Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.53 no.2 Cape Town jul. 2015
http://dx.doi.org/10.7196/SAJSNEW.7855
VASCULAR SURGERY
Management of chronic exertional compartment syndrome
J IslamI; JV RobbsII
IMBBS, DA (SA), FCS (SA), Cert Vasc Surg (SA), MMed Sci; Department of Vascular Surgery, Grey's Hospital, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IIMB ChB, ChM, FCS (SA), FRCS (Ed), FRCPS; Professor Emeritus, University of KwaZulu-Natal; Private practice at Entabeni Hospital, Durban, South Africa
ABSTRACT
BACKGROUND: Post-exercise pain is an uncommon symptom in young, healthy adults. Rest and avoidance of exercise are frequently ineffective and poorly accepted by young, active and otherwise healthy individuals.
METHODS: A total of 123 patients with extremity muscle pain, swelling and paraesthesia during the last 10 years were evaluated from a prospective database with compartment pressures and selectively evaluated with Doppler ultrasound and angiography.
RESULTS: Patients were young (average 28 years) with long duration of symptoms (average 3.5 years), affecting both upper limbs (3), and lower limbs (120), and 80% were bilateral. Eighty-six were male (70%). All of them were taking part either in active sports or exercise programmes, mostly athletics (49%). Common symptoms were isolated muscle pain in the anterolateral compartments in all patients, paraesthesia in 15% and swelling in 10%. Post-exercise mean compartment pressure was 61 mmHg (normal <30 mmHg). Modified open fasciotomies were performed by lateral and medial incisions in lower limbs and by a single incision in upper limbs. Minor complications occurred in 11% of patients. Full relief of symptoms occurred in 90%, 7% had some improvement of symptoms, and treatment failure occurred in 3% of patients.
CONCLUSION: Chronic exertional compartment syndrome is underdiagnosed and should be considered as a potential cause for post-exercise pain in young individuals, and should be treated surgically. Measurement of compartment pressure is important in order to confirm the diagnosis. Open fasciotomy is safe and effective and should be considered as the preferred surgical procedure.
Post-exercise pain is an uncommon symptom in young, healthy adults. Chronic leg pain can be a challenging diagnostic problem, especially in the young professional or recreational athlete. Chronic exertional compartment syndrome (CECS) is the most common cause of exercise-induced leg pain; other causes include medial tibial stress syndrome, stress fracture, nerve entrapment, vascular claudication, and popliteal artery entrapment syndrome.[1] Mavor[2] published the first description of CECS in 1956. French and Price[3] conclusively made the diagnosis of CECS by measuring intracompartment pressure, and Reneman[4] described multiple patients with CECS confirmed by pressure measurements. CECS of the lower limbs is well known, but it is rare in the upper limbs and only a few case reports have been published.[5,6]
Conservative management includes activity modification, rest and massage, stretching and non-steroidal anti-inflammatories. There is limited conclusive evidence in favour of any of these conservative treatments in returning the patients to their prior level of function. Activity modification and rest are not well accepted by young athletes. If conservative management fails, surgical intervention is the next best modality. There are many review articles[7-9] and case reports[10,11] in the literature on CECS, but only a few institutional reviews.[12-14] The objective of this study was to evaluate our own experience in the diagnosis and management of CECS.
Methods
Between January 2004 and December 2013, all patients referred from the sports medicine physicians and presented to a single practice at Entabeni Hospital, Durban, South Africa with extremity pain, swelling and paraesthesia were culled from a prospectively maintained database. One hundred and twenty three (123) patients were evaluated. All of them had intracompartment pressures measured and these were considered high if >30 mmHg 1 minute post exercise. Doppler ultrasound and angiography were considered only in selected cases, where compartment pressures were inconclusive or vascular disease could not be ruled out. Doppler ultrasound was done before and immediately after exercise, and the pre- and post-exercise test results were compared. The pre-exercise flow velocity was normal in all the patients, but the post-exercise flow velocity was low or dampened in most patients, which was suggestive of CECS. However, there are no consistent criteria that are pathognomonic for this diagnosis.
Technique
Modified open fasciotomy was performed under general anaesthesia in all lower limb and upper limb cases.
In the lower limb, the anterior, lateral and superficial posterior compartments were released via a lateral incision, and the deep posterior compartment is accessed using a medial incision. A 10 cm longitudinal lateral incision was made over the fibular shaft in the mid portion of the leg. Complete longitudinal releases of all three compartments were accomplished by three separate subcutaneous incisions under direct vision. The scissor is pushed proximally in the direction of the patella and distally toward the great toe; care must be taken to preserve the superficial peroneal nerve. Common peroneal nerve lies between the tendon of the biceps femoris and lateral head of the gastrocnemius muscle, winds around the neck of the fibula, and divides beneath the muscle into the superficial fibular nerve (superficial peroneal nerve) and deep fibular nerve (deep peroneal nerve). The superficial peroneal nerve travels in the lateral compartment and supplies the peroneus longus and brevis muscles, pierces the deep fascia at the lower third of the leg, and finally divides into two cutaneous branches to the lower leg and dorsum of the foot. These sensory nerves are prone to injury.
A 5 cm medial incision was made over the medial side of the distal third of the leg posterior to the tibial margin. Care should be taken to preserve the saphenous nerve and vein in this area. The deep posterior compartment was released distally and then proximally under the soleus bridge.
In the upper limb, a single 10 cm longitudinal incision was made on the medial side of the volar aspect over the pronator teres muscle, distal to the inferomedial border of the cubital fossa. The bicipital aponeurosis was released longitudinally, trying to preserve the branches of the medial cutaneous nerve of the forearm. The fascia was released from the elbow proximally, including the fascia over the pronator teres muscle, to the musculotendinous junction distally. The release of fascia was done under direct vision and this can be felt subcutaneously with the finger. Both the superficial and deep volar compartments were released through the same incision.
Physical therapy was started 1 - 2 weeks after surgery and all athletes could return to full activity in 6 - 8 weeks if they were symptom free. The patients were followed up after discharge at 1 month, 6 months and 12 months.
Results
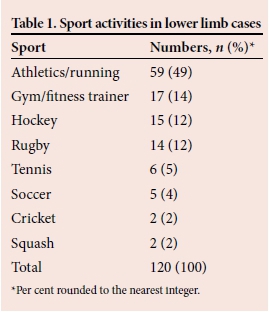
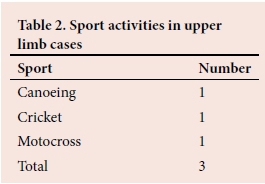
Between January 2004 and December 2013 (10 years), 221 limbs in 123 patients were treated by fasciotomy. The average age of the patients was 28 (range 18 - 53) years; the average duration of symptoms was 3.5 (range 1 - 6) years. Upper limbs were affected in three patients (2.5%) and lower limbs in 120 (97.5%) patients. Among the lower limbs, 96 were bilateral (80%) while two were bilateral in upper limbs. Eighty-six patients were male (70%). All of them were taking part either in active sports or exercise programmes (Table 1), and most of them were athletes/runners (49%). Sports activities involved among those with upper limb problem are shown in Table 2. In the lower limbs (n=216) common symptoms were isolated muscle pain in the anterolateral compartments in all patients, paraesthesia of the dorsum of the foot in 33 (15%) and swelling of the leg in 22 (10%).
One minute post-exercise mean compartment pressure was 61 (range 36 - 109) mmHg. Doppler ultrasound showed abnormal flow after exercise in 50 patients (40%). To exclude vascular disease, angiogram was done in two patients, one was normal and the other one showed femoral artery occlusive disease.
The most commonly affected lower limb muscle groups were anterolateral 163 (74%), deep posterior 36 (16%) and superficial posterior 22 (10%) compartments. Superficial and deep volar compartment muscles were affected in all upper limb cases.
Minor complications occurred in 14 patients (11%) with lower limb decompression. These included superficial wound infections (2), wound haematoma (4), and hypo-aesthesia of the foot due to nerve injury (8). There was no death in the series. One patient had residual symptoms post decompression and needed redo surgery.
Full relief of symptoms occurred in 111 (90%) patients, who returned to normal activity. Eight patients (7%) with initial hypo-aesthesia eventually resolved within 3 months. Twelve patients (10%) could not return to normal activity; seven had some improvement of symptoms, and one patient eventually needed stenting of the superficial femoral artery due to occlusive disease, and thereafter improved.
Discussion
Although uncommon, CECS should be included in the differential diagnosis of atypical claudication, as surgical intervention is the best way to achieve durable symptomatic relief in most patients.[13] The pathophysiology of CECS is not fully understood but there is general agreement that abnormally raised compartment pressures during exercise lead to vascular occlusion, ischaemic pain and possibly muscle damage.[15] During strenuous exercise, an increase of up to 20% may occur in muscle volume and weight due to the increased blood flow and oedema.[8] In addition, the normal muscular hypertrophy that occurs over time with chronic exercise reduces the reserve volume available within the fascial compartment. Chronic fascial thickening may also contribute to compartment noncompliance.[16]
The diagnosis of CECS requires detailed clinical history and is confirmed by measuring compartment pressure. One or more of the following criteria is consistent with the diagnosis of CECS, namely pre-exercise pressure of >15 mmHg, 1 minute post-exercise pressure >30 mmHg, and 5 minute post-exercise pressure of >20 mmHg.[7] There are evolving tests that may be used in the future to assess CECS, such as magnetic resonance imaging, infrared spectroscopy and thallium 201.[9]
Intracompartment pressure measurement remains the gold standard in investigation with 77% sensitivity and 85% specificity with the cut-off point at 35 mmHg.[17] One minute post-exercise mean intracompartment pressure in our series was 61 mmHg and we made the diagnosis on clinical history and pressure readings.
The incidence of CECS in the general population is unclear, and has been reported as between 14% and 27%.[18] The average age of our patients was 28 years, 70% of them were male, 80% of cases were bilateral, and in 74% of cases anterolateral compartments were involved, which is in accordance with the literature.[8,13,14] Though muscle herniation through defects in fascia can be palpated in 40 - 60% of patients with the syndrome, there were none identified in the present series.[19] All of our patients were either professional or recreational athletes.
The non-surgical approach involves modification of activity, appropriate conditioning and significant curtailment of physical activity, which is rarely acceptable to the individuals.[19] The surgical solution is decompression fasciotomy. In this group of patients, all four compartments were released in the lower limbs, and superficial and deep volar compartments in the upper limbs.
The most commonly performed surgical procedure is a subcutaneous fasciotomy via a 4 - 5 cm incision, and fasciectomy is done for recurrence after fasciotomy. Our preference is modified open fasciotomy for both the lower and upper limbs. We did not perform any fasciectomies. Open fasciotomy has fewer postoperative complications, fewer recurrences than subcutaneous fasciotomy, and there is no difference in the time to full recovery.[12] In addition to formal open fasciotomy, endoscopic techniques for fasciotomy have recently been described.[20,21] Though the endoscopic technique is less invasive in terms of tissue damage, and possibly has a quicker recovery time, there are no long-term results to determine their efficacy.
There is little in the literature concerning CECS affecting the upper limb, and most papers comprise either a single case report or small case series.[22,23] CECS of the upper limb mostly affects the volar compartment of the forearm, and rarely the dorsal compartment. The three upper limb cases in this series include a motocross rider, a rower and a professional cricketer. All three patients had volar compartments decompressed with full relief of symptoms.
Decompressive fasciotomy for CECS enjoys high success rates as reported in the literature (81 - 100%) for the anterior compartment.[8,17] Outcomes after surgical treatment of CECS have shown that patients do better after anterior and lateral compartment fasciotomies than patients who undergo single deep posterior compartment decompression. Full relief of symptoms occurred in 111 (90%) of our patients. Eight patients (7%) had some improvement of symptoms though could not return to previous activities, and there was treatment failure in four patients (3%). The exact cause of treatment failure could not be established. All of these four patients had repeat intracompartment pressure tests done, which were within normal limits, and the patients declined repeat surgery.
Complications of surgical treatment vary from 11% - 15%.[8,9,14] Complications include haemorrhage, infection, nerve damage, lymphocoele, vascular injury, deep vein thrombosis and recurrences. There were minor complications in 11% of our patients.
Conclusions
Chronic exertional compartment syndrome is underdiagnosed, should be considered as a potential cause for post-exercise pain in young individuals and should be treated surgically. Measurement of compartment pressure is important in order to confirm the diagnosis. Open fasciotomy is safe and effective and should be considered as the preferred surgical procedure.
REFERENCES
1. Brewer RB, Gregory AJ. Chronic lower leg pain in athletes: A guide for the differential diagnosis, evaluation, and treatment. Sports Health 2012;4(2):121-127. [http://dx.doi.org/10.1177/1941738111426115] [ Links ]
2. Mavor GE. The anterior tibial syndrome. J Bone Joint Surg (Br) 1956;38B(2):513-517. [ Links ]
3. French EB, Price WH. Anterior tibial pain. Br Med J 1962;2(5315):1290-1296. [ Links ]
4. Reneman RS. The anterior and the lateral compartmental syndrome of the leg due to intensive use of muscles. Clin Orthop Relat Res 1975;113:69-80. [ Links ]
5. Goubier JN, Saillant G. Chronic compartment syndrome of the forearm in competitive motor cyclists: A report of two cases. Br J Sports Med 2003;37(5):452-454. [http://dx.doi.org/10.1136/bjsm.37.5.452] [ Links ]
6. O'heireamhoin S, Baker JF, Neligan M. Chronic exertional compartment syndrome of the forearm in an elite rower. Case Rep Orthop 2011;2011:2 pages. [http://dx.doi.org/10.1155/2011/497854] [ Links ]
7. Pedowitz RA, Gershuni DH. Pathophysiology and diagnosis of chronic compartment syndrome. Oper Tech Sports Med 1995;3(4):230-236. [http://dx.doi.org/10.1016/S1060-1872(95)80021-2] [ Links ]
8. Bong MR, Polatsch DB, Jazrawi LM, Rokito AS. Chronic exertional compartment syndrome: Diagnosis and management. Bull Hosp Jt Dis 2005;62(3-4):77-84. [ Links ]
9. Tucker AK. Chronic exertional compartment syndrome of the leg. Curr Rev Musculoskelet Med 2010;3(1-4):32-37. [http://dx.doi.org/10.1007/s12178-010-9065-4] [ Links ]
10. Brown JS, Wheeler PC, Boyd KT, Barnes MR, Allen MJ. Chronic exertional compartment syndrome of the forearm: A case series of 12 patients treated with fasciotomy. J Hand Surg Eur Vol 2011;36(5):413-419. [http://dx.doi.org/10.1177/1753193410397900] [ Links ]
11. Snowden J, Becker JA, Brosky JA, Hazle C. Chronic leg pain in a division II field hockey player: A case report. Int J Sports Phys Ther 2014;9(1):125-134. [ Links ]
12. Turnipseed WD. Diagnosis and management of chronic compartment syndrome. Surgery 2002;132(4):613-619. [http://dx.doi.org/10.1067/msy.2002.128608] [ Links ]
13. Turnipseed WD. Clinical review of patients treated for atypical claudication: A 28-year experience. J Vasc Surg 2004;40(1):79-85. [http://dx.doi.org/10.1016/j.jvs.2004.02.034] [ Links ]
14. Waterman BR, Laughlin M, Kilcoyne K, Cameron KL, Owens BD. Surgical treatment of chronic exertional compartment syndrome. J Bone Joint Surg Am 2013;95(7):592-596. [http://dx.doi.org/10.2106/JBJS.L.00481] [ Links ]
15. Birtles DB, Rayson MP, Jones DA, et al. Effect of eccentric exercise on patients with chronic exertional compartment syndrome. Eur J Appl Physiol 2003;88(6):565-571. [http://dx.doi.org/10.1007/s00421-002-0740-z] [ Links ]
16. Detmer DE, Sharpe K, Sufit RL, Girdley FM. Chronic compartment syndrome: Diagnosis, management, and outcomes. Am J Sports Med 1985;13(3):162-170. [ Links ]
17. Zeineh N, Ardolino A, O'Connor D. Specialised chronic compartment measurement clinic in a district general hospital: Is it worthwhile? Ann R Coll Surg Engl 2009;91(6):505-508. [http://dx.doi.org/10.1308/003588409X432301] [ Links ]
18. Baltopoulos P, Papadakou E, Tsironi M, Karagounis P, Prionas G. Pre, during, and post exercise anterior tibial compartment pressure in long distance runners. J Sports Sci Med 2008;7(1):96-100. [ Links ]
19. Mubarak SJ. Surgical management of chronic compartment syndrome of the leg. Oper Tech Sports Med 1995;3(4):259-266. [ Links ]
20. Kitajima I, Tachibana S, Hirota Y, Nakamichi K, Miura K. One-portal technique of endoscopic fasciotomy: Chronic compartment syndrome of the lower leg. Arthrosocpy 2001;17(8):33. [http://dx.doi.org/10.1053/jars.2001.25261] [ Links ]
21. Knight JR, Daniels M, Robertson W. Endoscopic compartment release for chronic exertional compartment syndrome. Arthrosc Techn 2013;2(2):e187-e190. [http://dx.doi.org/10.1016/j.eats.2013.02.002] [ Links ]
22. Zandi H, Bell S. Results of compartment decompression in chronic forearm compartment syndrome: Six case presentations. Br J Sports Med 2005;39(9):e35. [http://dx.doi.org/10.1136/bjsm.2004.012518] [ Links ]
23. Volcke P, Kirby JH, Viviers PL, Viljoen JT. Chronic exertional compartment syndrome in the forearm of a rower. S Afr J SM 2014;26(2):62-63. [http://dx.doi.org/10.7196/SAJSM.547] [ Links ]
 Correspondence:
Correspondence:
J Islam
islam@telkomsa.net














