Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.53 n.3-4 Cape Town Dec. 2015
GENERAL SURGERY
The effect of opioids on field block for hernia repair: A study comparing pethidine with a placebo
M R AdjeiI; T S LetsaII; E MahamaIII; S Owusu-AgyeiIII
ITain District Hospital, Nsawkaw, BrongAhafo Region (BAR); Ghana
IIRegional Health Directorate, Sunyani, BAR; Ghana
IIIKintampo Health Research Centre, Kintampo, BAR; Ghana
ABSTRACT
BACKGROUND: Intramuscular (IM) pethidine injection is used as pre-analgesia (pre-medication) in hernia repair under local anaesthesia in some district hospitals. We evaluated the relevance of this practice in a facility based study at one of the district hospitals in Ghana.
METHOD: One hundred and twenty patients above 10 years of age with a mean age of approximately 49 years diagnosed as having inguinal hernias of different sizes were recruited into the study. Each group of 60 patients was randomly selected. A maximum of 50 ml 1% lignocaine plus 2 ml (100 mg) of pethidine was used in group A and 50 ml 1% lignocaine plus 2 ml of sterile water in group B. A score ranging from 0 to 3 was assigned at the end of each surgery depending on the degree of pain experienced.
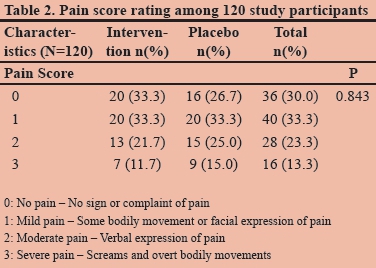
RESULTS: 33.3%, 33.3%, 21.7% and 11.7% of patients in group A scored 0, 1, 2, and 3 respectively in pain perception while 26.7%, 33.3%, 25% and 15.0% were the scores in group B. None of the patients in group B experienced an adverse effect to any of the agents used. 2% and 5% in group A experienced nausea and generalized pruritus respectively. Post-operation condition was satisfactory and all patients were discharged the same day.
DISCUSSIONS AND CONCLUSION: There was no significant difference in pain perception when IM pethidine is combined with local infiltration compared with local infiltration plus sterile water for herniorrhaphy. Good and adequate local infiltration is enough for the repair of simple hernias as the addition of pethidine does not give any significant analgesia but increases the chance of patient developing complications.
Hernias are one of the most common surgical cases seen at the outpatient departments (OPDs) of district hospitals in Ghana and constitute at least 24% of all surgeries carried out at a typical district hospital.1 Spinal and general anaesthesia are associated with more complications and relatively long hospitalization after surgery.2 Local anaesthesia is relatively economical, associated with few complications and patient can be discharged the same day after surgery.
Clinics and hospitals with few beds have found local anaesthesia ideal for herniorrhaphy and the same can be said for those without trained anaesthetist. It is however important to monitor the vital signs intraoperatively and with adrenaline handy in case of anaphylaxis.
Pethidine is used for treatment of moderate to severe pain and delivered as a hydrochloride salt in tablets, as a syrup or by intramuscular, subcutaneous or intravenous injection.3,4,5 Some surgeons prefer to add IM pethidine as an adjunct to local infiltration for hernia repair. It is anticipated that the addition of pethidine improves the anaesthetic effect desired by the surgeon due to its strong analgesic and sedating properties.
Elhakim et al6 found out that inclusion of low dose pethidine in lidocaine (lignocaine) for tonsillar infiltration improves pain relief following tonsillectomy in children. Pethidine exerts a local anaesthetic effect on peripheral nerves in vivo.4,6 Although this assertion was corroborated by Nikandish et al, it does not affect the dynamic pain state in the first 24 hours after tonsillectomy.7
A search prior to carrying out this study indicated that there had been no publication on IM pethidine use to improve the anaesthetic effect produced by local infiltration with lignocaine for hernia repair. This study was therefore carried out in order to establish if this addition improves the anaesthetic effect during hernia repair or not.
Materials and methods
All patients requiring hernia repair between January 2012 and December 2012 at the Tain district hospital were enrolled in to this study following an individual informed consenting process. All patients were given study identities with the numbers provided serially; the order based on the dates they were booked for surgery. The patients registered with odd numbers were randomised into group A while those registered with even numbers were randomized into group B. Basic demographic information of each patient was recorded in study files.
The standard practice in hernia repair under local anaesthesia is local infiltration only. Although we were evaluating whether pethidine improves the anaesthetic effect, the IM sterile water was meant to blind the patients in group B so that they feel equally treated as group A.
Each patient was prepared as for an elective surgery and the differentiating factor was that those in group A were treated with 2 ml (100 mg) pethidine while those in group B were treated with 2 ml sterile water, both intramuscularly prior to making the groin incision. A maximum of 50 ml of 1% plain lidocaine was infiltrated in the following fashion:8
1. Subdermal infiltration: Approximately 5 ml of 1% plain lidocaine was infiltrated along the line of the incision using a 2 inch 25 gauge needle inserted into the subdermic tissue parallel with the surface of the skin. Infiltration continues as the needle advances.
2. Intradermal injection: The needle previously inserted into the subdermal plane was slowly withdrawn until the tip of the needle reaches the intradermal level. Without extracting the needle completely a wheal was formed by slowly injecting about 3 ml of lidocaine.
3. Deep subcutaneous injection: 10 ml of 1% lidocaine was injected deep into the subcutaneous adipose tissue by vertical insertion of the needle 2 cm apart.
4. Subfascial infiltration: Approximately 8-10 ml of 1% lidocaine was injected immediately underneath the aponeurosis of the external oblique through a window created in the subcutaneous adipose tissue at the lateral corner of the incision.
5. Pubic tubercle and hernia sac injection: About 3 ml of 1% lidocaine was infiltrated at the level of the pubic tubercle around the neck and inside the indirect hernia sac.
The surgery was then performed occasionally engaging the patient in a conversation while monitoring the blood pressure (BP) and pulse of the patient every quarter of an hour. The average duration of each surgery was 60 minutes. The anaesthetist and the patient gave independent assessment of the pain which were scored as (0): No pain - No sign or complaint of pain; (1): Mild pain - Some bodily movement or facial expression of pain; (2): Moderate pain - Verbal expression of pain; (3): Severe pain - Screams and overt bodily movements. The highest score was taken as the patient's pain score.
Results
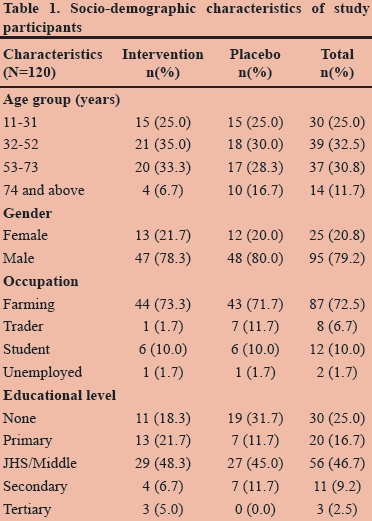
In total, one hundred and twenty patients with reducible inguinal hernias participated in this study. The mean age of the patient population requiring surgery was 49 years; they were mostly farmers residing in the Tain district where the hospital is located. Table 1 gives a summary of the population characteristics.
As shown in Table 2, 33.3% of patients in group A had complete anaesthesia during the procedure as compared with 26.7% of patients in group B. The remaining 66.7% of patients in group A and 73.3% of patients in group B had incomplete anaesthesia (Table 2). There was no significant difference in the variations in pulse and BP recorded during the procedures. Patients who had a pain score of 3 were given general anaesthesia that enabled them to complete the procedure. Though none of the patients in group B experienced adverse drug reactions, 2% and 5% respectively in group A experienced nausea and generalized pruritus presumably related to pethidine. All patients were ambulant within 3 hours of completion of surgery and were put on normal diet. A seven-day follow up of participants was uneventful.
To ascertain whether the results in both groups did not differ significantly, statistical analysis was carried out and the p-values compared as in Table 3.
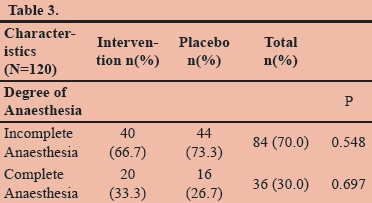
There was no significant difference in the proportion of patients achieving complete anaesthesia in the intervention group (A) compared to those in the placebo group (B) (p = 0.697). Similarly, there was no significant statistical difference in the proportion of patients who had incomplete anaesthesia in the intervention group compared with those in the placebo group as reported in Table 3.
Discussion
It is evident from the results that there were no significant differences in the pain scores recorded in group A who were treated with 2 ml (100 mg) pethidine compared with those in group B treated with 2 ml sterile water.
The pain scores were affected by the level of anxiety of the patient prior to the procedure. It was observed that patients who have had previous surgical operations under general anaesthesia were more anxious than their counterparts without and this affected their score. Of the participants who experienced different degrees of pain in both groups, majority felt it during manipulation of the hernia sac. Most of the participants with long-standing or huge hernias also had grade 3 pain rating.
The two treatment arms were equivalent therefore the combination is not recommended as it is an additional cost and the side effect of the opioid cannot be overemphasized.
Like other opioids, pethidine has the potential to cause physical dependency or addiction. It may be more likely to be abused than other prescription opioids, perhaps because of its rapid onset of action. Pethidine is associated with more euphoria, difficulty concentrating, confusion and impaired psychomotor and cognitive performance when administered to healthy volunteers.5 The side effect unique to pethidine i.e. serotonin syndrome, seizures, delirium, dysphoria and tremours are primarily or entirely due to the action of its metabolite norpethidine. Norpethidine is toxic and has convulsant and hallucinogenic effect.9,10 The toxic effect cannot be countered with opioid receptor antagonist. The metabolite is conjugated with glucuronic acid and exceptionally toxic to patients with liver and kidney disease as well as the elderly.
The success of local anaesthesia requires proper technique of administration and gentle manipulation. Several anaesthetic agents are currently available but the choice for this study was plain 1% lidocaine. In practice this can be improved by adding 0.5% bupivacaine in a 50:50 mixture. The therapeutic dose of lignocaine is 300 mg in the plain form and 175 mg for plain bupivacaine.
Lignocaine provides rapid onset and bupivacaine results in a longer duration of local anaesthesia. Anaesthetic duration can be prolonged further by addition of epinephrine but this may produce severe prolong hypertension in patients receiving monoamine oxidase inhibitors or tricyclic antidepressants.8
The use of two different anaesthetic agents decreases the likelihood of exceeding the therapeutic maximum dose of each agent and this is particularly useful in the case of simultaneous bilateral inguinal hernia repair.
Acknowledgements
The authors are grateful to the entire theatre and record staff of Tain District Hospital for their immense support during the study. We are very grateful to the patients who consented to be part of this study and to Kintampo Health Research Centre Institutional Ethics Committee for approving this study.
REFERENCE
1. Abantanga FA, Hesse AJ, Sory E, Osen H, Choo S, Abdulla F, et al. Policies for Improving Access to Quality and Essential Surgical Care at District Hospitals in Ghana. Postgraduate Medical Journal of Ghana,2012:1(1): 1-6 [ Links ]
2. Sanjay P and Woodward A. Inguinal Hernia Repair: Local or General Anaesthesia. Annals the Royal College of Surgeons, England, 2007; 89 (5): 497-503. [http//dx.doi.org/10.1308/003588407X202056] [PMID:2048598] [ Links ]
3. Kaiko RF, Foley KM, Grabinski PY et al (February 1983). Central Nervous System Excitatory Effects of Meperidine in Cancer Patients. Annals of Neurology (Wiley Interscience) 1983; 13 (2): 180-185.[http://dx.doi.org/10.1002/ana.410130213] [ PMID: 6187275] [ Links ]
4. Wagner, Larry E., II; Michael Eaton, Salas S. Sabnis, Kevin J. Gingrich (November 1999). "Meperidine and Lidocaine Block of Recombinant Voltage-Dependent Na+ Channels: Evidence that Meperidine is a Local Anaesthetic". Anaesthesiology (Lippincott Williams & Wilkins) 91 (5): 1481-1490. [ Links ]
5. Walker DJ, Zacny JP. Subjective, Psychomotor, and Physiological Effects of Cumulative Doses of Opioid μ Agonists in Healthy Volunteers. The Journal of Pharmacology andExperimental Therapeutics (American Society for Pharmacology and Experimental Therapeutics) 1999 289 (3): 1454-1464. [ Links ][PMID :10336539]
6. Elhakim M, Abdul Salam AY, Eid A, Kaschaf N, Mostafa BE "Inclusion of Pethidine in Lidocaine for Tonsillar Infiltration in Children" Acta Anaesthesiol Scand. 1997 41(2): 214-7 [PMID:9062602] [ Links ]
7. Nikandish R, Maghsoodi B, Khadami S, Motazedian S., Kaboodkhani R. Peritonsillar [ Links ]
8. Infiltration with Bupivacaine and Pethidine for Relief of Post-tonsillectomy Pain: A Randomized Double Blind Study. Anaesthesia 2008 63 (1):20-25 [PMID:18086066] [ Links ]
9. Amid PK, Shulman AG, Lichtenstein IL. Local Anesthesia for Hernia Repair, Step-by-Step Procedure. Annals of Surgery 1994 220(6): 735-737 [PMID:1234473] [ Links ]
10. Demerol: Is It the Best Analgesic? (PDF). Pennsylvania Patient Safety Reporting Service Patient Safety Advisory (Pennsylvania Patient Safety Authority) 2006 3 (2). [ Links ]
11. Latta KS, Brian G, Barkin RL. Meperidine: A Critical Review. American Journal of Therapeutics (Lippincott Williams & Wilkins) 2002 9 (1): 53-68.[http://dx.doi.org/10.1097/00045391-200201000-00010][ PMID: 11782820 [ Links ]
 Correspondence:
Correspondence:
Michael Adjei Rockson
bonnahk@yahoo.com














