Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.52 n.4 Cape Town Nov. 2014
http://dx.doi.org/10.7196/sajs.1934
CASE REPORT
The mystical foot with pink mushrooms: Imaging of maduromycosis - a rarity in southern Africa
G JacksonI; N KhanII
IMB ChB, DA (SA); Department of Radiology, Kalafong Hospital, Pretoria, and School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
IIMBBS, FCRad (D); Department of Radiology, Kalafong Hospital, Pretoria, and School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
Maduromycoses (Madura foot) are chronic granulomatous subcutaneous infections endemic to certain regions, but not southern Africa. The infection is caused by both pure fungi and bacteria. Imaging plays an important role in assessing the severity of disease and the direction of its spread, assisting in treatment planning and in the monitoring of treatment response. The typical 'dot-in-circle' sign on magnetic resonance imaging is diagnostic of Madura foot. We present the case of an adolescent South African boy who presented with fungoid growths on his foot, typical of this disease.
Case report
A 16-year-old boy presented with a 4-month history of progressive swelling of the distal third of the right leg and the right foot, associated with pain and pruritus. Multiple exophytic lesions had developed on the surface of the foot, and there were discharging sinuses (Fig. 1). He had no regional lymphadenopathy and no constitutional symptoms. A history was given of a similar but less dramatic episode 6 years previously, which had been treated medically with complete regression. However, no clinical records were available from that time to specifically relate the two pathologies. He could not relate any trauma to the onset of symptoms, did not suffer from any known comorbid conditions, and was not immunocompromised.

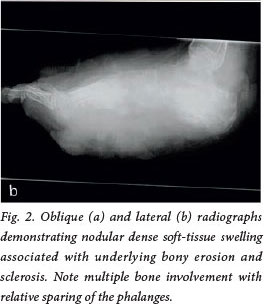
Radiographs (Fig. 2) demonstrated diffuse dense nodular soft-tissue swelling with effacement of the fascial planes. There was sclerosis and osteolysis with periosteal reactions in the underlying bones. The tarsals and metatarsals were involved, with relative sparing of the phalanges. These findings were confirmed with computed tomography (CT) on both bony and soft-tissue reconstruction algorithms.
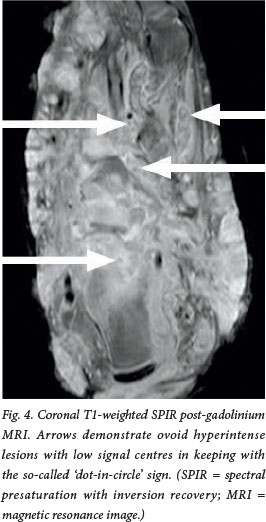
Magnetic resonance imaging (MRI) (Figs 3 and 4) demonstrated a diffusely infiltrating soft-tissue mass involving the subcutaneous tissue, muscles and intermuscular fascial planes. The bony elements, shown to be involved on previous imaging, were engulfed and destroyed. There was encasement but sparing of the tendons. The lesions were hypointense on Tl-weighted images, and of high signal intensity on T2-weighted and T2-weighted fatsaturated images. On a contrast-enhanced Tl-weighted sequence there was diffuse but heterogeneous enhancement. Of note were multiple discrete hyperintense nodularities with hypointense central foci seen on the post-gadolinium T2-weighted and T2-weighted fat-saturated sequences - the 'dot-in-circle' sign. The draining sinuses were well visualised as linear-enhancing tracts on all imaging sequences.
The differential diagnosis at the time of presentation, taking local epidemiological factors into account, was chronic osteomyelitis (bacterial or tuberculous), chronic fungal infection and leishmaniasis. Neoplastic disease was considered, but thought to be unlikely in view of the given history and clinical and radiological findings.
Histological findings
Multiple deep-tissue biopsies of the growths on the foot were taken. The morphological features of the organisms were compatible with an infection by Actinomyces species.
Discussion
Mycetoma or Madura foot is an insidious chronic granulomatous inflammatory disease affecting the subcutaneous tissues.[1] A wide range of organisms, present in the soil[1] and falling into one of two groups, cause mycetoma. The two groups are the eumyces, or true fungi, and the actinomyces, filamentous bacteria of the order Actinomycetales.[1]
Mycetoma is sporadically reported in South Africa (SA), but no specific epidemiological figures could be found for SA in the available literature, possibly owing to the rarity, under-reporting or misdiagnosis of the condition.
The disease mainly affects males, the majority of patients presenting between the ages of 20 and 40 years.[2] The most commonly affected site is the foot (80%),[1] although mycetoma can occur anywhere on the body.[2]
The hallmark of the disease is the formation of subcutaneous granulomas and tumefaction, with sinus tract formation or abscess fistularisation.[1] The disease evolves slowly and generally painlessly,[2] with patients, as in our case, presenting many years after the onset of infection, often with extensive soft-tissue and bone involvement.[2]
The most common differential diagnosis at the time of presentation is chronic bacterial osteomyelitis or tuberculosis. Other deep fungal infections such as blastomycosis or coccidiomycosis, leishmaniasis, yaws and syphilis should be considered, and the possibility of neoplastic disease must be kept in mind.[2]
The radiological features (Fig. 2, a and b) characteristically include soft-tissue swelling, obliteration of tissue planes and nodular opacities. The bones may demonstrate osteopenia and periosteal reaction (demonstrated prior to significant bony involvement - as opposed to osteomyelitis, where the bony findings are seen prior to the periosteal reaction). The periosteal reaction may also demonstrate a pattern indistinguishable from that caused by osteogenic sarcoma.[2] Bony erosion, multiple osteolytic 'punched-out'[2] lesions, and occasionally extensive bony destruction and bony sclerosis are further features.[3]
CT is invaluable in demonstrating bone destruction, periosteal reaction, erosions, coarsening of trabeculae and soft-tissue involvement, and may also be used for accurate patient follow-up and assessment of response to therapy.[4]
MRI visualises the soft-tissue and bone involvement on Tl-weighted (Fig. 3, a and b) images in terms of low-signal lesions.[41 More significantly, as mycetoma is characterised by the formation of 'grains' that are found within abscesses surrounded by abundant granulation tissue, a characteristic appearance is seen on T2-weighted, short tau inversion recovery (STIR) and T1-weighted fat-saturated post-gadolinium MRI (Fig. 4). Conglomerates of small round hyperintense lesions, representing the abscess and granulation tissue, surrounded by a low-signal-intensity rim, representing intervening fibrous septa, and a central low-signal-intensity 'dot', a result of the susceptibility effect caused by the presence of the grains, form the 'dot-in-circle' sign (Fig. 4) that is highly suggestive of mycetoma.[5]
Management of maduromycosis is based on the extent of the disease as assessed radiologically and on the causative agent as defined histologically. Actinomycetoma is amenable to medical treatment by antibiotics and antimicrobial agent combinations, while combined medical and surgical treatment is the gold standard in eumycetoma. In general, the current treatment for mycetoma is unsatisfactory - it needs to be of long duration to achieve cure, has many side-effects, has a high relapse rate, and is expensive for patients and health authorities.[2]
Conclusion
Madura foot/mycetoma is debilitating and difficult to treat, infrequently encountered by physicians in countries outside endemic areas, and often misdiagnosed as a neoplasm or other granulomatous disease. The diagnosis of mycetoma is often not even considered. The diagnosis relies on direct examination of the grains and isolation of the aetiological agents. Imaging studies are useful, not only for defining the extent of disease but also to assist the clinician in determining the true pathology and later to assess treatment response.
REFERENCES
1. Rouphael NG, Talati NJ, Franco-Paredes C. A painful thorn in the foot: A case of eumycetoma. Am J Med Sci 2007;334(2):142-144. [http://dx.doi.org/10.1097/MAJ.0b013e31812dfd70] [ Links ]
2. Fahal AH. Mycetoma Research Centre, University of Khartoum. Sudan. c2009 updates, review article. http://www.Mycetoma.Edu.Sd/Academic/Updates.Htm#EumycetomaMedicalTreatment (accessed 22 April 2012). [ Links ]
3. Murray RO, Jacobson HG, Stroker DJ. The Radiology of Skeletal Disorders. 3rd ed.New York: Churchill Livingstone, 1990:351-355. [ Links ]
4. Czechowski J, Nork M, Haas D, Lestringant G, Ekelund L. MR and other imaging methods in the investigation of mycetomas. Acta Radiol 2001;42(1):24-26. [http://dx.doi.org/10.1034/j.1600-0455.2001.042001024.x] [ Links ]
5. Cherian RS, Betty M, Manipadam MT, et al. The 'dot-in-circle' sign - a characteristic MRI finding in mycetoma foot: A report of three cases. Br J Radiol 2009;82(980):662-665. [http://dx.doi.org/10.1259/bjr/623866891 [ Links ]
 Correspondence:
Correspondence:
G Jackson
(gavin0330@polka.co.za)