Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.51 no.3 Cape Town ene. 2013
GENERAL SURGERY
A concept paper: Using the outcomes of common surgical conditions as quality metrics to benchmark district surgical services in South Africa as part of a systematic quality improvement programme
D L ClarkeI; V Y KongII; J HandleyIII; C AldousIV
IFCS (SA), MMedSci, MBA, MPhil Department of Surgery, Edendale Hospital, Pietermaritzburg, and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMB BCh, Department of Surgery, Edendale Hospital, Pietermaritzburg, and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIFCA (SA), Department of Anaesthetics, Edendale Hospital, Pietermaritzburg, and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IVPhD, Department of Surgery, Edendale Hospital, Pietermaritzburg, and Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
The fourth, fifth and sixth Millennium Development Goals relate directly to improving global healthcare and health outcomes. The focus is to improve global health outcomes by reducing maternal and childhood mortality and the burden of infectious diseases such as HIV/AIDS, tuberculosis and malaria. Specific targets and timeframes have been set for these diseases. There is, however, no specific mention of surgically treated diseases in these goals, reflecting a bias that is slowly changing with emerging consensus that surgical care is an integral part of primary healthcare systems in the developing world. The disparities between the developed and developing world in terms of wealth and social indicators are reflected in disparities in access to surgical care. Health administrators must develop plans and strategies to reduce these disparities. However, any strategic plan that addresses deficits in healthcare must have a system of metrics, which benchmark the current quality of care so that specific improvement targets may be set.
This concept paper outlines the role of surgical services in a primary healthcare system, highlights the ongoing disparities in access to surgical care and outcomes of surgical care, discusses the importance of a systems-based approach to healthcare and quality improvement, and reviews the current state of surgical care at district hospitals in South Africa. Finally, it proposes that the results from a recently published study on acute appendicitis, as well as data from a number of other common surgical conditions, can provide measurable outcomes across a healthcare system and so act as an indicator for judging improvements in surgical care. This would provide a framework for the introduction of collection of these outcomes as a routine epidemiological health policy tool.
Over the three-and-a-half decades since the Declaration of Alma Ata, healthcare systems have tended to become increasingly inequitable and cost-ineffective, implying that the traditional model of primary healthcare conceptualised at Alma Ata has to a large extent been unsuccessful.[1-7] This has necessitated a re-imagining of the model of primary healthcare. The new model views primary healthcare as a central hub, which focuses on strengthening the individual components of the health system beneath the overarching umbrella of primary healthcare. Traditionally the public health approach perceived surgical services as expensive curative services that benefited individuals rather than communities.[1-3] Since Nordberg first drew attention to the fact that much morbidity and mortality occurs in remote rural African villages because of common surgical conditions,[1-3] there has emerged a consensus that surgical care is an integral component of primary healthcare and that common surgical conditions such as trauma, hernias, appendicitis, obstetric emergencies and congenital anomalies are important public health problems.[1-7]
There are major disparities in access to surgical care across the world, and this disproportionately affects rural and marginal groups in low-income countries.[5-7] The World Health Organization (WHO) classifies countries as high, middle or low income based on the amount of money annually spent on healthcare per head of population, middle- to high-income countries spending between US$400 and US$1 000 per head of population. Only a third of the world's population lives in middle- to high-income countries, yet two-thirds of all surgical procedures are performed there, and the poorest third of the world's population undergoes less than 4% of all surgical procedures. It has been estimated that the global volume of major surgery in 2004 was between 187 million and 281 million cases, which equates to one operation for every 25 human beings.[7] Major morbidity complicates 3 - 16% of all surgical procedures, and there is an associated death or permanent disability rate from 0.5% to just under 1% in the developed world. The mortality rate of major surgery in the developing world is significantly higher, however, and has been estimated to be in the range of 5 - 10%. This means that approximately 7 million people a year experience a major complication, and 1 million people a year die, following surgery.[7] In view of the large numbers involved, improving outcomes for surgery is a public health priority, and the provision of adequate surgical services has been shown to be an extremely cost-effective healthcare intervention in the developing world.[7-10] Most of the strategies designed to address the disparities in access to surgical care focus on building the surgical capacity of district hospitals.[7-10]
Current resources and initiatives
Effective surgical services tend to bolster the entire health system and impact positively on other non-surgical services.[7-10] The WHO has responded to this new understanding of the importance of effective surgical systems by developing a number of resources and programmes. In 2005 the Global Initiative for Emergency and Essential Surgery Care was established to increase the capacity of low- and middle-income countries to provide effective surgical services. The Emergency and Essential Surgical Care Project, the Integrated Management of Emergency and Essential Surgical Care toolkit and the textbook Surgical Care at the District Hospital are designed to help resource-constrained institutions establish effective educational and service packages based on the WHO's prescribed minimum standards and technologies for emergency and essential surgical care.[11] The WHO has emphasised the importance of a systematic approach to healthcare.[11,12]
Systems thinking
A healthcare system involves inputs, processes and outcomes.[11,12] Improving the health of a population must address the inputs of healthcare and the processes of delivery of healthcare. The inputs are the money and resources invested in the system, and the processes the way in which healthcare is delivered. The inputs and the processes interact to produce a health outcome. The term 'health system' covers the entire spectrum of care from the recognition and diagnosis of a pathology, through to transfer of the patient to the appropriate facility, up to operative management and postoperative care. Effective treatment depends on all the steps of the healthcare system working harmoniously. Patients must be able to access healthcare facilities easily and timeously. Primary caregivers must be able to recognise surgical pathology and refer the patient to an appropriate facility. Logistics must be organised to ensure quick and efficient transportation of the patient to the appropriate facility, and the receiving facility must be adequately resourced to deal with the problem. If any links in this chain of care are broken, pathology may complicate, and this translates into poor outcomes.
It is important to understand that poor outcomes reflect systematic failure rather than individual failure. To understand the efficiency of the system, administrators need to develop metrics that measure the quality of the system. Mainz has provided an excellent review of quality metrics for healthcare and has identified the following objective criteria for a good metric:[13] It must be relevant, acceptable, feasible, reliable, sensitive to changes, valid, and able to differentiate. In addition, whatever disease is chosen as an indicator needs to be sufficiently common to provide a large enough denominator, and ideally should be curable.
What is the current state of surgery at district hospital level in South Africa?
In Surgical Care at the District Hospital, the WHO states that basic abdominal surgery should be undertaken at district hospitals. The following procedures are described: laparotomy for trauma, laparotomy for the diagnosis and management of intestinal obstruction, peritonitis, complicated peptic ulcer disease, and appendicitis.[11] However, there remains a discrepancy between the package of care that a district hospital is expected to deliver and the care that is actually delivered, and it is apparent that very few of the procedures discussed in the WHO text are routinely performed in South African district hospitals.
Voss and Duvenage audited the surgical output of 7 district hospitals in the rural Western Cape.[14] The volume of general surgical procedures undertaken was low, and almost no abdominal surgery was undertaken. In their year-long review, only 21 appendicectomies were performed at the 7 district hospitals. Of these, 19 were performed in one hospital and 2 in another. The most commonly performed operations in rural South Africa are obstetric procedures, yet the competency to deliver obstetric anaesthesia safely seems to be deficient in the South African district health system.[15]
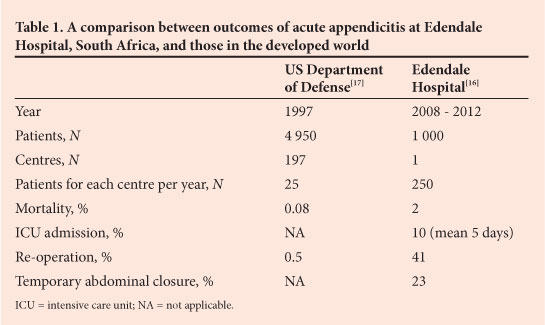
We recently published our experience with acute appendicitis at Edendale Hospital, Pietermaritzburg, South Africa, which differs markedly from that in the developed world. In our setting, acute appendicitis is a disease that presents late and is associated with diagnostic delay and significant morbidity and even mortality.[16] We reviewed 1 000 consecutive patients with acute appendicitis treated at Edendale Hospital between 2008 and 2012. Two-thirds were male, and the median age was 19.5 years. Medical care was sought on average 4 days after the onset of symptoms. Twenty-three per cent required temporary abdominal closure and 40% required repeat operation. The mortality rate was 2%, and just under 10% required intensive care unit (ICU) admission. There were significant complications, which included pneumonia (12.5%), wound dehiscence (7%) and renal failure (3%), and 11% required admission to the ICU. Our cohort had a perforation rate of 54%, and the high incidence of perforation often mandated formal laparotomy rather than a local incision. This is very different to the published experience with acute appendicitis from the developed world, where perforation rates are generally in the order of 20% or less and temporary abdominal closure and the need for ICU admission are almost unheard of.[17] Table 1 compares the outcomes of acute appendicitis at our institution with those in the developed world.
These poor outcomes reflect a dysfunctional system of surgical care, and it is apparent that the surgical system in the district hospitals of South Africa is deficient and has been allowed to deteriorate alarmingly. Strategies to turn this situation around are urgently required. Part of such a turnaround strategy must be the development of appropriate metrics to allow us to benchmark current performance, to develop targets, and to assess whether we ultimately reach these objectives.
Developing quality metrics for surgical care
There is a need to develop tools to measure the quality of our surgical care system in South Africa. Maternal and child health is very developed in terms of applying routinely collected statistics to assess the quality of a system. Infant mortality rates and maternal mortality rates are crude markers that reflect the overall quality of the service. Developing a marker for the efficiency of a modern surgical service remains a challenge. A number of operations and surgical conditions fit this definition. These include amputation, which generally occurs in the more elderly group and is associated with both morbidity and mortality, elective hernia repair, which is not generally associated with significant mortality, and traumatic brain injury.[18]
Acute appendicitis is a disease that may allow for the development of a qualitative measure of output of a surgical system. It is a common disease, which is completely cured by a relatively straightforward surgical intervention. Systems failure in the form of delayed diagnosis and recognition results in significant morbidity. A number of clinical outcomes in the management of acute appendicitis many be useful as markers of quality of care. These potential metrics include delay to definitive treatment, perforation rates, laparotomy rates, re-operation rates, ICU admission rates, open abdomen rates and mortality rates. These criteria meet the listed requirements for an effective indicator of quality of care and should be routinely collected by hospital and surgical administrators.
Ongoing efforts must be directed at developing and validating quality metrics for surgical care and using them to drive a turnaround strategy for district level surgery in South Africa.
Conclusion
The surgical capacity of district hospitals in South Africa has been allowed to deteriorate at an alarming rate, and a turnaround strategy is urgently needed. Part of this strategy must be the collection of a data set that functions as a quality metric for surgical services. This is analogous to the routine data collected to assess the quality of maternal and child health services. A number of potential pathologies and procedures meet the criteria to be considered markers of the quality of the system. Acute appendicitis in our environment is associated with prolonged delays to definitive treatment as well as significant morbidity, and is a good example of a potential quality metric. We suggest that the routine collection of basic data on acute appendicitis may well provide hospital managers with a tool to measure the output of a surgical system. These data would be relatively easy for managers to collect and collate and would expedite a repeatable and reproducible system of monitoring the effectiveness of a surgical service. Further research is needed to identify and validate a number of other potential quality markers, which include diabetic foot sepsis, traumatic brain injury and inguinal hernia repair.
REFERENCES
1. Nordberg EM. Incidence and estimated need of caesarean section, inguinal hernia repair and operation for strangulated hernia in rural Africa. BMJ 1984;289(6437):92-93. [http://dx.doi.org/10.1136/bmj.289.6437.92] [ Links ]
2. Nordberg E, Mwobobia I, Muniu E. Major and minor surgery output at district level in Kenya: Review and issues in need of further research. Afr J Health Sci 2002;9(1-2):17-25. [http://dx.doi.org/10.4314/ajhs.v9i1.30752] [ Links ]
3. Nordberg E. Surgical operations in eastern Africa: A review with conclusions regarding the need for further research. East Afr Med J 1990;67(3 Suppl):1-28. [ Links ]
4. Debas H, Gosselin R, McCord C, Thind A. Surgery. In: Jamison D, ed. Disease Control Priorities in Developing Countries. 2nd ed. New York: Oxford University Press, 2006. [ Links ]
5. Ozgediz D, Jamison D, Cherian M, McQueen K. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ 2008;6:646-647. [ Links ]
6. Spiegel DA, Gosselin RA. Surgical services in low-income and middle-income countries. Lancet 2007; 370(9592):1013-1015. [http://dx.doi.org/10.1016/S0140-6736(07)61457-3] [ Links ]
7. Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: A modeling strategy based on available data. Lancet 2008;372(9633):139-144. [http://dx.doi.org/10.1016/S0140-6736(08)60878-8] [ Links ]
8. Gosselin RA, Amardeep Thind A, Bellardinelli A. Cost/DALY averted in a small hospital in Sierra Leone: What is the relative contribution of different services? World J Surg 2008;30(4):505-511. [http://dx.doi.org/10.1007/s00268-005-0609-5] [ Links ]
9. Gosselin RA, Heitto M. Cost-effectiveness of a district trauma hospital in Battambang, Cambodia. World J Surg 2008;32(11):2450-2453. [http://dx.doi.org/10.1007/s00268-008-9708-41 [ Links ]
10. Bickler S, Spiegel D. Global surgery - defining a research agenda. Lancet 2008;372(9633):90-92. [http://dx.doi.org/10.1016/S0140-6736(08)60924-1] [ Links ]
11. World Health Organization. Surgical Care at the District Hospital. 2003. http://www.who.int/surgery/publications/en/SCDH.pdf (accessed 31 January 2013). [ Links ]
12. Bellagio Essential Surgery Group. http://essentialsurgery.org/bellagio/ (accessed 31 January 2013). [ Links ]
13. Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 2003;15(6):523-530. [http://dx.doi.org/10.1093/intqhc/mzg081] [ Links ]
14. Voss M, Duvenage R. Operative surgery at the district hospital. S Afr Med J 2011;101(8):521-522. [ Links ]
15. Farina Z, Rout C. 'But it's just a spinal': Combating increasing rates of maternal death related to spinal anaesthesia. S Afr Med J 2013;103(2):81-82. [http://dx.doi.org/10.7196/samj.6308] [ Links ]
16. Kong VY, Bulajic B, Allorto NL, Handley J, Clarke DL. Acute appendicitis in a developing country. World J Surg 2012;36(9):2068-2073. [http://dx.doi.org/10.1007/s00268-012-1626-9] [ Links ]
17. Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP (1995) Appendectomy-a contemporary appraisal. Ann Surg 225(3):252-261 [http://dx.doi.org/10.1097/00000658-199703000-00003] [ Links ]
18. Alexander T, Fuller G, Hargovan P, Clarke DL, Muckart DJ, Thomson SR. An audit of the quality of care of traumatic brain injury at a busy regional hospital in South Africa. S Afr J Surg 2009;47(4):120-126. [ Links ]
 Correspondence:
Correspondence:
D L Clarke
(damianclar@gmail.com)














