Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.51 no.3 Cape Town ene. 2013
TRAUMA
Open globe injuries in patients seen at Groote Schuur Hospital, Cape Town, South Africa
N du ToitI; H MustakII; C LevetanIII; C CookIV
IMMed, Division of Ophthalmology, Department of Surgery, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIDip Ophth, Division of Ophthalmology, Department of Surgery, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIIMB ChB, Division of Ophthalmology, Department of Surgery, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IVMPH, Division of Ophthalmology, Department of Surgery, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND: Ocular trauma accounts for a significant proportion of admissions to the eye ward at Groote Schuur Hospital (GSH), Cape Town, South Africa. There are few published studies on ocular trauma in South Africa. Some studies elsewhere have shown an association between open globe injuries and recent alcohol use, but no such study has been conducted in this country.
BJECTIVES: To identify causes of and outcomes after open globe injuries at GSH, with emphasis on the association between assault and alcohol use as well as the relationship, if any, between victim and assailant.
METHODS: This was a prospective case series of all adult patients admitted to GSH with open globe injuries over a 2-year period. Ocular findings were recorded with a minimum 3-month follow-up period.
RESULTS: There were 249 open globe injuries. Assault had occurred in 183 (73.5%), and 66 (26.5%) were accidental. In the assault-related cases, 95 (51.9%) of the assailants were reported to have used alcohol and 121 (66.1%) of the victims admitted to alcohol use prior to the assault. There was a statistically significant relationship between ethanol use and type of injury, 71.4% of assault cases overall being associated with ethanol use. In assault-related cases, the assailant was known to the victim in 113 cases (61.7%). Of the patients, 78.7% had a final acuity of <3/60 in the traumatised eye.
CONCLUSION: A significant number of open globe injuries due to assault are related to ethanol use and occur when the victim and assailant are known to each other. Such injuries are likely to have a poor prognosis.
Ocular trauma is known to be an important preventable cause of visual impairment. Penetrating eye (open globe) injuries generally have a poor visual prognosis, and awareness of the outcomes of these injuries needs to be increased. There is anecdotal evidence that a significant proportion of the ocular trauma seen at Groote Schuur Hospital (GSH), Cape Town, South Africa, is due to assault, is associated with alcohol consumption by the assailant and the victim, and has a poor visual outcome. It has already been shown that patients injured as a result of assault in South Africa are more likely to test positive for alcohol than patients who sustain road traffic or other accidental injuries.[1] Large studies from elsewhere have shown that between 24% and 48% of patients with open globe injuries showed evidence of alcohol use.[2,3] There have been 2 published case series of ocular trauma in South Africa.[4,5] Neither series reported the relationship with alcohol use.
Objectives
This study was undertaken to identify the risk factors, mechanisms of injury and visual acuity outcomes after open globe injury in patients seen at GSH, with emphasis on its associations with assault and alcohol use as well as the relationship, if any, between victim and assailant. The findings were compared with those of other studies internationally.
Methods
Data were prospectively collected on all patients admitted to GSH with an open globe injury over the 2-year period from the beginning of July 2009 to the end of June 2011. On admission, a standard assessment sheet was filled in by a resident ophthalmologist. Each patient was examined and findings documented. Data were recorded on patient demographics, injury demographics, times of initial medical and ophthalmological assessments, initial visual acuity, primary and secondary surgical operations, duration of hospitalisation and follow-up. The patients were asked whether they had been using alcohol at the time of the injury. If they had been assaulted and if they knew the assailant, they were asked if the assailant had been using alcohol at the time of the assault. The patients were followed up for a minimum period of 3 months, and the visual acuities at the last visit were documented. Patient anonymity was strictly maintained.
Data were analysed using Stata (version 11.1). Proportions were compared using the chi-square test and, where appropriate, Fisher's exact test. Means and standard deviations (SDs) were reported for normally distributed variables. Significant p-values were reported (level of significance <0.05). Ethical approval for the study was obtained from the Ethics Committee of the Faculty of Health Sciences, University of Cape Town.
Results
There were 3 153 elective and emergency admissions to the ophthalmology ward at GSH over the 2 years of the study. Of these, 398 (12.6%) were emergency admissions related to trauma, which were made up of 391 mechanical injuries and 7 chemical injuries. The mechanical injuries comprised 142 (34.6%) closed globe and 249 (63.7%) open globe types.
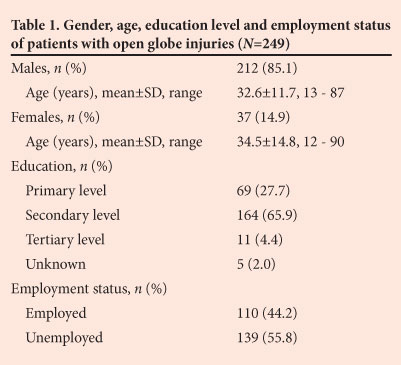
Of the 249 patients with open globe injuries, 64.9% were under the age of 35 years (Table 1). Levels of education and employment status of the patients are also listed in the table.
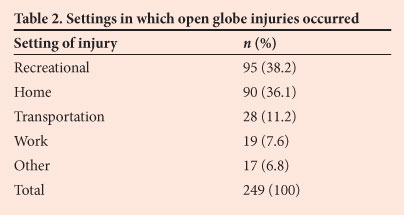
Assault was reported to have occurred in 183 (73.5%) of the open globe injuries, while 66 (26.5%) were accidental. Table 2 shows the settings in which the open globe injuries occurred.
Ethanol use was implicated in 126 (50.6%) of the 249 open globe cases, and also in 221 (55.5%) of the overall 398 eye trauma admissions. In the 183 assault-related open globe injuries, 95 assailants (51.9%) were reported to be under the influence of alcohol, and 121 patients (66.1%) admitted to using alcohol before they were injured. There was a statistically significant relationship between ethanol use and type of injury, with 71.4% of open globe assault cases being associated with ethanol use by the assailant and/or the victim (p<0.005). Other drugs were used at the time the injury took place in 11 (4.4%) of the 249 open globe cases.
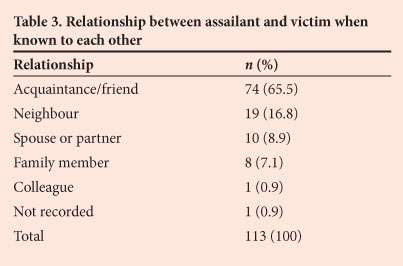
The assailant was known to the victim in 113 (61.7%) of the 183 cases of assault-related open globe injuries (i.e. they were not known to each other in 70 cases) (Table 3). A victim was significantly more likely to be assaulted by an assailant who was known to him or her (p<0.005). There was also a statistically significant relationship between the assailant being known to the victim and alcohol use.
Categories of objects that were used to inflict or were the cause of the 249 open globe injuries are set out in Table 4. Knives, bottles and glass accounted for 51.1% of all open globe injuries, and there was therefore a strong association (p<0.05) between them. There was a significant association between ethanol use by the assailant and the type of object used to inflict injury, with knives, bottles or glass accounting for 66% of cases (p<0.05).

Of the patients with open globe injuries, 195 (83.7%) presented for medical help within 24 hours. Presentation was delayed for more than 48 hours in only 9.4% of cases. Eye consultation took place within 24 hours of injury in 142 of the cases (61.2%) and was delayed beyond 48 hours of injury in only 7.1%.
For ease of analysis, Snellen visual acuity (VA) in the affected eye at presentation was divided into 3 groups roughly resembling the World Health Organization criteria, viz. group 1: normal (6/5 -6/12); group 2: visually impaired (6/18 - 3/60); and group 3: blind (<3/60). Of the patients with open globe injuries, 85.1% presented with VA in the blind range (group 3), with 30.5% having no light perception, i.e. completely blind; only 3.2% had VAs in the normal range (group 1) at presentation. An afferent pupillary defect (APD) was found to be present in 144 (57.8%) of the 249 open globe injuries.
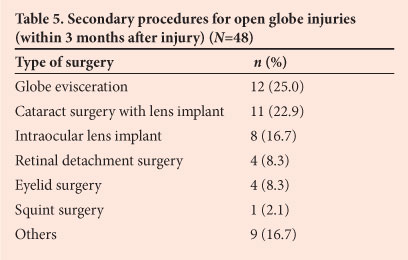
All 249 patients with open globe injuries underwent primary surgery. The primary procedures were 175 repairs (70.3%), 61 eviscerations (24.5%) and 13 others (5.2%). Corneal lacerations were repaired using 10-0 nylon interrupted sutures and scleral injuries with 9-0 nylon or 7-0 Vicryl, with anterior vitrectomy and lensectomy where required. Secondary procedures performed are listed in Table 5.
The mean (±SD) period of stay in hospital for open globe injury patients was 3.7±2.39 days (range 1 - 18 days).
Visual outcome was measured as the best corrected visual acuity (BCVA) at the 3-month follow-up visit. Seventy-five patients with open globe injuries (30.1%) were lost to follow-up and did not complete the 3-month follow-up period. These cases were not included in the analysis of visual outcomes. Ten patients with open globe injuries (4.0%) ended up legally blind (VA 3/60 or worse in the better eye). Table 6 shows outcomes in the traumatised eyes only.
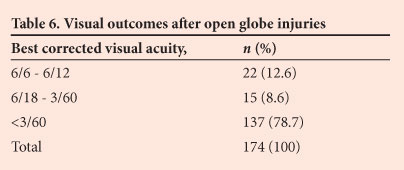
There was no significant difference in the BCVA at 3 months in injuries with or without an association with alcohol use (p=0.199). Analysis of all recorded variables revealed that only presenting VA, presence of an APD and open globe injuries were significant (p<0.005) as relevant predictors of final visual outcome. There was no statistical significance to the association between ethanol use and open globe injuries (p=0.059) in general, but there was statistical significance to the association between ethanol-related assaults and open globe injuries - 68.8% of assaults involving ethanol resulted in open globe injuries (p=0.021), i.e. were predictive of a poorer outcome. All the above associations were determined by using univariate and multivariate analysis, as well as logistic regression.
Discussion
About 12.5% of all admissions (elective and emergency) during the period of this study were trauma cases, and almost two-thirds of these were open globe injuries. This finding illustrates that serious ocular trauma accounts for a significant proportion of our admissions. In comparison, in a retrospective analysis of 28 340 patient records included in the National Trauma Data Bank in the USA from 2003 to 2007, the most common ocular trauma admissions were for superficial injuries and closed orbit fractures.[6]
Young adult males were the largest group admitted with open globe injuries. This finding is consistent with those of other authors.[2,3,7-16] A retrospective study on patterns of injury and outcomes after multi-system trauma revealed that 220 patients with open globe injuries presented to the Massachusetts Eye and Ear Infirmary (USA) over a 3-year period, with men more likely to suffer from penetrating injuries and women more likely to experience blunt globe rupture.[7] This gender difference in type of injury was not found in our study population. Another study performed on ocular trauma cases from 1984 to 1987 via the National Hospital Discharge Surveys (USA) found that males were 3 times more likely to be hospitalised for a principal diagnosis of ocular trauma than females.[8] A retrospective chart review of emergency department patients from 1987 to 1999 in a tertiary hospital (USA) enrolled 390 open globe injuries and found that 85% of patients were male, with a mean age of 29 years.[9]
The National Eye Trauma System Registry (USA) collected data from 1985 to 1991 on 2 939 cases of open globe injuries at 48 collaborating eye trauma centres. Men were affected in 83% of the cases (median age 27 years). The settings in which the injuries occurred included the home (28%), the workplace (21%), recreation (11%) and transportation (8%). Accidental injuries accounted for 77% of cases, and only 22% were the result of assault.[2] In a prospective UK study, 200 consecutive patients with closed head injury were admitted to a teaching hospital. The main causes of head injury were road traffic accidents (52.5%), followed by assaults (34%). There was ocular involvement in 167 cases (83.5%).[10] In another analysis of the National Eye Trauma System Registry (USA), there were 635 (22%) work-related open globe injuries among the 2 939 cases reported.[11]
In the study on open globe injuries mentioned above,[2] there was evidence of definite or possible alcohol use by at least 24% of the injured persons and of illicit drug use by 8%, compared with alcohol and illicit drug use by at least 48% and 6%, respectively, of the injured persons in a separate report on open globe assault-related injuries over the same time period.[3] In comparison, about 50% of all our open globe injuries and 66% of the assault-related injuries were associated with alcohol use by the patient, while 71% of assault-related injuries were associated with alcohol use by the victim and/or the assailant.
Studies have been done specifically on assault-related open-globe injuries - a retrospective study in the United States (US) over a 5-year period (1986 - 1991) included 42 patients with open globe injuries resulting from assault, of whom 86% were male (mean age 29 years). Two-thirds had consumed alcohol or used illegal drugs before their injuries. Fists and broken glass were the leading causes of injury.[12] These findings are similar to those in our sub-group of assault-related open globe injuries, although any case with reported alcohol use by victim and/or assailant was counted as an alcohol association in our analysis. Similarly, in a retrospective review of patients entering an adult regional trauma unit in Washington, DC (USA), 6 313 patients were included over a 6-year period and 856 (13.5%) had concomitant ocular trauma. Nearly one-third of patients with assault-related ocular trauma had blood alcohol levels exceeding 100 mg/dl.[13] Alcohol abuse therefore appears to have a significant association with assault-related open globe injuries in Cape Town, as well as in other parts of the world.
A new finding, not explored in previous studies, is the fact that in more than half of our assault-related cases the assailant was known to the victim. This relationship turned out to be 'acquaintance or friend' in almost two-thirds of cases. This disturbing finding was further highlighted by the statistically significant association between being assaulted by a known assailant and the use of alcohol, as well as the increased likelihood of being attacked with a knife, a bottle or broken glass.
Studies from other parts of the world show varying findings, some being similar to those of our study and others very different. A retrospective study done on adults in Croatia revealed that 383 patients with eye injuries (397 eyes) were hospitalised at a university hospital from 1998 to 2002. The male-to-female ratio was 5.4:1. Almost half of the injuries occurred at home and only 7.0% were a result of assault. There were 343 mechanical injuries, of which 67.3% were closed globe and 32.7% open globe.[14] A retrospective review of the epidemiology of patients with serious ocular trauma presenting to a hospital in Queensland, Australia, from 1995 to 2002 identified 226 cases. Of assault cases, 76.2% were alcohol-related, and 20.8% of patients were lost to follow-up.[15] A 2-year prospective study in Turkey included 203 patients (74% male, mean age 27.3 years) with injuries to 208 eyes. Most patients were hospitalised, and the leading cause of eye injury was work-related accidents.[16]
In our study, patients presented to the eye department within 24 hours of injury in over 60% of cases. This differs from a previous prospective study on the visual outcome of open globe injuries in South Africa (100 children between 2001 and 2002), in which only 25% presented to the hospital within 24 hours of injury.[5]
We found blindness to be rare following ocular trauma, since there were few bilateral injuries, but monocular blindness occurred as a result of open globe injuries in more than three-quarters of our cases. Trauma-induced eye injuries are the leading cause of monocular blindness in the US - in a retrospective study on open globe injuries, 63% were blind in the affected eye.[7] An analysis of 11 320 eyes in the US Eye Injury Registry database[17] revealed that poor visual outcome was associated with age over 60 years and injury by assault sustained on the street or by gunshot. Only poor presenting VA, the presence of an APD and open globe injuries themselves were found to be significant in our series.
In summary, most open globe injuries in our setting were due to assault, occurred in a recreational setting, and were associated with alcohol use. In most cases, the patient was unemployed and the assailant was known to the patient, and in most cases a knife or broken bottle was used. This pattern differs from those reported by others, where accidental injuries at home or at work accounted for the majority of cases.[2,10,11,16] However, in one study on assault-related open globe injuries, two-thirds of cases were related to the use of alcohol or another recreational drug, and in another, three-quarters of assault-related injuries were associated with the use of alcohol.[12,15]
This study has a number of weaknesses. Blood alcohol levels were not measured in our patients, and the association with alcohol use was based on the history or on clinical examination at the time of admission. Other studies reporting associations with alcohol use have also relied on the history and clinical examination.[2,3,12,15] Almost a third of our patients were lost to follow-up, and did not complete the 3-month period. The documented 3-month VAs may therefore be biased.
Conclusion
In comparison with other parts of the world, more cases of open globe injuries in Cape Town are due to assault and occur when both victim and assailant are under the influence of alcohol and even acquainted with each other.
Ocular trauma is known to be an important preventable cause of visual impairment and has a poor visual prognosis if the patient has a poor presenting VA after injury, an APD and an open globe. Injuries following ethanol-related assault are more likely to result in an open globe injury and therefore have a poorer prognosis.
Strategies to prevent open globe injuries related to assault and ethanol use should focus on the origins of violence in general. These are more difficult to devise than strategies to prevent, for example, work-related eye injuries. Continued efforts to reduce the abuse of alcohol, improve available treatments and implement prevention measures should reduce the incidence of blinding eye trauma.
Acknowledgements
We thank Pat Luiters for her assistance with data collection.
REFERENCES
1. Pludemann A, Parry C, Donson H, et al. Alcohol use in Cape Town, Durban and Port Elizabeth, South Africa: 1999-2001. Injury Control and Safety Promotion 2004;11(4):265-267. [http://dx.doi.org/10.1080/156609704/233/289599] [ Links ]
2. Parver LM, Dannenberg AL, Blacklow B, et al. Characteristics and causes of penetrating eye injuries reported to the National Eye Trauma System Registry, 1985-91. Public Health Rep 1993;108(5):625-632. [ Links ]
3. Dannenberg AL, Parver LM, Fowler CJ. Penetrating eye injuries related to assault: The National Eye Trauma System Registry. Arch Ophthalmol 1992;110(6):849-852. [http://dx.doi.org/10.1001/archopht.1992.01080180121039] [ Links ]
4. Cook C. Perforating eye injuries in KwaZulu. S Afr Med J 1991;80(9):441-444. [ Links ]
5. Grieshaber MC, Stegmann R. Penetrating eye injuries in South African children: Aetiology and visual outcome. Eye 2006;20(7):789-795. [http://dx.doi.org/10.1038/sj.eye.6702003] [ Links ]
6. Scruggs D, Scruggs R, Stukenborg G, Netland PA, Calland JF. Ocular injuries in trauma patients: An analysis of 28,340 trauma admissions in the 2003-2007 National Trauma Data Bank National Sample Program. Journal of Trauma and Acute Care Surgery 2012;73(5):1308-1312. [http://dx.doi.org/10.1097/TA.0b013e31825c78d9] [ Links ]
7. Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton MP. Gender differences in etiology and outcome of open globe injuries. J Trauma 2005;59(1):175-178. [http://dx.doi.org/10.1097/01.TA.0000173624.37438.D6] [ Links ]
8. Klopfer J, Tielsch JM, Vitale S, See LC, Canner JK. Ocular trauma in the United States: Eye injuries resulting in hospitalization, 1984 through 1987. Arch Ophthalmol 1992;110(6):838-842. [http://dx.doi.org/10.1001/archopht.1992.01080180110037] [ Links ]
9. Smith D, Wrenn K, Stack LB. The epidemiology and diagnosis of penetrating eye injuries. Acad Emerg Med 2002;9(3):209-213. [http://dx.doi.org/10.1197/aemj.9.3.209] [ Links ]
10. Kulkarni AR, Aggarwal SP, Kulkarni RR, Deshpande MD, Walimbe PB, Labhsetwar AS. Ocular manifestations of head injury: A clinical study. Eye 2005;19(12):1257-1263. [http://dx.doi.org/10.1038/sj.eye.6701753] [ Links ]
11. Dannenberg AL, Parver LM, Brechner RJ, Khoo L. Penetrating eye injuries in the workplace: The National Eye Trauma System Registry. Arch Ophthalmol 1992;110(6):843-848. [http://dx.doi.org/10.1001/archopht.1992.01080180115038] [ Links ]
12. Groessl S, Nanda SK, Mieler WF. Assault-related penetrating ocular injury. Am J Ophthalmol 1993;116(1):26-33. [ Links ]
13. Sastry SM, Paul BK, Bain L, Champion HR. Ocular trauma among major trauma victims in a regional trauma center. J Trauma 1993;34(2):223-226. [http://dx.doi.org/10.1097/00005373-199302000-00007] [ Links ]
14. Karaman K, Gverović-Antunica A, Rogosić V, et al. Epidemiology of adult eye injuries in Split-Dalmatian county. Croat Med J 2004;45(3):304-309. [ Links ]
15. Smith AR, O'Hagan SB, Gole GA. Epidemiology of open- and closed-globe trauma presenting to Cairns Base Hospital, Queensland. Clin Experiment Ophthalmol 2006;34(3):252-259. [http://dx.doi.org/10.1111/j.1442-9071.2006.01200.x] [ Links ]
16. Oner A, Kekec Z, Karakucuk S, Ikizceli I, Sözüer EM. Ocular trauma in Turkey: A 2-year prospective study. Adv Ther 2006;23(2):274-283. [http://dx.doi.org/10.1007/BF02850133] [ Links ]
17. Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol 2006;13(3):209-216. [http://dx.doi.org/10.1080/09286580600665886] [ Links ]
 Correspondence:
Correspondence:
N du Toit
(ndutoit@mweb.co.za; nagib.dutoit@uct.ac.za)
Conflict of interest. None.














