Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Science
versión On-line ISSN 1996-7489
versión impresa ISSN 0038-2353
S. Afr. j. sci. vol.119 no.1-2 Pretoria ene./feb. 2023
http://dx.doi.org/10.17159/sajs.2023/13594
RESEARCH ARTICLE
COVID-19 and common mental disorders among university students in South Africa
Jason BantjesI, II; Sonja SwanevelderIII; Esme JordaanIII; Nancy A. SampsonIV; Maria V. PetukhovaIV; Christine LochnerV; Dan J. SteinV, VI; Ronald C. KesslerIV
IAlcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Cape Town, South Africa
IIInstitute for Life Course Health Research, Department of Global Health, Stellenbosch University, Stellenbosch, South Africa
IIIBiostatistics Unit, South African Medical Research Council, Cape Town, South Africa
IVDepartment of Health Care Policy, Harvard Medical School, Boston, Massachusetts, USA
VSAMRC Unit on Risk and Resilience in Mental Disorders, Department of Psychiatry, Stellenbosch University, Stellenbosch, South Africa
VIDepartment of Psychiatry and Mental Health, University of Cape Town, Cape Town, South Africa
ABSTRACT
COVID-19 has had far-reaching economic, social and health consequences, with vulnerable groups disproportionally affected. Even before the COVID-19 pandemic, concern was expressed about university students' mental health, with global data suggesting students are more vulnerable than the general population to mental disorders. Yet, it is unclear what the pandemic's impact has been on the mental health of students in South Africa. We examined the impact of COVID-19 on first-year students at two universities in South Africa by analysing changes in the prevalence and age-of-onset of three common mental disorders (namely major depressive episode, generalised anxiety disorder, and suicidal ideation) before and during the pandemic, and comparing these to changes between 2015 and 2017. Our analysis of cross-sectional survey data collected in 2015, 2017 and 2020 shows no clear or consistent pattern of increases in prevalence of common mental disorders following the start of the pandemic. Lifetime prevalence rates of common mental disorders among students have been steadily increasing since 2015, and where increases before and during COVID-19 were observed, they are not consistently larger than increases between 2015 and 2020. No significant changes were observed in the 12-month prevalence of common mental disorders before and during COVID-19, except for an increase in prevalence of depression at one institution, and a decrease in suicidal ideation at the other. Findings suggest that in the context of ongoing adversity and disruptions on South African university campuses in recent years, COVID-19 may be just one more stressor local students face and that its impact on student mental health may not have been as marked in South Africa compared to other regions.
SIGNIFICANCE:
• This study is the first to explore COVID-19's impact on university students' mental health in South Africa, using data collected before and during the pandemic.
• High rates of psychopathology confirm the need for sustainable campus-based interventions to support student well-being.
• Rates of mental disorders among students have been increasing since 2015, and increases observed in 2020 were no larger than those observed in prior years.
• In the context of disruptions on university campuses in recent years, COVID-19 is just one more stressor for students, and its impact may not have been as marked in South Africa compared to other regions.
Keywords: COVID-19, university students, South Africa, depression, anxiety, suicidal ideation
Introduction
The global COVID-19 pandemic that started in December 2019 has had far-reaching economic, educational, and mental health consequences, not least of all because of widespread and sustained restrictions on people's movement, freedom, and ability to work. As with all pandemics, COVID-19 has exacerbated inequalities and disproportionally affected marginalised and vulnerable groups1, including young people in low- and middle-income countries (LMICs) whose education was severely disrupted as schools and universities closed their doors and moved to online teaching2. Increases in rates of depression and anxiety since the outbreak of COVID-19 have been documented in the general population3-5 and among university students6,7, although global suicide rates appear to have been largely unaffected so far8,9. However, many of the studies on mental health and COVID-19 have relied on cross-sectional data at a single point in time, with no direct comparisons to data collected in the same population and with the same methods before COVID-19. Understanding the impact of COVID-19 on the mental health of university students in LMICs is important to plan interventions to ameliorate the psychological consequences of the pandemic on higher education, particularly because academic performance is affected by students' mental health.10 Promoting university students' mental health (and hence educational retention and academic success) in the post-COVID-19 period will be integral to stimulating economic recovery, especially in LMICs where the economic fallout of the pandemic has been hard felt.11
Globally, universities have been increasingly concerned about the prevalence of common mental disorders and suicidal behaviour among undergraduate students even before COVID-19.12-14 One pre-COVID-19 survey of students from 19 universities across eight countries (Australia, Belgium, Germany, Mexico, Northern Ireland, South Africa, Spain, USA) reported 12-month prevalence rates of 35% for at least one common mental disorder among first-year students15, and 12-month prevalence rates for suicidal ideation, plan, and attempt of 17.2%, 8.8%, and 1.0%, respectively13. The prevalence of psychopathology among undergraduate students is partly attributed to psychosocial stressors associated with this developmental period (i.e. greater academic demands, leaving home for the first time, increased exposure to substances, and financial pressures) and the fact that the onset of mental disorders is typically in late adolescence or early adulthood. Depression, anxiety, and suicidal ideation are the most common symptoms of mental disorders reported by students and are associated with severe role impairment in academic and social functioning.16 Our earlier work in South Africa suggested that providing effective treatment to first-year students with major depressive disorder and/or attention deficit hyperactivity disorder could yield a 23.0% proportional reduction in prevalence of academic failure, highlighting the importance of promoting mental health as a strategy for raising educational attainment.17
There has been a marked increase in the incidence of depressive and anxiety disorders following the outbreak of COVID-19 in both the general population and among university students. An analysis of the best available global survey data with measurements of anxiety and depression both before and during the pandemic, using the Global Burden of Disease Study model, estimated an additional 53.2 million cases of depressive disorder and 76.2 million cases of anxiety disorder globally (equivalent to a 27.6% increase in depression and a 25.6% increase in anxiety disorders).4 Studies have also documented university students' psychological distress during COVID-19 in many countries including the UK18, Poland19, China20, Delhi21, Columbia22 and Bangladesh23. However, many of these studies, particularly those conducted in LMICs21-23, have relied on cross-sectional data measuring symptom severity at a single point in time during the pandemic without making direct or meaningful comparisons to pre-COVID-19 assessments. The aim of this study was to investigate changes before and during COVID-19 in the12-month prevalence of major depressive episode (MDE), generalised anxiety disorder (GAD), and suicidal ideation among first-year university students in South Africa. We report on data collected at two universities in 2015, 2017 and 2020 using identical survey methods at each of the three timepoints, as part of the ongoing work of the World Health Organization's World Mental Health Surveys International College Student Initiative (WMHS-ICS).24
Methods
The aim of this study was to investigate the impact of COVID-19 on the mental health of first-year university students in South Africa by: (1) comparing changes in the prevalence of symptoms of three common mental disorders (i.e. MDE, GAD and suicidal ideation) as well as changes in the pattern of onset of these disorders at three time points (i.e. 2015, 2017 and 2020) and (2) establishing if any changes in the prevalence of these disorders might be a result of changes in the demographic profile of students between 2015 and 2020.
Data collection
Data were collected as part of a larger study of student mental healthcare needs in South Africa and in conjunction with the ongoing work of the WMHS-ICS.24 All first-year students at Stellenbosch University (SU)
in 2015 (W=5338), 2017 (N=5163) and 2020 (N=5584), and the University of Cape Town (UCT) in 2017 (N=3662) and 2020 (N=5408), were invited via email (sent directly to students by the institution) to participate in an anonymous online survey, of which 2271 students completed the surveys. The 2020 data were collected between 14 April and 10 July 2020. To be included in the study, students had to be enrolled as first-year students at one of the participating universities and had to give informed consent.
Measures
The following data were collected via an online survey:
Sociodemographic characteristics
Participants were asked their age, parents' level of education, whether they had a serious physical impairment, whether they suffered from any chronic illnesses, and how they identify in terms of gender, population group, and sexual orientation. We identified students as 'first-generation students' if neither of their parents had completed tertiary education. Students were identified as having a disability if they reported any serious physical impairment (e.g. vision, hearing, and movement impairment) or chronic health problem (e.g. asthma, diabetes, migraine, chronic pain disorder). For gender, students self-identified as female, male or gender non-conforming. In terms of population group students identified as black (i.e. black African, coloured or Asian) or white. A broad definition of 'black' was used to identify all students from historically excluded population groups; the use of these categories is not intended to reify sociocultural constructs, but rather used with the aim of investigating ongoing social and economic disparities with access to health care, education, and employment opportunities in South Africa. Sexual orientation was dichotomised as heterosexual (i.e. no same sex attraction) or 'sexual minority' (i.e. lesbian, gay, bisexual, asexual or questioning).
Common mental disorders
We assessed the lifetime and 12-month prevalence and age of onset for MDE, GAD, and suicidal ideation using items adapted from the Composite International Diagnostic Interview Screening Scales (CIDI-SC).25,26 The CIDI-SC has good concordance with blinded clinical diagnoses based on the Structured Clinical Interview for DSM-IV (SCID)27, with an area under the curve in the range 0.70-0.78.25,26 Suicidal ideation was assessed using a modified version of the Columbia Suicidal Severity Rating Scale (C-SSRS), which has demonstrated good convergent and divergent validity with other multi-informant suicidal ideation and behaviour scales used with adolescents, as well as showing high sensitivity and specificity for suicidal behaviour classifications compared with other behaviour scales and clinician evaluation.28 We assessed passive suicidal ideation (i.e. Did you ever in your life wish you were dead or would go to sleep and never wake up?) and active suicidal ideation (Did you ever in your life have thoughts of killing yourself?). Students who endorsed either of these items were identified as reporting suicidal ideation.
Data analysis
Data were weighted by population group and gender within each institution across each year to adjust for differences between survey respondents and the populations of the student body, and changes in the demographic profile of students between 2015 (SU only), 2017 (SU and UCT) and 2020 (SU and UCT). First, we calculated lifetime and 12-month prevalence estimates for MDE, GAD, suicidal ideation, and any of these three outcomes within each university across each year, as well as the lifetime cumulative and conditional incidence of each of the above separately before COVID-19 (2015 and 2017) and during COVID-19 (2020). Second, we estimated the 12-month persistence among prior lifetime cases before and during COVID-19 along with age of onset curves for each disorder. Finally, we used regression analysis to establish if any observed changes in prevalence rates were a function of changes in the demographic profile of students admitted to university over this period. The results of the regression analysis are reported as corrected odds ratios (i.e. risk ratios) with 95% confidence intervals (CIs) for the adjusted main effects. Alpha was set as 0.05 for all tests of significance.
Ethical clearance
Ethical clearance for the study was obtained from the Health Sciences Research Ethics Committees at SU and UCT. Institutional permission to contact students was also obtained prior to data collection.
Results
Sample characteristics
The sociodemographic characteristics for the sample of students who completed the survey (N=2271) and the population of all first-year students at each institution in 2015, 2017 and 2020 are presented as supplementary material (see Supplementary tables 1 and 2). Although the samples from both institutions in all three years consisted predominantly of students who identified as female and black (Supplementary tables 1 and 2), there were significant differences in the sociodemographic profiles of the population of students across the different years in both institutions (p<0.001). Consequently, prior to substantive analysis, the data were weighted by gender and population group for each institution separately across the three years, to adjust for the differences between the sample and the population and to control for changes in the demographic profile of the student body over time.
Lifetime and 12-month prevalence of common mental disorders
The lifetime prevalence of MDE, GAD, suicidal ideation, and any of these three outcomes in each institution are shown in Table 1a (SU in 2015, 2017 and 2020) and Table 1b (UCT in 2017 and 2020). At SU between 2015 and 2017, there were significant increases in the lifetime prevalence of MDE (20.5% vs 27.4%, p=0.009) and suicidal ideation (42.9% vs 49.6%, p=0.035), but no changes for GAD and for any disorder (p>0.05). Between 2017 and 2020, the lifetime prevalence at SU increased significantly for all outcomes (MDE: 27.4% vs 47.6%, p<0.0001; GAD: 23.3% vs 29.6%, p=0.039; suicidal ideation: 49.6% vs 60.0%, p=0.003: any disorder: 57.8% vs 70.9%, p<0.0001). At UCT between 2017 and 2020, there were no significant changes in the lifetime prevalence for any of the outcomes we assessed (p>0.05).
The 12-month prevalence of MDE, GAD, suicidal ideation and any of these outcomes is shown in Table 2a (for SU) and 2b (for UCT). Prevalence estimates for co-morbidity are presented as supplementary material (see Supplementary table 3). The 12-month prevalence at SU increased significantly between 2015 and 2017 for MDE (16.8% vs 24.4%, p=0.002), suicidal ideation (24.1% vs 36.9%, p<0.0001) and any disorder (36.6% vs 47.8%, p=0.0004), but not for GAD (p=0.076). By comparison, between 2017 and 2020, the only significant change in 12-month prevalence was for MDE (24.4% vs 40.3%, p<0.0001), with no changes for GAD, suicidal ideation, and any disorder (p>0.05). Between 2017 and 2020 at UCT, the 12-month prevalence did not change significantly for MDE, GAD or any disorder (p>0.05), and decreased significantly for suicidal ideation (48.9% to 36.0%, p=0.006).
The 12-month prevalence among lifetime cases (i.e. the proportional persistence) of MDE, GAD, suicidal ideation and any of these outcomes is shown in Table 3a (for SU) and 3b (for UCT). The proportional persistence between 2015 and 2017 at SU increased significantly for suicidal ideation (56.2% vs 74.4%, p<0.0001) and for any disorder (71.0% vs 82.7%, p=0.002), but did not change significantly for MDE or GAD (p>0.05). Between 2017 and 2020 at SU no significant increases were observed in the proportional persistence for any of the outcomes (p>0.05), although a significant reduction was observed in persistence of suicidal ideation (74.4% vs 54.4%, p<0.0001), and no significant reductions were observed for MDE, GAD, and any disorder (p>0.05).
A similar pattern emerged at UCT between 2017 and 2020, with significant decreases for suicidal ideation (76.8% vs 58.0%, p=0.001) but no significant decreases for MDE, GAD, and any disorder (p>0.05).
The 12-month prevalence among lifetime cases as of 2 years ago (i.e. proportion of current cases with onset of symptoms 2 or more years previously) of MDE, GAD, suicidal ideation and any of these outcomes are shown in Table 4a (for SU) and 4b (for UCT). The proportion of 12-month cases with onset of symptoms 2 or more years previously increased significantly at SU between 2015 and 2017 for suicidal ideation (52.7% vs 70.7%, p<0.003) and for any disorder (69.8% vs 80.4%, p=0.011), but did not change significantly for MDE or GAD (p>0.05). Between 2017 and 2020 (i.e. before and after COVID-19), the proportion decreased significantly for suicidal ideation (70.7% vs 55.0%, p=0.002), and showed no significant changes for MDE, GAD, or any disorder (p >0.05). A very similar pattern was observed at UCT between 2017 and 2020 with a significant decrease observed for suicidal ideation (75.5% vs 58.5%, p=0.006) and no significant changes observed for all other disorders (p>0.05).
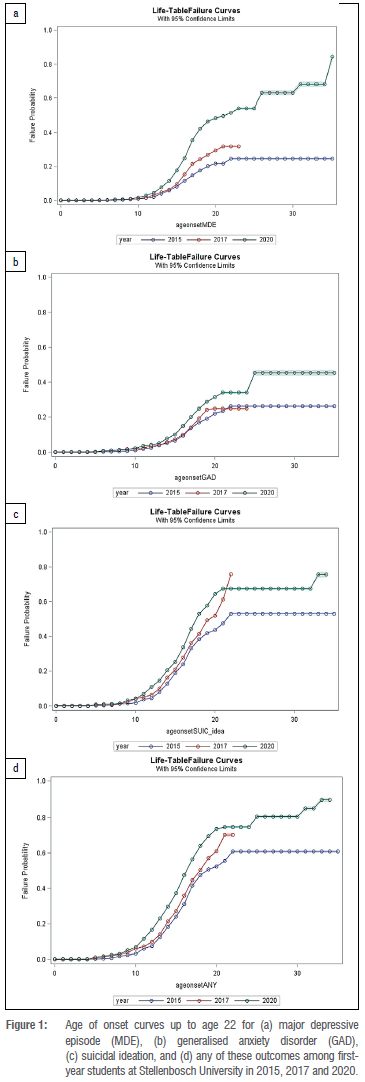
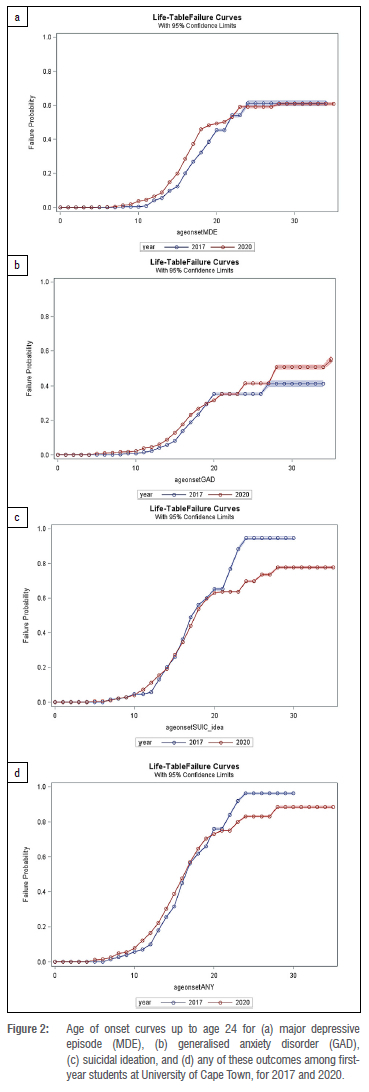
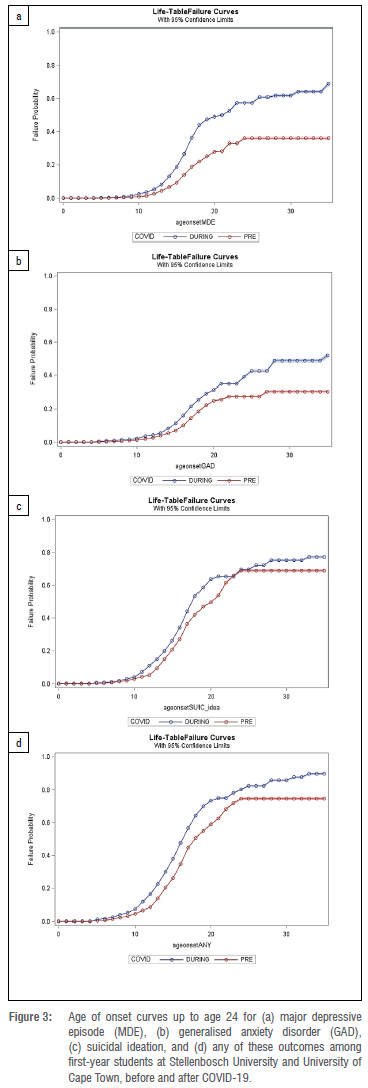
Age of onset for common mental disorders
The age of onset distribution for MDE, GAD, suicidal ideation, and any of these three outcomes up to age 22 years across both institutions is shown in Figure 1 (SU), Figure 2 (UCT) and Figure 3 (UCT and SU pooled). The log-rank tests (Tukey-Kramer adjustment) show that the age of onset failure times for MDE, GAD, suicidal ideation, and any of these outcomes at SU (across 2015, 2017 and 2022) and UCT (2017 and 2020) are all significantly different from each other (p<0.0001). These curves show consistently that the age of onset for all disorders in both institutions was earlier in 2020 compared to 2017, and at SU the age of onset for all disorders was earlier in 2017 compared to 2020. These results demonstrate that over time students were developing symptoms at a younger and younger age, and that this contributed to the higher prevalence rates observed before and after COVID-19.
Net effects controlling for demographic changes in student enrolment
Regression analysis was used to establish if the observed changes in prevalence estimates shown in Table 2 are a function of changes in the demographic composition of the students over time. Table 5 shows the analysis of net changes in lifetime prevalence as of 2 years prior for each of the outcomes, with Model 1 illustrating the gross effect over time and Model 2 including controls for changes in the sociodemographic profile of students. As seen in Table 5a, after controlling for changes in the demographic composition of the student body, there was a significant increase in the proportion of first-year students at SU already exhibiting symptoms of MDE before they arrived at university between 2015 and 2017 (RR=1.4, 95% CI=1.1-1.8) and between 2017 and 2020 (RR=1.8, 95% CI=1.5-2.1), with the changes observed between 2015 and 2017 not significantly different from changes between 2017 to 2020 (p=0.327). For GAD, the lifetime prevalence as of 2 years prior at SU showed no significant changes between 2015 and 2017 (RR=1.0, 95% CI=0.8-1.4) but increased significantly between 2017 and 2020 (RR=1.3, 95% CI=1.0-1.7), although again the change from 2015 to 2017 was not significantly different from the change between 2017 and 2020 (p=0.304). For suicidal ideation, no significant change was observed between 2015 and 2017 (RR=1.0, 95% CI=0.9-1.2) but a significant increase occurred between 2017 and 2020 (RR=1.2, 95% CI = 1.1-1.4), although the change between 2015 and 2017 was not significantly different from the change between 2017 and 2020 (p=0.407). Finally, for any disorder, the change between 2015 and 2017 was not significant (RR=1.0, 95% CI=0.9-1.2), but did change significantly between 2017 and 2020 (RR=1.3, 95% CI=1.2-1.4), although again the change between 2015 and 2017 was not significantly different from the change between 2017 and 2020 (p=0.249).
As shown in Table 5b, at UCT the lifetime prevalence as of 2 years prior increased significantly between 2017 and 2020 for MDE (RR=1.4, 95% CI=1.1-1.8), but did not change significantly for GAD (RR=11.1, 95% CI=0.8-1.6), suicidal ideation (RR=0.9, 95% CI=0.7-1.1) or for any of these outcomes (RR=1.0, 95% CI = 0.9-1.2) controlling for changes in demographic characteristics of students.
The regression analysis of the net effect of changes in 12-month prevalence among students with lifetime disorder as of 2 years ago, as well as the analysis of changes in 12-month prevalence among students without a lifetime disorder as of 2 years ago are provided as supplementary material (see Supplementary tables 4 and 5). At SU, the 12-month prevalence among lifetime cases as of 2 years prior for MDE and GAD did not change significantly between 2015 and 2017 or between 2017 and 2020, controlling for changes in demographic profile of the students. However, suicidal ideation increased significantly between 2015 and 2017 (RR=1.6, 95% CI = 1.3-2.0) and decreased significantly between 2017 and 2020 (RR=0.6, 95% CI=0.4-0.9), while for any disorder there was a significant increase between 2015 and 2017 (RR=1.3, 95% CI=1.1-1.6) and no change between 2017 and 2020 (RR=1.0, 95% CI=0.7-1.3). A similar pattern was seen at UCT between 2017 and 2020, with no significant changes observed in the 12-month prevalence among students with a lifetime diagnosis as of 2 years prior, for MDE, GAD or any disorder, although a decrease was observed for suicidal ideation (RR=0.4, 95% CI=0.3-0.7).
The 12-month prevalence among students without a lifetime diagnosis as of 2 years ago did not change at SU for MDE between 2015 and 2017 (RR=0.9, 95% CI=0.4-1.9), but increased significantly between 2017 and 2020 (RR=3.1, 95% CI=1.6-6.0) controlling for demographic changes in student composition. There were no significant changes for GAD between 2015 and 2017 (RR=1.6, 95% CI=0.8-2.9) or between 2017 and 2020 (RR=1.4, 95% Ci=0.8-2.5), while suicidal ideation increased between 2015 and 2017 (RR=2.2, 95% CI=1.3-3.7) and did not change between 2017 and 2020 (RR=0.8, 95% CI=0.5-1.5). For any disorder, there was an increase between 2015 and 2017 (RR=2.5, 95% CI=1.5-4.2) but no change between 2017 and 2020 (RR=0.8, 95% CI=0.5-1.4). At UCT between 2017 and 2020 there were no significant changes in the 12-month prevalence among students without a lifetime diagnosis as of 2 years ago in any of the outscores, controlling for demographic changes.
Discussion
We examined the impact of COVID-19 on the mental health of first-year students at two universities in South Africa by analysing changes in the prevalence and onset of three common mental disorders before and during the outbreak of the global pandemic, and comparing these to the changes observed between 2015 and 2017. Our analysis of cross-sectional survey data collected at SU in 2015, 2017 and 2020, and from UCT in 2017, showed no consistent pattern of increases in the prevalence of MDE, GAD and suicidal ideation before and during the first two waves of COVID-19. There were no significant changes in the 12-month prevalence of common mental disorders at either institution before and after the outbreak of COVID-19, except for an increase in prevalence of MDE at SU and a decrease in suicidal ideation at UCT. Our data suggest that while COVID-19 had an impact on the mental health of some students, this impact was not consistently observed across both institutions or across all mental health outcomes, and, where increases were observed between 2017 and 2020, these were mostly no larger than increases previously observed between 2015 and 2017.
These survey data highlight the prevalence of common mental disorders among university students in South Africa and the need for effective and accessible campus-based interventions to promote student wellness. In 2020 the 12-month prevalence for any of the three common mental disorders we assessed was 53.7% and 58.5% at SU and UCT, respectively. MDE was the most common mental health problem reported in the past 12 months (SU: 40.3%; UCT:45.3%), followed by suicidal ideation (SU:32.7%; UCT: 36.0%) and GAD (SU: 27.6%; UCT: 29.7%). These prevalence rates are significantly higher than those observed in the general population29 and confirm the need for an urgent focus on developing scalable student mental health interventions in South Africa.
Between 2017 and 2020, across both institutions, the only significant increase in 12-month prevalence was for MDE at SU (24.4% vs 40.3%). All other outcomes remained unchanged or, in the case of suicidal ideation at UCT, significantly decreased (48.9% vs 36.0%). In contrast, between 2015 and 2017 significant increases were observed at SU for MDE (16.8 vs 24.4%), suicidal ideation (24.1% vs 36.9%), and for any of the outcomes (36.6% vs 47.8%). While lifetime prevalence did not increase between 2017 and 2020 for any of the outcomes at UCT, significant increases were observed at SU for lifetime MDE (27.4% vs 47.6%), GAD (23.3% vs 29.6%), suicidal ideation (49.6% vs 60.0%) and any outcome (57.8% vs 70.9%). Crucially, our findings show that where increases were observed in lifetime prevalence rates, these had started to increase before the outbreak of COVID-19. Furthermore, when adjusting for changes in the demographic profile of students over time, the increases in risk ratios between 2017 and 2020 were not consistently higher than the increases observed between 2015 and 2017, suggesting that some of the changes we observed can be attributed to increased enrolment among students with higher risk of mental disorder (i.e. female students).
To contextualise our findings, it is important to note that university students in South Africa face several serious challenges that pre-date COVID-19, including food insecurity, housing insecurity, and the stress associated with living in a country where violence, crime and trauma are endemic.30-34 In the context of these adversities, COVID-19 is just one more challenge among many. Furthermore, pandemics are not new to South Africa; the enduring HIV and TB syndemic have long affected the lives of many South Africans, including university students.35,36 Indeed, South Africa has the highest number of people living with HIV in the world, with infection rates of 20.4% among 15-49 year olds and an estimated 80 000 TB-related deaths each year.37,38 Local historical, health, and socioenvironmental factors have shaped the impact of COVID-19 in South Africa and hence also students' experiences of the pandemic. 37 It is possible that growing up with the constant presence of multiple life-threatening infectious diseases may have de-sensitised some students to the psychological impact of COVID-19.
It is also important to note that between 2015 and 2017 university students across South Africa participated in mass protests as part of the #FeesMustFall movement39 that aimed, among other things, to resist increases in student fees and decolonise universities. These protests disrupted learning at all South African universities, caused widespread property damage, and led to the cancelation of exams.40,41 The military and riot police were deployed to campuses and sometimes clashed violently with students, resulting in student deaths.42 The disruptions and trauma caused by these protests no doubt had a profound impact on student mental health and likely attributed to the high rates of mental disorders we observed in 2017, especially at UCT where the #FeesMustFall campaign was prolonged and intense. Given this political context in 2017, it is unsurprising that very few changes were observed in the prevalence of common mental disorders between 2017 and 2020, even though there was a global pandemic in this time.
There are also at least three other interpretations of our findings. Firstly, students may be more resilient than is assumed in much of the current student mental health literature, as has been pointed out by authors who have highlighted the dangers of the rise in 'therapeutic education' and the positioning of all students as patients in need of treatment.43 Secondly, diagnostic criteria for mental disorders do not capture all forms of psychological distress and suffering.44 It is possible that there are much higher numbers of students who were distressed by COVID-19 but do not meet the threshold for a disorder and are thus not included in our prevalence estimates. The model of the pandemic as a trauma that leads to psychopathology may not be the most appropriate way to conceptualise the impact of the pandemic on students, despite the widespread usage of the trauma model in this context.44 Thirdly, the data we collected in 2020 was collected between April and July (i.e. during the first waves of the pandemic) and this may have been too soon to capture the full impact of the pandemic on students' mental health.
Limitations
This study is the first in South Africa to examine the impact of COVID-19 on the mental health of first-year university students using cross-sectional data at three timepoints, before and after COVID-19. As such it provides novel insights into the psychological impact of the global pandemic in a LMIC and helps to contextualise this impact within pre-existing high rates of psychological distress among students in South Africa. However, the study has several limitations. First, the low response rate could lead to bias in estimating trends. Nonetheless, the response rate did not change over time, reducing the plausibility of this accounting for lack of a trend. Second, there were important changes in prevalence rates before the pandemic, which makes it much more difficult than otherwise to evaluate pandemic effects. Third, the (non)-effects we observed are based on data collected in the first year of the pandemic and it is possible that effects may have increased in the following year. Finally, we considered data collected only from first-year students at two well-resourced universities in the Western Cape Province. It is possible that a different pattern would be observed among senior students and those attending rural and less well-resourced institutions.
Conclusion
COVID-19 has had far-reaching economic, social and health consequences across the globe, with vulnerable groups disproportionally affected. Concern has been expressed about the mental health of university students globally, even before the pandemic, with data suggesting students are more vulnerable than the general population to common mental disorders and that the prevalence of psychological distress has increased in the wake of COVID-19. Nonetheless our analysis of data collected from first-year students at two universities in South Africa before and during the pandemic suggests that there has not been a clear or consistent pattern of increases in prevalence of MDE, GAD or suicidal ideation, and that where increases are observed, they preceded the pandemic. These findings suggest that, in the context of ongoing adversity and disruptions on South African university campuses in recent years, COVID-19 may be just one more stressor that local students face and that its impact on student mental health may not be as marked in South Africa compared to in other regions.
Acknowledgements
We acknowledge the contributions of Elsie Breet, Wylene Saal and Janine Roos towards the data collection and data management for this project.
The work reported herein was made possible through funding by the South African Medical Research Council (SAMRC) through its Division of Research Capacity Development under the MCSP (awarded to J.B.). This research was also funded by the SAMRC Unit on Risk and Resilience in Mental Disorders. The content hereof is the sole responsibility of the authors and does not necessarily represent the official views of the SAMRC.
Competing interests
In the past 3 years, Dr Kessler was a consultant for Datastat Inc., Holmusk, RallyPoint Networks Inc., and Sage Therapeutics. He has stock options in Mirah, PYM, and Roga Sciences. There are no other interests to declare.
Authors' contributions
J.B.: Data collection; data analysis; writing - the initial draft ; funding acquisition. S.S.: Data analysis; writing - revisions. E.J.: Data analysis; writing - revisions. N.A.S.: Data collection; writing - revisions. M.V.P.: Data collection. C.L.: Data collection; writing - revisions. D.J.S.: Data analysis; writing - revisions; project leadership. R.C.K.: Conceptualisation; methodology; data analysis; writing - the initial draft; project leadership.
References
1. Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74fl1):964-968. http://dx.doi.org/10.1136/jech-2020-214401 [ Links ]
2. Banati P Jones N, Youssef S. Intersecting vulnerabilities: The impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. https://doi.org/10.1057/s41287-020-00325-5 [ Links ]
3. Bareeqa SB, Ahmed SI, Samar SS, Yasin W, Zehra S, Monese GM, et al. Prevalence of depression, anxiety and stress in China during COVID-19 pandemic: A systematic review with meta-analysis. Int J Psychiatry Med. 2021;56(4):210-227. https://doi.org/10.1177/0091217420978005 [ Links ]
4. Taquet M, Holmes EA, Harrison PJ. Depression and anxiety disorders during the COVID-19 pandemic: Knowns and unknowns. The Lancet. 2021;398(10312):1665-1666. https://doi.org/10.1016/S0140-6736(21)02221-2 [ Links ]
5. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health. 2020;16(1):57. https://doi.org/10.1186/s12992-020-00589-w [ Links ]
6. Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students' mental health in the United States: Interview survey study. J Med Internet Res. 2020;22(9), e21279. https://doi.org/10.2196/21279 [ Links ]
7. Wang C, Wen W, Zhang H, Ni J, Jiang J, Cheng Y et al. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: A systematic review and meta-analysis. J Am Coll Health. 2021;1-8. https://doi.org/10.1080/07448481.2021.1960849 [ Links ]
8. Pirkis J, John A, Shin S, DelPozo-Banos M, Arya V Analuisa-Aguilar P et al. Suicide trends in the early months of the COVID-19 pandemic: An interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579-588. https://doi.org/10.1016/S2215-0366(21)00091-2 [ Links ]
9. Pirkis J, Gunnell D, Shin S, del Pozo-Banos M, Arya V, Aguilar PA, et al. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: An interrupted time series analysis in 33 countries. EClinicalMedicine. 2022;51, Art. #101573. [ Links ]
10. Bruffaerts R, Mortier P Kiekens G, Auerbach RP Cuijpers P Demyttenaere K, et al. Mental health problems in college freshmen: Prevalence and academic functioning. J Affect Disord. 2018;225:97-103. https://doi.org/10.1016/j.jad.2017.07.044 [ Links ]
11. Miguel E, Mobarak AM. The economics of the COVID-19 pandemic in poor countries. SSRN. 2021 Oct 11 [cited 2022 Jan 26]. https://doi.org/10.3386/w29339 [ Links ]
12. Auerbach RP Alonso J, Axinn WG, Cuijpers P Ebert DD, Green JG, et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. 2016;46(14):2955-2970. https://doi.org/10.1017/S0033291716001665 [ Links ]
13. Mortier P Auerbach RP Alonso J, Bantjes J, Benjet C, Cuijpers P et al. Suicidal thoughts and behaviors among first-year college students: Results from the WMH-ICS project. J Am Acad Child Adolesc Psychiatry. 2018;57(4):263-273.e1. [ Links ]
14. Kiekens G, Hasking P Bruffaerts R, Alonso J, Auerbach RP Bantjes J, et al. Non-suicidal self-injury among first-year college students and its association with mental disorders: Results from the World Mental Health International College Student (WMH-ICS) initiative. Psychol Med. 2021:1-12. https://doi.org/10.1017/S0033291721002245 [ Links ]
15. Auerbach RP Mortier P Bruffaerts R, Alonso J, Benjet C, Cuijpers P et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623-638. https://doi.org/10.1037/abn0000362 [ Links ]
16. Alonso J, Vilagut G, Mortier P Auerbach RP Bruffaerts R, Cuijpers P et al. The role impairment associated with mental disorder risk profiles in the WHO World Mental Health International College Student Initiative. Int J Methods Psychiatr Res. 2019;28(2), e1750. https://doi.org/10.1002/mpr.1750 [ Links ]
17. Bantjes J, Saal W, Gericke F, Lochner C, Roos J, Auerbach RP et al. Mental health and academic failure among first-year university students in South Africa. S Afr J Psychol. 2020;51(3):396-408. https://doi.org/10.1177/0081246320963204 [ Links ]
18. Savage MJ, James R, Magistro D, Donaldson J, Healy LC, Nevill M, et al. Mental health and movement behaviour during the COVID-19 pandemic in UK university students: Prospective cohort study. Ment Health Phys Act. 2020;19, Art. #100357. https://doi.org/10.1016/j.mhpa.2020.100357 [ Links ]
19. Wieczorek T, Kotodziejczyk A, Ciutkowicz M, Maciaszek J, Zej Misiak B, Rymaszewska J, et al. Class of 2020 in Poland: Students' mental health during the COVID-19 outbreak in an academic setting. Int J Environ Res Public Health. 2021;18(6), Art. #2884. https://doi.org/10.3390/ijerph18062884 [ Links ]
20. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr Res. 2020;287, Art. #112934. https://doi.org/10.1016/j.psychres.2020.112934 [ Links ]
21. Chaturvedi K, Vishwakarma DK, Singh N. COVID-19 and its impact on education, social life and mental health of students: A survey. Child Youth Serv Rev. 2021;121, Art. #105866. https://doi.org/10.1016/j.childyouth.2020.105866 [ Links ]
22. Martinez L, Valencia I, Trofimoff V. Subjective wellbeing and mental health during the COVID-19 pandemic: Data from three population groups in Colombia. Data Brief. 2020;32, Art. #106287. https://doi.org/10.1016/j.dib.2020.106287 [ Links ]
23. Sayeed A, Kundu S, Al Banna MH, Hasan MT, Begum MR, Khan MSI. Mental health outcomes during the COVID-19 and perceptions towards the pandemic: Findings from a cross sectional study among Bangladeshi students. Child Youth Serv Rev. 2020;119, Art. #105658. https://doi.org/10.1016/j.childyouth.2020.105658 [ Links ]
24. Cuijpers P, Auerbach RP, Benjet C, Bruffaerts R, Ebert D, Karyotaki E, et al. Introduction to the special issue: The WHO World Mental Health International College Student (WMH-ICS) initiative. Int J Methods Psychiatr Res. 2019;28(2), e1762. https://doi.org/10.1002/mpr.1762 [ Links ]
25. Kessler RC, Santiago PN, Colpe LJ, Dempsey CL, First MB, Heeringa SG, et al. Clinical reappraisal of the Composite International Diagnostic Interview Screening Scales (CIDI-SC) in the Army Study to assess risk and resilience in servicemembers (Army STARRS). Int J Methods Psychiatr Res. 2013;22(4):303-321. https://doi.org/10.1002/mpr.1398 [ Links ]
26. Kessler RC, Calabrese JR, Farley PA, Gruber MJ, Jewell MA, Katon W, et al. Composite International Diagnostic Interview screening scales for DSM-IV anxiety and mood disorders. Psychol Med. 2013;43(8):1625-1637. https://doi.org/10.1017/S0033291712002334 [ Links ]
27. First MB, Gibbon M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). In: Hilsenroth MJ, Segal DL, Hersen M, editors. Comprehensive handbook of psychological assessment. Vol. 2: Personality assessment. Hoboken, NJ: John Wiley & Sons, Inc.; 2004. p. 134-143. Available from: https://psycnet.apa.org/record/2004-12821-011 [ Links ]
28. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-suicide severity rating scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatr. 2011;168(12):1266-1277. https://doi.org/10.1176/appi.ajp.2011.10111704 [ Links ]
29. Herman AA, Stein DJ, Seedat S, Heeringa SG, Moomal H, Williams DR. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of CMDs. S Afr Med J. 2009;99(5):339-344. [ Links ]
30. Masipa T. South Africa's transition to democracy and democratic consolidation: A reflection on socio-economic challenges. J Public Aff. 2018;18(4), e1713. https://doi.org/10.1002/pa.1713 [ Links ]
31. Breetzke GD. Crime and spatiality in South African cities. In: Massey R, Gunter A, editors. Urban geography in South Africa. Cham: Springer; 2020. p. 155-172. https://doi.org/10.1007/978-3-030-25369-1_10 [ Links ]
32. Cheteni P Mah G, Yohane YK. Drug-related crime and poverty in South Africa. Cogent Econ Finance. 2018;6(1), Art. #1534528. https://doi.org/10.1080/23322039.2018.1534528 [ Links ]
33. Beyene AS, Chojenta C, Roba HS, Melka AS, Loxton D. Gender-based violence among female youths in educational institutions of sub-Saharan Africa: A systematic review and meta-analysis. Syst Rev. 2019;8(1), e59. https://doi.org/10.1186/s13643-019-0969-9 [ Links ]
34. Ukegbu P Nwofia B, Ndudiri U, Uwakwe N, Uwaegbute A. Food insecurity and associated factors among university students. Food Nutr Bull. 2019;40(2):271-281. https://doi.org/10.1177/0379572119826464 [ Links ]
35. Mthembu Z, Maharaj P Rademeyer S. "I am aware of the risks, I am not changing my behaviour": Risky sexual behaviour of university students in a high-HIV context. 2019;18(3):244-253. https://doi.org/10.2989/16085906.2019.1655075 [ Links ]
36. Evans D, Musakwa N, Nattey C, Bor J, Lonnermark E, Larshans C, et al. Knowledge, risk perception and access to healthcare services for HIV and tuberculosis among university students in Johannesburg, South Africa. S Afr J Child Health. 2018;12(Special Issue):S19-31. https://doi.org/10.7196/SAJCH.2018.v12i2b.1525 [ Links ]
37. Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, et al. Global tuberculosis report 2020 - Reflections on the global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021;113:S7-12. https://doi.org/10.1016/j.ijid.2021.02.107 [ Links ]
38. TBFacts. TB in South Africa - high burden districts & strategic plan [webpage on the Internet]. No date [cited 2022 Mar 16]. Available from: https://tbfacts.org/tb-south-africa/ [ Links ]
39. HodesR. Questioning 'Fees Must Fall.' Afr Aff(Lond).2017;116(462):140-150. https://doi.org/10.1093/afraf/adw072 [ Links ]
40. Mavunga G. #FeesMustFall protests in South Africa: A critical realist analysis of selected newspaper articles. J Stud Aff Afr. 2019;7(1):81-99. https://doi.org/10.24085/jsaa.v7i1.3694 [ Links ]
41. Shepherd N. After the #fall. 2020:565-579. https://doi.org/101080/1360481320201784579 [ Links ]
42. Xaba W. Challenging Fanon: A Black radical feminist perspective on violence and the Fees Must Fall movement. 2017;31(3-4):96-104. https://doi.org/10.1080/10130950.2017.1392786 [ Links ]
43. Ecclestone K, Hayes D. The dangerous rise of therapeutic education. London: Routledge; 2008. https://doi.org/10.4324/9780203870563 [ Links ]
44. Stein DJ, Wessely S. Mental disorders and COVID-19: Towards a precision public mental health approach. Eur Neuropsychopharmacol. 2022;58:42-43. https://doi.org/10.1016/j.euroneuro.2022.02.008 [ Links ]
 Correspondence:
Correspondence:
Jason Bantjes
Email:Jason.Bantjes@mrc.ac.za
Received: 30 Mar. 2022
Revised: 24 Oct. 2022
Accepted: 10 Nov. 2022
Published: 31 Jan. 2023
Editor: Floretta Boonzaier
Funding: South African Medical Research Council














