Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.51 no.4 Cape Town Jan. 2013
GENERAL SURGERY
Endoscopic management of bile leaks after laparoscopic cholecystectomy
G E Chinnery; J E J Krige; P C Bornman; M M Bernon; S Al-Harethi; S Hofmeyr; M A Banderker; S Burmeister; S R Thomson
Surgical and Medical Gastroenterology Units, Groote Schuur Hospital and Departments of Surgery and Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: A bile leak is an infrequent but potentially serious complication after biliary tract surgery. Endoscopic intervention is widely accepted as the treatment of choice. This study assessed the effectiveness of endoscopic retrograde cholangiopancreatography (ERCP), sphincterotomy and biliary stenting in the management of postoperative bile leaks.
METHODS: An ERCP database in a tertiary referral centre was reviewed retrospectively to identify all patients with bile leaks after laparoscopic cholecystectomy. Patient records and endoscopy reports were reviewed.
RESULTS: One hundred and thirteen patients (92 women, 21 men; median age 47 years, range 22 - 82 years) with a bile leak were referred for initial endoscopic management at a median of 12 days (range 2 - 104 days) after surgery. Presenting features included intra-abdominal collections with pain in 58 cases (51.3%), abnormal liver function tests (LFTs) in 22 (19.5%), bile leak in 25 (22.1%), and sepsis in 8 (7.1%). Twenty-nine patients (25.7%) were found to have either major bile duct injuries without duct continuity, vascular injuries or other endoscopic findings requiring surgical or radiological intervention. Of 84 patients managed endoscopically, 44 had a cystic duct (CD) leak, 26 a CD leak and common bile duct (CBD) stones, and 14 a CBD injury amenable to endoscopic stenting. Of the 70 patients with CD leaks (group A), 24 underwent sphincterotomy only (including 8 stone extractions), 43 had a sphincterotomy with stent placement (including 18 stone extractions) and 1 had only a stent placed, while 2 patients with previous sphincterotomies required no further intervention. The average number of ERCPs in group A was 2.3 (range 1 - 7). Of the 14 patients with bile duct injuries treated endoscopically (group B), 7 had a class D, 5 an E5 and 2 a class B injury; 13 patients underwent sphincterotomy and stenting, and 1 had a sphincterotomy only. Group B required an average of 3.6 ERCPs (range 2 - 5). The 113 patients underwent a total of 269 ERCPs (mean 2.4, range 1 - 7). Seven patients had one or more complications related to the ERCP: 3 acute pancreatitis, 2 cholangitis, 2 sphincterotomy bleeds, 1 duodenal perforation and 1 impacted Dormia basket, the latter 2 requiring operative intervention.
CONCLUSIONS: Three-quarters of bile leaks after laparoscopic cholecystectomy were due to CD leaks (with or without retained stones) or lesser bile duct injuries and were amenable to definitive endoscopic therapy. Nineteen patients (16.8%) had major injuries that required operative intervention.
Laparoscopic cholecystectomy is the preferred and most widely used method of removal of the gallbladder in patients with symptomatic cholelithiasis. Although the technique was introduced more than 20 years ago, bile duct injuries occurring as a consequence of the procedure remain a major problem in surgical practice. Bile leaks after laparoscopic cholecystectomy represent a spectrum of extrahepatic biliary duct injuries, and range in severity from minor cystic duct (CD) leaks to complete transection of the common bile duct (CBD). Once a bile duct leak or injury is identified, the principles of management are well defined and include effective drainage of intra-abdominal collections and detailed cholangiographic evaluation of the biliary system.[1,2] In patients who have a CD leak or a side-hole in the bile duct, an operation may be avoided by either endoscopic or radiological biliary stenting if biliary continuity is present.[3-6] If a major duct injury has occurred and operative treatment is necessary, repair by a surgeon with expertise in biliary reconstructive surgery will be necessary.
An important factor limiting morbidity is early recognition of the injury and appropriate intervention to prevent the potentially life-threatening complications of bile peritonitis, sub-hepatic abscesses, interloop and intra-abdominal sepsis and cholangitis, or the later secondary sequelae of biliary cirrhosis, portal hypertension and end-stage liver disease. There is consensus that optimal management of a bile duct injury requires multidisciplinary management by surgeons, endoscopists and interventional radiologists.[3]
We aimed to evaluate the effectiveness of endoscopic retrograde cholangio-pancreatography (ERCP), sphincterotomy and biliary stenting in the management of biliary fistulas after laparoscopic chole-cystectomy.
Methods
A prospectively maintained ERCP database in a tertiary referral gastrointestinal endoscopy unit was retrospectively reviewed to identify all patients who had a bile leak after laparoscopic cholecystectomy between January 1991 and December 2011. Patients who developed a bile leak after conversion from a laparoscopic procedure to an open cholecystectomy were excluded from the study.
Patient demographics, indication for the cholecystectomy, details of intra-operative difficulties, postoperative presentation of the bile leak, investigations used and initial management by the referring surgeon were reviewed.
Bile duct injuries demonstrated at ERCP were classified according to the Strasberg grading system[7] (Fig. 1) and assessed with regard to their endoscopic management and outcome. The number of ERCPs required for bile leak resolution and complications that occurred after the endoscopic intervention were analysed.

ERCP procedure
Clotting profile and renal function were corrected before endoscopy and all patients received prophylactic antibiotics before and after ERCP. ERCP was performed under conscious sedation using midazolam and fentanyl or pethidine or (if necessary) propofol, or under general anaesthesia administered by anaesthetists. The CBD was selectively cannulated using a sphincterotome and a 0.035-inch hydrophilic guidewire (Boston Scientific, Natick, MA, USA). If initial attempts at cannulation were unsuccessful, sphincterotomy was performed using a needle knife to facilitate access to the bile duct. Once biliary access was achieved, cholangiography was used to demonstrate the biliary anatomy and the presence of a leak, stricture or retained stones was noted. An endoscopic sphincterotomy (ES), sphincterotomy and stenting or stenting alone was performed according to the endoscopic biliary findings. For biliary stenting, 10 French (10 Fr) plastic stents were routinely used. External drains were removed 2 days after cessation of bile drainage. If bile drainage had not reduced by day 3, further imaging with computed tomography intravenous cholangiography or magnetic resonance cholangiopancreatography (MRCP) was performed to ensure that no major biliary injury or transected accessory ducts had been overlooked. Repeat ERCP was performed 6 weeks after resolution of the biliary leak. Cholangiography was used to confirm healing of the biliary fistula and absence of a biliary stricture or residual stones. If a balloon cholangiogram performed after stent removal was normal, the plastic stent was not replaced. Statistical analysis was performed using the Fisher's and chi-square tests. A p-value
Results
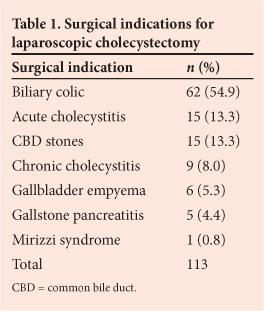
Between January 1991 and December 2011, 220 patients were referred with a bile leak following cholecystectomy. Of these patients, 113 presented with bile leaks after a laparoscopic cholecystectomy and 107 after an open cholecystectomy, including 35 conversions from laparoscopic to open cholecystectomy. For the purposes of this study, patients with bile leaks following open surgery were excluded from further analysis. One hundred and thirteen patients (92 women, 21 men; mean age 47 years, range 22 - 82 years) were referred for their initial endoscopic management at a median of 12 days (range 2 - 104 days, 25th centile 5 days, 50th centile 8.5 days, 75th centile 17 days) after laparoscopic cholecystectomy. The indication for laparoscopic cholecystectomy in most patients was symptomatic biliary colic (Table 1). In 52 patients (46.0%), the surgeon reported a difficult laparoscopic procedure owing to adhesions and difficulty in identifying biliary anatomy. Nine patients underwent intra-operative cholangiograms, 6 of which were helpful in confirming suspected CBD stones; 3 were performed for unclear anatomy, and only 1 indicated a possible injury to the biliary tree. In only 8 of the 113 patients (7.1%) was a bile duct injury suspected intra-operatively, in 7 cases due to free bile in the operative field, and 1 patient was suspected of having aberrant anatomy. Six of the 8 biliary tree injuries identified intra-operatively were reported to have been associated with difficult procedures. Of the 33 patients who sustained an injury more significant than a type A injury, 11 were reported by the operating surgeon to have had difficult cholecystectomies; however, this finding was not found to be significant (p=0.0989). The remaining 61 patients (54.0%) underwent a routine laparoscopic cholecystectomy.
The initial presenting features of the postoperative bile leak were an intraabdominal collection with pain in 58 patients (51.3%), bile leakage through a drain or the surgical wound in 25 (22.1%), abnormal liver function tests (LFTs) in 22 (19.5%), and sepsis in 8 (7.1%). Thirty-six patients had an ERCP as their primary postoperative intervention, the majority of whom presented with a bile leak or abnormal LFTs. Fifty-eight patients initially had an abdominal ultrasound scan and 28 had abdominal computed tomography before referral for endoscopic management (some patients had both). Forty patients had a percutaneous drain placed for intra-abdominal collection drainage pre-endoscopy. Two patients were referred after a bile leak was noted at relaparoscopy or laparotomy. Eight patients had internal catheters placed via percutaneous transhepatic cholangiography (PTC) before being referred for endoscopy. MRCP was performed pre-endoscopy in 3 patients, indicating the presence of retained CBD stones with CD leaks in all cases.
All 113 patients in this study underwent endoscopy. In 84 patients (74.3%) the bile leak was successfully managed endo-scopically. Seventy patients had a leak from the CD stump (group A); of these, 44 had a CD stump leak alone, while 26 had a CD stump leak in association with one or more retained CBD stones. Fourteen patients had minor CBD injuries amenable to endoscopic stenting (group B).
The 70 patients in group A either had a sphincterotomy alone with or without stone extraction or a sphincterotomy with or without stone extraction and placement of 10 Fr removable plastic stents (Table 2). Patients underwent a repeat ERCP after 6 weeks for stent retrieval. The median number of ERCPs required by the 70 patients in group A was 2 (range 1 - 7) for resolution of the leak with a clear duct; this includes subsequent removal of the stent. The 44 patients in this group with a CD leak only underwent sphincterotomy or sphincterotomy and stenting according to the endoscopist's preference. An 88% successful leak closure rate after initial ERCP was achieved with sphincterotomy alone compared with a 74% success rate after sphincterotomy and stenting.
Patients in group B with minor bile duct injuries included 2 class B, 7 class D and 5 class E5 injuries. While true type B injuries consisting of segmental branch ligations are not managed endoscopically, 1 patient with a segment 6/7 duct ligation also had a side leak from the right main duct demonstrated at PTC, which resolved after sphincterotomy and stenting. The second patient had a sphincterotomy and stent placed for a bile leak initially of undefined origin. During the repeat ERCP a leak was identified from a transected segment 5 duct, which resolved spontaneously.
Thirteen patients had a sphincterotomy and biliary stentings, and 1 patient's leak resolved after spincterotomy alone (Table 2). Group B patients required a median of 4 ERCPs (range 2 - 5) for resolution.
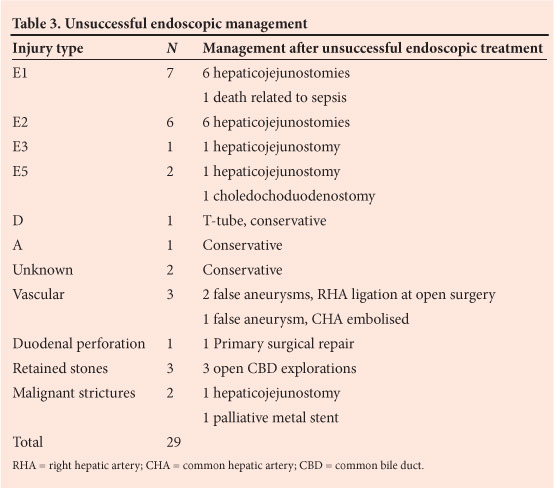
In 29 patients (25.7%) endoscopic management was not definitive (Table 3). In 16 (14.2%) ERCP demonstrated a major bile duct injury without ductal continuity, which required surgical repair by hepaticojejunostomy. These patients included 7 type E1, 6 type E2, 1 type E3 and 2 type E5 injuries. In 4 patients, CBD cannulation during ERCP was unsuccessful (1 had a confirmed CD leak on MRCP, and 1 a type D injury with a T-tube in situ; 2 unknown), and all 4 leaks resolved on conservative management. Three further patients required open CBD exploration after unsuccessful endoscopic CBD stone extraction; this included a patient with an impacted Dormia basket. One patient required duodenal repair after an iatrogenic injury during ERCP for suspected retained stones. In 2 patients, a distal malignant stricture was identified and, although their leaks settled on temporary plastic stenting, 1 patient required a palliative hepaticojejunostomy for repeated stent blockage. Three (15.8%) of the 19 major bile duct injuries were found to have an associated vascular injury (2 false aneurysms of the right hepatic artery ligated at open surgery, and a false aneurysm of the common hepatic artery which was embolised).
One hundred and thirteen patients underwent a total of 269 ERCPs (median 2 per patient, range 1 - 7). Seven patients (6.2%) developed one or more complications after their endoscopic interventions, with an ERCP complication rate of 3.7%. Ten specific ERCP-related complications occurred, and included 3 patients with post-procedural mild acute pancreatitis managed conservatively, 2 patients who developed cholangitis requiring treatment with intravenous antibiotics and repeat biliary decompression, 2 patients with sphincterotomy bleeds that were controlled by local injection of adrenaline 1:1000 solution, and 1 patient with early stent migration requiring a repeat ERCP. Two patients required surgical intervention. One patient had repair of an iatrogenic endoscopic duodenal perforation, and the other required an open CBD exploration and removal of an impacted Dormia basket.
One hundred and twelve patients (99.1%) were discharged from hospital. One patient died of multi-organ failure owing to persistent intra-abdominal sepsis following complete transection of the bile duct. One patient has required long-term balloon dilatation and stenting of a common hepatic duct stricture.
Of the group of patients who required surgical repair, 4 developed anastomotic strictures necessitating revision of their surgical repairs (3 hepaticojejunostomies, 1 choledochoduodenostomy). One patient with a suspected CBD stricture after bile duct injury eventually required a palliative hepaticojejunostomy for an irresectable carcinoma of the head of the pancreas and 1 required mesh repair of a large incisional hernia.
Discussion
In this study, three-quarters of postoperative bile leaks were suitable for endoscopic management and were treated with combinations of ES and bile duct stenting. Decreasing the transpapillary pressure to allow preferential duodenal biliary drainage and subsequent bile duct healing has been achieved by a variety of endoscopic techniques.[8] ES alone, ES and stenting, nasobiliary drainage and stenting without prior sphincterotomy have all been successfully employed in the management of bile leaks following cholecystectomy. [9,10] Nasobiliary drainage for bile leaks[3,11] has the advantage of allowing easy follow-up cholangiography and avoiding repeat ERCP, but owing to the potential disadvantages of patient discomfort, tube displacement, fluid loss, electrolyte imbalances and lengthy hospital stays, this technique is not routinely used in our unit.
Various endoscopic options exist to treat bile leaks; over 90% of leaks can be managed endoscopically if the distal obstruction is overcome.[5,10,12] Regardless of their origin in the biliary tree, minor leaks are defined as those demonstrated only after intrahepatic duct filling, whereas major leaks will be evident before intrahepatic duct filling has occurred.[13,14] Minor leaks seal in over 90% of patients following ES alone, while the recommendation for a major leak is temporary biliary stenting for 6 weeks.[12,13,15] Any patient who has an associated biliary stricture, a contraindication to ES or poor drainage of contrast after ES should also receive a temporary stent. No difference has been observed between patients managed by ES and stenting and stenting alone with regard to time of or success of biliary leak closure.[4,9,13]
There is currently no consensus regarding optimal endoscopic intervention, and there are no controlled data to indicate the optimal number, configuration, size, type and length of endoprostheses required for successful management of biliary leaks after laparoscopic cholecystectomy[9,15-17] Experimental data show that flow rates are better in vitro through straight than through pigtail stents, and fistula closure is more rapid in dogs with stents compared with sphincterotomy alone.[8,10,18,19] The ideal duration for biliary stenting is not known, and has varied from 3 to 8 weeks in previous reports.[10,13,15,16] In this study, we used single 10 Fr plastic stents after a conservative sphincterotomy for access and to facilitate stent insertion. The 10 Fr stent was used in preference to smaller 7 Fr stents, which carry the risk of early occlusion by inspissated bile, although a comparative study has found no difference in outcome based on stent size.[16] If residual stones were identified in the CBD a larger sphincterotomy was created to allow stone extraction. Generally only a short 7 cm stent that traverses the sphincter of Oddi is required. That it is not necessary to stent the leak site is supported by the current study and other published data.[20] The stents were left in situ for 6 weeks after external bile drainage had stopped. Using this protocol, all the fistulas in our study healed without recurrence.
Biliary leaks generally present 3 - 4 days postoperatively. Clinical features range from obvious biliary drainage via an intra-operatively placed drain or from the surgical wound to abdominal discomfort or pain, abdominal distension and ileus, peritonitis or systemic features of sepsis, abnormal LFTs or localised collections noted on ultrasound examination[12-14] Early recognition of a biliary leak is essential to minimise the potentially high morbidity and mortality associated with biliary tree injuries. Initial focus must be on controlling sepsis by ensuring adequate external drainage of any biliary collections; identifying the source and extent of the biliary leak is the primary step in planning further management options. MRCP allows non-invasive evaluation of the biliary tree, with a reported diagnostic sensitivity of 95% and a specificity of 100% in detecting a leak,[21,22] and is generally widely available. However, minor leaks may be missed, the leak site can only be identified with 70% accuracy, and no therapeutic input is possible. In our practice there may be a delay in obtaining an MRCP, while an ERCP is available immediately. We therefore prefer initial endoscopic evaluation of the biliary tree by ERCP when presented with a biliary leak in order to define the anatomy, assess the leak and allow simultaneous therapeutic intervention, but this can only be recommended in a high-output endoscopy unit with an acceptably low complication rate.
The most common site of a bile leak after cholecystectomy is the CD stump (Strasberg type A injury) (54 - 78% of patients), followed by the ducts of Lushka (13 - 19%). The remainder of the leaks (9 -20%) originate from the common hepatic duct, CBD, intrahepatic ducts and intra-operatively placed T-tubes.[4,13,14,231 This is in keeping with our findings of 66.4% of biliary leaks resulting from CD stump leaks. In this series of 75 patients with CD stump leaks, 40% of leaks were associated with retained CBD stones. Common causes of CD stump leaks include clip displacement after resolution of duct oedema, incorrect clip application, increased intrabiliary pressure transmitted to the CD stump as a result of distal CBD stones, CD necrosis and unrecognised distal CD injury. In patients with wide, oedematous ducts we recommend routinely tying off the duct to avoid clip slippage. We also advocate routine pre-operative LFTs, which if abnormal are followed by transabdominal ultrasound examination of the biliary tree. Should choledocholithiasis be confirmed, we perform a pre-operative ERCP. It is our policy to perform selective intra-operative cholangiograms in patients with abnormal LFTs but no ultrasonographic evidence of choledocholithiasis pre-operatively, or if there are any concerns intra-operatively in identifying the biliary anatomy.
The reported incidence of endoscopic complications after biliary manipulation and stenting for biliary leaks ranges from 1.8% to 7.2%, and complications include pancreatitis, cholangitis, bleeding from the sphincterotomy site and, rarely, duodenal perforation.[4,10,24-29] Later difficulties encountered are cholangitis due to stent blockage, dislodgement or stent migration. Seven patients in this study developed one or more complications after their endoscopic interventions, including mild acute pancreatitis, cholangitis, sphincterotomy bleeding and stent migration. Two patients required surgical intervention for complications following ERCP, 1 for repair of an iatrogenic duodenal perforation and the other for removal of an impacted Dormia basket. If there is no need for removal of CBD stones or placement of multiple simultaneous stents, an alternative option is to place a temporary biliary stent without first performing an ES. This is an attractive option in the elderly and in any situation where patient co-morbidities make it advisable to avoid all potential endoscopic complications.[25] In younger patients ES has been associated with an increased risk of cholangitis in the long term.[30] Late complications of temporary stenting include stent dysfunction, both stent migration and blockage occurring more frequently with plastic stents.[31] Our complication rate of 6.2% following ERCP for biliary leaks is in keeping with the reported literature.[4,10,24-29] While stent size does not affect biliary leak resolution, using a larger stent without an ES does increase the risk of mild pancreatitis, although not significantly.[25]
In this study, we used only plastic stents due to costs. Removable fully covered self-expanding metal stents are equally effective in sealing biliary leaks.[15] In this study, stents were removed after 6 weeks, and repeat cholangiography was routinely performed when the stent was removed to confirm duct integrity and the absence of a leak or stricture or residual stones; 91.3% of our endoscopically managed biliary leaks had sealed. In our setting, a routine balloon cholangiogram and pull-through is recommended owing to the high incidence of associated biliary sludge, stones or possible residual biliary leaks after stenting.[32,33]
In this study, ERCP was useful for confirming the diagnosis of minor biliary injury and for definitive management with internal biliary drainage in all patients. This study emphasises that a bile leak should be suspected in any patient who does not make a rapid postoperative recovery. In experienced centres, an ERCP is a safe initial approach to a post-cholecystectomy bile leak, and offers both accurate anatomical identification and grading of biliary leak severity with the option of immediate therapeutic intervention with low complication rates.[34] Post-cholecystectomy bile leaks occur most commonly from the CD stump, and associated CBD stones are found in one-third of cases.[35] Where there is duct continuity, over 90% of biliary leaks will resolve after endoscopic management. The issue of which technique of endoscopic drainage (particularly as it relates to the role of sphincterotomy and the choice of stent size) to use is still controversial, but ERCP in this setting can be performed with minimal morbidity. Biliary sphincterotomy alone will be sufficient in most patients, but does have potential complications. A biliary leak will seal fastest after stenting, which can be performed without a sphincterotomy but has the disadvantage of requiring a second procedure for stent removal. Individual patient preference, degree and positioning of the leak, the presence of potential distal obstruction and endoscopist preference together dictate the appropriate endoscopic approach. This study has shown that endoscopic therapy is safe and effective in the management of bile leaks after laparoscopic cholecystectomy.
REFERENCES
1. Sahajpal AK, Chow SC, Dixon E, et al. Bile duct injuries associated with laparoscopic cholecystectomy: Time of repair and long-term outcomes. Arch Surg 2010;145(8):757-763. [http://dx.doi.org/10.1001/archsurg.2010.153] [ Links ]
2. Krige JEJ, Bornman PC, Kahn D. Bile leaks and sepsis: Drain now, fix later. Arch Surg 2010;145(8):763. [http://dx.doi.org/10.1001/archsurg.2010.154] [ Links ]
3. Perera MT, Silva MA, Hegab B, et al. Specialist early and immediate repair of post-laparoscopic cholecystectomy bile duct injuries is associated with an improved long-term outcome. Ann Surg 2011;253(3):553-560. [http://dx.doi.org/10.1097/SLA.0b013e318208fad3] [ Links ]
4. Singh V, Singh G, Verma GR, Gupta R. Endoscopic management of postcholecystectomy biliary leakage. Hepatobiliary Pancreat Dis Int 2010;9(4):409-413. [ Links ]
5. Agarwal N, Sharma BC, Garg S, et al. Endoscopic management of postoperative bile leaks. Heapatobiliary Pancreat Dis Int 2006;5(2):273-277. [ Links ]
6. Kim JH, Kim WH, Kim JH, et al. Management of patients who return to the hospital with a bile leak after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A 2012;20(4):317-322. [http://dx.doi.org/10.1089/lap.2009.0241] [ Links ]
7. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995;180(1):101-125. [ Links ]
8. Youngelman DF, Marks JM, Ponsky T, Ponsky JL. Comparison of bile duct pressures following sphincterotomy and endobiliary stenting in a canine model. Surg Endosc 1997;11(2):126-128. [http://dx.doi.org/10.1007/s004649900313] [ Links ]
9. Mavrogiannis C, Liatsos C, Papanikolaou IS, et al. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: A prospective randomized study. Eur J Gastroenterol Hepatol 2006;18(4):405-409. [http://dx.doi.org/10.1097/00042737-200604000-00014] [ Links ]
10. Dumonceau J-M, Tringali A, Blero D, et al. Biliary stenting: Indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012;44(3):277-298. [http://dx.doi.org/10.1055/s-0031-1291633] [ Links ]
11. Chow S, Bosco JJ, Heiss FW, et al. Successful treatment of post-cholecystectomy bile leak using nasobiliary tube drainage and sphincterotomy. Am J Gastroenterol 1997;92(10):1839-1843. [ Links ]
12. Kimura T, Suzuki K, Umehara Y, Kawabe A, Wada H. Features and management of bile leaks after laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg 2005;12(1):61-64. [http://dx.doi.org/10.1007/s00534-004-0935-2] [ Links ]
13. Sandha GS, Bourke MJ, Haber GB, Kortan PP. Endoscopic therapy for bile leak based on a new classification: Results in 207 patients. Gastrointest Endosc 2004;60(4):567-574. [http://dx.doi.org/10.1016/S0016-5107(04)01892-9] [ Links ]
14. Braghetto I, Bastias J, Csendes A, Debandi A. Intraperitoneal bile collections after laparoscopic cholecystectomy: Causes, clinical presentation, diagnosis, and treatment. Surg Endosc 2000;14(11):1037-1041. [http://dx.doi.org/10.1007/s004649900029] [ Links ]
15. Canena L, Liberato M, Horta D, et al. Short-term stenting using fully covered self-expanding metal stents for treatment of refractory biliary leaks, post-sphincterotomy bleeding, and perforations. Surg Endosc 2013;27(1):313-324. [http://dx.doi.org/10.1007/s00464-012-2368-3] [ Links ]
16. Katsinelos P, Kountouras J, Paroutoglou G, et al. A comparative study of 10-Fr vs, 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg Endosc 2008;22(1):101-106. [http://dx.doi.org/10.1007/s00464-007-9381-y] [ Links ]
17. Donnellan F, Zeb F, Courney G, Aftab AR. Successful outcome of sphincterotomy and 7 French pigtail stent insertion in the management of post-cholecystectomy bile leaks. Hepatobiliary Pancreat Dis Int 2009;8(3):309-311. [ Links ]
18. Olweny EO, Portis AJ, Afane JS, et al. Flow characteristics of 3 unique ureteral stents: Investigation of a Poiseulle flow pattern. J Urol 2000;164(6):2099-2103. [http://dx.doi.org/10.1016/S0022-5347(05)66977-7] [ Links ]
19. Marks JM, Ponsky RB, Shillingstad RB, Singh J. Biliary stenting is more effective than sphincterotomy in the resolution of biliary leaks. Surg Endosc 1998;12(4):327-330. [ Links ]
20. Bjorkman DJ, Carr-Locke DL, Lichtenstein DR, et al. Postsurgical bile leaks: Endoscopic obliteration of the transpapillary pressure gradient is enough. Am J Gastroenterol 1995;90(12):2128-2133. [ Links ]
21. Aduna M, Larena JA, Martin D, et al. Bile duct leaks after laparoscopic cholecystectomy: Value of contrast-enhanced MRCP. Abdom Imaging 2005;30(4):480-487. [http://dx.doi.org/10.1007/s00261-004-0276-2] [ Links ]
22. Ragozzino A, De Ritis R, Mosca A, et al. Value of MR cholangiography in patients with iatrogenic bile duct injury after cholecystectomy. AJR Am J Roentgenol 2004;183(6):1567-1572. [http://dx.doi.org/10.2214/ajr.183.6.01831567] [ Links ]
23. Shaikh IA, Thomas H, Joga K, et al. Post-cholecystectomy cystic duct stump leak: A preventable morbidity. J Dig Dis 2009;10(3):207-212. [http://dx.doi.org/10.1111/j.1751-2980.2009.00387.x] [ Links ]
24. Cotton P, Garrow D, Gallagher J, et al. Risk factors for complications after ERCP: A multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 2009;70(1):80-88. [http://dx.doi.org/10.1016/j.gie.2008.10.039] [ Links ]
25. Simmons DT, Petersen BT, Gostout CJ, et al. Risk of pancreatitis following endoscopically placed large-bore plastic biliary stents with and without biliary sphincterotomy for management of postoperative bile leaks. Surg Endosc 2008;22(6):1259-1263. [http://dx.doi.org/10.1007/s00464-007-9643-8] [ Links ]
26. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: A prospective multicenter study. Gastrointest Endosc 1998;48(1):1-10. [http://dx.doi.org/10.1016/S0016-5107(98)70121-X] [ Links ]
27. Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: A prospective multicenter study. Am J Gastroenterol 2001;96(2):417-423. [http://dx.doi.org/10.1111/j.1572-0241.2001.03594.x] [ Links ]
28. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: A prospective, multicenter study. Gastrointest Endosc 2001;54(4):425-434. [http://dx.doi.org/10.1067/mge.2001.117550] [ Links ]
29. Vandervoort J, Soetikno RM, Tham TC, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc 2002;56(5):652-656. [http://dx.doi.org/10.1016/S0016-5107(02)70112-0] [ Links ]
30. Elmi F, Silverman WB. Long-term biliary endoscopic sphincterotomy restenosis: Incidence, endoscopic management, and complications of retreatment. Dig Dis Sci 2010;55(7):2102-2107. [http://dx.doi.org/10.1007/s10620-009-0957-3] [ Links ]
31. Arhan M, Odemis B, Parlak E, et al. Migration of biliary plastic stents: Experience of a tertiary centre. Surg Endosc 2009;23(4):769-775. [http://dx.doi.org/10.1007/s00464-008-0067-x] [ Links ]
32. Jain V, Yeasted N, Pooran N. Necessity of a repeat cholangiogram during biliary stent removal after postcholecystectomy bile leak. Can J Gastroenterol 2012;26(10):701-704. [ Links ]
33. Cote GA, Ansstas M, Shah S, et al. Findings at endoscopic retrograde cholangiography after endoscopic treatment of postcholecystectomy bile leaks. Surg Endosc 2010;24(7):1752-1756. [http://dx.doi.org/10.1007/s00464-009-0842-3] [ Links ]
34. Tarantino I, Mangiavillano B, Di Mitri R, et al. Fully covered self-expandable metallic stents in benign biliary strictures: A multicenter study on efficacy and safety. Endoscopy 2012;44(10):923-927. [http://dx.doi.org/10.1055/s-0032-1310011] [ Links ]
35. De Palma GD, Iuliano GP, Puzziello A, et al. Biliary leaks after laparoscopic cholecystectomy: Results of the endoscopic treatment. Minerva Chir 2002;57(2):123-127. [ Links ]
 Correspondence:
Correspondence:
G E Chinnery
(galyachinnery@gmail.com)














