Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.1 Cape Town Mar. 2016
PAEDIATRIC SURGERY
An experience of ultrasound-guided hydrostatic reduction of intussusception at a tertiary care centre
M M Ahmad; M D Wani; H M Dar; I N Mir; H A Wani; A N Raja
Department of Surgery, Government Medical College Srinagar, Karan Nagar, Srinagar, Jammu and Kashmi, India
ABSTRACT
BACKGROUND: Intussusception is an important and one of the most commonly encountered diagnoses of intestinal obstruction in the paediatric age group. Ultrasound-guided hydrostatic reduction is an effective, nonoperative treatment modality for this condition and is associated with a high success rate. In addition, it is simple and safe as the entire procedure is carried out with real-time ultrasound, without the hazard of radiation. The aim of this study was to evaluate the efficacy and safety of ultrasound-guided hydrostatic reduction in the management of intussusceptions in the paediatric age group.
METHODS: A case study was carried out on 89 patients diagnosed with intussusception using high-resolution ultrasonography over a period of two years, spanning February 2012 to January 2014. Ultrasound-guided hydrostatic reduction was performed in 78 of these patients, and 11 patients were excluded owing to clinical contraindications. Follow-up ultrasound was performed after 24 hours to rule out recurrence.
RESULTS: The disease was most prevalent in the age group 6-24 months. The ileocolic type was the most common. Mean duration (hours) was 17.02 ± 20.81 for time to presentation. Complete therapeutic reduction was achieved in 70 of the 78 cases, with a success rate of 90%. Two recurrences occurred in the following 24 hours, which were successfully reduced on the second attempt. Complications and mortality did not occur secondary to the procedure.
CONCLUSION: Our study found that ultrasound-guided hydrostatic reduction is a simple, safe and effective nonoperative treatment for intussusceptions in the paediatric age group, and should be the first line of management in appropriate patients.
An intussusception is the invagination of a segment of the proximal bowel (intussusceptum) into the lumen of the distal bowel, i.e. intussuscipiens. The majority (90%) of intussusceptions are ileocolic, while the remaining 10% are of the ileoileal or colocolic type.1
An idiopathic intussusception is the most common cause of small intestinal obstructions in the infant-toddler age group. Peak incidence occurs from six months to three years of life.1,2 The presence of pathological lead points, such as enlarged lymph nodes, a Meckel's diverticulum, polyps and duplication cysts, should be sought if an intussusception occurs outside the peak age group.1-3 Intussusceptions, in correlation with cystic fibrosis, Henoch-Schonlein purpura, haemophilia or intussusception following operative abdominal procedures, are even more rare.4 Ultrasonography is highly accurate in diagnosing intussusceptions, with a specificity of 100% and a sensitivity of 88-93%.5,6 Colour Doppler ultrasound seems to be a promising technique with regard to identifying the vascular changes which occur with intussusception, and is possibly predictive of bowel necrosis.7 Nonoperative reduction is the primary aim once a diagnosis of intussusception has been made.
The nonoperative reduction of intussusceptions, involves the use of air, saline, barium, oxygen, water and water-soluble iodinated contrast medium under fluoroscopic guidance.8-10 There are several publications on the use of air in intussusception reduction.11,12
Ultrasound-guided saline reduction has gained considerable acceptance in recent years as the initial procedure used for both the evaluation and nonoperative treatment of children with intussusception. The success rate of this modality varies at different centres, but is ≥ 80%.8,13,14 Besides radiological changes, the patient experiences several clinical changes during the reduction. Clinical and surgical end points of success are utilised with this technique. The diagnosis and treatment of intussusception is more accurate and favourable, respectively, when performed in collaboration with radiologists and clinicians.
The purpose of our study was to ascertain the effectiveness of ultrasound guidance in the hydrostatic reduction of intussusception in children, in order to spare them exposure to ionising radiation associated with barium enema, as well as standard risks associated with surgery and postoperative complications.
Method
This case study was carried out in the Department of General Surgery, Government Medical College Srinagar, India, over a period of two years from Februrary 2012 to January 2014. Eighty-nine children were evaluated with ultrasonography to confirm the presence of intussusceptions, and were further evaluated with colour Doppler imaging to rule out ischaemia. Seven children with scattered or no vascularity were excluded from the study, in order to avoid complications such as perforation of the bowel. Hydrostatic reduction was not performed in four children with the ileoileal type of intussusception. Inclusion criteria were:
• Children with symptoms of obstruction for a duration of ≤ 48 hours.
• The absence of generalised toxicity, fever and severe dehydration.
• The absence of signs of peritonitis.
• A history of no previous surgery.
• The absence of pnemoperitoneum.
• The presence of blood flow in the affected segment of the bowel on colour Doppler imaging.
Procedure
Patients who fulfilled the inclusion criteria were rehydrated with a solution of Ringer's lactate. A nasogastric tube was inserted, after which they were transferred to the radiology department. The procedure was explained in detail to the children's parents and informed consent obtained. Reduction took place in the ultrasound room by a team consisting of a radiologist and surgeon.
A GE Logiq® linear array transducer of 7.5-10.0MHz (GE Healthcare, Chicago, USA) was used to diagnose the intussusceptions. Transverse and longitudinal views were obtained. Colour Doppler imaging was used in patients, whenever necessary, to evaluate the vascularity of an affected bowel loop. A well lubricated Foley catheter (16-18) (size in French units) was introduced into the rectum for 6-9cm, with the child in the left lateral position. The bulb of the Foley catheter was inflated with 25-30ml of distilled water, and its position confirmed with ultrasonography.
The catheter was connected to an intravenous fluid line and the free flow of normal saline (pre-warmed to normal body temperature) was allowed into the rectum. The saline bottle was suspended at 100-120cm from the bed level.
Gradual distension of the colon and the retrograde movement of the intussusceptum towards the caecum were monitored by real-time ultrasound. Complete reduction was assumed to have taken place once the oedematous ileocaecal value and the passage of saline through the ileocecal valve into the ileum could be observed.
Saline flow was allowed into several loops of ileum. The peritoneal cavity was observed for signs of perforation. The surgeon simultaneously examined the abdomen for guarding and tenderness, and recorded the general condition of the child, the character of the stool and the presence of crying and pain. The procedure was terminated if the abdominal distension worsened, or the abdominal tenderness or general condition became more severe. A maximum of three attempts was made, each lasting for 20-30 minutes, with a gap of 6-8 hours inbetween the two consecutive attempts.
The bowel was decompressed with digital help immediately after the successful reduction. Normal saline instilled in the large bowel was allowed to drain back into the enema can. Before removing the Foley catheter, an ultrasound examination was carried out to confirm the complete reduction of the intussusceptions, and to rule out leakage of fluid into the peritoneum, the presence of any lead point, and the status of the bowel peristalsis. Successfully reduced patients were then transferred back to the ward and monitored with respect to abdominal distension, guarding and tenderness in the abdomen, as well as their general condition, the character of the stool and the presence of crying and pain. They were not discharged until their bowel motion had returned to normal and oral feeding could successfully resume. A follow-up ultrasound study was performed after 24 hours to rule out any recurrences. If the reduction was unsuccessful after three attempts, or if the patient developed signs of peritonitis, he or she was immediately transferred to the operating room for surgery.
Results
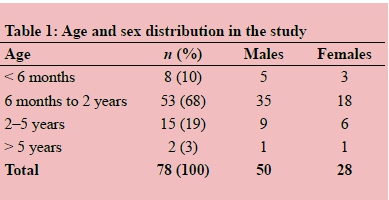
Ultrasound-guided hydrostatic reduction was attempted in 78 of 89 children with intussusceptions that had been confirmed using ultrasound. The youngest patient in the study group was five months' old and the oldest 5 years and 7 months. The mean age of the patients was 18 months. Most of the patients were 6-24 months' old. The male to female distribution was 1.8:1.0, as depicted in Table 1.
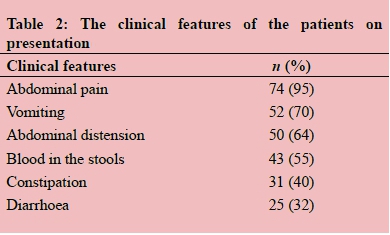
Intermittent colicky abdominal pain was the most commonly reported symptom (Table 2).
The duration of the symptoms was highly variable, with a range of 3-130 hours and an average of 17.02 ± 20.81. Complete reduction was achieved in 70 of the 78 patients in whom it was attempted, with a success rate of 90%. Partial reduction was possible in three patients, following failure to achieve reduction up to the caecum. Henceforth, there was no inflow of fluid into the ileum. There was persistent sonographic evidence of intussusceptions on post-evacuation ultrasound in these patients. Two patients experienced recurrence within 24 hours of the procedure. These were detected on follow-up ultrasound, and successfully reduction was achieved on the second attempt.
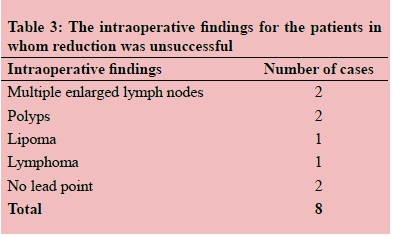
Eight patients in whom reduction was unsuccessful underwent an operation. The intraoperative findings are detailed in Table 3.
The amount of normal saline used for successful reduction ranged from 500-1 000ml (with an average of 700ml). The average time taken for the procedure was 15 minutes (with a minimum of six minutes, and a maximum of 28 minutes). Complications, mortality or morbidity did not occur secondary to the procedure.
Discussion
Intussusception is a common cause of acute intestinal obstruction in children. The exact cause is unknown in most cases. Swollen Peyer's patches, lymph nodes, polyps, submucosal lipomas, a Meckel's diverticulum and duplication cysts are some of the aetiological causes cited.1-5
Once diagnosed, they should be treated as soon as possible. If untreated, the bowel loop may become gangrenous, resulting in sloughing, perforation and peritonitis, and may eventually lead to death.15 Occasionally, intussusceptions can reduce spontaneously.16
Ultrasound scanning is a very useful examination with which to diagnose intussusceptions, with high sensitivity (98-100%) and specificity (88-100%).11 The "target sign" described in the literature is very useful, and can easily be detected by a high-resolution ultrasonography transducer (7.5-10.0MHz).17 The absence of blood flow in the lesion on colour Doppler imaging correlates significantly with the high incidence of complications and irreducibility seen with the non-surgical methods.18 Nonoperative procedures are the initial modality of treatment for intussusceptions. Barium enema reduction is the classical nonsurgical reduction of intussusception. More recently, air insufflation has become popular worldwide. However, exposure of the child and the reduction team to ionising radiation is a disadvantage of both techniques.19-21
An ultrasound-guided hydrostatic reduction, with the use of normal saline, is believed to be one of the most promising method of non-surgical treatment of a paediatric intussusception.11,18 It is a relatively simple, effective, economical, quick procedure, and associated with relatively few complications (i.e. a very low perforation rate), the absence of the hazard of radiation and a minimal hospital stay.22 Our study documents the same as a success rate of 90% was achieved, with an average time of 15 minutes to achieve the ultrasound-guided hydrostatic reduction. The clinical findings in our study, i.e. the age and sex of the patient and the mean time taken for the reduction were comparable with those reported in other studies previously.18,22 Ultrasound-guided hydrostatic reduction is also associated with less morbidity, i.e. there is an absence of pseudoreduction, as seen with fluoroscopic-guided procedures, and there is no fluctuation in the intracolonic pressure, as seen with an air enema. The possibility of perforation is extremely low because the pressure exerted on the bowel wall is more evenly distributed with saline.23 However, if intestinal perforation occurs, it is immediately and accurately recognised using ultrasound.19 Moreover, if perforation occurs, the flow of the saline into the peritoneal cavity does not result in chemical peritonitis, as is seen when perforation occurs with a barium enema, and does not cause tension pneumoperitoneum, as with an air enema.19,20 The mortality rate is also nil, i.e. there is no reported case of death; not the case with an air enema.18,19,24 Contraindications to a hydrostatic reduction include absent or scattered vascularity within the lesion on colour Doppler imaging, evident signs of perforation and peritonitis, ascites, multiple intussusceptions and recurrent intussusceptions with known pathological lead points. However, minimal free fluid without any signs of perforation or peritonitis is not a contraindication to the hydrostatic reduction of an intussusception. Complete ultrasound-guided hydrostatic reduction of the intussusceptions was achieved in our case study in 70 of the 78 patients, with a success rate of 90%. There were two recurrences in our study within 24 hours of the procedure, similar to the findings in other studies.22 Our results further suggest that age, duration of symptoms and the site of the intussusception are not contraindications to a non-surgical reduction. Re-intussusception was present in two of our patients after successful reduction. This indicates that the family and thr surgeon should be careful about the risk of intussusception recurring a few hours to a few days subsequent to a successful reduction. Although this technique is very useful in recent-onset intussusceptions, i.e. within 48 hours, the longer time lapses to presentation should not be a contraindication to trying this method in the absence of abdominal or systemic complications.18,19 Being able to assess the affected bowel loop for the presence of vascularity using colour Doppler ultrasound is an added advantage when deciding the prognostic outcome of cases, in addition to the selection of cases for surgery without any delay if the vascularity is compromised.
Conclusion
Ultrasound with colour Doppler imaging followed by ultrasound-guided hydrostatic reduction using normal saline for intussusceptions in the paediatric age group is a safe, simple, effective and radiation-free technique. It is not time consuming, is cost-effective, prevents the exposure of children to radiation, and is associated with almost no complications and a minimal hospital stay. There is a high success rate using the procedure in properly selected patients. It is strongly advised that this procedure is advocated as the first-line treatment in selected patients to avoid harmful radiation and unwarranted surgery with associated complications. We reported a success rate of nearly 90%, with no morbidity or mortality occurring secondary to the procedure. However, complete reduction is not possible in cases where a pathological lead point is present. Nevertheless, the introduction of a normal saline enema helps to partially reduce the intussusceptions, and the surgery can then be planned accordingly.
Conflict of interest
The authors do not declare a conflict of interest.
REFERENCES
1. Silverman FN, Pkuhn J. Intussusception. Caffey's paediatric X-ray diagnosis. 9th ed. London: Mosby, 1993, p. 1076-1085. [ Links ]
2. Limberg B. Invagination. In: Limberg B, editor. Sonographie des gastrointestinaltrakts. Berlin: Springer Verlag, 1998; p. 93-97. [ Links ]
3. Sutton D, editor. Textbook of radiology and imaging. 7th ed. London: Churchill Livingstone, 2003; p. 849-850, 872-874. [ Links ]
4. Eich FG, Willi UV. Acute abdomen in children. In: Krestin GP, Choyke P, editors. Acute abdomen. Stuttgart: Georg Thieme Verlag, 1996; p. 255-259. [ Links ]
5. Verschelden P, Filiatrault D, Garel L, et al. Intussusception in children: reliability of US in diagnosis - a prospective study. Radiology. 1992;184(3):601-602. [ Links ]
6. Bhisitkul DM, Listernick R, Shkolnik A, et al. Clinical application of ultrasonography in the diagnosis of intussusception. J Pediatr. 1992;121(2):182-186. [ Links ]
7. Kong MS, Wong HF, Lin SL, et al. Factors related to detection of blood flow by color Doppler ultrasonography in intussusception. J Ultrasound Med. 1997;16(2):141-144. [ Links ]
8. Hadidi AT, El Shal N. Childhood intussusception: a comparative study of nonsurgical management. J Pediatr Surg. 1999;34(2):304-307. [ Links ]
9. Riebel TW, Nasir R, Weber K. US-guided hydrostatic reduction of intussusception in children. Radiology. 1993;188(2):513-516. [ Links ]
10. Choi SO, Park WH, Woo JK. Ultrasound guided water enema: an alternative method of nonoperative treatment for childhood intussusception. J Pediatr Surg. 1994;29(4):498-500. [ Links ]
11. Del-Pozo G, Albillos JC, Tejedor D, et al. Intussusception in children: current concepts in diagnosis and enema reduction. Radiographics. 1999;19(2):299-319. [ Links ]
12. Daneman A, Alton DJ. Intussusception: issues and controversies related to diagnosis and reduction. Radiol Clin North Am. 1996;34(4):743-756. [ Links ]
13. González-Spínola J, Del Pozo G, Tejedor D, Blanco A. Intussusception: the accuracy of ultrasound-guided saline enema and the usefulness of a delayed attempt at reduction. J Pediatr Surg. 1999;34(6):1016-1020. [ Links ]
14. Wang GD, Liu SJ. Enema reduction of intussusception by hydrostatic pressure under ultrasound guidance: a report of 377 cases. J Pediatr Surg. 1988;23(9):814-818. [ Links ]
15. Ugwu BT, Legbo JN, Dakum NK, et al. Child hood intussusception: 9 year review. Ann Trop Paediatr. 2000;20(2):131-35. [ Links ]
16. Swischunk LE, John SD, Swischunk PN. Spontaneous reduction of intussusception: verification with ultrasound. Radiology. 1994;192(1):269-271. [ Links ]
17. Mirilas P, Koumanidou C, Vakaki M, et al. Sonographic features indicative of hydrostatic reducibility of intestinal intussusception in infancy and early childhood. Eur Radiol. 2001;11(12):2576-2580. [ Links ]
18. Krishnakumar, Hameed S, Maheshwari U. Ultrasound guided hydrostatic reduction in the management of intussusception. Indian J Paediatr. 2006;73(3):217-220. [ Links ]
19. Daneman A, Navarro O. Intussusception. Part 2: An update on the evolution of management. Pediatr Radiol. 2004;34(2):97-108. [ Links ]
20. Sorantin E, Lindbichler F. Management of intussusception. Eur Radiol. 2004;14 Suppl 4:L146-L154. [ Links ]
21. Chan KL, Saing H, Peh WC, et al. Childhood intussusception: ultrasound-guided Hartmann's solution hydrostatic reduction or barium enema reduction? J Pediatr Surg. 1997;32(1):3-6. [ Links ]
22. Tander B, Baskin D, Candam M, et al. Ultrasound guided reduction of intussusception with saline and comparison with operative treatment. Ulus Travma Acil Cerrahi Derg. 2007;13(4):288-293. [ Links ]
23. Zambuto D, Bramson RT, Blickman JG. Intracolonic pressure measurements during hydrostatic and air contrast barium enema studies in children. Radiology. 1995;196(1):55-58. [ Links ]
24. Khong PL, Peh WC, Lam CH, Chan KL. Ultrasound-guided hydrostatic reduction of childhood intussusception: technique and demonstration. Radiographics. 2000;20(5):E1. [ Links ]
 Correspondence:
Correspondence:
Mir Mujtaba Ahmad
drmirmujtaba1@gmail.com














