Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.53 no.3-4 Cape Town Dez. 2015
HEAD AND NECK SURGERY
The surgical management of parotid gland tumours
M A F CastroI; R A DedivitisII; A V GuimarãesIII; C R CerneaII; L G BrandãoII
ISchool of Medical Sciences, Fundação Lusíada UNILUS; Head and Neck Surgery, Hospital Ana Costa, Santos, São Paulo, Brazil
IIDepartment of Head and Neck Surgery, Hospital das Clinicas, São Paulo School of Medicine, University of São Paulo, Santos, São Paulo, Brazil
IIIDepartment of Otorhinolaryngology, Head and Neck Surgery, Universidade Metropolitana de Santos, Santos, São Paulo, Brazil
ABSTRACT
BACKGROUND: The parotid tissue can give rise to a large variety of benign and malignant neoplasms. The objective of this study was to describe the management and outcome of parotid gland tumours over a 15-year period.
METHOD: The records of consecutive patients treated by parotid gland excision from January 1995 to December 2008 were reviewed retrospectively. Data recorded were age, gender, history, physical findings, surgical procedure, fine-needle aspiration biopsy (FNAB), final pathological diagnosis and complications.
RESULTS: The vast majority of patients (306) had benign neoplasms, and 14 patients had malignant neoplasms. Overall, pleomorphic adenoma contributed to 76% of the lesions, and Warthin's tumour to 17%. The sensitivity and specificity of FNAB was 79% and 100%, respectively. There were 15 cases of marginal mandibular transitory paresis and 12 cases of seroma. Marginal mandibular definitive paralysis was observed in three cases with malignant tumour.
CONCLUSION: Standardised parotidectomy is a safe operation, with a low complication rate.
The parotid is the largest salivary gland in the body. The acinar, ductal and myoepithelial cells, which comprise parotid tissue, can give rise to a large variety of benign and malignant neoplasms. Parotid tumours are seen as painless, slowly growing lumps, and most of these are benign, with pleomorphic adenoma predominating.1 Salivary gland tumours are uncommon, accounting for 3% of all head and neck tumours.2 Fine-needle aspiration biopsy (FNAB) is safe, simple and well tolerated, and can be used selectively or as a routine evaluation.3 Superficial parotidectomy for pleomorphic adenoma is the most frequent operation performed.2 The aim of this study is to describe the management and outcome of parotid gland tumours over a 15-year period.
Method
Chart review was possible for 320 consecutive patients from January 1995 to December 2008. Demographic and follow-up clinical information was obtained from a review of the patients' medical histories. The data recorded were age, gender, history, physical findings, surgical procedure, fine-needle aspiration biopsy (FNAB), final pathological diagnosis and complications. Ages ranged from 19-87 years (median 47 years) and included 171 men and 149 women (1.14:1). The charts were analysed with regard to the following perioperative complications: seroma, haematoma, salivary fistula and complicated wound healing. Complicated wound healing was defined as a wound that was not closed within 10 days of surgery. The facial nerve function of the patients was recorded at discharge. Paralysis was defined as the complete loss of muscle function on the affected side, without any sign of voluntary muscle potential in needle electromyography. Partial paresis was defined as paresis of one or several peripheral facial nerve branches. An isolated paresis of the marginal mandibular branch was also documented. Nerve-integrity monitoring was not used in our series. Sialadenitis and sialolithiasis cases were previously excluded from this study. FNAB and frozen section were carried out on the patients.
Limited superficial parotidectomy was usually performed. It was recognised that at least part of the operation in most cases would involve controlled dissection of the capsule of the tumour, where it abuts the plane of the facial nerve. Initial superficial parotidectomy, in which all branches of the facial nerve are exposed, might be necessary to facilitate the safe removal of a tumour lying deep to the plane of the facial nerve.
The patients were followed-up for a minimum of six months, with a mean of 12 months for patients with benign neoplasms, and 48 months for patients with malignant tumours.
Results
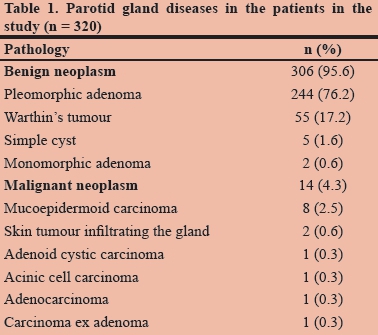
Three hundred and twenty patients who were diagnosed with parotid gland neoplasms were analysed retrospectively. The vast majority of patients (306) had benign neoplasms, and 14 patients had malignant neoplasms (Table 1). Overall, pleomorphic adenoma contributed to 76% of the lesions and Warthin's tumour to 17%.
The sensitivity and specificity of the FNAB investigation was 79% and 100%, respectively. The predictive value of the negative test was 99%, and the predictive value of the positive test 100%. The accuracy was 99%.
Patients with benign tumours experienced no recurrence during the follow-up period. The patient with carcinoma ex-adenoma underwent gland resection with unilateral selective supraomohyoid neck dissection and adjuvant radiation therapy. Two patients with mucoepidermoid carcinoma presented with high jugular lymph node recurrence 12 and 20 months after the surgery, respectively. Both were salvaged with supraomohyoid neck dissection and did not undergo adjuvant treatment. They were alive with no evidence of disease after 24 and 30 months, respectively. The other patients with malignant disease did not undergo radiation therapy, and did not present with recurrence.
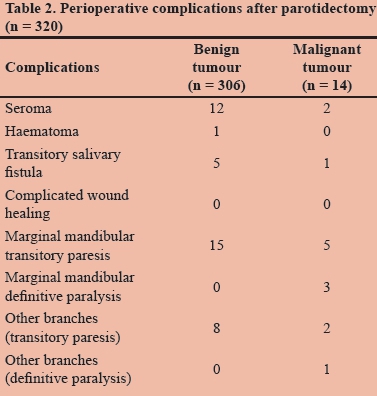
Fifteen cases of marginal mandibular transitory paresis and 12 cases of seroma were verified, and conservatively managed. Marginal mandibular definitive paralysis was observed in three malignant tumour cases. The rates of complications occurring in the patients are presented in Table 2.
Discussion
The parotid gland is divided into a superficial lobe (80% of the gland) and a deep lobe (20% of the gland) by the facial nerve, so complete anatomical separation does not exist. The close relation between the facial nerve and the parotid gland demands a special technique during surgery. Most often, parotid tumours are painless and slow growing. The pain relates to the inflammatory process or an aggressive tumour. Rapidly evolving facial nerve palsy4 relates to malignancy, the involvement of overlying skin, facial nerve dysfunction and the presence of associated lymphadenopathy in the neck,1 all of which indicate the likelihood of a malignant diagnosis.
The FNAB can be used selectively, or as a routine evaluation. There is still controversy about the role of preoperative FNAB. Some authors previously argued against its routine use, recommending that a cytological examination should be used selectively, that is, when the results will have a direct bearing on treatment. Circumstances when an operation might be avoided include the following:
- In the case of an elderly or medically unfit patient, who might be managed nonoperatively in the case of benign diagnosis.
- When it is unclear whether or not the mass is arising from the parotid gland.
- When evaluating a parapharyngeal mass (a diagnosis of malignancy might change the surgical approach).
- When a mass is clinically malignant, and facial nerve sacrifice might be necessary.
- When metastatic cutaneous malignancy is suspected (because the scope of the operation might be changed by the addition of concomitant neck dissection).1
The main reasons for performing FNAB are:
- When conducting preoperative planning and counselling: limited parotidectomy only may be required for a Warthin's tumour. A plan with regard to the type and extension of surgery and closer attention to tumour margins may be needed in the case of malignancy. Schwannoma patients should be warned of the high risk of facial palsy.
- If no parotid lumps are suspected: the tail of parotid lumps may be lymph nodes and branchial cysts.
- If the avoidance of surgery is preferred: this refers to, for example, benign and infectious lymphadenopathy in children, and benign tumours in unfit elderly patients.3
There was sensitivity of 62% and specificity of 98% for malignancy diagnosis in a series in which 153 cases of parotid neoplasms were included.5
Radiological imaging is crucial for the evaluation of advanced malignant disease involving the parotid gland. Ultrasound can be useful when needing to confirm the dimensions and/or anatomical location of a lump in the preauricular region.6 The depth of invasion into the parotid gland can be delineated using computed tomography and magnetic resonance imaging scans, which can also provide information on the degree of infiltration of the surrounding structures, such as the skin, facial nerves, external auditory canal and temporal bone. This enables a more accurate determination of the structures which require resection in order to achieve complete extirpation, and also facilitates preoperative consultation with the reconstructive team. In addition, radiological imaging facilitates clinical staging of the cervical neck.6
The surgeon's ability to assess frozen section results is very important. The surgical findings are the best guide for decisions.5 Performing enucleation, instead of superficial parotidectomy, is the most common cause of recurrence of parotid pleomorphic adenoma.7 However, there is no agreement in the medical literature on identification of the exact margin of parotid tissue to be resected in order to avoid recurrence.2
A superficial parotidectomy with conservation of the facial nerve is the policy for a malignant parotid tumour when it is limited to the superficial lobe. If facial nerve infiltration is confirmed preoperatively, or tumour infiltration is detected at the time of surgery, total parotidectomy with resection of the facial nerve is indicated.6 The neoplasms of the parotid gland can be treated, and the facial nerve spared when it is not involved. Its sacrifice is not always able to improve the survival rate. The removal of deep lobe parotid tumours from the parapharyngeal space is often difficult because of limited surgical access and the critical vascular and neurological structures nearby. Mandibulotomy, when necessary, is useful in improving wider visibility and control of the vascular bundle. However, it may cause damage to the inferior dental and lingual nerves.2
Total parotidectomy was associated with a significantly higher incidence of facial nerve dysfunction during the first postoperative period (61% at day 1, and 45% at month 1) than superficial parotidectomy (18% at day 1, and 11% at month 1)(p < 0.001) in a series of 131 patients. Close contact of the tumour with the facial nerve was found to have statistical causal relation with facial nerve weakness.8 Frey's syndrome and the impact of the sternocleidomastoid muscle flap in its prevention have been previously studied.9
Conclusion
Standardised parotidectomy is a safe operation, with a low rate of complications. FNAB accuracy is 99%.
Declaration
Financial support was not provided for this study.
REFERENCES
1. O'Brien CJ. Current management of benign parotid tumors - the role of limited superficial parotidectomy. Head Neck. 2003;25(11):946-952. [ Links ]
2. Obaid MA, Yusuf A. Surgical management of epithelial parotid tumours. J Coll Physicians Surg Pak. 2004;14(7):394-399. [ Links ]
3. Lim LH, Chao SS, Goh CH, et al. Parotid gland surgery: 4-year review of 118 cases in an Asian population. Head Neck. 2003;25(7):543-548. [ Links ]
4. Brandão LG, Magalhães RP, Silva GB, et al. Análise retrospectiva de 100 parotidectomias/parotidectomy: retrospective analysis of 100 cases. Rev Col Bras Cir. 1990;17(3):46-50. [ Links ]
5. Carvalho MB, Soares JMA, Rapoport A, et al. Perioperative frozen section examination in parotid gland tumors. São Paulo Med J. 1999;117(6):233-237. [ Links ]
6. Bova R, Saylor A, Coman WB. Parotidectomy: review of treatment and outcomes. ANZ J Surg. 2004;74(7):563-568. [ Links ]
7. Guntinas-Lichius O, Kick C, Klussmann JP, et al. Pleomorphic adenoma of the parotid gland: a 13-year experience of consequent management by lateral or total parotidectomy. Eur Arch Otorhinolaryngol. 2004;261(3):143-146. [ Links ]
8. Gaillard C, Périé S, Susini B, St Guily JL. Facial nerve dysfunction after parotidectomy: the role of local factors. Laryngoscope. 2005;115(2):287-291. [ Links ]
9. Queiroz Filho W, Dedivitis RA, Rapoport A, Guimarães AV Sternocleidomastoid muscle flap preventing Frey syndrome following parotidectomy. World J Surg. 2004;28(4):361-364. [ Links ]
 Correspondence:
Correspondence:
R Dedivitis
dedivitis.hns@uol.com.br














