Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Science
versión On-line ISSN 1996-7489
versión impresa ISSN 0038-2353
S. Afr. j. sci. vol.118 no.11-12 Pretoria nov./dic. 2022
http://dx.doi.org/10.17159/sajs.2022/12047
REVIEW ARTICLE
Extreme heat events, high ambient temperatures and human morbidity and mortality in Africa: A systematic review
Albert E. ManyuchiI; Matthew ChersichII; Coleen VogelI; Caradee Y WrightIII, IV; Ruwadzano MatsikaI; Barend ErasmusV
IGlobal Change Institute, University of the Witwatersrand, Johannesburg, South Africa
IIWits Reproductive Health and HIV Institute, University of the Witwatersrand, Johannesburg, South Africa
IIIEnvironmental and Health Research Unit, South African Medical Research Council, Pretoria, South Africa
IVDepartment of Geography, Geoinformatics and Meteorology, University of Pretoria, Pretoria, South Africa
VOffice of the Dean, Faculty of Natural and Agricultural Sciences, University of Pretoria, Pretoria, South Africa
ABSTRACT
Temperature extremes vary across Africa. A continent-wide examination of the impacts of heat on health in Africa, and a synthesis of Africa-informed evidence is, however, lacking. A systematic review of articles published in peer-reviewed journals between January 1992 and April 2019 was conducted. To be eligible, articles had to be Africa-specific, in English, and focused on how heatwaves and high ambient temperatures affect morbidity and mortality. A secondary systematic analysis on policies and interventions comprising 17 studies was also conducted, and the findings synthesised together with those of the 20 primary studies. Eleven studies showed that high ambient temperatures and heat waves are linked with increased mortality rates in Africa. These linkages are characterised by complex, linear and non-linear (J or U) relationships. Eight of the nine primary studies of morbidity outcome reported that an increase in temperature was accompanied by raised disease incidence. Children and the elderly were the population groups most vulnerable to extreme heat exposure. Location-specific interventions and policy suggestions include developing early warning systems, creating heat-health plans, changing housing conditions and implementing heat-health awareness campaigns. In summary, this review demonstrates that, while heat-health relationships in Africa are complex, extreme temperatures are associated with high mortality and morbidity, especially amongst vulnerable populations. As temperatures increase across Africa, there is an urgent need to develop heat-health plans and implement interventions. Future studies must document intervention effectiveness and quantify the costs of action and inaction on extreme heat-related mortality and morbidity.
SIGNIFICANCE:
• Empirical evidence shows that the relationship between heat and human health is complex in the African context. This complexity has implications for the development of interventions and policies for heat-health on the continent.
• This review is important for African policymakers, practitioners and others who support Africa's adaptation to climate change. Through this review, a compendium of Africa-specific and relevant empirical information is aggregated and made readily available to various interested and affected parties.
Keywords: Africa, heat-health plans and policy, heat-health interventions, heatwaves, high ambient temperature
Introduction
Heatwaves and high ambient temperatures affect human health.1,2 Biological, environmental, medical, socio-behavioural and geographical factors influence how extreme heat exposure affects morbidity and mortality.3 The sub-groups most vulnerable to extreme temperatures include infants, the elderly, persons living with disabilities, persons on chronic medications, pregnant persons and outdoor workers.4-8 Extreme heat-related diseases and deaths disproportionately affect the poor.9
Studies set in Africa which provide continent-specific insights on the effects and association between extreme temperatures on health are essential for planning actions to increase resilience, as well as programmes and policies for heat-health adaptation and mitigation.10 The majority of studies on the relationship between extreme heat exposure, and morbidity and mortality have been carried out in high-income countries.11-13 There are thus major gaps in knowledge about the effects of heatwaves on health outcomes among different sub-groups in low-and middle-income countries.11,14-17 The few existing studies that address this topic in Africa largely focus on other continents and include selected African countries usually as an add-on. For example, Campbell et al.18 undertook a review of global evidence which included no studies on Africa but generalised the conclusion from other continents to Africa. Green et al.13 found few studies on Africa relative to other continents and observed that there are more studies on cities such as Brisbane and Phoenix than there are on cities in Africa.
To date, review studies examining Africa-wide effects and association between extreme heat events and high ambient temperatures on morbidity and mortality are lacking. Yet, observed climate trends show considerable increases in near surface temperatures over most parts of Africa in the past 50 to 100 years, with minimum temperatures warming rapidly relative to maximum temperatures.19 In addition, future climate projections show that temperatures in Africa will rise much faster than the global average.9
The main objectives of this article were thus to provide an Africa-wide systematic review of evidence on the effects and association between heatwaves and high ambient temperatures on morbidity and mortality, to summarise the population groups most vulnerable to extreme heat exposure, and to explore the suggested heat-health interventions and policies to protect people on the African continent.
Methods
Scope of review
We conducted a systematic review of published peer-reviewed literature on the effects of extreme heat events and high ambient temperatures on morbidity and mortality in Africa. An adapted, realist review method was used. A realist review or synthesis broadly falls under systematic reviews. It takes a systematic approach to reviewing and synthesising available evidence.20 A realist review attempts to provide answers to complex issues21 by seeking detailed explanations of the issues22. It aims to provide practice and policy relevant evidence through a determination of what works in what circumstances, and for which particular persons, and why or how it works. It includes qualitative critical analyses which provide for depth rather than breadth.23
While the general principles of systematic reviews include 'the need for clear question(s), the need for transparency of methods and the use of wide-ranging, comprehensive searches to reduce the effects of publication bias'24, a realist review encompasses tighter inclusion and exclusion criteria, and a smaller number of articles relative to other approaches25. A realist review is applicable for 'complex interventions where evidence of effect may be lacking'26.
Rather than applying all the core features of the realist review method in their entirety, here we used an adapted realist synthesis. We retained the core features of a realist review, including developing a set of guiding questions and strict inclusion and exclusion criteria as well as conducting a wide-ranging and comprehensive search to minimise bias. However, instead of responding to the question of what works, our adapted realist review mainly responds to questions of effect and association between heat and heatwaves and human health.
Our adaptation of the realist review method is in agreement with Petticrew24 who argues that systematic reviews should evolve from answering simple questions to respond to complex phenomena. We further undertook a secondary analysis of published data with less strict inclusion and exclusion criteria to examine policy and practice suggestions - something uncommon in realist synthesis. We considered the adapted realist review method most suitable to explore the complex subject of extreme heat-health relationships in data-scarce African settings.
In line with the adapted realist method, the following four background questions guided the review process: (1) What is the association between heatwaves and high ambient temperatures and morbidity and mortality in Africa? (2) What are the effects of extreme heat events and high ambient temperatures on specific population groups in Africa? (3) What are the suggested interventions to reduce morbidity and mortality from heatwaves and high ambient temperatures in Africa? Finally, (4) what are the policy propositions suggested to deal with heatwaves and high ambient temperature related morbidity and mortality? This study was approved by the Human Research Ethics Committee (Non-Medical) of the University of the Witwatersrand (protocol number H18/11/18). Although this review addresses heat exposure and human morbidity and mortality, we are not diminishing the major importance of heat impacts on morbidity and mortality in other animals and plants, which warrant equal attention.
Search strategy
Africa-focused, peer-reviewed studies published between 1 January 1992 and 30 April 2019 were reviewed. Reviewed studies focused on the effects and association between heatwaves and high ambient temperatures on morbidity and mortality in Africa. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.27 A topic search using the 'advanced search' option was performed within the Web of Knowledge, Scopus and PubMed electronic databases and applied the following phrases: Extreme heat events and mortality in Africa; Extreme heat events and morbidity in Africa; Heatwaves and mortality in Africa; Heatwaves and morbidity in Africa; High ambient temperatures and mortality in Africa; and High ambient temperatures and morbidity in Africa.
Eligibility criteria
All article titles and abstracts arising from the literature search were manually screened based on the inclusion and exclusion criteria presented in Table 1. Where the article titles and abstracts proved inadequate to determine relevance or eligibility, the full-text article was retrieved and assessed.
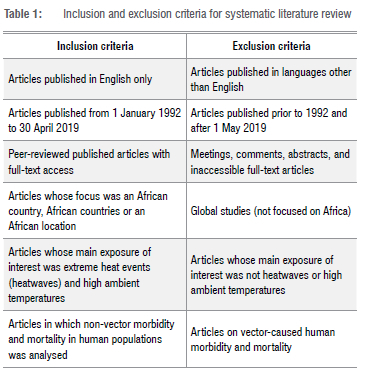
We also reviewed the reference lists of the retrieved full-text articles. From these lists, relevant references aligned to the inclusion criteria not initially identified were extracted and added. We included both qualitative and quantitative studies.
Data extraction
The first author extracted data using a standardised data collection form. The variables for data extraction included inter alia: the country or location of study; year of study; study design; study setting; study aims; study population; study outcome measures; geographical and temperature units (lags, temperature units); and results and conclusion of the study. Emphasis was placed on estimates of association (i.e. relative risk, attributable risk or percentage increase in morbidity and mortality) and effects on study population, especially sub-groups (by gender, age, cause of death, among others) obtained from tables, text descriptions and any other supplementary materials. The co-authors moderated the data extraction, resolved any differences, and provided any additional publications not located by the first author.
Synthesis of results and risk of bias
We collated extracted data and reviewed it using thematic analysis. In order to stress important points, we provide a synthesis of key results of some individual studies.
Additional secondary analyses of published data
We undertook an additional, secondary analysis encompassing global studies and Africa-specific studies that did not meet the review criteria, but where authors had suggested potential interventions and policies. For quality reasons, grey literature was excluded, and only peer-reviewed published literature was included in this additional policy-focused secondary analysis. For these studies, we outline the reported variables and summarise the interventions and policies suggested. While the studies did not meet all the study inclusion criteria, they nevertheless provided key insights (Supplementary table 1). The inclusion of the additional literature broadened the literature base from which we drew our findings. Supplementary table 1 shows the 17 reviewed articles included in the secondary analysis.
Results
Study selection and study characteristics
A flow diagram (Figure 1) shows the study selection informed by the inclusion and exclusion criteria.
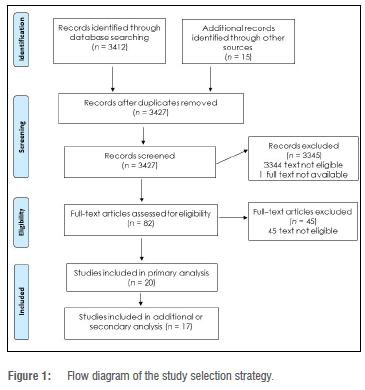
The study characteristics and findings for the 20 primary studies that were included in the review are summarised in Supplementary table 2. Based on the United Nations geoscheme classification of African sub-regions, the largest number of primary studies were set in the Southern Africa region (n=7), made up of six studies in South Africa and one in Botswana. There were six studies in Eastern Africa, with two in Kenya, two in Tanzania and one each in Mozambique and Zambia. Five studies were set in Western Africa, with two in Burkina Faso, two in Ghana and one in Senegal. Only one study in Cameroon was done in the Central (Middle) Africa region. Most studies were published between 2016 and 2019 (inclusive). The years in which data were collected in the primary studies ranged from 1974 to 2015.
Most studies (n=15) applied time-series methodology. The primary studies covered rural and urban areas of Africa and were either location specific, multi-location or nationwide. Among the primary studies, 11 adjusted for both seasonality and lag effect, 3 adjusted for seasonality but not lag effect, 4 adjusted for lag effect and not seasonality, and 2 did not report whether they adjusted for seasonality or lag effect. Several studies estimated the relative risk of association between daily mean temperature and daily mortality using lag strata.
Temperature data, including data sources
Diverse temperature measurements were used in the studies, including daily minimum and maximum temperatures, daily mean temperature, monthly mean temperature, and apparent air temperature (also called Tapp). Most studies (n=17) focused on high ambient temperature, with only three assessing extreme heat events (heatwaves). Most temperature data were gathered from in-country National Meteorological and Hydrological Services, including those affiliated to the World Meteorological Organization. The National Meteorological and Hydrological Services providing temperature data were located in the study area or in close proximity. Some studies supplemented or combined in-country temperature data with those from external sources such as the National Oceanic and Atmospheric Administration of the United States of America, South Africa's Agriculture Research Council, the Climate Research Unit of the University of East Anglia, United Kingdom, and the Royal Netherlands Meteorological Institute's Climate Explorer website.
Health outcome measures
Of the 20 primary studies, 10 focused on mortality, 9 on morbidity and 1 covered both outcomes. Studies of mortality outcomes reported on all-cause mortality, as well as disease-specific mortality such as cardiovascular mortality. Most studies with mortality as an outcome measure ascertained cause of death through verbal autopsy questionnaires. Studies of morbidity outcome examined cholera and Ebola virus outbreaks (n=3), diarrhoea (n=4), acute respiratory infections (n=1) and cardiovascular diseases (n=1), among others.
Population groups examined
Most studies examined heat effects on specific age groups. The age categories were typically 0-4 years; 5-19 years; 20-19 years; 5059 years and, 60 years and above. One study did not follow this age categorisation and its categories were from 40-64 years and then 65 years and above.28 Four studies included only children or adolescents aged <18 years.29 32
Synthesis of key findings
(1) Extreme heat exposure and morbidity and mortality in Africa
Taking all the evidence together, it is clear that the association between extreme heat exposure and mortality in Africa is complex and varies considerably across settings (Supplementary table 2). Two studies found a linear association between high ambient temperatures and mortality.33,34 Three studies found a non-linear relationship.11,35,36 Three studies found a U-shaped relationship between heat exposure and mortality.11,33,37 One reported a J-shaped temperature-mortality association for all-ages mortality and a U-shape for under-five mortality.36 Most studies reported associations between temperature and all-cause mortality, but four described heat impacts on mortality related to non-communicable diseases such as cardiovascular disease.
Eight of the nine studies on temperature-morbidity relationships showed positive associations, that is, an increase in temperature resulted in an increased incidence of the conditions assessed. For example, a study reported that incidences of diarrhoea, respiratory infection, asthma, meningitis and malaria increased with an increase in temperature.30 Six studies reported that rates of diarrhoeal diseases increased at higher temperatures, including two studies on cholera. Studies of morbidity outcome commonly pointed out that increased minimum temperature affects the prevalence of diseases in Africa. One study on heat and Ebola virus outbreaks found an association with cold, but not hot temperatures.
(2) Effects on population sub-groups
Most studies (n=11) whose outcome measure was mortality analysed the effects of extreme heat events and high ambient temperature on given population groups by age and gender (Supplementary table 2). The studies found that infants, children and young adolescents as well as the elderly (0-4 years; 5-12 years; 13-19 years and 50 years and above, respectively) were most vulnerable to deaths associated with exposure to extreme heat. In addition, higher mortality was found amongst male individuals than female individuals in one study assessing heat impacts on mortality from non-communicable diseases in Ghana.
Few studies of morbidity outcome analysed the effects of extreme heat events or high ambient temperature on population sub-groups. In one example, a study found increased incidences of diarrhoea, respiratory infections and malaria, particularly among male children compared to female children.30 Two studies observed increased ambient temperatures were linked with increased diarrhoeal incidence among children under five years.31,32 One study noted increased acute respiratory infections among children aged 18 years and younger.29
(3) Suggested interventions
Although we combined primary and secondary analysis results to elaborate the heat-health interventions focused on African localities, 21 out of the 37 studies explicitly offered Africa-appropriate suggestions, as shown in Table 2.
Table 2 shows that a few studies suggested either preventative or treatment-related interventions at individual, household and community levels.30,3238 Although most studies were location specific, most of the suggestions made were likely to be applicable to other similar localities. Several individual- and household-level preventative interventions were identified, such as increased educational campaigns aimed at raising awareness about the effects and association between extreme heat events and human health.29,30,39 Another example is seasonal forecast-based vaccination campaigns aimed at reducing hospital admissions from acute respiratory infection and reducing exposure to extreme temperature particularly among vulnerable groups such as young children and the elderly.11,29
Importantly, because there is a high mortality associated with meningitis during the dry season in the meningitis belt in Africa, the main suggestions were to redesign housing structures so that they have proper ventilation, to change sleeping arrangements as well as to reduce dust, smoke and carbon dioxide exposure.38 It is worth noting that better ventilation may not necessarily mean providing air conditioning in the African context but constructing structures with larger and well-positioned windows and doors, for example.14 In order to reduce smoke at household level, cooking stoves with better combustion properties were suggested.38
A community-level preventative measure suggested was the proper allocation of resources, especially to guarantee that vulnerable persons are protected against the effects of extreme heat. This suggestion was focused on governments as well as other persons with authority to distribute resources in Africa. In fact, reviewed studies focusing on South Africa - where there are extensive informal settlements - generally pointed out that informal settlements must be replaced, and new heat-adapted housing structures should be developed.14 The same study pointed out that traditional, round thatch huts - especially in the rural areas of Africa - should also be modified for adaptation to extreme heat events and high ambient temperatures.14
Studies focused on diarrhoea and cholera incidences suggested the importance of strengthening household and community interventions for preventing weather-induced diarrhoea and cholera diseases in Africa.32,39-41 One study pointed out the potential benefits of conditional cash transfers to deal with vulnerability related to heat exposure12, while another alluded to the use of clothing suitable to hot climates36.
Early warning system interventions were suggested several times, to ensure that the African populace is informed of impending extreme heat events before they occur.13,35,40-43 While being informed may not directly translate to action, early warning systems might enable the populations that will be affected by exposure to extreme heat to prepare in advance. This suggestion implicitly calls for the strengthening of climate information services for health on the continent. The few reviewed studies offering policy suggestions posited that better climate data are essential for better health-focused responses. Indeed, quality data from all relevant stakeholders and actors are essential for heat-health planning efforts required. Surveillance systems were suggested in several studies reviewed.39,44,45
(4) Suggested policies
Few studies proffered concrete policy suggestions useful for extreme heat-health policymaking in Africa. Only nine out of 37 studies gave some explicit policy suggestions, as shown in Table 3.
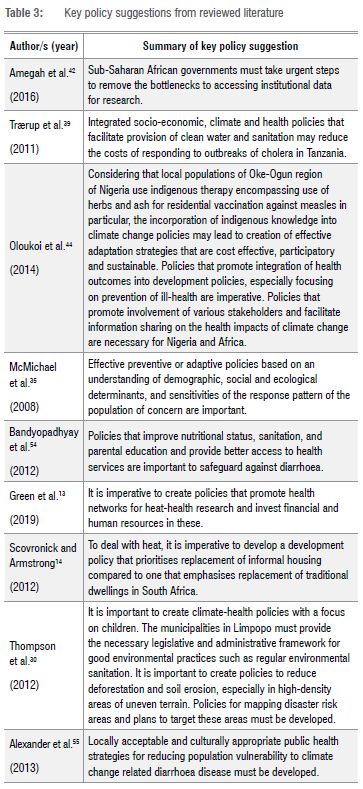
Three of these studies implicitly pointed out the importance of developing heat-health plans in Africa.14,35,44 However, not much detail was provided on the content and implementation of such plans. The cautionary advice provided was, as Africa comprises widely diverse localities, developing a 'one-size-fits-all' heat plan could be ineffective. The findings of Scott et al.46 on urban heat islands in Nairobi were informative as they emphasised location-specific factors when assessing morbidity and mortality in Africa, particularly demonstrating that studies with large spatial coverage might not accurately illuminate the range of heat-morbidity and -mortality relationships. Rather, more localised heat plans should be an imperative.
Another key suggestion is for authorities to formulate policies that target vulnerable populations that would be affected by exposure to extreme temperatures.30 Heat plans must explicitly outline the different levels and categories of vulnerability in the communities they cover.35 Therefore, data that explicitly delineate vulnerable populations are essential for crafting an effective heat plan.
Discussion
This review summarises the evidence published between January 1992 and April 2019 on the effects of extreme heat events and high ambient temperatures on mortality and morbidity in Africa. To our knowledge, this is the most up-to-date Africa-focused systematic review on this subject, notwithstanding the existence of other studies that have included African countries in reviews that cover studies across the globe.13,47 A previous review focused on countries in sub-Saharan Africa and excluded studies in North Africa42, and a more recent study included only 10 studies from Africa among many studies from other continents13.
The general pattern among studies that explored the heat-health relationship in Africa was exclusionary (limited in coverage) and
non-exhaustive (referencing the continent in passing). Our review encompassed 20 primary studies and 17 secondary studies, and importantly highlighted Africa-specific nuances on mortality and morbidity arising from extreme heat exposure. This review underscores the fact that Africa has particular climatic and population health features that demand a focused and thorough exploration.
Overall, the review confirmed the effects of extreme heat on mortality and morbidity in Africa. This finding is in line with previous related reviews in Africa and globally. For instance, a study reported the dominance of heat effects in studies conducted in sub-Saharan Africa, with heat-related mortality observed in Burkina Faso, Ghana and Kenya.47 Even though Green et al.13 included studies from other continents, they similarly point out that
the vast majority of studies found a positive association between heat and morbidity and mortality, and only nine either found no association or a negative association between the heat exposure and the health outcome of interest. (p. 84)
Not many reviews provide unequivocal, continent-wide evidence on the effects of extreme heat exposure on mortality and morbidity.
This review further points out that the association between extreme heat and mortality or morbidity is complex. Indeed, the heat-mortality and heat-morbidity relationships were found to be linear or non-linear, with the latter showing U- and J-shaped relationships. We suggest that the complexity in these relationships may result from the uneven geographic spatial distribution of climate elements and the epidemiological heterogeneity of the continent. The complex relationship found demands further research to explore other factors, including inter alia whether the methodology employed in the studies, the sub-populations investigated, and other independent variables directly or indirectly influence the relationship.
The evidence indicates that although extreme heat effects affect persons of all age groups, the African population groups most affected by exposure to extreme heat were infants (0-4 years), children (5-19 years) and the elderly (over 50 years). Similar findings have been reported in studies from South Asia where heat-mortality effects are more pronounced among children48-50, and in Latin America and China where heat-mortality effects were observed among the elderly51,52.
A few studies suggested some practical interventions and policies to deal with the effects of extreme heat events and high ambient temperatures in Africa. Many of these suggestions pertained to preventative and treatment interventions, as well as polices for early warning systems and heat-health plans. The suggested interventions and policies, however, lack depth and detail. More intervention and policy-oriented studies that focus on these study areas are needed. For studies to offer useful programme and policy suggestions, more Africa-specific intervention projects must be carried out.
There are some limitations to this review. The main limitation is that we did not evaluate the quality or potential biases of studies included in this review. Heterogeneity of included studies made it difficult to consider doing a meta-analysis for this review. The allocation of studies into those fitting primary or secondary analysis was not error-free. The general limitation of the adapted realist review method, which is that it may not be reproducible and transparent, applies to this review.26 Some key concepts with fluid definitions such as extreme heat and heatwaves were not explicitly defined, especially within the context of the continent which has predominantly warm/hot tropical and subtropical climates. In addition, the causal effects of heat impacts on health, for example, physiological or cardio-metabolic stress versus communicable diseases, were not fully explored. However, some of these concepts are complex to explain robustly without oversimplifying them and making erroneous attributions. These are areas for future studies to explore.
Conclusion
While there is a growing body of evidence suggesting that Africa will be disproportionately affected by climate change, the effects of extreme temperature changes on health on the continent have not been explored in detail to date. This systematic review established the effects and association between extreme heat and high ambient temperatures on mortality and morbidity in Africa and explored the population sub-groups most vulnerable. The evidence shows that the extreme heat-health relationship is complex and confirmed the effects of extreme temperature on mortality and morbidity, especially among children and the elderly.
African countries have a substantial mortality and disease burden. It is imperative to reduce extreme temperature related deaths and diseases. Future climate projections show increased temperatures across many countries on the continent. Therefore, policy and programmatic measures that curb future heat-health mortality and morbidities are urgently needed. Research that explores the economic costs of proactively and reactively acting on heat-health morbidities and mortalities must be carried out to inform policymakers and practitioners.
Suggested interventions and policies to deal with the effects of exposure to extreme heat in Africa were also sought in the review. Unfortunately, only a few of the reviewed studies provided detailed heat-health policy and programme suggestions. Further intervention and policy-focused research is encouraged. Large-scale, Africa-specific transdisciplinary studies that examine extreme heat-health relationships at sub-regional or continental scales are recommended.
Acknowledgements
A.E.M. received a bursary from the Global Change Institute (GCI) of the University of the Witwatersrand for this research, which was carried out as part of his PhD research. The GCI funding partners played no role in the design, execution or writing of this paper.
Competing interests
We have no competing interests to declare.
Authors' contributions
A.E.M. designed the study and performed the data extraction, and wrote the first and final drafts, taking into consideration the different sections and reviews by the co-authors. M.C. reviewed the data collection instruments, guided data collection and reviewed the first draft and updated the methodology section. C.YW., C.V. and R.M. reviewed the drafts and C.YW. and R.M. worked on all tables. B.E. helped with the analysis and review of extracted articles and reviewed the final manuscript.
References
1. Huang C, Barnett AG, Wang X, Vaneckova P Fitzgerald G, Tong S. Projecting future heat-related mortality under climate change scenarios: A systematic review. Environ Health Perspect. 2011;119(12):1681-1690. https://doi.org/10.1289/ehp.1103456 [ Links ]
2. Zeng Q, Li G, Cui Y Jiang G, Pan X. Estimating temperature-mortality exposure-response relationships and optimum ambient temperature at the multi-city level of China. Int J Environ Res Public Health. 2016;13(3):279-290. https://doi.org/10.3390/ijerph13030279 [ Links ]
3. Xu Y Dadvand P Barrera-Gómez J, Sartini C, Marí-Dell'Olmo M, Borrell C, et al. Differences on the effect of heat waves on mortality by sociodemographic and urban landscape characteristics. J Epidemiol Community Health. 2013;67(6):519-525. https://doi.org/10.1136/jech-2012-201899 [ Links ]
4. Oudin Ástròm D, Bertil F, Joacim R. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas. 2011;69(2):99-105. https://doi.org/10.1016/j.maturitas.2011.03.008 [ Links ]
5. Benmarhnia T, Deguen S, Kaufman JS, Smargiassi A, Benmarhnia T, Deguen S, et al. Vulnerability to heat-related mortality: A systematic review, metaanalysis, and meta-regression analysis. Epidemiology. 2015;26(6):781-793. https://doi.org/10.1097/EDE.0000000000000375 [ Links ]
6. Costello A, Abbas M, Allen A, Ball S, Patterson C. Managing the health effects of climate change. Lancet. 2009;373(9676):1693-1733. https://doi.org/10.1016/S0140-6736(09)60935-1 [ Links ]
7. Loughnan M, Tapper NJ, Phan T, Lynch K, McInnes J. A spatial vulnerability analysis of urban populations during extreme heat events in Australian capital cities [document on the Internet]. c2013 [cited 2021 Aug 20]. Available from: https://nccarf.edu.au/wp-content/uploads/2019/03/Loughnan_2013_Spatial_vulnerability_analysis.pdf [ Links ]
8. Yin Q, Wang J. The association between consecutive days' heat wave and cardiovascular disease mortality in Beijing, China. BMC Public Health. 2017;17(1):1-9. https://doi.org/10.1186/s12889-017-4129-7 [ Links ]
9. Hoegh-Guldberg O, Jacob D, Taylor M, Bindi M, Brown S, Camilloni I, et al. Impacts of 1.5°C global warming on natural and human systems. In: Masson-Delmotte V Zhai P Pörtner H-O, Roberts D, Skea J, Shukla PR, et al., editors. Global warming of 1.5°C. An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty. Cambridge, UK: Cambridge University Press; 2018. p. 175-312. https://doi.org/10.1017/9781009157940.005 [ Links ]
10. Fraser A, Leck H, Parnell S, Pelling M, Brown D, Lwasa S. Meeting the challenge of risk-sensitive and resilient urban development in sub-Saharan Africa: Directions for future research and practice. Int J Disaster Risk Reduct. 2017;2:106-109. https://doi.org/10.1016/j.ijdrr.2017.10.001 [ Links ]
11. Azongo DK, Awine T, Wak G, Binka FN, Oduro AR. A time series analysis of weather variability and all-cause mortality in the Kasena-Nankana districts of Northern Ghana, 1995-2010. Glob Health Action. 2012;5:14-22. https://doi.org/10.3402/gha.v5i0.19073 [ Links ]
12. Wichmann J. Heat effects of ambient apparent temperature on all-cause mortality in Cape Town, Durban and Johannesburg, South Africa: 20062010. Sci Total Environ. 2017;587-588:266-272. https://doi.org/10.1016/j.scitotenv.2017.02.135 [ Links ]
13. Green H, Bailey J, Schwarz L, Vanos J, Ebi K, Benmarhnia T. Impact of heat on mortality and morbidity in low and middle income countries: A review of the epidemiological evidence and considerations for future research. Environ Res. 2019;171:80-91. https://doi.org/10.1016/j.envres.2019.01.010 [ Links ]
14. Scovronick N, Armstrong B. The impact of housing type on temperature-related mortality in South Africa, 1996-2015. Environ Res. 2012;113:46-51. http://dx.doi.org/10.1016/j.envres.2012.01.004 [ Links ]
15. MacVicar S, Berrang-Ford L, Harper S, Huang Y Bambaiha DN, Yang S. Whether weather matters: Evidence of association between in utero meteorological exposures and foetal growth among Indigenous and non-Indigenous mothers in rural Uganda. PLoS ONE. 2017;12(6), e0179010. https://doi.org/10.1371/journal.pone.0179010 [ Links ]
16. Medina-Ramón M, Zanobetti A, Cavanagh DP Schwartz J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006;114(9):1331-1336. https://doi.org/10.1289/ehp.9074 [ Links ]
17. Michelozzi P Accetta G, De Sario M, D'Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med. 2009;179(5):383-389. https://doi.org/10.1164/rccm.200802-217OC [ Links ]
18. Campbell S, Remenyi TA, White CJ, Johnston FH. Heatwave and health impact research: A global review. Health Place. 2018;53:210-218. https://doi.org/10.1016/j.healthplace.2018.08.017 [ Links ]
19. Niang I, Ruppel OC, Abdrabo MA, Essel A, Lennard C, Padgham J, et al. Africa. In: Barros VR, Field CB, Dokken DJ, Mastrandrea MD, Mach KJ, Bilir TE, et al., editors. Climate change 2014: Impacts, adaptation, and vulnerability. Part B: Regional aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press; 2014. p. 1199-1265. https://doi.org/10.1017/CBO9781107415386.002 [ Links ]
20. Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: Meta-narrative reviews. BMC Med. 2013;11(20):1-15. https://doi.org/10.1186/1741-7015-11-20 [ Links ]
21. Greenhalgh T, Wong G, Westhorp G, Pawson R, Wong G. RAMESES publication standards: Realist syntheses. BMC Med. 2013;11(21):1-14. https://doi.org/10.1186/1741-7015-11-21 [ Links ]
22. Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review - a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1): 21-34. https://doi.org/10.1258/1355819054308530 [ Links ]
23. Thompson HE, Berrang-Ford L, Ford JD. Climate change and food security in sub-Saharan Africa: A systematic literature review. Sustainability. 2010;2(8):2719-2733. https://doi.org/10.3390/su2082719 [ Links ]
24. Petticrew M. Time to rethink the systematic review catechism? Moving from 'what works' to 'what happens'. Syst Rev. 2015;4:36. https://doi.org/10.1186/s13643-015-0027-1 [ Links ]
25. Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: Illustrating the method for implementation research. Implement Sci. 2012;7(1):1-10. https://doi.org/10.1186/1748-5908-7-33 [ Links ]
26. Petticrew M, Rehfuess E, Noyes J, Higgins JPT, Mayhew A, Pantoja T, et al. Synthesizing evidence on complex interventions: How meta-analytical, qualitative, and mixed-method approaches can contribute. J Clin Epidemiol. 2013;66(11):1230-1243. http://dx.doi.org/10.1016/j.jclinepi.2013.06.005 [ Links ]
27. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339(7716):332-336. http://dx.doi.org/doi:10.1136/bmj.b2535 [ Links ]
28. Kynast-Wolf G, PreuB M, Sié A, Kouyaté B, Becher H. Seasonal patterns of cardiovascular disease mortality of adults in Burkina Faso, West Africa. Trop Med Int Health. 2010;15(9):1082-1089. http://dx.doi.org/10.1111/j.1365-3156.2010.02586.x [ Links ]
29. Tchidjou HK, Vescio F, Boros S, Guemkam G, Minka E, Lobe M, et al. Seasonal pattern of hospitalization from acute respiratory infections in Yaoundé, Cameroon. J Trop Pediatr. 2010;56(5):317-320. https://doi.org/10.1093/tropej/fmp127 [ Links ]
30. Thompson AA, Matamale L, Kharidza SD. Impact of climate change on children's health in Limpopo province, South Africa. Int J Environ Res Public Health. 2012;9(3):831-854. https://doi.org/10.3390/ijerph9030831 [ Links ]
31. Musengimana G, Mukinda FK, Machekano R, Mahomed H. Temperature variability and occurrence of diarrhoea in children under five-years-old in Cape Town metropolitan sub-districts. Int J Environ Res Public Health. 2016;13(9):1-12. https://doi.org/10.3390/ijerph13090859 [ Links ]
32. Thiam S, Diène AN, Sy I, Winkler MS, Schindler C, Ndione JA, et al. Association between childhood diarrhoeal incidence and climatic factors in urban and rural settings in the health district of Mbour, Senegal. Int J Environ Res Public Health. 2017;14(9):1-16. https://doi.org/10.3390/ijerph14091049 [ Links ]
33. Diboulo E, Sié A, Rocklöv J, Niamba L, Yé M, Bagagnan C, et al. Weather and mortality: A 10 year retrospective analysis of the Nouna health and demographic surveillance system, Burkina Faso. Glob Health Action. 2012;5:6-13. https://doi.org/10.3402/gha.v5i0.19078 [ Links ]
34. Mrema S, Shamte A, Selemani M, Masanja H. The influence of weather on mortality in rural Tanzania: A time-series analysis 1999-2010. Glob Health Action. 2012;5:33-43. https://doi.org/10.3402/gha.v5i0.19068 [ Links ]
35. McMichael AJ, Wilkinson P, Kovats RS, Pattenden S, Hajat S, Armstrong B, et al. International study of temperature, heat and urban mortality: The 'ISOTHURM' project. Int J Epidemiol. 2008;37(5):1121-1131. https://doi.org/10.1093/ije/dyn086 [ Links ]
36. Egondi T, Kyobutungi C, Kovats S, Muindi K, Ettarh R, Rocklöv J. Time-series analysis of weather and mortality patterns in Nairobi's informal settlements. Glob Health Action. 2012;5:23-32. https://doi.org/10.3402/gha.v5i0.19065 [ Links ]
37. Scovronick N, Sera F, Acquaotta F, Garzena D, Fratianni S, Wright CY, et al. The association between ambient temperature and mortality in South Africa: A time-series analysis. Environ Res. 2018;161:229-235. https://doi.org/10.1016/j.envres.2017.11.001 [ Links ]
38. Dukic V Hayden M, Forgor AA, Hopson T, Akweongo P Hodgson A, et al. The role of weather in meningitis outbreaks in Navrongo, Ghana: A generalized additive modeling approach. J Agric Biol Environ Stat. 2012;17(3):442-460. https://doi.org/10.1007/s13253-012-0095-9 [ Links ]
39. Trœrup SLM, Ortiz RA, Markandya A. The costs of climate change: A study of cholera in Tanzania. Int J Environ Res Public Health. 2011;8(12):4386-4405. https://doi.org/10.3390/ijerph8124386 [ Links ]
40. Horn LM, Hajat A, Sheppard L, Quinn C, Colborn J, Zermoglio MF, et al. Association between precipitation and diarrheal disease in Mozambique. Int J Environ Res Public Health. 2018;15(4), Art. #709. https://doi.org/10.3390/ijerph15040709 [ Links ]
41. Reyburn R, Kim DR, Emch M, Khatib A, Von Seidlein L, Ali M. Climate variability and the outbreaks of cholera in Zanzibar, East Africa: A time series analysis. Am J Trop Med Hyg. 2011;84(6):862-869. https://doi.org/10.4269/ajtmh.2011.10-0277 [ Links ]
42. Amegah AK, Rezza G, Jaakkola JJK. Temperature-related morbidity and mortality in sub-Saharan Africa: A systematic review of the empirical evidence. Environ Int. 2016;91:133-149. https://doi.org/10.1016/j.envint.2016.02.027 [ Links ]
43. Heunis JC, Olivier J, Bourne DE. Short-term relationships between winter temperatures and cardiac disease mortality in Cape Town. S Afr Med J.1995;85(10):965-967. [ Links ]
44. Oloukoi G, Bob U, Jaggernath J. Perception and trends of associated health risks with seasonal climate variation in Oke-Ogun region, Nigeria. 2014;25:47-55. http://dx.doi.org/10.1016/j.healthplace.2013.09.009 [ Links ]
45. Ng S, Basta NE, Cowling BJ. Association between temperature, humidity and ebolavirus disease outbreaks in Africa, 1976 to 2014. Euro Surveill. 2014;19(35), Art. #20892. http://dx.doi.org/10.2807/1560-7917.es2014.19.35.20892 [ Links ]
46. Scott AA, Misiani H, Okoth J, Jordan A, Gohlke J, Ouma G, et al. Temperature and heat in informal settlements in Nairobi. PLoS ONE. 2017;12(11), e0187300. https://doi.org/10.1371/journal.pone.0187300 [ Links ]
47. Burkart K, Khan MMH, Schneider A, Breitner S, Langner M, Kramer A, et al. The effects of season and meteorology on human mortality in tropical climates: A systematic review. Trans R Soc Trop Med Hyg. 2014;108(7):393-401. https://doi.org/10.1093/trstmh/tru055 [ Links ]
48. Hashizume M, Armstrong B, Hajat S, Wagatsuma Y Faruque ASG, Hayashi T, et al. Association between climate variability and hospital visits for non-cholera diarrhoea in Bangladesh: Effects and vulnerable groups. Int J Epidemiol. 2007;36(5):1030-1037. [ Links ]
49. Lindeboom W, Alam N, Begum D, Streatfield PK. The association of meteorological factors and mortality in rural Bangladesh, 1983-2009. Glob Health Action. 2012;5:61-73. https://doi.org/10.1093/ije/dym148 [ Links ]
50. Ingole V Kovats S, Schumann B, Hajat S, Rocklöv J, Juvekar S, et al. Socioenvironmental factors associated with heat and cold-related mortality in Vadu HDSS, western India: A population-based case-crossover study. Int J Biometeorol. 2017;61(10):1797-1804. https://doi.org/10.1007/s00484-017-1363-8 [ Links ]
51. Wu W, Xiao Y Li G, Zeng W, Lin H, Rutherford S, et al. Temperature-mortality relationship in four subtropical Chinese cities: A time-series study using a distributed lag non-linear model. Sci Total Environ. 2013;449:355-362. http://dx.doi.org/10.1016/j.scitotenv.2013.01.090 [ Links ]
52. Goggins WB, Chan EY Yang C, Chong M. Associations between mortality and meteorological and pollutant variables during the cool season in two Asian cities with sub-tropical climates: Hong Kong and Taipei. Environ Health. 2013;12(1), Art. #59. https://doi.org/10.1186/1476-069X-12-59 [ Links ]
53. Grace K, Davenport F, Funk C, Lerner AM. Child malnutrition and climate in sub-Saharan Africa: An analysis of recent trends in Kenya. Appl Geogr. 2012;35(1-2):405-413. http://dx.doi.org/10.1016/j.apgeog.2012.06.017 [ Links ]
54. Bandyopadhyay S, Kanji S, Wang L. The impact of rainfall and temperature variation on diarrheal prevalence in sub-Saharan Africa. Appl Geogr. 2012;33(1):63-72. http://dx.doi.org/10.1016/j.apgeog.2011.07.017 [ Links ]
55. Alexander KA, Carzolio M, Goodin D, Vance E. Climate change is likely to worsen the public health threat of diarrheal disease in Botswana. Int J Environ Res Public Health. 2013;10(4):1202-1230. https://doi.org/10.3390/ijerph10041202 [ Links ]
56. Fernandez LMÁ, Bauernfeind A, Jiménez JD, Gil CL, El Omeiri N, Guibert DH. Influence of temperature and rainfall on the evolution of cholera epidemics in Lusaka, Zambia, 2003-2006: Analysis of a time series. Trans R Soc Trop Med Hyg. 2009;103(2):137-143. https://doi.org/10.1016/j.trstmh.2008.07.017 [ Links ]
57. Bunker A, Sewe MO, Sié A, Rocklöv J, Sauerborn R. Excess burden of non-communicable disease years of life lost from heat in rural Burkina Faso: A time series analysis of the years 2000-2010. BMJ Open. 2017;7(11), e018068. https://doi.org/10.1136/bmjopen-2017-018068 [ Links ]
58. Egondi T, Kyobutungi C, Rocklöv J. Temperature variation and heat wave and cold spell impacts on years of life lost among the urban poor population of Nairobi, Kenya. Int J Environ Res Public Health. 2015;12:2735-2748. http://dx.doi.org/10.3390/ijerph120302735 [ Links ]
 Correspondence:
Correspondence:
Albert Manyuchi
Email: albertedgar.manyuchi@gmail.com
Received: 21 Aug. 2021
Revised: 30 Aug. 2022
Accepted: 21 Sep. 2022
Published: 30 Nov. 2022
Editor: Pascal Bessong
Funding: University of the Witwatersrand














