Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.51 n.4 Cape Town Jan. 2013
CASE REPORT
Gastric heterotopia causing jejunal ulceration and obstruction
G E ChinneryI; M M BernonI; M A BanderkerI; R RobertsII; J E J KrigeI
ISurgical Gastroenterology Unit, Department of Surgery, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, South Africa
IIDivision of Anatomical Pathology and National Health Laboratory Services, Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
A young woman with persistent postprandial vomiting was found to have a high-grade proximal jejunal stricture. The stricture was surgically excised, and histopathological examination showed gastric heterotopia with localised ulceration and fibrosis. Symptomatic gastric heterotopia in the small bowel is rare, and to our knowledge this is the first report of jejunal gastric heterotopia resulting in ulceration with subsequent stricturing and obstruction.
Case report
A 17-year-old girl presented to her local hospital with persistent projectile bile-stained postprandial vomiting of 3 months' duration. She had lost 15 kg in weight during this period. She had no prior medical history besides having recently delivered her first child after an uneventful pregnancy. The vomiting had started soon after the birth. On examination the only finding was a gastric succussion splash. Gastroscopy confirmed a distended stomach with residual bile-stained gastric content and a normal upper gastrointestinal tract to the third part of the duodenum.
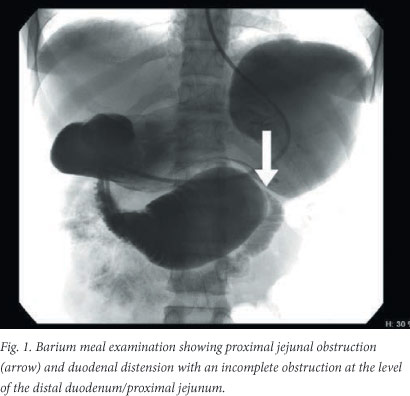
At Groote Schuur Hospital (Cape Town, South Africa) a contrast meal and follow-through study showed a proximal near-complete jejunal obstruction (Fig. 1). Superior mesenteric artery syndrome (Wilkie syndrome) was excluded, as the level of obstruction demonstrated on the contrast study was beyond the midline and the history was not compatible.
At operation, a high-grade proximal jejunal stricture 2 cm in length was found 15 cm distal to the ligament of Treitz (Fig. 2). Localised inflammatory adhesions were released to expose the stricture. The stricture was resected and gastrointestinal continuity restored with an end-to-side jejunojejunostomy to accommodate the differences in bowel diameter. Local mesenteric lymph nodes were included in the resection to exclude abdominal tuberculosis. The patient had no further vomiting after the operation and was discharged home on day 7.

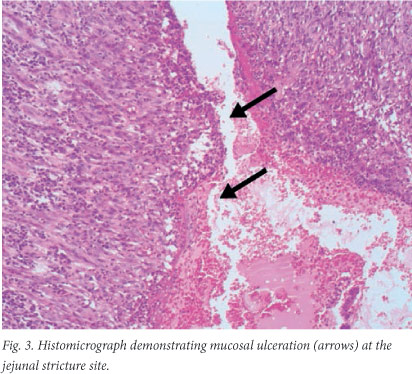
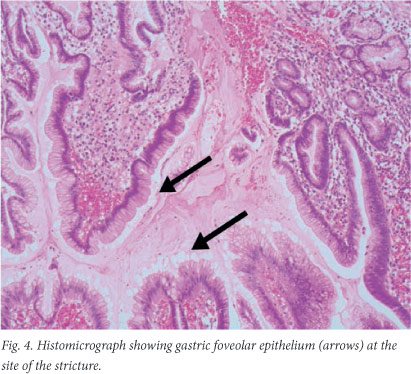
Histological examination of the specimen showed jejunal gastric heterotopia. Sections of the resected small intestine showed extensive mucosal ulceration, extending deep into the submucosa (Fig. 3). Where mucosa was preserved, gastric foveolar epithelium was present, overlying a thickened muscularis mucosa (Fig. 4). Additionally, dense submucosal fibrosis with luminal narrowing and serosal adhesions were noted. There was no evidence of dysplasia or malignancy. The lymph nodes showed reactive lymphoid hyperplasia.
Discussion
Gastric heterotopia is either congenital or acquired, is usually benign and asymptomatic, and is defined as the presence of normal gastric mucosa in an abnormal location.[1] While gastric heterotopia has been reported anywhere within the length of the gastrointestinal tract, from the oropharynx to the anorectal canal, it is most common in the oesophagus and, excluding a Meckel's diverticulum or intestinal duplication, is rarely found beyond the ligament of Treitz. Other unusual sites reported include the salivary glands, biliary ducts and gallbladder, umbilicus and respiratory tract, bronchogenic and thyroglossal cysts, the spinal column, intra-abdominal and intrathoracic locations, and the urinary bladder and scrotum.[2]
Congenital gastric heterotopia may be associated with other entities such as a Meckel's diverticulum or duplications; it is believed that these lesions develop from the primitive gut epithelium as a congenital anomaly, becoming hyperplastic over time.[3]
Genta et al.[4] hypothesised that in acquired lesions, hyper-gastrinaemia induced by proton pump inhibitors may result in hyperplasia of congenital microscopic foci of ectopic gastric fundal tissue, resulting in macroscopic lesions. There does not appear to be an association with Helicobacter pylori.[4,5]
While gastric heterotopia is generally an asymptomatic and incidental finding, there are reports of patients presenting with bleeding, perforation, intermittent intussusception or intestinal obstruction and pain.[1-7] Symptomatic gastric heterotopia has rarely been reported in the small bowel beyond the ligament of Treitz, and if present usually consists of single polypoid mass lesions a few centimetres from the ligament of Treitz, with potential to cause intermittent intussusception.[1,6,7] The usual presenting age is around 14 years.[6] While jejunal gastric heterotopia may present with a clinical spectrum related to peptic ulceration, including acute or chronic bleeding with anaemia, perforation and intussusception, to our knowledge this is the first report of jejunal gastric heterotopia resulting in ulceration with subsequent jejunal stricturing and obstruction.
REFERENCES
1. Khan MJ, Mullerat P, Desai A. A polypoid gastric heterotopia of jejunum diagnosed by capsule endoscopy. J Coll Physicians Surg Pak 2009;19(10):661-662. [ Links ]
2. Heo YS, Jeong SY, Son SW, et al. Heterotopic gastric mucosa in the umbilicus. Ann Dermatol 2010;22(2):223-225. [http://dx.doi.org/10.5021/ad.2010.22.2.223] [ Links ]
3. Jimenez JC, Emil S, Steinmetz B, et al. Recurrent gastrointestinal tract bleeding secondary to jejunal gastric heterotopia. J Pediatr Surg 2005;40(10):1654-1657. [ Links ]
4. Genta RM, Kinsey RS, Singhal A, Suterwala S. Gastric foveolar metaplasia and gastric heterotopia in the duodenum: No evidence of an etiological role for Helicobacter pylori. Hum Pathol 2010;41(11):1593-1600. [http://dx.doi.org/10.1016/j.humpath.2012.04.010] [ Links ]
5. Conlon N, Logan E, Veerappan S, et al. Duodenal gastric heterotopia: Further evidence of an association with fundic gland polyps. Hum Pathol 2013;44(4):636-642. [http://dx.doi.org/10.1016/j.humpath.2012.07.014] [ Links ]
6. Boybeyi O, Karna I, Gucers S, et al. Common characteristics of jejunal heterotopic gastric tissue in children: A case report with review of the literature. J Pediatr Surg 2008;43(7):e19-22. [http://dx.doi.org/10.1016/j.jpedsurg.2008.02.072] [ Links ]
7. Omotosho PA, Varnholt H, Tirabass MV et al. Giant polypoid gastric heterotopia of the jejunum presenting with intermittent intussusception. Journal of Laparoendoscopic and Advanced Surgical Techniques 2007;17(2):249-251. [http://dx.doi.org/10.1089/lap.2006.0071] [ Links ]
 Correspondence:
Correspondence:
G E Chinnery
(galyachinnery@gmail.com)














