Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.51 n.2 Cape Town Jan. 2013
CASE REPORT
Posterolateral diaphragmatic hernia with small-bowel incarceration in an adult
G Wenzel-Smith
StateExamMed (Germany), FCFP (SA) Victoria Hospital, Wynberg, Cape Town, South Africa
ABSTRACT
Bochdalek hernia (BH), a closing defect ofthe peripheral posterior aspect ofthe diaphragm, is the most common ofthe congenital diaphragmatic hernias and is usually diagnosed in neonates. Symptomatic presentation of a right-sided diaphragmatic hernia in an adult is unusual. Owing to their rarity and varied presentation, these hernias can pose a diagnostic challenge. A right-sided BH in a 40-year-old woman who presented with respiratory distress associated with abdominal pain and symptoms of small-bowel obstruction is reported. Midline laparotomy revealed necrotic small bowel and faecothorax of the pleural cavity. Diaphragmatic hernias should be included in the differential diagnosis of patients with acute or chronic gastrointestinal, or less frequently respiratory, symptoms.
A posterolateral diaphragmatic hernia (Bochdalek hernia, BH) in a 40-year-old woman is reported. The patient presented with respiratory distress and symptoms of small-bowel obstruction. At emergency laparotomy the perforated small bowel in the hernia was resected. She recovered well. A review of the literature confirms the extreme rarity of this condition and its often delayed presentation in adults, together with the value of a chest radiograph and computed tomography (CT) scanning in establishing the diagnosis.
Case report
A 40-year-old woman, known to have hypertension and asthma, presented with a 4-day history of severe abdominal pain, with nausea, vomiting and constipation for the past 2 days. There was no history of blunt or penetrating abdominal or thoracic injury.
The patient had dyspnoea and tachycardia. Her systolic blood pressure was 124 mmHg and there was reduced air entry into the right lung. Her abdomen was distended, with maximal pain and rebound tenderness in the right upper quadrant.
The white cell count was 18x109/l and the oxygen saturation 82% on room air. Measurement of arterial blood gases indicated the presence of type I respiratory failure.
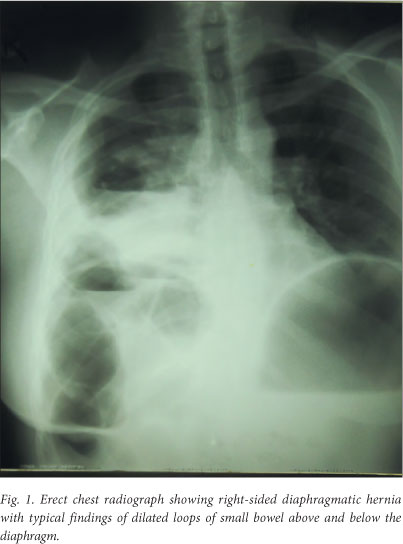
Chest radiographs (Figs 1 and 2) showed dilated loops of small bowel in the right pleural cavity, which were also seen on the abdominal radiograph. A diagnosis of right-sided diaphragmatic hernia was made.

At emergency midline laparotomy, 15 cm of herniated perforated necrotic small bowel was removed from the right pleural cavity and resected, and the bowel was anastomosed. After pleural toilet, a right-sided intercostal drain was inserted, the 10 cm defect in the posterior diaphragm repaired with interrupted polydiaxonone sutures, and the abdomen closed. The patient required organ support postoperatively and was transferred to the intensive care unit (ICU).
Postoperatively, gut function was slow to return and a small empyema resolved with sustained drainage and antibiotics. She spent 8 days in the ICU and was discharged on day 12 after initial presentation. At follow-up 1 month later she was well despite some superficial wound sepsis.
Discussion
Vincent Alexander Bochdalek named the fusion defect of the posterolateral foramina of the diaphragm in 1848.[1] The prevalence of the condition ranges from 1:2 000 to 1:12 500 births.[1,2]
The diaphragm develops during the 1st - 4th month of embryonic development, in which period fusion defects of the diaphragm can occur, resulting in posterolateral defects (BH, 95%), anterior-retrosternal defects (Morgagni hernias, 4%) and hiatal hernias and septum transversum defects (1%).[2] Only 20% of BHs are on the right side,[1] and fewer than 20 clinical cases presenting with complications have been reported in adults.[1,3] The reasons postulated for these observations are the earlier closure of the pleuroperitoneal canal on the right side than on the left, and the protective effect of the liver on the right diaphragm.
Incarcerated diaphragmatic hernias present with a variety of symptoms - abdominal, respiratory, and even urinary tract. BH can therefore easily be misdiagnosed. Despite a fairly- characteristic abnormality on the plain chest radiograph in our patient, the small bowel had already perforated and she was fortunate to recover from the critical illness so well. Delay in diagnosis inevitably increases morbidity and mortality associated with this condition. Granier et al. reported a case in which delayed diagnosis of an incarcerated BH contributed to the death of a 54-year-old woman due to sepsis.[4]
Slesser et al.[3] compared 12 cases of BH containing colon. The patients were aged 20 - 76 years, and the majority (10 out of 12) were female. Eight of the 12 patients had spontaneous hernias, while the remaining 4 had suffered trauma or developed their hernias postoperatively. This is interesting, as it goes against the previously postulated theory that the usual cause of BH in adults is post-traumatic.[5]
The majority of the hernias in the report by Slesser et al.m were diagnosed by CT. It is clear from more recent reports in the era of multi-detector computed tomography (MDCT) that small asymptomatic hernias are being detected to an increasing extent when scanning for other indications. Temizöz et al. reported a 10.5% prevalence of BHs in MDCTs of 1 350 asymptomatic adults,[2] and Kinoshita et al. a 12.7% prevalence in MDCTs of 3 107 patients.[6] Prevalences in the age groups 50s, 60s and 70s were 10.5% (168/1 596), 13.7% (137/1 003) and 20.3% (80/394), respectively.[6]
Because incidentally observed BHs might be more common than previously postulated[2,6] occurring in up to 20% of people by age 70 years,[6] the differential diagnosis should be considered in patients with acute or chronic gastrointestinal or respiratory symptoms.
There seems to be little evidence that BHs should be surgically repaired unless they are symptomatic.
Competing interests. None declared.
Funding. None.
Ethical approval. Written informed consent to the publication was obtained from the patient.
REFERENCES
1. Laaksonen E, Silvasti S, Hakala T. Right-sided Bochdalek hernia in an adult: A case report. Journal of Medical Case Reports 2009;3:9291-9296. [http://dx.doi.org/10.1186/1752-1947-3-92911 [ Links ]
2. Temizöz O, Gençhellaç H, Yekeler E, et al. Prevalence and MDCT characteristics of asymptomatic Bochdalek hernia in adult population. Diagn Interv Radiol 2010;16(1):52-55. [http://dx.doi.org/10.4261/1305-3825.DIR.2750-09.11 [ Links ]
3. Slesser A, Ribbans H, Blunt D, Stanbridge R, Buchannan G. A spontaneous right-sided Bochdalek hernia containing perforated colon. JRSM Short Reports 2011;2(7):54-58. [http://dx.doi.org/10.1258/shorts.2011.0110561 [ Links ]
4. Granier V, Coche E, Hantson P, Thoma M. Intrathoracic caecal perforation presenting as dyspnea. Case Report Med 2010;296730. [http://dx.doi.org/10.1155/2010/2967301 [ Links ]
5. Sofi FA, Ahmed SH, Dar MA, Nabhi DG, Bhat MA, Tabassum PN. Nontraumatic massive right-sided Bochdalek hernia in an adult: An unusual presentation. Am J Emerg Med 2011;29(3):356.e5-356.e7. [http://dx.doi.org/10.1016/j.ajem.2010.03.0341 [ Links ]
6. Kinoshita E, Ishiyama M, Honda S, Matsuzako M, Oikado K, Kinoshita T. Late-presenting posterior transdiaphragmatic (Bochdalek) hernia in adults: Prevalence and MDCT characteristics. J Thorac Imaging 2009;24(1):17-22. [http://dx.doi.org/10.1097/RTI.0b013e31818c6bc81 [ Links ]
 Corresponding author:
Corresponding author:
G Wenzel-Smith
(gisela@doctors.org.uk)














