Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.53 n.1 Cape Town Mar. 2015
http://dx.doi.org/10.7196/SAJS.2250
VASCULAR SURGERY
Time since injury is the major factor in preventing tranexamic acid use in the trauma setting: An observational cohort study from a major trauma centre in a middle-income country
B ThurstonI; S ChowdhuryII; S EduII; A J NicolIII; P H NavsariaIV
IMA, MRCS (Eng); Trinity College, Oxford University, UK; Trauma Centre, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, South Africa
IIFCS (SA); Trauma Centre, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, South Africa
IIIPhD, FCS (SA); Trauma Centre, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, South Africa
IVMMed, FCS (SA), FACS; Trauma Centre, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Haemorrhage is responsible for about a third of in-hospital trauma deaths. The CRASH-2 trial demonstrated that early administration of tranexamic acid, ideally within 3 hours, can reduce mortality from trauma-associated bleeding by up to 32%.
OBJECTIVE: To explore whether, in our trauma network in a middle-income country, patients arrived at hospital soon enough after injury for tranexamic acid administration to be effective and safe.
METHODS: A prospective cohort study of 50 consecutive patients admitted to our trauma unit was undertaken. Inclusion criteria were as for the CRASH-2 study: systolic blood pressure <90 mmHg and/or heart rate >110 beats per minute, with injuries suggestive of a risk of haemorrhage. Patients with isolated head injuries were excluded. The mechanisms of injury, time since injury and any reasons for delay were recorded.
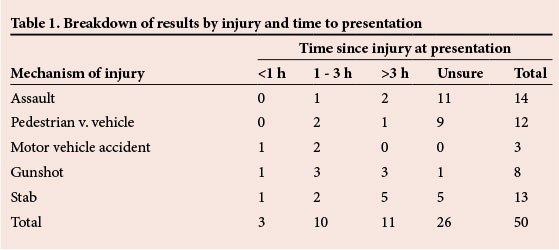
RESULTS: Thirteen (26%) patients presented early enough for tranexamic acid administration. Of these, only three patients presented within the 1st hour. Eleven patients had a documented time of injury >3 hours prior to presentation. We were unsure of the time of injury for 26 patients, although for most of these it was likely to be >3 hours before presentation.
CONCLUSIONS: The majority (74%) of bleeding trauma patients did not present within the timeframe allowed for safe administration of tranexamic therapy. Of those who did, most would have benefited from even earlier commencement of therapy. This raises the possibility that tranexamic acid may be more effective on a population basis if incorporated into prehospital rather than in-hospital protocols; future studies should explore the benefits and risks of this approach.
Trauma results in 5 million deaths each year worldwide, with 90% of these deaths occurring in lower-income countries.[1] Haemorrhage is responsible for up to a third of in-hospital trauma deaths; therefore, there is a need for an effective and inexpensive method of preventing the coagulopathy seen in bleeding trauma patients.[2]
Tranexamic acid is an antifibrinolytic that competitively inhibits the activation of plasminogen to plasmin. At high concentrations, it is also a non-competitive inhibitor of plasmin. It has an established role in elective surgery, where it is used to address the coagulopathy associated with major operations such as complex cardiac surgery.[3] Recently, the CRASH-2 trial demonstrated a survival advantage when tranexamic acid was given to trauma patients with significant haemorrhage, although the mechanism of this effect was unclear.[4] Analysis of the CRASH-2 data has shown that for the best outcome, tranexamic acid needs to be administered within the 1st hour of trauma, and that after 3 hours it conversely results in an increase in mortality.[5]
It has been suggested that tranexamic acid is unlikely to be used as a first-line treatment in hospitals in high-income countries where there is established and widespread use of blood products that can ameliorate the coagulopathy of trauma.[6] However, in low-and middle-income countries, where access to blood products is more difficult, tranexamic acid could be a practical, affordable and effective treatment for bleeding trauma patients.
Objective
We are based in a large trauma centre in South Africa, a middle-income country, where it has been suggested that tranexamic acid use may be incorporated into trauma protocols. Tranexamic acid is not currently a routine component of our care pathway nor is it at present readily available in our hospital. We explored whether patients arrived at our unit within a timeframe in which administering tranexamic acid on admission would be both safe and effective.
Methods
We undertook a prospective cohort study of 50 consecutive patients admitted to our trauma unit. We included any patient who had an injury that was suggestive of a risk of haemorrhage and who had a systolic blood pressure of <90 mmHg or a heart rate of >110 beats per minute (bpm) at any time from admission to 3 hours after injury. Any patient with an isolated head injury was excluded, as was any who, despite meeting the criteria based on vital signs, did not have injuries suggestive of haemorrhage as assessed by an experienced clinician.
For each patient we recorded the time of injury, time with prehospital services, any reasons for delay in reaching our unit, the mechanism of injury, all significant injuries sustained, the blood pressure or heart rate that triggered inclusion into the study and whether the patient survived to discharge from our unit.
Results
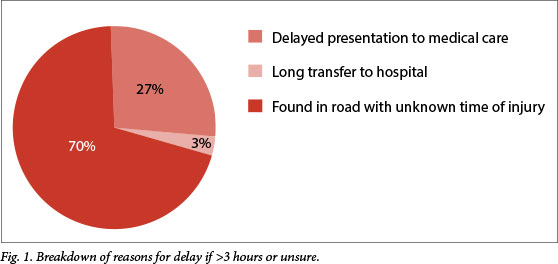
Fifty patients were recruited into the study over a period of 3 months. Of these, 47 were male and 3 were female, with a mean age of 32 years (range 15 - 78). Three patients arrived within the 1st hour after injury, 10 patients between 1 and 3 hours, 11 patients after 3 hours and the remaining 26 patients had an unknown time of injury (Table 1). Regarding the 26 patients with unknown time of injury, these patients were often found in the road following a presumed community assault or hit-and-run pedestrian v. car accident (Fig. 1) and, given the networks in place for reporting and responding to these incidents, the time from injury to presentation was unlikely to be >3 hours.
Within our cohort there was a 22% mortality rate (n=11), with 5 patients dying in the emergency department and a further 6 not surviving to discharge. The data collected are summarised in Table 2.
For all patients for whom we did not have a documented time of injury from the paramedics, we recorded reasons for being unable to obtain this information from the patient; of the 26 patients, 14 were intoxicated, 8 had a Glasgow Coma Scale score of <15, and 4 were unable to remember with any certainty the time of their injury.
We recorded the time from initial call to emergency services to arrival in the emergency department. Owing to the tendency of prehospital staff to round to the nearest 5 minute mark on their timesheets, we took the same approach and rounded all timings to the nearest 5 minutes. There was one outlier in which 270 minutes elapsed between call and arrival - this case was an anomaly where normal prehospital protocols were not followed. With this anomaly excluded, there was no significant difference between time from call to emergency department arrival for those patients for whom we knew the time of injury compared with those where we were unsure (mean (SD) 65 (20.3) minutes v. 60 (20.5) minutes, respectively; p<0.25 using the unpaired two-tailed ί-test). There was a significant difference in time from call to emergency department arrival between patients who presented <1 hour from injury and those who presented between 1 and 3 hours after injury, as could be expected (mean 35 (10.0) minutes v. 80 (9.7) minutes; p<0.001, unpaired two-tailed ί-test). Interestingly, there was no significant difference in the time with prehospital services between patients who arrived <3 hours following injury and those who arrived >3 hours following injury (mean 70 (23.1) minutes v. 60 (15.6) minutes; p<0.300, unpaired two-tailed ί-test). The times with prehospital services prior to hospital arrival are summarised in Fig. 2.
Discussion
Tranexamic acid is a cheap, effective and easily stored drug that has been shown to have a survival benefit when given to bleeding trauma patients. In lower- and middle-income countries where access to blood products is limited, tranexamic acid could have a considerable effect on reducing mortality from trauma. However, there is evidence that it needs to be used as soon as possible after injury - most benefit is seen in the 1st hour after injury; after 3 hours, administering tranexamic acid increases mortality.
In high-income countries with well-developed trauma networks and pre-hospital infrastructure, patients may often present to hospital within the 1st hour and almost certainly within 3 hours from injury. In lower- and middle-income countries, the presentation is often delayed. We explored whether bleeding trauma patients who met certain haemodynamic criteria reached our hospital early enough for administering tranexamic to be both safe and effective. Our results showed that only 6% of patients reached hospital within the ideal 1-hour period, and that in total only 26% arrived within a timeframe where it was safe to administer tranexamic acid. This suggests that the hospital environment would only serve a small minority of patients effectively, with 74% of patients unable to receive treatment and the subsequent survival benefit available from tranexamic acid.
The data from the paramedics regarding time from call to arrival at the emergency department suggests that emergency personnel are with the patient for a considerable proportion of the time from injury to hospital. Particularly for those patients arriving between 1 and 3 hours from injury, the delay would appear to be within the trauma system compared with those who arrive <1 hour from injury. This could be for a variety of reasons, including prolonged extrication time at the scene or the requirement to perform certain lifesaving procedures prior to departure (e.g. intubation or intercostal drain insertion). However, there is no statistical difference in the prehospital time between patients who presented <3 hours from injury and those who presented >3 hours from injury. The data therefore imply that the latter group presents later to medical care and that this delay in seeking care is the greatest factor in their ineligibility for tranexamic acid, rather than the time taken to reach hospital once the emergency services are aware of the incident.
The most common reason for patients not meeting the criteria for tranexamic therapy was an inability to pinpoint a time of injury. This made the administration of tranexamic acid potentially unsafe, as it increases mortality if given after 3 hours from time of injury. The proportion of patients for whom we could not establish a definite time of injury was surprising and in conflict with the CRASH-2 data, which had only 9 out of >20 000 patients for which injury time was unknown. There are some cultural differences in our population that could explain this, along with a limiting factor in our data collection (see below); however, the most likely explanation for this difference is that the CRASH-2 trial entry proforma only required an estimated time of injury rather than clear documentation or proof of injury time. It would be interesting to see whether estimating in this fashion correlates well with the actual time of injury.
The injury profiles of our cohort could explain the lack of data on precise injury time. A total of 22% of our patients arrived having suffered from community assault - a phenomenon not often seen in many other countries - where the community imposes its own retribution on members of that community who have committed crimes, often leaving that person for dead following physical assault. A further 24% of patients were victims of hit-and-run accidents that had no available witnesses. Apparent amnesia for events, either secondary to injuries sustained or due to intoxication, was also a complicating factor.
Unfortunately, we did not have access to the transcripts or recordings of the initial telephone calls to the emergency services, which may have enabled the time of injury to have been established in more cases. Our data relied on information provided from discussion with paramedics at handover and prehospital documentation (as would be available to our emergency physicians). There is an opportunity for a further multi-agency trial to explore whether the time of injury in our patients can be established more frequently and documented more accurately.
If tranexamic acid therapy were to be implemented in the prehospital setting, then it is likely that many of the 20% of patients who would have received treatment between 1 and 3 hours following injury may receive therapy within the 1st hour, potentially improving outcomes. Some of the patients who presented with a time from injury >3 hours previously may also become eligible for treatment. This possibility has been raised before;[6] however, given the results of recent studies that have demonstrated an increased risk of thrombosis in patients given tranexamic acid, further work should be done on the safety of this approach before it is incorporated into routine practice.[6,7] Within our system, there would have to be considerable retraining of paramedics to ensure that indications for tranexamic acid use are correctly identified, along with appropriate awareness of relative contraindications. Subsequent to this, regulatory approval would need to be sought. These processes alone may present a significant barrier to implementation of protocol change even if the results of future studies suggest that tranexamic acid is safe to be used in this environment.
Conclusion
The use of tranexamic acid therapy in bleeding trauma patients has been shown by the CRASH-2 trial to decrease mortality by up to 32% if given in the 1st hour after injury. In low- and middle-income countries, there is a lack of other affordable and available agents to combat the coagulopathy associated with trauma; therefore, tranexamic acid has the potential to dramatically improve patient survival from trauma in these countries. However, as the CRASH-2 trial demonstrated an increased mortality if tranexamic acid was administered >3 hours after injury, it is paramount that the time of injury is ascertained and therapy commenced as soon as possible. In our study, the majority of our patients did not meet the time criteria necessary to receive treatment.
The time-critical nature of tranexamic acid therapy unfortunately limits its utility in low- and middle-income countries. Within our population, only 6% of trauma patients received maximum benefit; however, this is largely due to community actions and cultural attitudes to trauma, with only a small percentage of patients for whom a delay within the trauma network itself was responsible for delayed presentation. This study therefore does not clearly support the use of tranexamic acid in the prehospital setting, although for those patients with a known time of injury, tranexamic acid therapy should be administered as soon as possible and prehospital administration would therefore be ideal. We suggest that routine incorporation of tranexamic acid into trauma protocols would have a far more modest effect overall than that proposed by CRASH-2.
Acknowledgements. B Thurston would like to thank the Oppenheimer Fund for their support in enabling this manuscript to be created.
REFERENCES
1. Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: The neglected burden in developing countries. Bull World Health Organ 2009;87(4):246-246a. [ Links ]
2. Sauaia A, Moore FA, Moore EE, et al. Epidemiology of trauma deaths: A reassessment. J Trauma 1995;38(2):185-193. [ Links ]
3. Henry DA, Carless PA, Moxey AJ, et al. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2011;(3):CD001886. [http://dx.doi.org/10.1002/14651858.CD001886.pub41 [ Links ]
4. CRASH-2 trial collaborators, Shakur H, Roberts I, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): A randomised, placebo-controlled trial. Lancet 2010;376(9734):23-32. [http://dx.doi.org/10.1016/S0140-6736(10)60835-5] [ Links ]
5. The CRASH-2 collaborators, Roberts I, Shakur H, et al. The importance of early treatment with tranexamic acid in bleeding trauma patients: An exploratory analysis of the CRASH-2 randomised controlled trial. Lancet 2011;377(9771):1096-101. [http://dx.doi.org/10.1016/S0140-6736(11)60278-X] [ Links ]
6. Mitra B, Fitzgerald M, Cameron PA, Gruen RL. Tranexamic acid for trauma. Lancet 2010;376(9746):1049; author reply 1050-1051. [http://dx.doi.org/10.1016/S0140-6736(10)61476-6] [ Links ]
7. Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ. Military application of tranexamic acid in trauma emergency resuscitation (MATTERs) Study. Arch Surg 2012;147(2):113-119. [http://dx.doi.org/10.1001/archsurg.2011.287] [ Links ]
 Correspondence:
Correspondence:
B Thurston
benjamin.thurston@gmail.com














