Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.53 n.1 Cape Town Mar. 2015
http://dx.doi.org/10.7196/SAJS.2407
VASCULAR SURGERY
Lessons learned from the endovascular management of blunt thoracic aortic injuries: A single-centre experience
J PillaiI; C YaziciogluII; T MonarengIII; T B RangakaIV; R JayakrishnanV; M G VellerVI
IBSc, MB BCh, FCS, CVS; Division of Vascular Surgery, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIBSc, BHSc (Hons); Division of Vascular Surgery, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIBDS, MB BCh, FCS; Division of Vascular Surgery, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVMB BCh, MMed; Division of Vascular Surgery, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VMBBS, HDip Surg, FCS; Division of Vascular Surgery, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIMB BCh, FCS, MMed; Division of Vascular Surgery, Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Blunt thoracic aortic injuries (BTAIs) remain a leading cause of death after blunt trauma. In severe injuries, thoracic endovascular aortic repair (TEVAR) has provided a less invasive alternative to conventional open repair.
OBJECTIVE: To report the TEVAR-related complications and uncertainties in patients who presented with traumatic pseudoaneurysms (grade III BTAI).
METHODS: From April 2004 to February 2012, 55 patients (42 male, mean age 34.7 years) with severe BTAI were treated with stent grafts. Computed tomography (CT) was used to diagnose the injuries, and follow-up scans were planned at 6 and 12 months. We report the complications and the technical uncertainties related to the procedure.
RESULTS: Successful sealing of the injury sites was achieved in all patients, either with a thoracic stent graft (53/55) or infrarenal aortic aneurysm extender cuffs (2/55). During hospitalisation, 13 patients died after TEVAR (mean 14 days). Procedure-related complications included left common carotid artery coverage (1/55), ischaemic left leg (1/55) and graft collapse (1/55). The procedure-related uncertainties included excessive graft oversizing (15/55), poor graft apposition to the inner curve of the aorta (19/55) and left subclavian artery coverage (24/55).
CONCLUSION: Stent grafts appear safe and effective in treating pseudoaneurysms caused by BTAI. However, they are likely to be associated with long-term complications and monitoring strategies of >30 years may be necessary.
Recent reports suggest that endovascular therapy is safe and effective for the treatment of pseudo-aneurysms caused by blunt traumatic aorta injury (BTAI).[1-6] Although the numbers of patients in these reports are small, technical success approaches 100% and procedure-related mortality and complications are reported to be low.[1,2,5,7,8] This is compared with the perioperative mortality of open surgery, which is reported to be 15 - 71% and is influenced by the haemodynamic stability of the patient and the severity of coexisting injuries.[2-4,6,9] Thoracic endovascular aortic repair (TEVAR) is therefore preferred in trauma centres where appropriate facilities and expertise exist. However, this complex procedure often has to be performed as an emergency in unstable patients with challenging anatomy. TEVAR-related complications may affect mortality and morbidity.
The objective of this study was to evaluate the limitations and potential adverse effects related to the endovascular management of pseudoaneurysms due to BTAI.
Methods
From April 2004 to February 2012, 55 patients (42 male, mean age 34.7 years) with traumatic pseudoaneurysms caused by blunt trauma to the thoracic aorta were treated with endovascular stent grafts in the Charlotte Maxeke Johannesburg Academic Hospital Vascular Unit. Data were collected prospectively. Only pseudoaneurysms that were identified with computed tomography (CT) were included.
Of the 55 patients, 45 were involved in motor vehicle accidents (MVAs), 8 in motor bike accidents and 2 fell from a height. The preoperative CT scans were used to assess aortic arch anatomy and assisted in stent graft measurement planning. The injuries were repaired with 53 thoracic endografts (38 GORE TAG Thoracic Endoprosthesis, W L Gore and Associates, USA; 15 Medtronic Vascular Talent Thoracic Stent Grafts, Medtronic Vascular, USA) and 5 EVAR extender cuffs (2 Excluder AAA Endoprosthesis Extender Cuffs, W L Gore and Associates, USA; 3 Vascutek Anaconda Extender Cuffs, Terumo Company, UK). The five extender cuffs were used in two patients. Procedures were performed either in the operating theatre (9/55) or an interventional angiosuite using standard endovascular protocols. Follow-up CT scans were scheduled at 6 months, 12 months and annually thereafter. Data were collected from the measurement planning CT scan, from the intraoperative angiogram and the follow-up CT scan. Procedure-related complications were also documented. Patient data were compiled from the admission files and intensive care unit (ICU) charts.
Results
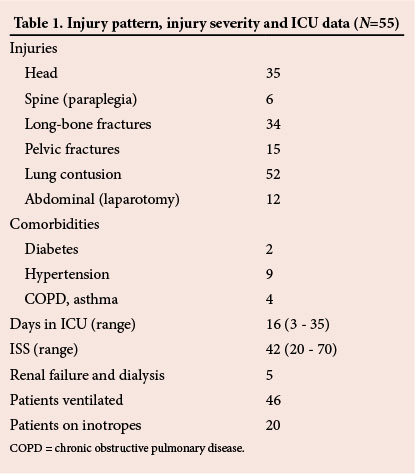
The injury pattern, injury severity, comorbidities and ICU stay data are shown in Table 1. The patients showed a typical injury profile that affected the timing and planning of the stent graft procedure. Of the 55 patients, 32 were treated on day 1 of admission, and the remainder between days 2 and 5. In 9 cases, another operative procedure was performed during the same anaesthesia (7 orthopaedic, 2 neurosurgical). Neurological injuries were confirmed on CT scans, and seven of these required neurosurgical interventions. Twenty-one patients with long-bone fractures required orthopaedic surgery within 24 hours of sustaining their injuries. The patients with lung injuries had X-ray evidence of fractured ribs or parenchymal contusion. Of the 55 patients, 24 required ventilation and 15 required inotropes prior to stent graft placement. In all patients, the stent graft was successfully inserted, the aortic injury appeared to be adequately treated and no endoleaks were detected.
Thirteen patients died after insertion of the stent grafts, at an average of 14 days. There was a trend that these patients were older, had a higher injury severity score (ISS) and a higher prevalence of comorbidities. None of the patients who died had preoperative CT scans and we were unable to evaluate whether a graft complication contributed to the death. However, events leading to death included pneumonia, acute respiratory distress syndrome, multi-organ dysfunction, cerebral oedema, myocardial contusion and renal failure.
Table 2 also shows other complications and technical uncertainties that may have affected outcomes. Of these, 19 patients had poor apposition of the stent graft to the inner curve of the aortic arch. This is likely to be due to significant stent graft oversizing in an acutely shaped aortic arch. Stent graft collapse is a potential complication of this and was seen in a 20-year-old patient who presented at 6 months follow-up with incomplete collapse of the proximal portion of a GORE TAG stent graft. His presenting problem at this time was severe hypertension, and he was treated by elective open repair of the aorta and removal of the stent graft; he recovered uneventfully.
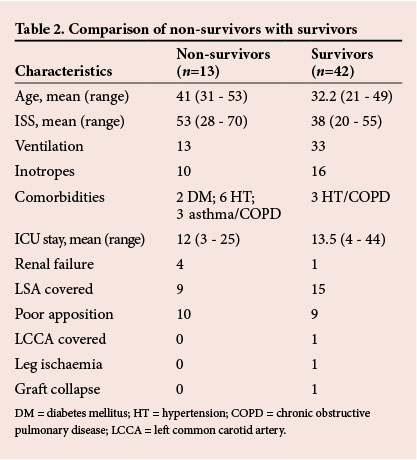
In one patient, the left common carotid artery was inadvertently covered during stent graft deployment. This was treated during the same procedure by retrograde insertion of a left carotid 'chimney' peripheral stent graft to re-establish flow into the carotid artery.
One patient developed an ischaemic lower limb 24 hours after stent graft insertion and required a femoral embolectomy.
In 24 patients, the left subclavian artery (LSA) was intentionally covered with the stent graft in order to secure the proximal part of the graft in a horizontal part of the arch. A potential complication of this was posterior cerebral or left arm ischaemia. None of this was apparent, but we cannot rule this type of complication out as 13 patients had associated head injuries. In this small series, none of these complications appeared to affect mortality.
Of the 42 survivors, 19 follow-up CT scans were available at 6 months, 6 at 1 year and 2 at 2 years. Although all patients were asked to return for follow-up and contact details were documented, we were still unable to trace many from the details supplied.
The stent graft characteristics in Table 3 indicate oversizing by up to 30%. Fifteen patients were oversized in excess of 20% as smaller-size grafts were not available. The long-term outcome of this is unknown and, as follow-up was poor, this remains a particular concern.
Discussion
TEVAR is rapidly being accepted as the standard of care to treat BTAI. The evolution of stent grafts and a better understanding of the natural history of the aortic injury are likely to improve outcomes in the future.
Although we were able to treat severely injured patients by apparently successful TEVAR, >25% still succumbed to their injuries. The numbers in this series are small and it is not possible at present to identify a subgroup of critically injured patients who would have died despite TEVAR. Many of these patients would not have been offered intervention in the past owing to the high risk associated with open surgery. There is likely to be a trend towards aggressive TEVAR management in patients with BTAI.
We have demonstrated that complications such as leg ischaemia and carotid ostial compromise, while uncommon, are still possible and may affect outcomes if not dealt with appropriately.
Of more concern is the lack of long-term data in young patients treated with TEVAR. Very few areas of vascular medicine demand stringent follow-up in excess of 30 years. The poor graft apposition to the inner curve, the excessive oversizing and the single case of graft collapse in this study support this view. Some of these concerns may be addressed by the current availability of smaller stent grafts (20 mm) and the more extensive use of infrarenal aortic extender cuffs. In the future, fenestrated grafts may solve the problem of LSA coverage.
Follow-up remains a major concern, and novel strategies such as medical alert bracelets may need to be assessed. We recommend that, where possible, multiple family members be informed of the need for follow-up. The notion that TEVAR is considered a damage control strategy and that a subset of patients undergo elective open surgery if stable, requires further investigation.
In view of these findings, it is imperative that interventionists pay attention to detail and adopt the most appropriate stent graft strategy for individual patients. Under stressful emergency situations one often forgets the potential long-term complications and uses what is available rather than what is appropriate. Inevitable complications are best treated by high-volume vascular centres.
Conclusion
The evolution of TEVAR as the standard of care in patients with BTAI is likely to be associated with long-term complications that we have not yet realised. The implementation of institutional protocols regarding stent graft measurements and follow-up may be helpful. In the future, lower-profile, arch-dedicated fenestrated stent grafts may alleviate current problems.
REFERENCES
1. Bell RE, Taylor PR, Aukett M, Sabharwal T, Reidy JF. Results of urgent and emergency thoracic procedures treated by endoluminal repair. Eur J Vasc Endovasc Surg 2003;25(6):527-531. [http://dx.doi.org/10.1053/ejvs.2002.1926] [ Links ]
2. Czermak BV, Fraedrich G, Perkmann R, et al. Endovascular repair of thoracic aortic disease: What we have learned. Curr Probl Diagn Radiol 2004;33(6):269-282. [http://dx.doi.org/10.1067/j.cpradiol.2004.08.001] [ Links ]
3. Iannelli G, Piscione F, Di Tommaso L, Monaco M, Chiariello M, Spampinato N. Thoracic aortic emergencies: Impact of endovascular surgery. Ann Thorac Surg 2004;77(2):591-596. [http://dx.doi.org/10.1016/S0003-4975(03)01348-1] [ Links ]
4. Scheinert D, Krankenberg H, Schmidt A, et al. Endoluminal stent-graft placement for acute rupture of the descending thoracic aorta. Eur Heart J 2004;25(8):694-700. [http://dx.doi.org/10.1016/j.ehj.2004.02.022] [ Links ]
5. Wellons ED, Milner R, Solis M, Levitt A, Rosenthal D. Stent-graft repair of traumatic thoracic aortic disruptions. J Vasc Surg 2004;40(6):1095-1100. [http://dx.doi.org/10.1016/j.jvs.2004.09.003] [ Links ]
6. Lachat M, Pfammatter T, Witzke H, et al. Acute traumatic aortic rupture: Early stent-graft repair. Eur J Cardiothorac Surg 2002;21(6):959-963. [ Links ]
7. Von Oppell UO, Dunne TT, De Groot MK, Zilla P. Traumatic aortic rupture: Twenty-year meta-analysis of mortality and risk of paraplegia. Ann Thorac Surg 1994;58(2):585-593. [ Links ]
8. Morishita K, Kurimoto Y, Kawaharada N, et al. Descending thoracic aortic rupture: Role of endovascular stent-grafting. Ann Thorac Surg 2004;78(5):1630-1634. [http://dx.doi.org/10.1016/j.athoracsur.2004.05.014] [ Links ]
9. Reed AB, Thompson JK, Crafton CJ, Delvecchio C, Giglia JS. Timing of endovascular repair of blunt traumatic thoracic aortic transections. J Vasc Surg 2006;43(4):684-688. [http://dx.doi.org/10.1016/j.jvs.2005.12.006] [ Links ]
 Correspondence:
Correspondence:
C Yazicioglu
c_yazicioglu@yahoo.com














