Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.52 no.4 Cape Town Nov. 2014
http://dx.doi.org/10.7196/sajs.2116
GENERAL SURGERY
Developing a clinical model to predict the need for relaparotomy in severe intra-abdominal sepsis secondary to complicated appendicitis
V Y KongI; S van der LindeII; C AldousIII; J J HandleyIV; D L ClarkeV
IMB ChB, MSc, PhD, MRCS (Ed); Department of General Surgery, Pietermaritzburg Metropolitan Hospital Complex, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
IIMSc; Department of General Surgery, Pietermaritzburg Metropolitan Hospital Complex, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
IIIPhD; Department of General Surgery, Pietermaritzburg Metropolitan Hospital Complex, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
IVFCA (SA); Department of General Surgery, Pietermaritzburg Metropolitan Hospital Complex, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
VMMedSci, MPhil, MBA, FCS (SA); Department of General Surgery, Pietermaritzburg Metropolitan Hospital Complex, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
ABSTRACT
INTRODUCTION: Complex intra-abdominal sepsis secondary to acute appendicitis is common in South Africa, and management frequently involves relaparotomy. The decision to perform relaparotomy is often difficult, and this study aimed to develop a clinical model to aid the decision-making process.
METHODS: The study was conducted from January 2008 to December 2012 at Edendale Hospital, Pietermaritzburg. All patients with intraoperatively confirmed acute appendicitis and all patients in this group who subsequently underwent relaparotomy were included. The clinical course, intraoperative findings and outcome of all patients were recorded until discharge (or death). Using a combination of preoperative and intraoperative parameters, a clinical model was developed to predict the need for relaparotomy.
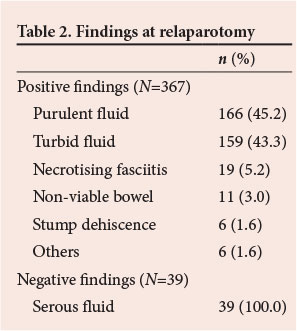
RESULTS: Of the total of 1 000 patients identified, 54.1% were males. The median age for all patients was 21 years. Of 406 relaparotomies, 227 (55.9%) were planned and 179 (44.1%) on demand (expectant treatment). In the relaparotomy group, 367 patients (90.4%) had positive findings. Logistic regression analysis showed that the following four factors accurately predicted the need for subsequent relaparotomy: patients referred from any rural centre, duration of illness >5 days, heart rate >120 bpm, and perforation associated with generalised intra-abdominal sepsis. This model had a predictive value of >90%.
CONCLUSIONS: We have constructed a model that uses clinical data available at initial laparotomy to predict the need for subsequent relaparotomy in patients with complicated acute appendicitis. It is hoped that this model can be integrated into routine clinical practice, but further study is first needed to validate this model.
In southern Africa, acute appendicitis is often associated with late presentation and advanced pathology, and surgeons are therefore frequently required to manage complex intra-abdominal sepsis.[1-5] This condition is associated with significant morbidity and even mortality, and aggressive surgical management is essential, as source control remains the cornerstone of therapy.[6,7] Achieving source control frequently requires one or more relaparotomies.[7] Deciding on the need for relaparotomy and its optimal timing is often highly subjective. The decision to reoperate is frequently challenging when faced with a critically ill patient with nonspecific signs and symptoms of partially treated sepsis.[8] There is a lack of general consensus as to which patients should be subjected to relaparotomy.[8-10] There are essentially two approaches to the management of complex intra- abdominal sepsis. These are the so-called planned relaparotomy (PR) approach and the on-demand relaparotomy (OD) approach.[11] The PR approach takes all patients with complex sepsis back to the operating room at regular 48-hour intervals until adequate source control has been achieved. With the OD approach, all patients are treated expectantly and only those with signs of unresolved intra-abdominal sepsis are subjected to relaparotomy.[7] The use of temporary abdominal closure (TAC) is generally reserved for patients with abdominal compartment syndrome, or when technical issues preclude primary closure.[11-13] For practical and ethical reasons, it is difficult to formally compare the efficacy of the different approaches (PR v. OD) in a randomised study, and most of the current evidence is at best level 2.[13,14] The available evidence to date does not seem to suggest that either approach confers a superior advantage in terms of mortality.[15] There are very few data on this specific problem from the developing world, where the spectrum of disease is markedly different from that in the developed world.[1-5,8,16] The objective of this study was to identify preoperative and intraoperative clinical factors that may predict the need for relaparotomy in order to construct a clinical model to assist clinicians in predicting the need for relaparotomy in patients with complex intra-abdominal sepsis following acute appendicitis.
Methods
Clinical setting
This study was conducted from January 2008 to December 2012 at Edendale Hospital, Pietermaritzburg, South Africa. Ethical approval was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal and the Umgungundlovu Health Ethics Review Board (ethics reference number: BE 237/12). Edendale Hospital is a regional hospital in the city of Pietermaritzburg. It provides definitive surgical care to the city as well as the surrounding rural areas. The region comprises two different health districts, namely the rural Sisonke Health District and the urban Umgungundlovu Health District, and covers a total catchment population of over 3 million people. All patients either present directly to our hospital from within the urban district or are referred by one of the four rural hospitals in the catchment area.
Current protocol
The management of abdominal sepsis following acute appendicitis is currently at the discretion of the individual surgeon. All patients who require TAC undergo mandatory relaparotomy. In the OD group we have a very low threshold for relaparotomy and tend to invert the thinking process somewhat by emphasising to staff that the patient must earn the right not to have a relaparotomy rather than earn the right to have one.
The study
All patients with intraoperatively confirmed acute appendicitis were eligible for inclusion. Basic demographic data were collected. The clinical symptoms, findings on physical examination, baseline vital signs and laboratory results were recorded. Intraoperative details included the surgeon's assessment of the macroscopic appearance of the appendix and the presence of perforation. The severity of abdominal contamination was classified clinically as either localised contamination (LC) or generalised four-quadrant contamination (GC). The clinical progress of all patients was followed up until discharge (or death). All patients who had TAC were subjected to PR. In the OD group, any clinical suggestion of persistent sepsis was an indication for relaparotomy. The findings at relaparotomy were classified as either positive or negative. Positive findings included turbid intra-abdominal fluid, purulent intra-abdominal fluid, appendix stump dehiscence, necrotising fasciitis and other pathologies including perforated stress ulcers or acalculous cholecystitis. Negative findings included minimal amounts of serous fluid with no other new findings in the abdomen.
Statistical analysis
Detailed statistical analysis was performed to compare the relaparotomy and non-relaparotomy groups. Pearson's χ2 test was used when the sample size assumption was adhered to, Fisher's exact test was utilised in cases where the χ2 assumption was not fulfilled, and the Mann-Whitney U-test was performed to identify any significant differences between the two groups after the data distributions were proven to be asymmetrical. Non-parametric (asymmetrical) data were descriptively described in terms of a median. Finally, logistic regression analysis was performed to investigate prediction of the need for relaparotomy. A range of variables were considered and included based on clinical relevance. The final remaining variables in the model were reached via a backward stepwise regression. The level of statistical significance was set at p<0.05. All statistical analysis was performed using SPSS version 21 (IBM Corp., released 2012).
Statistical model
A logistic regression analysis (backward stepwise conditional method) was conducted to predict whether a relaparotomy would occur, using specific preoperative and intraoperative data as predictors (Table 1). These data were used to generate a receiver operating curve (ROC) plotting the true-positive rate against the false-positive rate (or sensitivity v. 1- specificity). Accuracy was also measured by the area under the ROC curve (AUC).
Results
A total of 1 000 patients with intraoperatively confirmed acute appendicitis were managed from January 2008 to December 2012. Males comprised 54.1% and females 45.9% of the cohort, with a median age of 21 years. The median length of time from the onset of symptoms to seeking medical care was 4 days. Of the entire cohort, 394 (39.4%) had a local incision and 606 (60.6%) a laparotomy. A total of 405 (40.5%) had inflamed non-perforated appendicitis, while 595 (59.5%) had a perforated appendix. Of the 595 with a perforated appendix, 177 (29.7%) had localised intra-abdominal sepsis and 418 (70.3%) generalised four-quadrant sepsis. A total of 406 patients ultimately required relaparotomy. The two groups were compared, and Table 1 summarises the differences between the relaparotomy and non-relaparotomy groups. Of the 406 relaparotomies, 227 (55.9%) were PR and 179 (44.1%) OD. Of the relaparotomy group, 367 (90.4%) had positive findings at relaparotomy. Table 2 summarises the findings at relaparotomy.
Regression model
Based on the differences between the relaparotomy and non-relaparotomy groups, a number of parameters were considered for inclusion in a logistic regression model to predict the need for relaparotomy. The criteria could either be categorical (yes or no) or a discrete number. The following five variables were selected:
- Referral. Patients referred from any rural centre (present = 1, absent = 0).
- Duration. Duration (days) of illness prior to contact with healthcare system.
- Heart rate. Heart rate on admission (bpm).
- Perforation with LC. Perforation with localised contamination (present = 1, absent = 0).
- Perforation with GC. Perforation with generalised contamination (present = 1, absent = 0).
The Wald criterion demonstrated that the mode of referral (urban v. rural) (p=0.019) and perforation v. non-perforation (p<0.001) made a significant contribution to a confirmatory relaparotomy prediction.
The following multivariable logistic model was fitted incorporating the criteria listed above and resulted in the following coefficients for these predictors:
where
log it (p) = -6.116 + 0.566X1 + 0.075X2 + 0.012X3 + 2.961X4 + 5.933X5
and
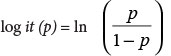
X1 = Referral; X2 = Duration; X3 = Heart rate; X4 = Perforation with LC; X5 = Perforation with GC.
Prediction success for this model overall was 90.8% (sensitivity 90.1%, specificity 91.2%). The ROC curve indicates an AUC of 0.948 (95% confidence interval 0.934 - 0.962) with a p-value of <0.001, confirming excellent performance (predictive power) of the above model. Fig. 1 shows the ROC curves for the five selected predictors and Fig. 2 the ROC curve for the combined model. A test of the full model against a constant-only model was statistically significant, indicating that the predictors as a set reliably distinguished between patients who required a relaparotomy v. those who did not (χ2=827.663; p<0.001 with 5 degrees of freedom (df)). The Hosmer and Lemeshow goodness-of-fit test indicated that the data had a good fit to the predictive model (χ2=7.442; p=0.490 with 8 df). Nagelkerke's R2of 0.760 indicated a good relationship between prediction and grouping.
Clinical model
A simplified clinical scoring system derived from the above model can be utilised. In the presence of the following four major predictive factors, there is a 90% probability that a relaparotomy is required: (i) referral from a rural centre; (ii) duration of illness >5 days; (iii) heart rate >120 bpm; and (iv) perforation with associated GC.
Discussion
In the developing world, acute appendicitis is associated with significant morbidity and even mortality as a result of late presentation and complex intra-abdominal sepsis.[1-5] The management of complex intra-abdominal sepsis is challenging, and frequently requires relaparotomy to ensure adequate source control.[7] Although literature on predictors of the need for the relaparotomy exists, most studies have been undertaken in the developed world and have not focused on a specific disease process.[8,16] Of the methods currently employed for the management of complex intra-abdominal sepsis, it has been suggested that OD relaparotomy is the most cost-effective approach.[13] A randomised study was published by van Ruler et al.[15] in 2007 comparing PR and OD approaches for patients with complex intra-abdominal sepsis. A total of 232 patients were randomised. In the PR group, relaparotomy was undertaken every 36 - 48 hours after the initial procedures until all intra-abdominal sepsis was cleared. In the OD group, relaparotomy was only performed for patients who either deteriorated clinically or failed to improve. However, the general expert consensus is that if an OD approach is adopted, early recognition of the need for further surgery is essential as delay in source control results in dramatically increased morbidity and mortality.[6,7,15,18,19] This makes a model to predict the need for relaparotomy important.[11,15]
Our proposed model allows for a predictive value of >90%. However, as the logistic regression process takes several variables into consideration in reaching the final predictive model, it should be noted that heart rate is only a weak predictor and therefore should not be considered in isolation. We believe that a simplified clinical model would be easier to use in clinical practice and that a relaparotomy is strongly advised if all of the risk factors are present. It is hoped that this would simplify the decision-making process by allowing individual surgeons to be cognisant of the key predictive factors rather than having to calculate a specific number using the mathematical model. Further prospective work is required to validate this model.
Conclusions
The management of complex intra-abdominal sepsis secondary to appendicitis is challenging and has relied on clinical judgement. Our proposed clinical scoring system accurately predicts the need for relaparotomy. When all the clinical risk factors are present, relaparotomy should be strongly advised. Further validation studies are required before widespread adoption of this scoring system into routine surgical practice.
REFERENCES
1. Kong VY, Bulajic B, Allorto NL, Handley J, Clarke DL. Acute appendicitis in a developing country. World J Surg 2012;36(9):2068-2073. [http://dx.doi.org/10.1007/s00268-012-1626-9] [ Links ]
2. Kong VY, Aldous C, Handley JJ, Clarke DL. The cost effectiveness of the early management of acute appendicitis underlies the importance of curative surgical services to a primary health care program. Ann R Coll Surg Engl 2013;95(4):280-284. [http://dx.doi.org/10.1308/003588413X13511609958415] [ Links ]
3. Kong VY, van der Linde S, Handley JJ, Aldous C, Clarke DL. Quantifying the disparity in outcome between urban and rural patients with acute appendicitis in South Africa. S Afr Med J 2013;103(10):742-745. [http://dx.doi.org/10.7196/SAMJ.7109] [ Links ]
4. Kong VY, Aldous C, Clarke DL. Understanding the reasons for delay to definitive surgical care of patients with acute appendicitis in rural South Africa. S Afr J Surg 2014;52(1):2-5. [http://dx.doi.org/10.7196/SAJS.1737] [ Links ]
5. Kong VY, van der Linde S, Aldous C, Handley JJ, Clarke DL. The accuracy of Alvarado score in predicting acute appendicitis in the black South African population needs to be validated. Can J Surg 2014;57(4):E121-E125. [http://dx.doi.org/10.1503/cjs.023013] [ Links ]
6. Sartelli M, Viale P, Catena F, et al. 2013 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg 2013;8(1):3. [http://dx.doi.org/10.1186/1749-7922-8-3] [ Links ]
7. Van Ruler O, Lamme B, De Vos R, et al. Decision making for relaparotomy in secondary peritonitis. Dig Surg 2008;25(5):339-346. [http://dx.doi.org/10.1159/000158911] [ Links ]
8. Schein M. Planned reoperations and open management in critical intra-abdominal infections: Prospective experience in 52 cases. World J Surg 1991;15(4):537-545. [http://dx.doi.org/10.1007/BF01675658] [ Links ]
9. Hutchins RR, Gunning MP, Lucas DN, et al. Relaparotomy for suspected intraperitoneal sepsis after abdominal surgery. World J Surg 2004;28(2):137-141. [http://dx.doi.org/10.1007/s00268-003-7067-8] [ Links ]
10. Lamme B, Mahler CW, van Ruler O, et al. Clinical predictors of ongoing infection in secondary peritonitis: Systematic review. World J Surg 2006;30(12):2170-2181. [http://dx.doi.org/10.1007/s00268-005-0333-1] [ Links ]
11. Lamme B, Boermeester MA, Belt EJ, et al. Mortality and morbidity of planned relaparotomy versus relaparotomy on demand for secondary peritonitis. Br J Surg 2004;91(8):1046-1054. [http://dx.doi.org/10.1002/bjs.4517] [ Links ]
12. Bosscha K, Hulstaert PF, Visser MR, et al. Open management of the abdomen and planned reoperations in severe bacterial peritonitis. Eur J Surg 2000;166(1):44-49. [http://dx.doi.org/10.1080/110241500750009690] [ Links ]
13. Lamme B, Boermeester MA, Reitsma JB, et al. Meta-analysis of relaparotomy for secondary peritonitis. Br J Surg 2002;89(12):1516-1524. [http://dx.doi.org/10.1046/j.1365-2168.2002.02293.x] [ Links ]
14. Bader FG, Schroder M, Kujath P, et al. Diffuse postoperative peritonitis - value of diagnostic parameters and impact of early indication for relaparotomy. Eur J Med Res 2009;14(11):491-496. [http://dx.doi.org/10.1186/2047-783X-14-11-491] [ Links ]
15. Van Ruler O, Mahler CW, Boer KR, et al. Comparison of on-demand vs planned relaparotomy strategy in patients with severe peritonitis: A randomized trial. JAMA 2007;298(8):865-872. [http://dx.doi.org/10.1001/jama.298.8.865] [ Links ]
16. Clarke DL, Thomson SR, Bissetty T, et al. A single surgical unit's experience with abdominal tuberculosis in the HIV/AIDS era. World J Surg 2007;31(5):1087-1096; discussion 1097-8. [http://dx.doi.org/10.1007/s00268-007-0402-8] [ Links ]
17. Van Ruler O, Lamme B, Gouma DJ, et al. Variables associated with positive findings at relaparotomy in patients with secondary peritonitis. Crit Care Med 2007;35(2):468-476. [http://dx.doi.org/10.1097/01.CCM.0000253399.03545.2D] [ Links ]
18. Mulier S, Penninckx F, Verwaest C, et al. Factors affecting mortality in generalized postoperative peritonitis: Multivariate analysis in 96 patients. World J Surg 2003;27(4):379-384. [http://dx.doi.org/10.1007/s00268-002-6705-x] [ Links ]
19. Koperna T, Schulz F. Relaparotomy in peritonitis: Prognosis and treatment of patients with persisting intraabdominal infection. World J Surg 2000;24(1):32-37. [http://dx.doi.org/10.1007/s002689910007] [ Links ]
 Correspondence:
Correspondence:
V Y Kong
(victorywkong@yahoo.com)














