Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.53 n.3-4 Cape Town Dec. 2015
GENERAL SURGERY
Validation of the mortality prediction equation for damage control surgery in an independent severe trauma population
N OshunI; T C HardcastleII
IGeneral Surgery, University of KwaZulu-Natal, Durban, South Africa
IITrauma Unit, Inkosi Albert Luthuli Central Hospital; University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: A prediction model was developed in Cape Town which utilised age, preoperative lowest pH and lowest core body temperature to derive an equation for the purpose of predicting mortality in damage control surgery. It was shown to reliably predict death despite damage control surgery. The equation derivation dataset and the validation set showed the equation to have 100% positive predictive value (PPV) for both datasets and 24% sensitivity. The aim of the study was to validate the prediction model in an independent dataset from a prospective trauma registry.
METHOD: Retrospective analysis of an ethics-approved prospectively collected database and electronic medical records was performed on trauma patients undergoing damage control surgery at the Inkosi Albert Luthuli Central Hospital, Durban, between 2007 and 2013. Age, lowest preoperative core body temperature and the pH of the patients were analysed using the previously derived equation. The output from the equation was then classified as a prediction of death, based on the obtained values, and then compared to the actual outcome of whether the patients survived or died.
RESULT: A total of 48 patient records were analysed in the study. Twenty-nine patients in the cohort died. The equation predicted mortality in only four cases, of whom three died and one survived (75% PPV and 10% sensitivity). The unexpected survivor reduced the PPV to 75%, compared to 100% PPV achieved in the original study.
CONCLUSION: The results of this study were inconsistent with those of the original study, and the 0.500 cut-off value used in the equation yielded PPV and sensitivity which were relatively non-clinically useful for the average patient in this cohort.
Severe trauma for which damage control surgery is required carries a high risk of mortality. There is a paucity of literature on the subject of mortality prediction in "damage control surgery". Aoki et al.1 analysed 174 parameters, and concluded that pH and worst partial thromboplastin time could be predictive of mortality. Kairinos et al. showed that the use of age, preoperative pH and preoperative core body temperature predicted mortality in damage control surgery in 2010.2 Kairinos3 analysed 30 variables, and concluded that the parameters with the highest predictability of mortality were age, pH and body temperature. They proposed a formula for mortality prediction.
Severe trauma patients consume enormous resources, blood and blood products, theatre time, sundries and intensive care unit (ICU) resources. Patients may require multiple operations, many days in the ICU, and still eventually die, usually with multiple organ dysfunction syndrome. A formula derived to predict survivability in these patients is a welcome development in view of the huge cost of managing these patients, together with a scarcity of resources in many areas.
In addition, such a formula, if it was able to reliably predict outcome, would be very useful in triaging patients in mass casualty situations to ensure that available resources were utilised by the most deserving patients.
The modern concept of abbreviated laparotomy was first described by Stone in 1983.4 The concept of "damage control" was introduced in 1993, and popularised by Rotondo and Schwab , using a three-phase approach.5 In 1998, Moore et al. extended the concept and described the five-stage approach.6
The aim of damage control surgery is to prevent severely injured patients from developing the "lethal triad" of hypothermia, coagulopathy and worsening acidosis, as this confers a dismal prognosis. Damage control surgery has succeeded in reducing the mortality associated with severe abdominal trauma from 90% to an average of 50%.2,5-7
A prediction model which utilised age, preoperative lowest pH and lowest core body temperature to derive an equation aimed at predicting mortality in damage control surgery was developed in Cape Town. This equation was shown to reliably predict death despite damage control surgery. Two studies had previously been carried out by the Cape Town group. The results from both the studies demonstrated 100% positive predictive value (PPV) and 25% and 24% sensitivity, respectively, across the two study cohorts.2,3
Aim
The aim of the current study was to compare and validate the Cape Town equation by using a different dataset of patients in the Durban severe trauma population, treated at Inkosi Albert Luthuli Central Hospital, Durban. The validation of the score by an institution outside the one in which the score was designed was expected to provide credibility to the equation in surgical practice.
Method
Retrospective analysis of a prospectively collected, ethics-approved database and electronic medical records (University of KwaZulu-Natal-BREC BE207-09) was performed on trauma patients undergoing damage control surgery at Inkosi Albert Luthuli Central Hospital, Durban, over a period of six years from 2007-2013. Basic demographic data were collated. Forty-eight patients who underwent damage control surgery were included in the study. Children aged < 13 years were excluded, in accordance with the criteria for the previous studies. Age, lowest preoperative core body temperature and the pH of the patients were analysed using the previously derived equation: X = age (0.012) - (0.707) pH - (0.032) temperature + 6.002, where "X" is the logit of the equation. Case records for the identified patients were analysed, and the parameters entered into the equation. The output from the equation was then classified as a predictor of death, that is X > 0.500, or likely survival, based on the obtained values, and then compared to the actual outcome of whether the patients survived or died. Laparotomy was considered to be damage control surgery:
- If the patient was physiologically unstable (a temperature < 35°C, a pH < 7.2, lactate > 5 mmol/l, or massive transfusion was utilised).
- Organ packing or temporary abdominal closure was required.
- When multiple sources of competing injuries were present.8
Results
The age of the 48 patients ranged from 14-65 years, with a median age of 30.5 years. All of the patients underwent damage control surgery. Nineteen other patients over that period underwent emergency non-damage control surgery laparotomy. The patients were admitted to Inkosi Albert Luthuli Central Hospital directly from the scene, and were operated on within the first two hours of admission. Of the 48 patients, there were 37 males (77%). Vehicular-related incidents included occupants, pedestrians and a motorbike collision, totalling 30 cases; gunshot wounds involving the abdomen afflicted 31 patients, three of the patients had stab wounds and one of the study participants fell from a height. Of the 48 patients, 29 died (60% overall mortality), i.e. 21 males (57% ) and 8 females (73%). Of these 29 deaths, 22 died in the first 24 hours, one in 48 hours, and one each in the second, third, fourth and fifth weeks post-injury. The median injury severity score (ISS) for all of the patients was 34 [interquartile range (IQR) 27-43]. The median ISS for the deceased patients was 38 (IQR 28-44), and for the survivors 32 (IQR 25-38). This result was statistically significant, with a p-value of 0.034. The arithmetic mean ISS for the survivors was 29, and for those who died, 39.
The equation predicted mortality in only four cases, of whom three died (75% PPV and 10% sensitivity). One of the subjects who had been predicted to be unsalvageable survived, which brought the PPV down to 75%, compared to 100% PPV recorded in the original study. The patient who survived was 65 years old, in contradiction of the dismal prognosis often assigned to advanced age. Twenty-six other patients, predicted to potentially survive, subsequently demised, leading to sensitivity of only 10%.
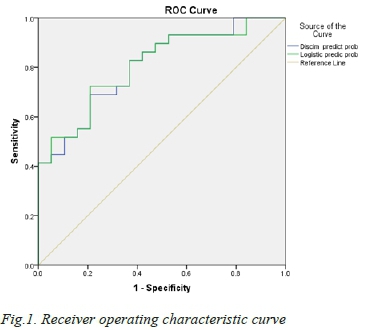
It was determined when assessing the validity of the equation, that the arbitrary value of 0.500 was the most appropriate value with which to determine nonsurvivability. This was established using logistic regression analysis, and it was validated as being the most appropriate in terms of being most predictive without compromising either the PPV or sensitivity (Figure 1). The area under the curve was 0.808, considered to be of significance and more sound than pure clinical judgement.
Discussion
Individually, the parameters analysed in this study hold mortality prediction value. Hypothermia on its own is a poor prognostic indicator in polytrauma.9 A core body temperature of less than 32°C invariably correlates with mortality of 100%.10 Every patient with a temperature of < 33°C died in this study, of whom there were four in total.
High mortality rates have been documented in patients with metabolic acidosis, who take 48-72 hours to clear lactate or correct the base deficit.7,10,11 Every patient with a pH of < 7 died in this study, of whom there were seven in total.
The age of patients undergoing damage control surgery is a significant mortality prediction variable, owing to the fact that physiological reserves diminish with age. However, individual levels of health differ, based on medical co-morbidities. Severe trauma in which damage control surgery was required in patients aged > 70 years is believed by some to result in inevitable mortality.12 The oldest patient in the current study was 65 years, and an unexpected survivor, which suggests that age alone is not an absolute predictor of futility. None of the patients in this study were aged > 70 years, so this variable could not be independently assessed. However, a number of severely injured older patients have been treated successfully at Inkosi Albert Luthuli Central Hospital without damage control surgery, and survived.
Although the total number of patients in this study was smaller than that in previous studies, the results are not consistent with those obtained in the original study in which there was 100% PPV and 25% sensitivity. There was one unexpected survivor (75% PPV) among the four predicted not to survive in this study, which indicated that one potentially salvageable patient (25%) could have died should the patient have been excluded from surgery. The sensitivity of 10% indicates that 90% of the patients who actually died had not been predicted to die. According to the equation only four patients in this cohort were predicted to die over the six-year study period. This indicates the low clinical value of this equation. It also demonstrates a negligible cost-saving benefit in the long run as the overall prediction of outcome was poor.
Although used routinely, a discrimination point of p 0.500, utilised to distinguish survivors from those who will die, is problematic. Patients with similar risks may be separated into different outcomes, and those with disparate risks may be included in the same category. For example, although mathematically correct, it is clinically impractical to believe that a patient with a probability of death of 0.490 would be markedly different from one with a probability of 0.510, yet the former would be predicted to survive, and the latter to die. Similarly, although both patients with probabilities of 0.050 and 0.490 would be predicted to survive, the risk would be substantially greater in the latter. Mathematically objective predictive systems assess average, and not individual, risk. Increasing the 0.500 cut-off value would increase the PPV of the equation, but would lessen the sensitivity. Reducing the cut-off point to below 0.500 would increase the sensitivity, but reduce the PPV. Either way, the clinical usefulness of the equation would be diminished. These factors also make the equation relatively clinically unhelpful for the average patient with high injury severity in need of damage control surgery. Further research is required to establish a more sensitive, and at the same time specific, equation.
Conclusion
The results of this study were not consistent with those obtained in the original two studies. A PPV of 75% and 10% sensitivity renders the equation clinically unhelpful in predicting mortality in our cohort who underwent damage control surgery for predefined indications, and is also not useful for cost-reduction purposes with respect to trauma patients.
REFERENCES
1. Aoki N, Wall MJ, Demsar J. Predictive model for survival at the conclusion of a damage control laparotomy. Am J Surg. 2000;180(6):540-545. [ Links ]
2. Kairinos N, Hayes PM, Nicol AJ, Kahn D. Avoiding futile damage control laparotomy. Injury. 2010;41(1):64-68. [ Links ]
3. Kairinos N, Nicol AJ, Timmermans J, Navsaria PH. Predicting mortality in damage control for major abdominal trauma. S Afr J Surg. 2010;48(1):6-9. [ Links ]
4. Schreiber MA. Damage control surgery. Crit Care Clin. 2004;20(1):101-118. [ Links ]
5. Dadhwal US, Pathak N. Damage control philosophy in polytrauma. medIND [homepage on the Internet]. [ Links ] 2010. c2015. Available from: http://medind.nic.in/maa/t10/i4/maat10i4p347.pdf
6. Moore EE, Burch JM, Franciose RJ, et al. Staged physiologic restoration and damage control surgery. World J Surg. 1998;22(12):1184-1191. [ Links ]
7. Jansen JO, Thomas R, Brooks A. Damage control resuscitation for patients with major trauma. Br Med J. 2009;338:b1778. [ Links ]
8. Hoey BA, Schwab CW. Damage control surgery. Scan J Surg. 2002;91(1):92-103. [ Links ]
9. Jaunoo SS, Harji DP. Damage control surgery. Int J Surg. 2009;7(2):110-113. [ Links ]
10. Jurkovich GJ, Greiser WB, Luterman A, Curreri PW. Hypothermia in trauma victims: an ominous predictor of survival. J Trauma. 1987;27(9):1019-1024. [ Links ]
11. Heinonen E, Hardcastle TC, Barle H, Muckart DJJ. Lactate clearance predicts outcome after major trauma. African Journal of Emergency Medicine [homepage on the Internet]. [ Links ] 2014. c2015. Available from: http://www.afjem.org/article/S2211-419X(14)00015-9/abstract
12. Morris JA, Eddy VA, Blinman TA, et al. The staged celiotomy for trauma issues in unpacking and reconstruction. Annal Surg. 1993;217(5):576-586. [ Links ]
 Correspondence:
Correspondence:
N Oshun
nsoshun@gmail.com














