Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.51 no.4 Cape Town Jan. 2013
GENERAL SURGERY
Using a structured morbidity and mortality meeting to understand the contribution of human error to adverse surgical events in a South African regional hospital
D L Clarke; H Furlong; G L Laing; C Aldous; S R Thomson
Department of General Surgery, Edendale Hospital, Pietermaritzburg Metropolitan Complex, and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Several authors have suggested that the traditional surgical morbidity and mortality meeting be developed as a tool to identify surgical errors and turn them into learning opportunities for staff. We report our experience with these meetings.
METHODS: A structured template was developed for each morbidity and mortality meeting. We used a grid to analyse mortality and classify the death as: (i) death expected/death unexpected; and (ii) death unpreventable/death preventable. Individual cases were then analysed using a combination of error taxonomies.
RESULTS: During the period June - December 2011, a total of 400 acute admissions (195 trauma and 205 non-trauma) were managed at Edendale Hospital, Pietermaritzburg, South Africa. During this period, 20 morbidity and mortality meetings were held, at which 30 patients were discussed. There were 10 deaths, of which 5 were unexpected and potentially avoidable. A total of 43 errors were recognised, all in the domain of the acute admissions ward. There were 33 assessment failures, 5 logistical failures, 5 resuscitation failures, 16 errors of execution and 27 errors of planning. Seven patients experienced a number of errors, of whom 5 died.
CONCLUSION: Error theory successfully dissected out the contribution of error to adverse events in our institution. Translating this insight into effective strategies to reduce the incidence of error remains a challenge. Using the examples of error identified at the meetings as educational cases may help with initiatives that directly target human error in trauma care.
The realisation that error contributes significantly to mortality and morbidity in trauma and acute-care surgery has generated interest in quality improvement initiatives that directly target human error.[1-6] The starting point for the development of appropriate quality improvement programmes is to create a mechanism to identify cases of error. Once the error has been recognised, it needs to be dissected using an appropriate taxonomy. This will facilitate understanding of the problem and has the potential for the development of appropriate error reduction interventions. The traditional forum for identifying and discussing surgical complications is the morbidity and mortality meeting.
The traditional morbidity and mortality meeting has not been an effective driver of improved patient safety. In 2003, Pierluissi et al.[7] reported their audit of these meetings at four US medical schools. Error was discussed at 10% of the internal medicine meetings and at 34% of all surgical meetings. Internal medicine meetings tended to focus on didactic lectures, whereas the surgical meetings focused on case presentations and discussion. Although surgical residents were exposed to discussion on error more frequently than their counterparts in internal medicine, in both disciplines error was infrequently discussed or even acknowledged. Several authors have attempted to use the morbidity and mortality meeting to highlight error and patient safety. Unstructured meetings are unlikely to provide such a platform and often degenerate into an overview of the literature on a particular topic. We therefore attempted to develop a structured morbidity and mortality meeting that focuses on assessing the contribution of error in its totality to an adverse event. The objective of these restructured meetings is to separate adverse outcomes into those that are a direct consequence of the pathology being treated, and those that are a result of error. Once the error has been identified we seek to analyse the cause, using a modern taxonomy of error. These data are collated at the end of the semester and reviewed with the intention of identifying the common themes in error and developing targeted strategies to attempt to prevent or reduce the incidence of error in the future.
This report discusses our experience with these structured morbidity and mortality meetings and attempts to classify our findings.
Methods
Previously, the surgical morbidity and mortality meetings were run by each individual surgical unit. The meetings were unstructured, and involved the unit concerned listing all the patients admitted and operated on for the previous month. Each death was discussed and any complications were listed and discussed. A single complication was then discussed in depth and a brief overview of the academic literature on the topic was given.
A new structured format was introduced in June 2011. The morbidity and mortality meeting is now run by a dedicated moderator and presenter who works in the acute ward of the hospital. The acute team looks after all high-risk patients who do not qualify for admission to the formal intensive care unit (ICU) or high-care unit. Surgical care is undertaken by the admitting surgical team. This means that the presenter has a good knowledge of all high-risk patients and the patients who experience morbidity, but is not directly involved in their surgery, so reducing bias.
A standard PowerPoint template is used for each meeting. This consists of a table that divides the week's admissions into trauma and non-trauma admissions. The next two slides list all the transfers out of the acute ward, either to the ICU or to another institution, and all the transfers or down-referrals into the acute ward from the ICU. The rest of the presentation lists all the recorded morbidity and mortality for the week.
Analysing mortality
Mortality data are obtained from the ward and the accident and emergency registers. We used a grid to analyse mortality and classify it as (i) death expected/death unexpected; and (ii) death unpreventable/ death preventable. The initial classification of the death is established by the moderator and the trainee who presents the meeting. At the meeting, which is attended by senior staff, the classification is discussed and consensus is reached. This is then recorded as the final classification.
Analysing morbidity
Morbidity data are obtained by monitoring sentinel events, including unexpected patient returns to the operating theatre, re-admissions to the acute ward or the ICU, and surgical site sepsis. Morbidity is identified from self-reporting by the surgical team concerned as well as by analysis of morning hand-over data, theatre emergency list data and ICU admission data. The moderator and presenter classify each adverse event as pathology-related, error-related or combined adverse events. An error is defined as failure of a planned action to be completed as intended, or use of a wrong plan to achieve an aim. An error-related adverse event is defined as an unintentional, definable injury that is the result of medical management. Error-related adverse events are subjected to a detailed analysis.
Dissecting out error
Once an adverse event has been classified as either error-related or combined, the individual case is analysed using modern error taxonomies. We have modified Chang's taxonomy,[2] which the Joint Commission on Accreditation of Healthcare Organizations adopted to produce a standardised nomenclature for the taxonomy of adverse outcomes. This taxonomy classifies error into five complementary root nodes, which equate to the general descriptive terms in parentheses below.
Impact (How bad was the error?). The degree of harm experienced as a result of the error.
Type (What went wrong?). This refers to the processes of care that failed. We divide the processes of care into broad categories, namely errors of resuscitation, errors of assessment, operative or technical error, and logistical failure. A patient may experience any number of combinations of failed processes.
Domain (Where did it go wrong?). In this report, the errors occurred in the acute-care ward of the hospital.
Cause (Why did it go wrong?). We divide the causes into errors of planning, errors of execution, errors of omission (failure to undertake a necessary action), and errors of commission (the performance of an inappropriate action). Resuscitation and logistical failures are errors of execution, while assessment failures are errors of planning.
Prevention (What are we going to do about it?). All error reduction programmes need to develop interventions to reduce the incidence of error and to limit its effect.
Results
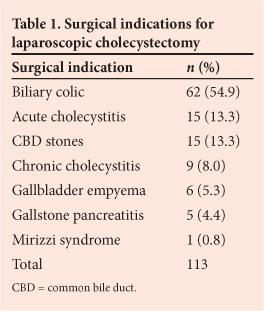
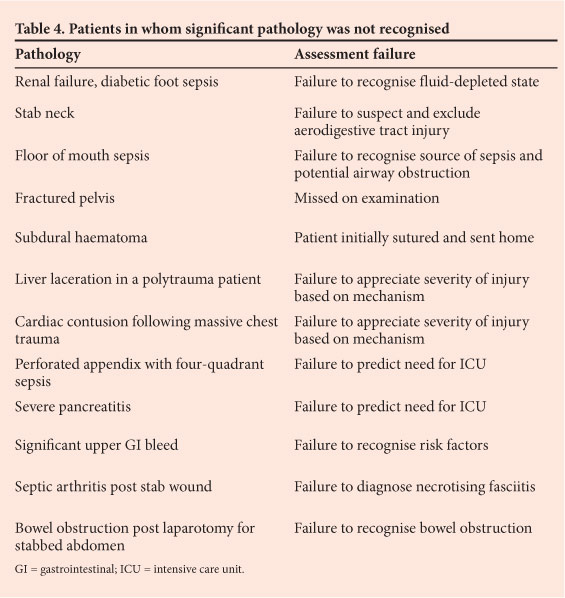
During the period June - December 2011, a total of 400 patients were managed by the acute admissions firm at Edendale Hospital, Pietermaritzburg, South Africa. There were 195 trauma admissions and 205 non-trauma admissions. During this period, a total of 20 morbidity and mortality meetings were held, and a total of 43 process errors were recognised and discussed. Table 1 summarises the attribution of errors presented at our meetings, using Chang's taxonomy. The vast majority were assessment failures, with logistical and resuscitation failures accounting equally for the remaining 23.2%. There were 35 errors of omission, 8 errors of commission, 16 errors of execution and 27 errors of planning. We did not identify any technical or operative errors in this period. There were 10 deaths, of which 5 were unexpected and potentially avoidable (Table 2). Of the 7 patients who experienced multiple errors (Table 3), 5 died. There were 8 drug-related errors. Drugs were not given when they ought to have been given in 6 cases, and a patient with acute renal impairment was given a non-steroidal anti-inflammatory drug; the same patient experienced opioid toxicity (Table 3). In 4 cases, the radiologist reported a computed tomography scan as normal and missed significant pathology, and in 12 cases staff failed to recognise significant pathology. These are errors of assessment, and are listed in Table 4. Failure to associate pathology with the mechanism of injury, or complications with the surgery performed, were the most common problems. Logistical failures included miscommunication about the availability of an ICU bed and miscommunication during the transfer of patients between hospitals in the metropolitan complex.
Discussion
Since the turn of the millennium when the Institute of Medicine (IOM) released the monograph To Err is Human: Building a Safer Health System}[1] there has been much interest in the issue of error in healthcare. The IOM recommended that, when discussing error, we should recreate the story and attempt to understand the meaning of the error. This will allow the development of strategies to reduce the incidence of error. The morbidity and mortality meeting is ideally placed to fulfil this role. We have attempted to use current taxonomies of error to help analyse the errors identified in our meetings.[18-12]
Assessment failure was the biggest source of error in this series. Junior staff tend to see what they know and make what they see fit their preconceived view of reality. We have commented on this tendency to ignore alterations in clinical signs and early mild changes in laboratory results rather than act upon them.[13-15] The phenomenon of cognitive dissonance helps to explain this finding.
Decision making is a complex process, and human beings have a tendency to make a superficial assessment and then resist prompts that should make them reconsider their initial assessment[16-19] Our findings are consistent with previously published data on error and on human decision making. If we are going to err, we would prefer to err by not acting than by acting. This is illustrated by the finding in our study that errors of omission far outweigh errors of commission. The psychological tendency to stick with an incorrect assessment and persist with a predetermined course of action needs to be addressed in surgical education. Table 1 summarises the potentially preventable deaths in our series. The common theme in all the preventable deaths is one of staff not appreciating the significance of a clinical scenario. Not understanding the tenuous nature of a swollen infected upper airway resulted in a death. Not appreciating the importance of postoperative intensive care for elderly patients with several comorbidities requiring surgery resulted in 2 deaths. Failure to realise that new signs of sepsis after gastrectomy may herald anastomotic breakdown shows limited understanding of gastrointestinal surgery.
Table 4 summarises the 12 cases in which failure to make the correct diagnosis contributed to the adverse events. There were 4 trauma cases in which staff did not make the connection between the mechanism of the trauma and the potential injuries. Massive blunt chest trauma can result in a cardiac contusion. Similarly, a penetrating wound of the neck can result in an aerodigestive tract injury. Based on the mechanism and history alone, the managing staff should elevate their level of concern and dramatically increase either the level of investigation or the level of care. Working in a busy, under-resourced environment reduces the time available to thoroughly assess and properly manage these patients. This almost certainly contributed to the death of a patient with a subdural haematoma who was inappropriately discharged. Adverse events frequently revolved around the failure to associate a clinical diagnosis with systemic pathology. Sepsis of the floor of the mouth can lead to an obstructed airway, and diabetic sepsis is associated with gross fluid depletion.
The concept of an error cascade refers to the fact that a final poor outcome is often the result of the interaction of numerous factors (Table 3). Once the initial error occurs, it is reinforced by other errors. For example, the diabetic patient with a septic foot was not given sufficient fluid. This error was compounded by two drug-related errors, namely administration of non-steroidal anti-inflammatory drugs in the setting of renal dysfunction, and excessive administration of opioids. The staff did not appreciate that renal dysfunction may result in the decreased clearance of opioids. The mortality rate in the group of patients who suffered an error cascade was high at 71.4% (5/7).
While it is clear that our previous reliance on self-reporting of morbidity by individual units was inadequate,[20,21] a tendency to under-report morbidity remains a problem, as implied by the fact that we did not detect any technical errors in this series. Identifying and developing mechanisms such as sentinel event monitoring to capture morbidity ensures that most significant morbidity will be discussed at the meeting. Ideally, the culture of an organisation should be one in which adverse events are self-reported, but this is difficult to achieve. Developing mechanisms to reduce the errors we have identified requires creative and innovative approaches. It is unlikely that the resources available to us will increase or that the burden of pathology we treat will decrease. This means that we are left with altering the process of care. There are several ways to do this: attempting to restructure the ergonomics of the patient care situation (e.g. by establishing an acute-care ward with dedicated staff to care for all new admissions) as well as ongoing targeted educational programmes. The data from our ongoing morbidity and mortality meetings are a useful starting point for such programmes.
Conclusion
By using a structured format, we have been able to dissect out the human error involved in adverse surgical events in our institution. We have formalised our mechanisms to capture morbidity, have found the available taxonomies to be appropriate and user friendly, and have confirmed that the most common errors are those of assessment and omission. This is in keeping with the literature on error from healthcare and other high-risk environments. Although we suspect that a problem with under- or non-reporting of technical errors still exists, we are beginning to develop an understanding of error in acute care. The challenge is to use this understanding to develop strategies to prevent or limit the impact of errors. Incorporating error training into educational courses is a potential strategy, and cases highlighted at our meetings can be converted into compact case studies for use by small focus groups.
REFERENCES
1. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press, 2000. [ Links ]
2. Chang A, Schyve PM, Croteau RJ, O'Leary DS, Loeb JM. The JCAHO patient safety event taxonomy: A standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care 2005;17(2):95-105. [http://dx.doi.org/10.1093/ intqhc/mzi021- [ Links ]
3. Leape LL. Error in medicine. JAMA 1994;272(23):1851-1857. [http://dx.doi.org/10.1001/jama.272.23.18511 [ Links ]
4. Davis JW, Hoyt DB, McArdle MS, Mackersie RC, Shackford SR, Eastman AB. The significance of critical care errors in causing preventable death in trauma patients in a trauma system. J Trauma 1991;31(6):813-818; discussion 818-819. [http://dx.doi.org/10.10/00005373-199106000-000121 [ Links ]
5. Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: Lessons learned from 2,594 deaths. Ann Surg 2006;244(3):371-380. [ Links ]
6. Teixeira PG, Inaba K, Hadjizacharia P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma 2007;63(6):1338-1346; discussion 1346-1347. [http://dx.doi.org/10.1097/TA.0b013e31815078ae] [ Links ]
7. Pierluissi E, Fischer MA, Campbell AR, Landefeld CS. Discussion of medical errors in morbidity and mortality conferences. JAMA 2003;290(21):2838-2842. [http://dx.doi.org/10.1001/jama.290.21.2838] [ Links ]
8. Rosenfeld JC. Using the morbidity and mortality conference to teach and assess ACGME general competencies. Curr Surg 2005;62(6):664-669. [http://dx.doi.org/10.1016/j.cursur.2005.06.009] [ Links ]
9. Risucci DA, Sullivan T, DiRusso S, Savino JA. Assessing educational validity of the morbidity and mortality conference: A pilot study. Curr Surg 2003;60(2):204-209. [http://dx.doi.org/10.1016/S0149-7944(02)00735-3] [ Links ]
10. Prince JM, Vallabhaneni R, Zenati MS, et al. Increased interactive format for morbidity and mortality conference improves educational value and enhances confidence. J Surg Educ 2007;64(5):266-272. [http://dx.doi.org/10.1016/j.jsurg.2007.06.007] [ Links ]
11. Abdulrasheed I, Zira DI, Eneye AM. Modification of the surgical morbidity and mortality meetings as a tool to improve patient safety. Oman Med J 2011;26(4):290-292. [http://dx.doi.org/10.5001/omj.2011.72] [ Links ]
12. Gordon LA. Rediscovering the power of the surgical M&M conference: The M+M matrix. Morbidity and mortality rounds on the web. http://www.webmm.ahrq.gov/perspectives.aspx (accessed 15 July 2012). [ Links ]
13. Alexander T, Fuller G, Hargovan P, Clarke DL, Muckart DJ, Thomson SR. An audit of the quality of care of traumatic brain injury at a busy regional hospital in South Africa. S Afr J Surg 2009;47(4):120- 122, 124-126. [ Links ]
14. Stewart WW, Farina Z, Clarke DL, Thomson SR. Variations in levels of care within a hospital provided to acute trauma patients. S Afr J Surg 2011;49(4):194-198. [ Links ]
15. Clarke DL, Gouveia J, Thomson SR, Muckart DJ. Applying modern error theory to the problem of missed injuries in trauma. World J Surg 2008;32(6):1176-1182. [http://dx.doi.org/10.1007/s00268-008-9543-7] [ Links ]
16. Perkinson HJ. Learning from our mistakes. Et Cetera 1979;36:37-57. [ Links ]
17. Bransford J, Brown AL, Cocking RR, eds. How people learn: Brain, Mind, Experience and School. Washington, DC: National Academy Press, 2000 [ Links ]
18. Boks CL. Forgive and Remember: Managing Medical Failure. Chicago, Ill.: University of Chicago Press, 1979. [ Links ]
19. Hallinan JT. Why We Make Mistakes: How We Look Without Seeing, Forget Things in Seconds, and Are All Pretty Sure We Are Way Above Average. New York: Broadway Books, 2009. [ Links ]
20. Reason J. Understanding adverse events: Human factors. Qual Health Care 1995;4:80-89. [http://dx.doi.org/10.1136/qshc.4.2.80] [ Links ]
21. Reason J. Human error: Models and management. BMJ 2000;320(7237):768-770. [http://dx.doi.org/10.1136/bmj.320.7237.768] [ Links ]
 Correspondence:
Correspondence:
D L Clarke
(damianclar@gmail.com)














