Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.52 n.4 Cape Town Nov. 2014
http://dx.doi.org/10.7196/sajs.1917
PLASTIC SURGERY
Regional anaesthesia for cleft lip surgery in a developing world setting
V MalherbeI; A T BosenbergII; A K Lizarraga LomeliIII; C NeserIV; C H PienaarV; A MadareeVI
IMB ChB; Kimberley Hospital Complex, Northern Cape, South Africa
IIMB ChB, FFA (SA); Department of Anesthesia and Pain Management, Seattle Children's Hospital, WA, USA
IIIMD (USA); Operation Smile Inc., Norfolk, Virginia, USA
IVMB ChB; Department of Plastic Surgery, Tygerberg Hospital, Cape Town, South Africa
VMB ChB, FC Plast Surg (SA); Private practice, Cape Town, South Africa
VIMB ChB, FCS (SA), MMed (Plastic and Reconstructive Surgery) FRCS (Eng), FRCS (Irel); Plastic and Reconstructive Surgery, Inkosi Albert Luthuli Hospital, Durban, South Africa
ABSTRACT
BACKGROUND: The role of regional anaesthesia in cleft lip surgery in the developing world is not well documented
OBJECTIVE: To report on the use of regional anaesthesia in cleft lip surgery in adults and adolescents in a developing world setting
METHOD: A retrospective chart review of 100 patients aged >14 years who had cleft lip surgery during an Operation Smile South Africa (OSSA) volunteer surgical programme in Madagascar during 2007 and 2008. The nerve blocks used included a bilateral infraorbital nerve block, a dorsal-nasal nerve block and a septal block supplemented with peri-incisional local infiltration. Appropriateness of the regional anaesthesia alone for cleft lip surgery was determined by absence of any intraoperative complications, postoperative complications or conversions to general anaesthesia
RESULTS: Seventy-four patients commenced their operation under regional anaesthesia. There were no intraoperative or postoperative complications documented, and no patient required conversion to general anaesthesia. Two patients required additional analgesia in the immediate postoperative period
CONCLUSION: Regional anaesthesia for cleft lip surgery in patients >14 years of age was well tolerated and associated with few complications. It is a safe and effective option when used as the sole anaesthetic modality for cheiloplasty in the developing world
Cleft lip is a common craniofacial abnormality. The prevalence of cleft lip, with or without an associated cleft palate, is 0.1% in the general population.[1] Surgery is usually performed during infancy. Unfortunately patients in developing countries often present late because they do not have ready access to cleft lip repair.
There is limited literature on regional analgesia as the sole anaesthetic for cleft lip repair in adults and adolescents. Hodges and Hodges[2] developed a protocol for safe anaesthesia for cleft lip and palate surgery appropriate for remote centres with only basic facilities in Uganda, suggesting that patients aged >10 years could have cleft lip surgery performed under sedation using local anaesthesia alone.
Regional anaesthesia carries an extremely low risk of complications. In a large prospective survey from the French-language anaesthesia societies (Association des Anesthésistes Réanimateurs Pédiatriques d'Expression Française), 21 278 patients received a peripheral nerve block and the incidence of complications was 0.005% deaths, 0.08% seizures and 0.01% cardiac arrests.[3] Regional anaesthesia has been well documented to be safe and effective in upper extremity blockade.[4]
The objective of this study was to determine the value of regional anaesthesia as the sole anaesthetic modality for cleft lip surgery in patients >14 years of age.
Methods
The study was approved by the Health and Research Ethics Committee, Stellenbosch University, Western Cape Province, South Africa, and received the support of the Operation Smile International Research Center in Norfolk, VA, USA.
One hundred charts of patients older than 14 years who underwent cleft lip surgery during OSSA volunteer surgical missions in Madagascar during November 2007, May 2008 and November 2008 were reviewed. An arbitrary age limit of 14 years was based on the triage system developed by Operation Smile International, provided patients were able to give informed consent. Patients with contraindications to regional anaesthesia (allergy, refusal) were excluded. Patients younger than 14 years received general anaesthesia. The charts were randomly selected from those who fulfilled the inclusion criteria of ≥14 years and had cleft lip surgery.
The data collected included age, weight, gender, type of lip defect, presence of associated palate or other deformities, type of lip repair, and intraoperative and postoperative complications. All patient identifiers were removed to protect the study participants' privacy and confidentiality.
Of the 100 patients whose charts were reviewed, 26 were considered to need general anaesthesia from the outset, the reasons including patient refusal of regional anaesthesia and complex surgery (more than a standard cleft lip repair). None of these 26 cases was a conversion from a regional nerve block.
Technique
The patient was positioned comfortably on the operating table in the supine position. Before the regional block was placed, all surgical markings were made on the lip. A gauze swab was placed into the mouth to absorb any blood. The area was cleaned using an antiseptic alcohol preparation.
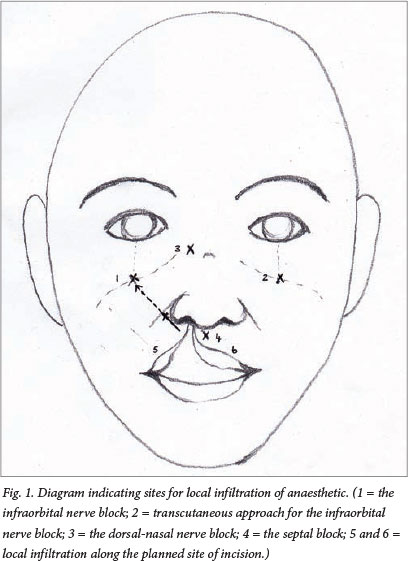
The anaesthetic solution consisted of bupivacaine 0.5% (2.5 mg/ kg) and 1 ml adrenaline (1:1 000), diluted with normal saline to a 1:100 000 concentration. Depending on the size of the patient, 10 - 15 ml of this mixture was used for infiltration to vasoconstrict the surgical area. Individual nerve blocks were performed using 0.5% bupivacaine. The same solution as for the infiltration was used, i.e. not excluding the adrenaline (the amount given was limited to a total of 2.5 mg/kg). A bilateral infraorbital nerve block was performed initially. The site of injection was in the apex of the triangle formed between the nasolabial fold and the ala nasi. The needle was directed supralaterally towards the infraorbital foramen about 5 mm below the margin of the infraorbital rim, and 1 - 1.5 ml of solution was injected around the infraorbital foramen (not within the foramen, in an attempt to avoid nerve damage or intraneural injection). Alternatively, the infraorbital foramen was palpated and 1 ml 0.5% bupivacaine injected transcutaneously by introducing a needle perpendicular to the skin at the point where bone contact was made.
Supplementary nerve blocks included the dorsal nasal nerve and a septal block. The dorsal-nasal nerve block was achieved by infiltrating 0.5 - 1 ml of the adrenaline-bupivacaine solution 0.6 cm lateral to the midline of the dorsum of the nose at the junction of the nasal bone and upper lateral cartilage. The septal block was achieved by infiltrating 0.5 - 1 ml solution at the columella-lip junction on either side of the nasal septum by running the needle along the base of the septum. Subsequently 1 - 2 ml of solution was infiltrated painlessly along the planned site of incision and dissection to supplement the nerve blocks and provide local vasoconstriction. The technique is illustrated diagrammatically in Fig. 1.
No sedation was given. An interpreter was available to communicate with the patient, to allow the surgeon to explain the procedure and the patient to communicate his or her needs and concerns.
On completion of the surgery, the patients were able to walk to the acute care unit. Nursing staff completed a standard monitoring sheet for each patient in the unit and subsequently in the ward. Any immediate postoperative complications were noted.
Patient data were captured electronically and identifiers removed. The medical records were stored in Operation Smile International's headquarters and research centre in Norfolk, VA, USA.
Results
Seventy-four patients, 45 males and 29 females, were included in the study. The mean age (standard deviation) was 23.47 (7.53) years (range 14 - 46). There were 11 bilateral and 63 unilateral lip repairs. There was no relationship between pathology and gender.
There were no intraoperative complications, and no patient required conversion to general anaesthesia. Postoperative complications are listed in Table 1. Only two patients needed further analgesia (paracetamol/acetaminophen) in the immediate postoperative period.

Discussion
Regional anaesthesia provides analgesia without the risk of respiratory depression induced by opiate analgesia. Nerve blocks can be administered with minimal equipment and have a low risk of complications, and it is not surprising that regional anaesthesia is popular for cleft lip surgery among international volunteer missions operating in the developing world [2,5-8]
Cleft lip surgery is usually performed on infants and young children, who require general anaesthesia. General anaesthesia with a supplemental infraorbital nerve block is well documented in children. A nerve block allows lower concentrations of inhalation anaesthesia and reduced intraoperative opioid use.[9-14] These benefits are of particular value where resources are limited and complications of anaesthesia are harder to deal with.
Various regional anaesthetic techniques have been described. Prabhu et al.[11] compared the postoperative analgesic effect of bilateral infraorbital nerve block with that of peri-incisional infiltration in infant cleft lip surgery and demonstrated the superiority of nerve blocks. Eipe et al.[9] reported the use of infraorbital nerve blocks and local skin infiltration for surgical repair of cleft lips in 20 patients >12 years of age, concluding that it was a safe and effective method that provided postoperative analgesia for up to 24 hours. Simion et al.[13] compared supplemental bilateral infraorbital nerve blocks with intravenous fentanyl for analgesic effect during cleft lip surgery in infants. There were no significant differences in the pain scores between the two groups over time, but additional analgesia was required earlier in the fentanyl-only group. In a larger study that included children aged 3 months - 10 years, Rajamani et al.[14] found that a bilateral infraorbital nerve block was superior to fentanyl in terms of analgesia, time to awakening and early feeding.
In our retrospective study, regional anaesthesia allowed surgery to be performed without supplemental general anaesthesia. The technique was used for both unilateral and bilateral cleft lip repairs. The dorsal-nasal, septal and infraorbital nerve block combined with local infiltration provided complete anaesthesia to the operative field. Opiate analgesia was not needed, thus avoiding its side-effects.[15]
Regional anaesthesia in minor surgery is known to decrease the demand on post-anaesthetic care providers[15] and allows patients to be discharged sooner. All these benefits add value to its use in the developing world and on volunteer missions.
An interpreter or supportive care provider plays an essential role in the success of this technique. The psychological discomfort of being awake during surgery can be reduced by adequate preoperative preparation and explanation during the procedure. Most patients fear the pain of injections, and some find the numbness of the lip (which may last for several hours after surgery) disquieting.
Financial constraints and limited healthcare resources have been documented as primary reasons for preventing patients from receiving timely cleft lip surgery.[9] The benefit of being able to perform a surgical procedure at the lowest possible cost and with the minimum of equipment and staff is a significant advantage of regional anaesthesia in developing countries.
Conclusion
Regional anaesthesia for cleft lip surgery in patients >14 years of age is easily administered, has minimal complications and is well tolerated by patients. It negates the need for general anaesthesia. In this study regional anaesthesia was safe and effective when used as a sole anaesthetic for cheiloplasty in this age group.
Disclaimer. There were no conflicts of interest, and the authors were not paid to write this article and did not receive any gifts. No financial incentives were involved, and neither Operation Smile nor any other party sponsored or provided any remuneration for the completion of this study. All patients and volunteers on Operation Smile South Africa surgical programmes have given signed consent to be photographed.
REFERENCES
1. Nussbaum R, Mclnnes R, Willard H. Thompson & Thompson Genetics in Medicine. Philadelphia: Saunders, 2007. [ Links ]
2. Hodges SC, Hodges AM. A protocol for safe anaesthesia for cleft lip and palate surgery in developing countries. Anaesthesia 2000;55(5):436-441. [http://dx.doi.org/10.1046/j.1365-2044.2000.01371.x] [ Links ]
3. Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious complications related to regional anesthesia: Results of a prospective survey in France. Anesthesiology 1997;87(3):479-486. [http://dx.doi.org/10.1016/j.rapm.2008.07.527] [ Links ]
4. Neal JM, Gerancher JC, Hebl JR, et al. Upper extremity regional anesthesia: Essentials of our current understanding, 2008. Reg Anesth Pain Med 2009;34(2):134-170. [http://dx.doi.org/10.1097/AAP.0b013e31819624eb] [ Links ]
5. Ugburo AO, Desalu I, Adekola AF, Fadeyibi IO. Day case clet lip surgery in Lagos, Nigeria. Cleft Palate Craniofac J 2009;46(6):636-641. [http://dx.doi.org/10.1597/07-156.1] [ Links ]
6. Aziz SR, Rhee ST, Redai I. Cleft surgery in rural Bangladesh: Reflections and experiences. J Oral Maxillofac Surg 2009;67(8):1581-1588. [http://dx.doi.org/10.1016/j.joms.2008.11.021] [ Links ]
7. Pham AM, Tollefson TT. Cleft deformities in Zimbabwe, Africa: Socioeconomic factors, epidemiology, and surgical reconstruction. Arch Facial Plast Surg 2007;9(6):E1-E7. [http://dx.doi.org/10.1001/archfaci.9.6.qsp70001] [ Links ]
8. Tollefson TT, Wong KJ, Sykes JM, Larrabee WF. Clet lip-palate deformities in Western China: Epidemiology, surgical reconstruction and cost. Arch Facial Plast Surg 2006;8(4):234-239. [http://dx.doi.org/10.1001/archfaci.8.4.234] [ Links ]
9. Eipe N, Choudhrie A, Pillai DA, Choudhrie R. Regional anaesthesia for clet lip repair: A preliminary study. Cleft Palate Craniofac J 2006;43(2):138-141. [http://dx.doi.org/http://dx.doi.org/10.1597/05-025.1] [ Links ]
10. Zide B, Swit R. How to block and tackle the face. Plastic Reconstr Surg 1998;101(3):840-851. [http://dx.doi.org/10.1097/00006534-199803000-00041] [ Links ]
11. Prabhu KPK, Wig J, Grewal S. Bilateral infraorbital block is superior to peri-incisional infiltration for analgesia after repair of cleft lip. Scand J Plast Reconstr Surg Hand Surg 1999;33(1):83-87. [ Links ]
12. Giaufre E, Dalens B, Gombert A. Epidemiology and morbidity of regional anaesthesia in children: A one-year prospective survey of the French Language Society of Pediatric Anesthesiologists. Anesth Analg 1996;83(5):904-912. [http://dx.doi.org/10.1213/00000539-199611000-00003] [ Links ]
13. Simion C, Corcoran J, Iyer A, Suresh S. Postoperative pain control for primary clet lip repair in infants: Is there an advantage in performing peripheral nerve blocks? Pediatric Anesthesia 2008;18(11):1060-1065. [http://dx.doi.org/10.1111/j.1460-9592.2008.02721.x] [ Links ]
14. Rajamani A, Kamat VI, Rajavel VP, Murthy J, Hussain SA. A comparison of bilateral infraorbital nerve block with intravenous fentanyl for analgesia following cleft lip repair in children. Pediatric Anesthesia 2007;17(2):133-139. [http://dx.doi.org/10.1111/j.1460-9592.2006.02032.x] [ Links ]
15. Salloum ML, Ebelin KR, Sethna N, Hamadan US. Combined use of infraorbital and external nerve blocks for effective perioperative pain control during and after cleft lip repair. Cleft Palate Craniofac J 2009;4(6):629-365. [http://dx.doi.org/10.1597/08-142.1] [ Links ]
 Correspondence:
Correspondence:
VMalherbe
(vanessa.malherbe@gmail.com)














