Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.53 no.3-4 Cape Town Dez. 2015
INTENSIVE CARE
Tracheostomy, ventilation and anterior cervical surgery: Timing and complications
K DüsterwaldI; N KrugerII; R N DunnIII
IUniversity of Cape Town
IIDivision of Orthopaedic Surgery, University of Cape Town
IIIDivision of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
ABSTRACT
BACKGROUND: Cervical spine injured patients often require prolonged ventilatory support due to intercostal paralysis and recurrent chest infections. This may necessitate tracheotomy. Concern exists around increased complications when anterior cervical spine surgery and tracheotomies are performed.
OBJECTIVE: The primary aim of this study was to evaluate the effect of tracheostomy in anterior cervical surgery patients in term of complications. In addition, the aetiology of trauma and incidence of anterior surgery and ventilation in this patient group was assessed.
METHODS: Patients undergoing anterior cervical surgery and requiring ventilation were identified from the unit's prospectively maintained database. These patients were further sub-divided into whether they had a tracheotomy or not. The aetiology of injury and incidence of complications were noted both from the database and a case note review.
RESULTS: Of the 1829 admissions over an 8.5 year period, 444 underwent anterior cervical surgery. Of the 112 that required ventilation, 72 underwent tracheotomy. Motor vehicle accidents, followed by falls, were the most frequent cause of injury. There was a bimodal incidence of tracheostomy insertion, the day of spine surgery and 6-8 days later. There was no difference in the general complication rate between the two groups. With regards to specific complications attributable to the surgical approach/tracheotomy, there was no statistically significant difference. The timing of the tracheotomy also had no effect on complication rate. Although the complications occurred mostly in the formal insertion group as opposed to the percutaneous insertion group, this was most likely due to selection bias.
CONCLUSION: Anterior cervical surgery and subsequent tracheostomy are safe despite the intuitive concerns. Timing does not affect the incidence of complications and there is no reason to delay the insertion of the tracheostomy. Ventilation in general is associated with increased complications rather than the tracheostomy tube per se.
Anterior cervical surgery via the Smith Robinson approach has become a popular choice for managing sub-axial cervical spinal pathology. This approach exploits the intermuscular plane between sternocleidomastoid muscle, carotid artery and jugular vein laterally and the strap muscles, trachea and oesophagus medially. It allows for minimal tissue disruption and ease of access.1 This excellent access provides for decompression of the spinal cord by means of bony resection (corpectomy) and reconstruction or fusion with instrumentation. Surgical intervention is done early following injury to optimise the chance of neurological recovery but also to provide mechanical stability, obviating the need for extraneous traction and thus facilitating nursing care.2,3
Respiratory embarrassment is common in cervical cord injured patients due to the loss of intercostal innervation and the reliance on diaphragmatic breathing. Initially the patients may fatigue with resultant hypercapnia.
Reduced chest motion and air flow results in atelectasis and subsequent infection. This may necessitate ventilator support for a prolonged period. For this reason, patients with cervical cord injury frequently require tracheostomy to avoid the problems of medium to long term oral/nasal endotracheal tubes (ETT).
Thus one is often faced with the dilemma of converting an ETT to a tracheostomy in a patient who has recently undergone anterior cervical surgery. There are obvious concerns regarding subsequent wound infection, especially in the light of the implanted spinal instrumentation, as well as increased dysphagia.4-6
The primary aim of this study was to evaluate the effect of tracheostomy in anterior cervical surgery patients in term of complications. In addition, the aetiology of trauma and incidence of anterior surgery and ventilation in this patient group was assessed.
Methods
A retrospective study was performed on acute spinal cord injury (ASCI) patients admitted to Groote Schuur Hospital (GSH) ASCI unit between 1 January 2004 and 17 July 2013 by analysing a prospectively maintained database. This database included patient information history, diagnosis, complications sub-classified by anatomical system, ventilation requirements and surgical procedure. The surgery detail included approach, date, description, and levels of the spine affected. Additional data was recorded but was not relevant for the study. The choice of procedure was determined by the nature of the injury and the surgeon's preferences. All patients had prophylactic cefazolin pre-incision and for 24 hours post operatively unless penicillin sensitive, when clindamycin was used.
The database was interrogated for patients having undergone anterior surgery in the cervical (C1-T1) region. Among these, patients who were ventilated were identified and a case note review was performed with respect to type of tracheostomy and subsequent events.
Twelve cases were excluded based on unavailability of folders (7), inadequate notes (4), or because surgery had taken place at another hospital where surgery-related data was not available (1).
Results were analysed using MySQL database package and Libre Office Calc. A frequency analysis of the timing of tracheostomy procedures relative to anterior cervical surgery was done. Complication number was compared between the group with tracheostomy and the group without tracheostomy using the χ2 test. The χ2 test was also used to compare intervals of timing in order to determine the significance for complication of tracheostomies performed within 5 days of anterior cervical surgery compared to tracheostomies performed later than 5 days after the procedure. The influence of the type of tracheostomy procedure on complication numbers was then analysed statistically. A significance level of p = 0.05 was used.
Results
During the 9.5 year period, 1 829 spine injured patients were admitted to the Groote Schuur Hospital ASCI unit giving an average of 192 admissions annually. Of these, 444 (24.3%) patients underwent anterior cervical surgery. Ventilation was required in 124 (27.9%) of these patients. Of the anterior surgery patients who were ventilated, 12 (9.7%) patients' folder records were unavailable and were excluded. Of the remaining 112 patients, 72 (64.3%) underwent tracheostomy procedures.
Table 1 summarises the aetiology of the injuries with motor vehicle accidents being the predominant cause followed by falls. Interpersonal violence was a more prevalent cause in the tracheostomy group.
Of the 72 tracheostomies, 52 (72.2%) were done formally in theatre, 17 (23.6%) were percutaneous and 3 were of unknown type. There was no statistically significant association between tracheostomy type and general complication number (χ2 = 0.001, p > 0.9).
The median time between surgery and tracheostomy was 7 (-30 - 61 ± 9.2) days with an inter-quartile range of [0; 12.25] days. One tracheostomy was done 667 days after the anterior cervical procedure owing to re-admission, and was excluded from the aforementioned range. The others were done within two months of the anterior cervical surgery. Four patients had tracheostomies before their anterior cervical surgery, hence the negative 30 days as the minimum value in the range. Fifteen tracheostomies were performed on the same day as surgery, and 14 performed 6-8 days after surgery. These two high frequencies created the bimodal distribution depicted in Figure 1.
Respiratory complications, most often bronchopneumonia, were present in 94.2% of the tracheostomy patients and in 86.2% of those without tracheostomy. A non-respiratory general complication rate, i.e. irrespective of whether it was thought to be related to the tracheostomy or surgery or not, of 55 of 72 (76.4%) occurred in the tracheostomy group and 29 of 42 (69.0%) in the non-tracheostomy group. These included decubitus ulcers, urinary tract infections and venous thrombosis. This difference was not statistically significant (χ2 = 0.74, p > 0.3).
When compared to the entire database of patients that underwent anterior surgical procedures irrespective of ventilation status, there was a statistically significant increased complication rate when a tracheostomy was present (%2 = 47.14, p < 0.0005). Similarly, results were statistically significant for complication development in the entire ventilated group compared to the anterior cervical surgery patients who did not need to be ventilated (χ2 = 76.00, p < 0.0005).
All the patients who had tracheostomies before surgery had developed bronchopneumonia prior to tracheostomy. For the group of patients with tracheostomies performed within 5 days after the anterior cervical procedure, there was a 70.0% chance of developing some complication, whereas for the group that had a tracheostomy between 5 and 10 days after the procedure there was an 87.0% complication rate. Among the group with an interval of 10 to 15 days there was a 58.3% complication occurrence. The χ2 test revealed that timing of tracheostomy after anterior procedure, classed in intervals of 0-5 days, 5-10 days, 10-15 days, 15-20 days and 20-45 days, disregarding outliers, was however statistically insignificant in the development of complications (χ2n=4 = 5.71, p > 0.2).
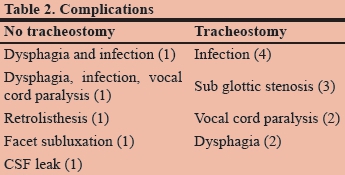
Complications directly attributable to anterior surgery or tracheostomy were then assessed. Table 2 tabulates the 5 complications in the non-tracheostomy group and 11 in the tracheostomy group. Of the latter, 10 were formal open tracheostomies as opposed to the percutaneous technique. The results were evenly spread over the entire range of timings. There was no statistical difference in the frequency of these complications (p = 0.90). There was a trend to increased non-orthopaedic complications in the non-tracheostomy group (p = 0.13).
Discussion
The acute management of respiratory failure is endotracheal intubation. In the cervical spinal cord injured patient, prolonged ventilation is required due to poor respiratory effort from chest wall paralysis and frequent pulmonary infections from atelectasis, retained secretions and respiratory failure.3,7-9 When ventilation is expected for more than a few days, conversion to tracheostomy is employed as it facilitates oral care, feeding and avoids the complications of oral and nasal pressure areas from the tube. In addition, dead space is reduced which facilitates weaning. A reduction in mortality with the use of tracheostomy has been reported by Kollef et al.10
There is an intuitive concern that anterior cervical spine surgery may be compromised by subsequent insertion of a tracheostomy tube due to wound contamination as there is generally some local skin irritation around the mobile tracheostomy tube. This study confirms that this is not the case. There was no increase in wound infection between the tracheostomy and non-tracheostomy group.
This is probably due to the nature of the surgical access. The anterior spine is approached via the Smith Robinson approach which utilises the plane between sternocleidomastoid and the strap muscles whereas the tracheostomy is a direct anterior approach between the strap muscles. Depending on the level of the spine addressed, the spine approach incision may be cephalad to the tracheostomy incision or at the same level if lower down the axial spine. In addition, due to the intermuscular plane, the anterior cervical approach generally results in minimal bleeding and is thus less likely to cause post-operative haematoma. The surrounding muscle provides a well vascularised area which may also reduce the risk of infection.
The increased complication rate of ventilated patients versus non-ventilated is probably indicative of the severity of neurological insult and underlying co-morbidities.
The timing of tracheostomy procedures relative to anterior cervical surgery was bimodal (with two groups of high frequency). The high frequency of procedures done immediately after spinal surgery could be accounted for by the practical advantage of being able to perform both procedures on the patient already in theatre and avoiding a second anaesthetic. The second peak, which occurred about a week later, is generally due to the clinicians recognition of a prolonged wean and thus the conversion to tracheostomy.
In our unit we prefer to limit the use of ETT to a week or less. Weaning is easier with a tracheostomy due to the reduced dead space as well as allowing oral feeding. Logistic delays are common because of limited availability of ENT surgeons and the perceived low priority of tracheostomy procedures in operating theatre scheduling. Reluctance to schedule tracheostomies too soon after spinal surgery because of fear of complications in recovering patients has also been noted as a factor in other authors' work.11 Babu reviewed 1 184 ACDF patients over a 5 year period and identified 20 (1.7%) that required post-spine surgery tracheostomy at a mean of 6.9 days. He reported no wound infection and concluded that early post-surgery tracheostomy was safe.12 Stahel criticised the aforementioned paper on the basis that 6.9 days post-surgery was too late, and advocated tracheotomy at the same sitting as ACDF to potentially reduce the incidence of pneumonia.13
Tracheostomies done prior to anterior cervical surgery in our series were rare as the spinal procedure is prioritised above tracheostomy in most cases. In addition, it is technically demanding to approach the spine around an existing tracheostomy tube. In the 4 cases that had tracheotomies before spine stabilisation, two experienced tracheostomy related complications (50%). These cases were assessed as too physiologically unstable for prolonged spinal surgery. This small number makes analysis difficult.
In our series timing was statistically insignificant in the development of complications - early and same day tracheostomies were statistically and qualitatively safe. Comparisons of the number of direct post-operative complications of surgery or tracheostomy in patients in the ventilated group supported the conclusion, despite a slight increase in complication rate in tracheostomy patients.
This is supported by Young who addressed timing in a multicentre randomised control study. He compared two cohorts of tracheostomy less than 4 days from ACDF and greater than 10 days. He noted no difference in 30 day mortality, tracheostomy related complications, total hospital stay or 30 day antibiotic use.14
With regard to the type of tracheostomy placements, the majority of the complications occurred in the formal group as opposed to the percutaneous group. Not only was this not statistically significant, there was selection bias in that only patients with slender necks and no swelling undergo the percutaneous approach in our unit. Higgens performed a meta-analysis on tracheostomy type and concluded that the percutaneous technique had fewer wound complications but no difference in false passage, haemorrhage, subglottic stenosis and overall complications. The main advantage of the percutaneous option was quicker with less exposure and allowed bedside insertion.15
Our tracheostomy-associated complications of dysphagia and dysphonia are confirmed by other authors.5,6
In summary, anterior cervical surgery and tracheostomy appear safe despite the intuitive concerns. Timing does not affect the incidence of complications and there is no reason to delay the insertion of the tracheostomy. Ventilation in general is associated with increased complications rather than the tracheostomy tube.
Acknowledgement
The authors would like to acknowledge Siza Gusha, second year medical student, for assistance with data collection.
REFERENCES
1. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40:607-624 [ Links ]
2. Bourassa-Moreau É, Mac-Thiong J-M, Ehrmann Feldman D, Thompson C, Parent S. Complications in acute phase hospitalization of traumatic spinal cord injury: does surgical timing matter? J Trauma Acute Care Surg. 2013 Mar;74(3):849-54 [ Links ]
3. Frielingsdorf K, Dunn RN. Cervical spine injury outcome-a review of 101 cases treated in a tertiary referral unit. S Afr Med J. 2007 Mar;97(3):203-7 [ Links ]
4. Berney S, Opdam H, Bellomo R, Liew S, Skinner E, Egi M, et al. An assessment of early tracheostomy after anterior cervical stabilization in patients with acute cervical spine trauma. J Trauma. 2008 Mar;64(3):749-53 [ Links ]
5. Kirshblum S, Johnston M V, Brown J, O'Connor KC, Jarosz P. Predictors of dysphagia after spinal cord injury. Arch Phys Med Rehabil. 1999 Sep;80(9):1101-5 [ Links ]
6. Myers EN, Johnson JT, editors. Tracheostomy: Airway Management, Communication, and Swallowing. 2nd ed. Oxfordshire: Plural Publishing; 2008. [ Links ]
7. Zimmer MB, Nantwi K, Goshgarian HG. Effect of Spinal Cord Injury on the Respiratory System: Basic Research and Current Clinical Treatment Options. J Spinal Cord Med. 2007; 30(4):319-330 [ Links ]
8. Claxton A, Wong D. Predictors of hospital mortality and mechanical ventilation in patients with cervical spinal cord injury. Canadian journal of Anaesthesia. 1998; 45(2): 144-9 [ Links ]
9. Chen Y. Identification of risk factors for respiratory complications in upper cervical spinal injured patients with neurological impairment. Acta Orthopaedica et Traumatologica Turcica. 2013;47(2):111-7 [ Links ]
10. Kollef MHM, Ahrens TSR, Shannon WP. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999;27(9):1714-20. [ Links ]
11. O'Keeffe T, Goldman R. Tracheostomy after anterior cervical spine fixation. J Trauma 2004 Oct;57(4):855-60 [ Links ]
12. Babu R, Owens TR, Thomas S, Karikari IO, Grunch BH, Moreno JR, et al. Timing of tracheostomy after anterior cervical spine fixation. J Trauma Acute Care Surg. 2013 Apr;74(4):961-6 [ Links ]
13. Stahel, Philip F. MD; Moore, Timothy A. MD; VanderHeiden, Todd F. MD. Comment on: Timing of tracheostomy after anterior cervical spine fixation. J Trauma Acute Care Surg. 2013 Sept: 75(3): 538-914. [ Links ]
14. Young D, Harrison DA, Cuthbertson BH, Kathy Rowan. Effect of Early vs Late Tracheostomy Placement on Survival in Patients Receiving Mechanical Ventilation - The TracMan Randomized Trial. JAMA 2013 309(20):2121-9 [ Links ]
15. Higgins KM, Punthakee X. Meta-Analysis Comparison of Open Versus Percutaneous Tracheostomy. Laryngoscope 2007 117:447-454 [ Links ]
 Correspondence:
Correspondence:
Robert Dunn
robert.dunn@uct.ac.za














