 We present the experience of four patients, all of whom had suffered major injury and were treated in the trauma intensive care unit (TICU) at Inkosi Albert Luthuli Central Hospital, and who developed a fever of unknown origin, the source of which was successfully identified by PET/CT scanning.
Method
Ethical approval was obtained from the University of KwaZulu-Natal Bioethics Committee (BE 2007/09). Patients who develop new-onset fever in the TICU undergo a septic screen. This consists of the replacement of all vascular catheters at a new site with culture of the catheter tip, simultaneous peripheral blood cultures, a tracheal trap specimen, catheter specimens of urine and specimens from the surgical sites, if appropriate. Procalcitonin is measured daily, and beta-D-glucan, if fungal sepsis is suspected. Bedside ultrasound is performed for acalculous cholecystitis and plain facial X-rays are taken to identify sinus effusions. An empirical antimicrobial policy is employed in the TICU with respect to both community-acquired and nosocomial sepsis, based on microbiological surveillance. Unenhanced CT was performed using a Biograph® (Siemens, Erlangen, Germany), with a weight-calculated injection of 18F-FDG and an oral dose of water-soluble E-Z-CAT® contrast (Bracco Diagnostics, Monroe Township, USA) for anatomical correlation, followed by delayed PET imaging.
Results
The clinical characteristics of the four patients are summarised in Table 1 (next page).
Case study 1
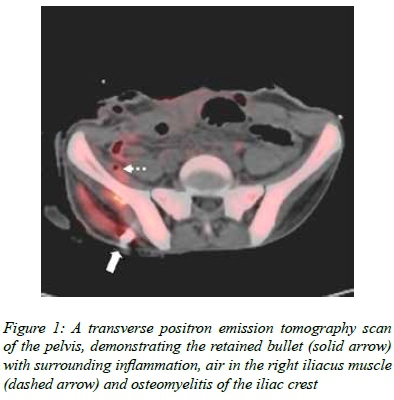
A 30-year-old man, referred from a district hospital, sustained multiple gunshot wounds to the face, abdomen and right leg. Gross faecal contamination from the distal small bowel and ascending colon perforations necessitated a damage control procedure consisting of a haemicolectomy, stapling of the ileal and colonic lumens and a vacuum closure of the abdomen. Microbiology of intraoperative specimens confirmed the adequacy of empirical antimicrobial choice. The combination of four relaparotomies with microbiological sampling and directed therapy, and septic screens, when indicated, appeared to eradicate all sepsis. However, following a quiescent period of 10 days, the patient again became febrile, reaching a zenith of 40°C. Vascular catheters were reinserted and further specimens of tracheal aspirates, urine and blood failed to reveal any pathogens. A CT scan revealed a normal gall bladder and possible fluid collection behind the right kidney and air in the iliacus muscle. A PET/CT scan demonstrated osteomyelitis in the pelvic crest which the bullet had traversed, and an abscess in the iliacus muscle in proximity to a retained missile (Figure 1). The bullet was removed, the abscess drained, the bony sequestrum removed and the bone curetted during surgery. Microbiology revealed Escherichia coli and Proteus mirabilis, both sensitive to tazobactam. The patient was discharged to the base hospital 40 days after admission following surgery and a further course of directed antimicrobial therapy.
Case study 2
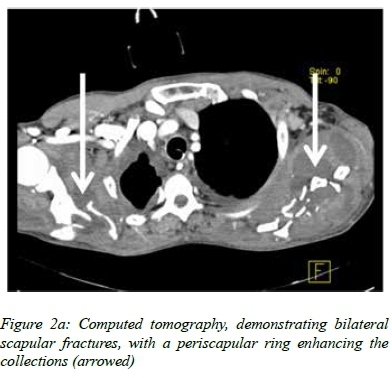
A 49-year-old man, who had fallen from a tractor and subsequently been run over by the same vehicle, sustained multiple injuries. An early VAP, due to Staphylococcus aureus, was treated successfully with cloxacillin. One week later, he developed a swinging pyrexia, which failed to settle, despite changing the vascular catheters, resampling the sputum and urine, taking numerous random blood cultures, and commencing directed therapy for Candida albicans in a tracheal aspirate and empirical meropenem. The CT suggested ring-enhancing lesions of both scapulae (Figure 2a) and the right iliac crest. However, serous fluid only, with no cultured organisms, was shown by aspiration of the latter. The PET/CT scan demonstrated maximal uptake around the comminuted fracture of the left scapula (Figure 2b), from which pus was aspirated. Twenty millilitres of frank pus and necrotic bone were removed during formal drainage under anaesthesia, the culture of which grew S. aureus sensitive to cloxacillin. Valvular lesions were not demonstrated on echocardiography. The fever subsided, and the patient was discharged 50 days after referral.
Case study 3
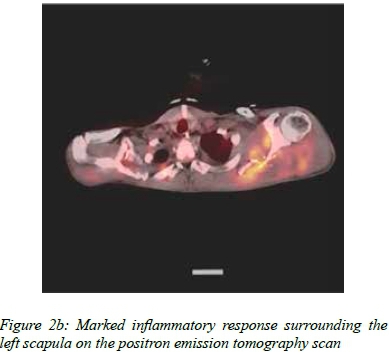
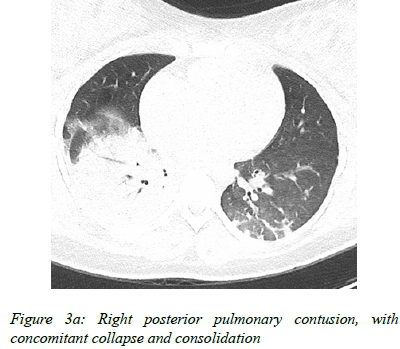
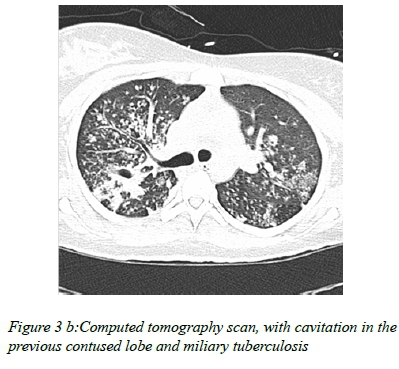
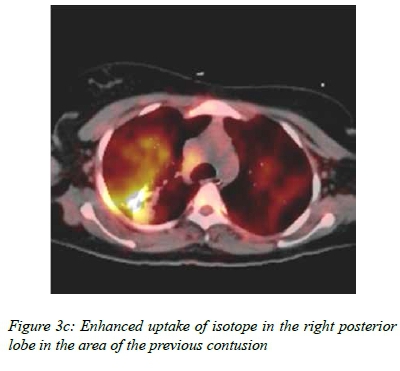
A 23-year-old woman, who had sustained multiple injuries in a pedestrian vehicle collision, was referred from a rural regional hospital for mechanical ventilation after progression of her lung contusions and a possible diagnosis of fat embolism syndrome. A full body trauma CT did not reveal brain pathology nor cervical injury, but the chest phase demonstrated extensive bilateral lung contusions, noted to be worse on the right (Figure 3a). After stabilisation in the TICU, she underwent sequential fracture fixation and wound closure over a period of 17 days. Despite a VAP being treated with culture-directed antimicrobial agents and antifungal medication, and all fractures being internally fixed, her pyrexia and tachycardia persisted. Subsequently, the patient underwent PET/CT on day 30, which demonstrated miliary tuberculosis with right lung middle lobe hyperintensity and associated cavitations, highly suggestive of active disease (Figures 3b and 3c). On further enquiry, there was a history of tuberculosis contact with a first degree relative. Unfortunately, the gene expert specimens were lost in transit, but antituberculous treatment was commenced empirically. She was weaned off ventilation over the following 10 days after a rapid clinical response, and transferred to her referring hospital for rehabilitation 57 days after admission.
Case study 4
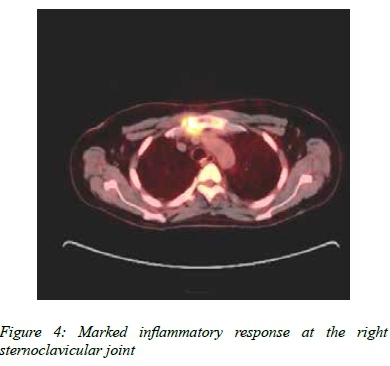
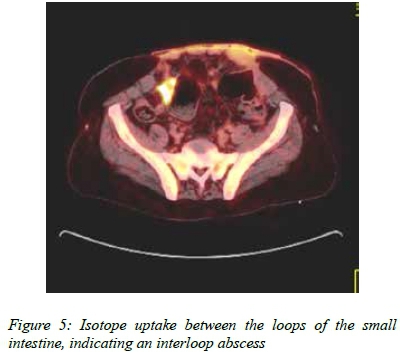
After laparotomy for an abdominal gunshot wound, a 49-year-old man was transferred to the TICU. Shortly after admission, he became haemodynamically unstable and was taken for relaparotomy, where a missed jejunal perforation was found and repaired. Following further relaparotomies, whereby two anastomotical leaks were resected and repaired, he developed an enterocutaneous fistula, for which parenteral nutrition was required. Multiple episodes of sepsis occurred during his protracted hospital stay, but despite adequate abdominal source control, antimicrobial agents and antifungal medication, he developed several episodes of pyrexia, for which a focus could not be identified. A PET/CT scan suggested an infective process involving the right sternoclavicular joint, with intrathoracic extension into the anterior mediastinum, with a small anterior mediastinal inflammatory mass in close proximity to the brachiocephalic artery (Figure 4). This was suspected to be septic arthritis, possibly from repeated difficult central line placement attempts. Two fluid collections were identified, one between the bowel loops, which was metabolically active (Figure 5), and another below the left anterior abdominal wall, which showed no metabolic activity. His fever subsided following CT-guided drainage of the active interloop collection. The left-sided intra-abdominal collection did not undergo drainage. His course was complicated further by a vesicocutaneous fistula and profound hypokalaemia, for which daily infusions of potassium were required, as well as colonic pseudo-obstruction. Despite correction of all electrolyte abnormalities, the gut function failed to recover, and he died following the onset of multiple organ dysfunction 133 days after admission.
Discussion
Fever of unknown origin was defined by Petersdorf and Beeson as an illness of three weeks' duration, a temperature of more than 38.3°C on several occasions, and lack of diagnosis after one week of hospital investigation.6 The differential diagnosis is extensive, and up to one third of patients die as a consequence.7 The definition of fever in the critically ill is identical to that of Petersdorf and Beeson, and new-onset pyrexia of ≥ 38.3°C prompts a number of diagnostic procedures in the search for nosocomial sepsis, and frequently the use of empirical antimicrobial agents while the culture results are awaited.8 Failure of the pyrexia to respond to empirical therapy may result in escalation to ultra-broad-spectrum antimicrobial agents with the potential for selecting multidrug-resistant pathogens. Ongoing inflammation results in a persistent catabolic state, with nutritional and immune depletion, and a protracted length of stay in the intensive care unit, as exemplified by the patients reported herein who spent a combined total of 280 days in intensive care.
Failure in patients who have undergone operative intervention to respond to antimicrobial agents should elicit a search for a surgically correctable focus, especially in those who have suffered hollow visceral abdominal injuries with faecal contamination. Contrast-enhanced CT scanning may demonstrate fluid collections, but these may not contain pus and pathogens and evidence of increased white cell metabolism will distinguish benign from infective foci. Although radio-labelled white blood cells are ideally suited to the evaluation of occult sepsis, and may identify the source with a high degree of accuracy,3,9 there are several disadvantages to this technique. Repeat scans may be required over a number of hours, necessitating frequent transportation of a critically ill patient. Also, the radiation dose may be high, depending on the choice of isotope, and exact localisation is problematic owing to planar imaging.1 Although not universally available, PET/CT scanning has many advantages over the use of labelled white cells in identifying occult sepsis. The results are immediately available, transportation times are minimised, the radiation dose can be substantially reduced, and the investigation has high positive and negative predictive values for a vast spectrum of pathologies, including tuberculosis. Thus, PET/CT has emerged as the diagnostic tool of choice for pyrexias of unknown origin.
Gram-positive metastatic sepsis is difficult to locate because of a paucity of symptoms and localising signs. Early identification is crucial as extended antimicrobial therapy or surgical drainage may be required for these foci, failing which the relapse and mortality rates are significantly higher.10 Given that all the fractures in our patients were closed, and cloxacillin-sensitive S. aureus was isolated from a tracheal aspirate, and subsequently from the scapular abscess, it would appear that the scapular collection arose as a result of bacteraemia and a metastatic staphylococcal deposit. CT scanning alone failed to identify the exact source, as evidenced by the initial aspirate from the fluid collection around the iliac crest. The addition of PET pinpointed the specific location. This emphasises the benefit of this hybrid approach, where CT defines the anatomy, and PET the metabolic activity. An echocardiography was used to exclude valvular disease, as recommended in patients with metastatic Gram-positive infections.11
Activated macrophages and lymphocytes are the initial defensive mechanism against tuberculosis. This immune response may eradicate infection entirely, or induce a latent condition whereby bacteria persist in a nonreplicating state to be reactivated during stress or immune suppression. These inflammatory cells accumulate 18F-FDG, making this isotope an ideal tracer for both the diagnosis and the assessment of response to therapy of granulomatous inflammatory conditions.12 Although the diagnosis of pulmonary tuberculosis may be missed with CT scanning, there was no evidence of the disease on the initial CT scan in our patient. The sole abnormality was bilateral pulmonary contusions. Recrudescence of this disease in countries where tuberculosis is endemic should be considered in the critically ill who develop a fever for which a source cannot be found.
Although used predominantly in non-critically ill patients with a fever of unknown origin, the few studies which have addressed its use in intensive care have been extremely promising, reporting both positive and negative predictive values of ≥ 90%.3,13 These studies have addressed pyrexia of unknown origin in a general ICU population, and a word of caution is necessary with regard to the critically injured, where increased metabolic activity at the fracture sites may result in a false positive scan.14 Fortunately, a comparison could be made with the opposite side in our patient with bilateral scapular fractures, and failed to demonstrate excessive 18F-FDG uptake.
Occult sepsis confers substantial morbidity and mortality in the critically ill. PET/CT scanning may be a valuable and accurate diagnostic modality in situations when conventional screening fails to reveal a source.
REFERENCES
1. Basu S, Chryssikos T, Moghadam-Kia S, et al. Positron emission tomography as a diagnostic tool in infection: present role and future possibilities. Semin Nucl Med. 2009;39(1):36-51. [ Links ]
2. Balink H, Verberne HJ, Bennink RJ, van Eck-Smit BLF. A rationale for the use of F-18 FDG PET/CT in fever and inflammation of unknown origin. Int J Mol Imaging. 2012;2012:165080. [ Links ]
3. Meller J, Sahlmann C-O, Scheel AK. 18F-FDG-PET and PET/CT in fever of unknown origin. J Nucl Med. 2007;48(1):35-45. [ Links ]
4. Tseng J-R, Chen K-Y, Lee M-H, et al. Potential usefulness of FDG PET/CT in patients with sepsis of unknown origin. PLoS One. 2013;8(6):e66132. [ Links ]
5. Haroon A, Zumla A, Bomanji J. Role of fluorine 18 fluorodeoxyglucose positron emission tomography-computed tomography in focal and generalized infectious and inflammatory disorders. Clin Infect Dis. 2012;54(9):1333-1341. [ Links ]
6. Petersdorf RG, Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine (Baltimore). 1961;40:1-30. [ Links ]
7. Mourad O, Palda V, Detsky AS. A comprehensive evidence-based approach to fever of unknown origin. Arch Intern Med. 2003;163(5):545-551. [ Links ]
8. Marik PE. Fever in the ICU. Chest. 2000;117(3):855-869. [ Links ]
9. Minoja G, Chiaranda M, Fachinetti A, et al. The clinical use of 99m-Tc labelled white blood cell scintigraphy in critically ill surgical and trauma patients with occult sepsis. Int Care Med. 1996;22(9):867-871. [ Links ]
10. Vos FJ, Bleeker-Rovers CP, Sturm PD, et al. 18F-FDG PET/CT for detection of metastatic infection in Gram positive bacteremia. J Nucl Med. 2010;51(8):1234-1240. [ Links ]
11. Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30(4):633-863. [ Links ]
12. Heysell SK, Thomas TA, Sifri CD, et al. 18 fluorodeoxyglucose positron emission tomography for tuberculosis diagnosis and management: a case series. BMC Pulm Med. 2013;13:14. [ Links ]
13. Simons KS, Pickkers P, Bleeker-Rovers CP, et al. F-18-fluorodeoxyglucose positron emission tomography combined with CT in critically ill patients with suspected infection. Intensive Care Med. 2010;36(3):504-511. [ Links ]
14. Shon IH, Fogelman I. F-18 FDG positron emission tomography and benign fractures. Clin Nuc Med. 2003;28(3):171-177. [ Links ]
 Correspondence:
Correspondence:
DavidMuckart
davidmuc@ialch.co.za














