Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.51 no.3 Cape Town Jan. 2013
CASE REPORT
A paediatric case of AAST grade IV duodenal injury with application of damage control surgery
G L LaingI; F GhimentonI; D L ClarkeII
IMB ChB, FCS (SA), Grey's Hospital, Pietermaritzburg, KwaZulu-Natal, South Africa
IIMB ChB, FCS (SA), MBA, MMedSci, MPhil, Grey's Hospital, Pietermaritzburg, KwaZulu-Natal, South Africa
ABSTRACT
Isolated severe blunt duodenal injuries are rare. We present an American Association for the Surgery of Trauma grade IV duodenal injury in a paediatric patient. The strategic use of damage control surgical principles, involving an initial abbreviated laparotomy followed by a delayed reconstruction, resulted in a successful outcome.
Case report
An 8-year-old boy was referred to Grey's Hospital, Pietermaritzburg, South Africa, 32 hours after being trapped under a collapsing wall. On arrival, the child was in hypovolaemic shock with a systolic blood pressure of 90 mmHg and a pulse rate of 158 beats/min. He was profoundly hypothermic with a core body temperature of 33.2oC. The abdomen was clinically peritonitic.
Arterial blood gas measurement revealed a profound metabolic acidosis, with a pH of 7.06, a serum bicarbonate level of 14.2 mmol/l and a base deficit of -15.0 mmol/l. The International Normalized Ratio was 2.04.
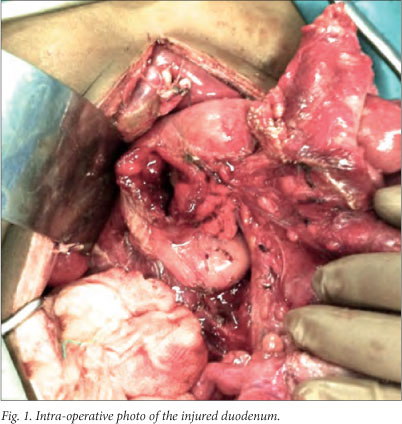
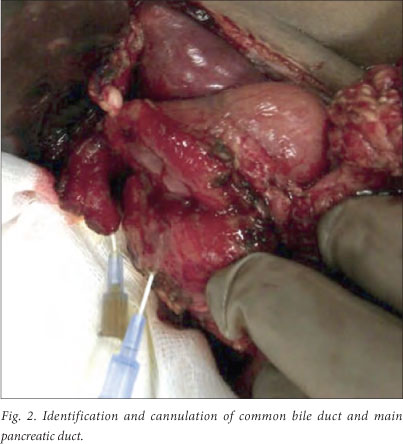
The patient was resuscitated according to standard principles and subjected to a damage control laparotomy. This revealed full-thickness rupture of both the anterior and posterior walls of the first, second and third portions of the duodenum (Fig. 1), with an avulsed distal common bile duct and ampulla of Vater (Fig. 2). The abdomen was washed out and large-bore, closed suction drains were placed adjacent to the injury. The abdomen was closed using a temporary abdominal closure technique.
The patient was admitted to the intensive care unit (ICU) for continued resuscitation. After 48 hours he was returned to theatre. Definitive management involved a total duodenectomy, followed by an end-to-end gastrojejunostomy, choledochojejunosotomy and pancreaticojejunostomy. After reconstruction, the patient spent 1 week in the ICU and a further 5 weeks in the ward. Total parenteral nutrition was commenced and gradually weaned as the patient was transitioned to naso-enteral feeds over the subsequent fortnight. The postoperative course was complicated by the development of a pancreatic fistula, which drained approximately 350 ml of clear amylase-rich fluid per day for a month. The fistula resolved spontaneously 30 days after admission. The patient progressed to a full ward diet, and was discharged 6 weeks after initial admission.
Discussion
Duodenal injuries in children are rare and are most commonly due to blunt trauma. Considering the retroperitoneal position of the duodenum, clinical signs may be subtle and predispose to a delay in diagnosis.[1]
Investigations are reserved for the stable patient without overt signs of peritonitis. Computed tomography with oral contrast is very sensitive for the detection of retroperitoneal or intra-peritoneal free air, fluid or extra-luminal contrast medium.[2,3]
Operative exploration is mandatory for the unstable, peritonitic patient or when radiological features suggest a full-thickness duodenal injury. In the past, complex operative strategies of temporary duodenal diversion such as pyloric exclusion were advocated to protect the duodenal repair. The modern trend appearing in the literature is towards less complicated operative strategies and, after adequate mobilisation, most duodenal injuries can safely be managed by primary closure.[1] However, more severe grades of pancreatico-duodenal injury may still necessitate technically complex operative solutions. Destructive injuries proximal to the sphincter may require antrectomy and gastrojejunostomy. If the injury involves the sphincter complex, formal pancreaticoduodenectomy may be required. This is a major procedure and should not be undertaken as an emergency, as patients presenting with such severe injuries are too unwell to tolerate it. These patients should rather undergo an initial abbreviated damage control laparotomy.[4] Definitive resection and reconstruction can be performed after resuscitation.
This case is testament to the applicability of the damage control approach in the appropriate patient.
REFERENCES
1. Degiannis E, Boffard K. Duodenal injuries. Br J Surg 2000;87(11):1473-1479. [http://dx.doi.org/10.1046/j.1365-2168.2000.01594.x] [ Links ]
2. Kunin JR, Korobkin M, Ellis JH, Francis IR, Kane MN, Siegel SE. Duodenal injuries caused by blunt abdominal trauma: Value of CT in differentiating perforation from hematoma. Am J Roentgenol 1993;160(6):1221-1223. [http://dx.doi.org/10.2214/ajr.160.6.8498221] [ Links ]
3. Shilyansky J, Pearl RH, Kreller M, Sena LM, Babyn PS. Diagnosis and management of duodenal injuries in children. J Pediatr Surg 1997;32(6):880-886. [http://dx.doi.org/10.1016/S0022-3468(97)90642-4] [ Links ]
4. Kauder DR, Schwab CW, Rotondo MF. Damage control. In: Ivantury RR, Cayten CG, eds. The Textbook of Penetrating Trauma. Baltimore, MD: Williams & Wilkins, 1996:717-725. [ Links ]
 Correspondence:
Correspondence:
G L Laing
(grantlaing@me.com)














