Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Science
On-line version ISSN 1996-7489
Print version ISSN 0038-2353
S. Afr. j. sci. vol.116 n.1-2 Pretoria Jan./Feb. 2020
http://dx.doi.org/10.17159/sajs.2020/6359
REVIEW ARTICLE
Cardiac surgery publications in Africa over the last 20 years: A literature review
Yihan LinI, II, III, *; Brian M. TillII, IV, *; Sojung YiII, V; James S. DahmII, VI; Kathryn TaylorII, VII; Nguyen LuVIII; Peter ZillaIX; Ralph M. BolmanIII
IDepartment of Surgery, University of Colorado, Denver, Colorado, USA
IIProgram in Global Surgery and Social Change, Harvard Medical School, Boston, Massachusetts, USA
IIIDivision of Cardiothoracic Surgery, University of Colorado, Denver, Colorado, USA
IVCollege of Medicine, University of Vermont, Burlington, Vermont, USA
VGeorge Washington School of Medicine, Washington, Washington DC, USA
VISchool of Medicine and Public Health, University of Wisconsin, Madison, Wisconsin, USA
VIIHarvard Medical School, Boston, Massachusetts, USA
VIIISchool of Medicine, University of Colorado, Denver, Colorado, USA
IXChris Barnard Division of Cardiothoracic Surgery, University of Cape Town, Cape Town, South Africa
ABSTRACT
There is a significant burden of surgically correctable cardiovascular disease in Africa. The goal of this research was to review the last 20 years of literature on this topic. A systematic search was performed using PubMed, Embase and African Index Medicus for the period 1996-2016. Publications came from 29 countries, all of different income brackets. Research output increased by 15-fold over the 20-year time period, with the majority of publications authored by local teams (71.4%) compared to visiting (4.9%) and mixed teams (23.7%). Although increasing, clinical reporting on cardiac surgery is still limited. Increased publication of results should be encouraged to better benchmark capacity and improve research capacity.
SIGNIFICANCE:
•The majority of the cardiovascular publications came from local research teams affiliated with public hospitals which suggests strong local engagement in research and cardiovascular care.
•Research output significantly increased and the share of literature from major research contributors has relatively shrunk over the study period, which suggests emerging research capacities from previously underrepresented regions.
•A demographic analysis of publications showed that studies were set in countries from all income brackets, with the majority of the studies originating from low-income countries.
•There is a need to standardise reporting of surgical outcomes which is dependent on perioperative care and maintenance of high-quality health records.
•Over half of the publications lacked evidence of outpatient follow-up or data on postoperative care, which highlights the need to focus on patient outcomes as a metric
Keywords: cardiac research, collaboration, mortality, cardiovascular, cardiothoracic surgery
Background
There is a significant and growing burden of cardiac disease, and this is especially true on the African continent. Surgically amenable congenital heart disease is believed to account for 63 302 disability-adjusted life years in sub-Saharan Africa and an additional 1 692 728 in North Africa and the Middle East1 - two of the largest shares of this burden found in the world. Nonetheless, there is only one paediatric cardiac surgeon per 38 000 000 persons on the continent, compared to one per 3 500 000 persons in Europe and North America.2 Valvular heart disease also represents a significant share of the total burden of disease.3 Estimates of the prevalence of clinically significant valvular dysfunction among children in Africa range from 7.5 to 51.6 per 1000 population, with significant variation based on region.4,5 In terms of structural heart disease, endomyocardial fibrosis - the most common restrictive cardiomyopathy in the world - remains understudied, and may correspond to 7% of paediatric heart failure in Uganda.6 The prevalence of endomyocardial fibrosis remains as high as 19.8% in rural Mozambique, and carries with it a life expectancy of 2 years once patients become symptomatic.7,8
These pathologies are increasingly joined by cardiac diseases typically associated with high-income countries.9 Rapid urbanisation, dietary changes and smoking have increased the prevalence of obesity, diabetes and hypertension. Cardiovascular disease now accounts for 1 million deaths per year in sub-Saharan Africa alone.10 In Tunisia, coronary artery disease mortality increased significantly between 1997 and 2009 (70-87 deaths per 100 000 for men, 28-41 deaths per 100 000 for women)11, and a 2009 autopsy study in Kenya found cardiovascular disease to be the cause of death in 13% of patients.12 Nigeria has a coronary artery disease prevalence of 16 per 1000, with those affected being predominantly male and urban-dwelling individuals.13
Despite this growing burden of cardiovascular disease, cardiovascular surgery needs are not being met. Cardiac surgery needs have been estimated to be 200 operations per million in low-income countries and >1000 operations in high-income countries non-endemic to rheumatic heart disease. However, cardiac surgery is provided at a rate of only 0.5 operations per million in low- and lower-middle-income countries and 500 operations per million in high-income countries.14 Additionally, the quantity, quality, location and scope of cardiac surgical research emerging from Africa remains poorly defined. A 2015 systematic review of all surgical literature from low-income countries found that 62% of publications were case reports or case series, 43% lacked clinical outcome measures, 21% of articles were written with collaboration between authors of high-income countries (HIC) and lower- and middle-income countries (LMIC), and 55% were written exclusively by local authors. HIC and LIC were defined by the guidelines set by the World Bank.15 Only 3% of the papers included data about cardiac surgery.16 A bibliometric study of the Journal of Cardiothoracic and Vascular Anesthesia found that the total number of publications from Africa has remained unchanged from 1990 to 2011 (average 0.9 per year)17 - a period in which the share of high-income contributions shrank and contributions from LMIC in other regions expanded.
There is also a paucity of literature surrounding the type and extent of engagement between HIC cardiac surgery programmes and African institutions. As of 2012, Sliwa and Zilla18 reported fully independent programmes in only five African countries: South Africa, Egypt, Sudan, Kenya and Namibia. A recent study of non-governmental organisations involved in surgical care found 77 groups provide cardiac surgical care19, while a recent survey by the World Society for Pediatric and Congenital Heart Surgery found 80 non-governmental groups involved in such work, with 18% of groups working in Africa. Of these, 13% of groups reported being involved in exclusively educational and diagnostic partnerships, and 87% reported educational components to their work. This survey also showed that 26% of respondents reported that LMIC partners do not perform operations between HIC partner visits.20
The goals of the present review are to describe the demographics of those producing literature on cardiac surgery in Africa over the previous 20 years, to describe the degree of collaboration between HIC and LMIC actors, and to analyse whether the origin, type and quality of this research have evolved over the study period.
Patients and methods
Search strategy
We conducted a systematic search of literature related to cardiac surgery in Africa published from 1996 to 2016. PubMed, Embase and African Index Medicus databases were searched using cardiac surgery MeSH and Emtree terms, relevant anatomic and procedural terms, and geographical terms related to Africa. Geographical terms included regional terms as well as individual country names and derivatives. Our full search terms are included in Appendix 1 of the supplementary material.
Study selection
Articles identified by our search were compiled in an Endnote X7 library and duplicates were removed. Remaining titles and abstracts were screened in duplicate by four members of the research team (JSD, BMT, KT, SY). Articles pertaining exclusively to percutaneous, vascular or thoracic procedures were excluded from our study. Non-English language studies and those published before 1996 were excluded. In cases of ambiguity surrounding type of procedure or location, the full-text of the article was reviewed. Further uncertainty was resolved by a senior member of the research team (YL).
Data abstraction
After title and abstract screening, full-text articles were acquired via EndNote full-text search, Harvard Countway Library full-text article search, Google search, or interlibrary loan. A data abstraction tool was developed using Microsoft Excel. Data abstraction categories included: study identification (author names, dates, country and institutional affiliations), study design, patient population, indication for surgery, type of surgery, mortality data, major and minor morbidities as defined by the American College of Surgeons National Surgical Quality Improvement Program, and health-related quality of life (HRQL) measures, such as: New York Heart Association Heart Failure classifications, return to work status, measures of economic strain/medical impoverishment, and indications of difficulty managing anticoagulation due to cost or logistics.
To ensure quality and consistency, the abstraction tool was amended by consensus after each data abstractor (JD, BT, KT, SY) had reviewed 10 articles. A senior member of the research team (YL) reviewed a random 25% sample of each abstractor's data at two intervals during the abstraction process, and disagreements were reconciled.
Results
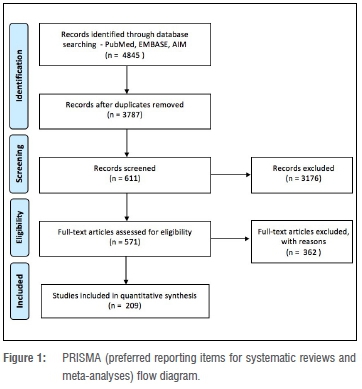
The initial search returned 2122 articles from PubMed, 2723 from Embase and 39 from African Index Medicus (Figure 1). Of the literature retrieved, 209 full-text articles and abstracts met the study inclusion criteria (Appendix 2).
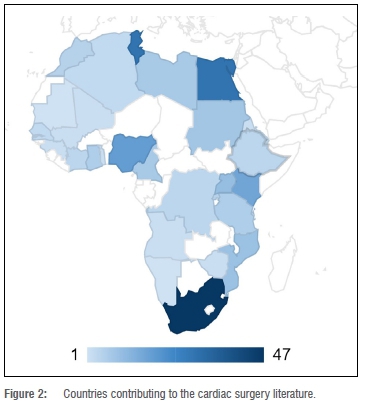
Study setting
Studies were set in 29 of 54 African countries, of which 13 were low-income (44.8%), 11 were lower-middle-income (37.9%), and 5 were upper-middle-income (17.2%). The majority of articles published were set in just four countries: South Africa (19.8%), Tunisia (12.2%), Egypt (12.2%) and Kenya (6.8%), all of which are middle-income status (Figure 2).
Surgical care
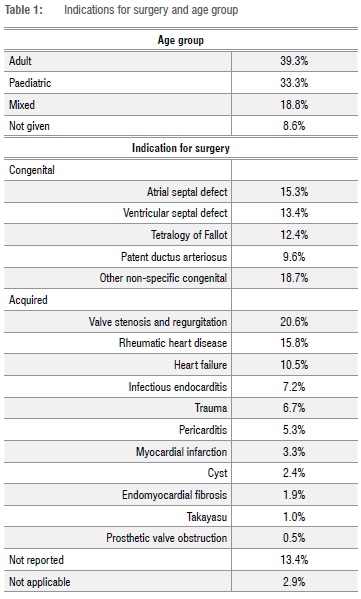
Indications for surgeries were reported in 83.7% of all studies. Of these, congenital indications included: atrial septal defect (15.3%), ventral septal defect (13.4%), patent ductus arteriosus (9.6%), Tetralogy of Fallot (12.4%), and other non-specific congenital aetiologies (18.7%) (Table 1). The most common indications for acquired conditions included: unspecified valvular stenosis and regurgitation (20.6%), rheumatic heart disease (15.8%) and heart failure (10.5%). Other reported conditions were infectious endocarditis (7.2%), trauma (6.7%), pericarditis (5.3%), myocardial infarction (3.3%), cysts (2.4%), endomyocardial fibrosis (1.9%), Takayasu's disease (1.0%) and prosthetic valve obstruction (0.5%). The surgeries performed for these indications were described for adult patients (39.3%), paediatric patients (33.3%) or both (18.8%), or not given (8.6%).
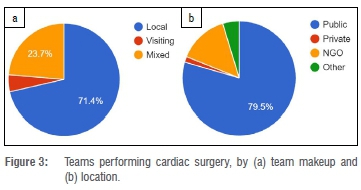
Who and where
The majority of cardiac surgeries included in these studies were performed by local teams (71.4%), compared to visiting teams (4.9%) and mixed teams (23.7%). Authors were predominantly associated with academic institutions (73.2%). Public hospitals were the most common site of practice (79.5%), compared to non-governmental organisations (14.2%), private (1.6%) and other (4.7%) (Figure 3).
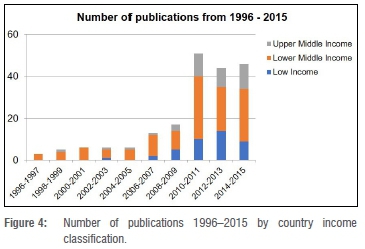
Research capacity
First authors were affiliated with institutions in a total of 34 countries, of which 69.9% were African. South Africa (19.1%), Tunisia (12.4%), Egypt (12.4%) and Nigeria (7.2%) represented the most common African affiliations, while the USA (6.7%) was the most common affiliation outside of Africa. Over the last 10 years, the overall volume of research has increased substantially. When looking at years with full data, we find that total output increased more than 15-fold between the first 2 years and the last 2 years of the sample (1996-1997 and 2014-2015). Research produced by the four major contributors to the literature (South Africa, Egypt, Tunisia and Kenya) continued to grow during this period, but its share of total research output dropped (66.6% to 51.1%) (Figure 4).
Study design
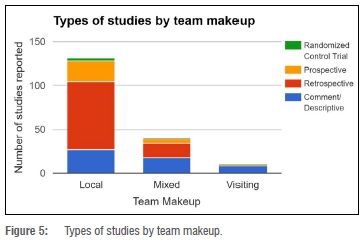
Almost half (48.7%) of the studies were retrospective in design. Case reports, comments and descriptive studies represented 35.7% of publications. Only 14.1% were prospective studies, with interventional and observational design split evenly. Finally, three studies (1.5%) were randomised control trials. The share of lower quality evidence produced (case reports, comments and descriptive studies) was notably higher in the first decade of our sample (46.7%) compared to the last 10 years (29.4%).
Local teams produced randomised control trials (2.3%), compared to none in mixed teams or visiting teams (Figure 5). Local teams were more likely to produce prospective studies (59.5%), compared to mixed teams (41.0%) (p=0.32) and visiting teams (11.1%) (p<0.01). Mixed teams and visiting teams were more likely to publish case reports or comments (46.2% and 88.9%) compared to local teams (20.6%) (p<0.01) (Figure 5).
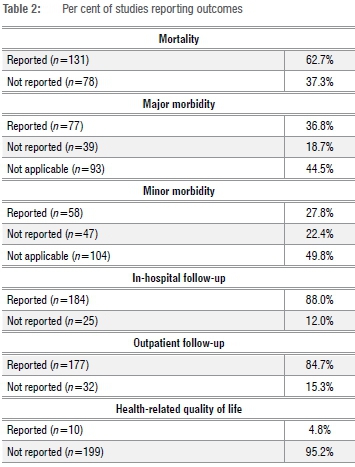
Outcomes
Fewer than half of the studies reported inpatient postoperative care data (45.9%) or evidence of outpatient follow-up (40.7%). Mortality outcomes were reported in 62.7% of publications (Table 2). Morbidity was reported in 45.5% of the studies, although the type of detail provided varied greatly. Major morbidities were reported in 36.8% of studies, of which reoperation for any reason (55.8%), permanent stroke (11.7%) and renal failure (11.7%) were most commonly reported. Minor morbidities were reported in 27.8% of studies. The most commonly reported minor morbidities were prolonged length of stay (36%), surgical site infections (32.8%) and wound dehiscence (10.4%). Health-related quality of life measures were reported in 4.8% of studies.
Discussion
Our results show that 29 out of 54 (52.7%) African countries contributed to the cardiac surgical literature in our study period. The majority of this work was from African surgeons affiliated with public hospitals. This suggests a strong local engagement in cardiac surgical care and research. Overall, output increased substantially over our study period, and the share of literature produced by the largest contributors has shrunk in relative terms, suggesting emerging capacity in other states in the region. There was a notable increase in research productivity in our sample from 2009 to 2010. There are several possible reasons for this increase in production. One possible driving factor is the Fogarty Institute's Medical Education Partnership Initiative (MEPI) grants, which totalled USD130 million and was awarded to institutions in 12 African countries and US partner medical schools during this period.21 While MEPI is credited with generating rich collaborations between US and African institutions, and between African institutions that previously were not in collaboration with one another22,23, the effect of these collaborations on research output remains poorly studied.
In addition to the contributions of MEPI, there has been a growing interest and investment in international initiatives on reducing cardiovascular disease and increasing surgical capacities in LMIC between LMIC and HIC. This emphasis on international collaborations is especially important for fostering the development of research capacity in Africa. In recent years, there has been a call to develop cardiac care and research in low- and middle-income countries. The Cape Town Declaration aimed to accomplish this through policy advocacy and international initiatives and collaborations.24 This focus on international initiatives was put into practice by the World Heart Federation Emerging Leader and the National Institute of Health Fogarty Wits Non-communicable Disease Research Leadership Training Programmes. These two global initiatives have been at the forefront of supporting and training leaders in research and policy change in Africa. Over the past decade, the two programmes have trained master's, doctoral and postdoctoral talents who have engaged in research that examined the social, genetic, epigenetic, clinical and physical factors that contribute to cardiovascular disease.25
In terms of developing surgical capacities in LMIC, interests in global surgery have increased in faculty and surgical trainees in HIC. Global surgery provides opportunities for mutually beneficial relationships between HIC and LMIC. Surgeons in HIC will be able to access the clinical workload in LMIC to develop surgical and clinical skills, research region-specific diseases, and explore their passion for global health. For LMIC partners, the interest in global surgery has led many Western organisations to assist LMIC in developing their surgical capacities by helping establish new surgical residencies and providing research training.26 The growing interest and investment in cardiovascular disease and global surgery creates an important opportunity to build bilateral partnerships between HIC and LMIC. The financial support of MEPI and the symmetric exchange of knowledge and experience seen between HIC and LMIC are important catalysts that have likely facilitated the increased research production seen in this study. Therefore, promoting and supporting mutually beneficial, respectful and longitudinal relationships and collaborations is imperative in expanding the research capacity and growth of health care in both HIC and LMIC.
Research of overall higher quality evidence, such as prospective studies and randomised control trials, was more likely to be produced by local authors. On the other hand, research by visiting surgeons and collaborations between visiting and local teams was most likely to yield comments, case reports and descriptive studies. This raises important questions about the extent to which collaborations between HIC and LMIC surgeons are effectively leveraging the research experience and resources of high-income partners, and why the exceptional level of connectivity afforded in the world today is not permitting more long-term, long-distance, collaborative research.
One answer to this question may be the barriers in sustaining these collaborations longitudinally for surgeons in HIC. A survey performed by the Society of University Surgeons and the Association for Academic Surgery showed as few as 30% of academic medical centres in the USA held international partnerships and 70% of these partnerships were unfunded or relied on variable funding; 41% of the programmes reported a lack of allowance for time off to engage in international work.27 Even though there has been a rise in global surgery engagement, there is currently inadequate infrastructure in place to support these longitudinal partnerships in the USA. Policy changes in academic medical centres in HIC that allow for time away and funding to engage in international partnerships can promote desired long-term, long-distance, collaborative research between HIC and LMIC.
In only half of the studies, surgical outcomes were reported, highlighting the need to improve the overall quality of the literature being produced. The reporting of outcomes needs further standardisation, with increased emphasis on the value of measuring morbidities and HRQL outcomes. It is notable that the reporting of such data is often contingent upon adequate perioperative care and the maintenance of high-quality health records.
Engagement with the academic medical literature plays an invaluable role in elevating the quality of care that can be delivered, and meaningful contributions to literature can inform broader priority setting both at national and international levels. The ability to participate in the community of academic surgery can bolster the perspectives of LMIC surgeons, and lead to significant opportunities for further collaboration and career and institutional advancement.
Inadequate research capacity was identified by the Lancet Commission as an obstacle to improving surgical programmes in LMICs.28 In south sub-Saharan Africa, most countries allocated less than 1% of their gross domestic product to their health budget and less than 0.5% of this health budget was spent on health research.29 Growing and investing in the research capacity of African LMICs can reduce inequities in research partnerships30 and expand the applications of research findings to strengthen local programmes and policies31.
For the last 20 years, there has been an ongoing debate in the literature about how to best tackle inequity in cardiac surgical care and the role that HIC institutions have in levelling this disparity.32-34 The rise of medical tourism has complicated the dynamic, and within the literature, there is debate about the role high-income surgeons and institutions can and should play evaluating LMIC cardiac programmes.35 Our study reveals considerable and ongoing collaboration in the context of surgical research. It also highlights the need to ensure that these efforts be refocused, such that these partnerships begin producing the highest quality of evidence possible. Restructuring these collaborations around larger, prospective and randomised trials can bolster LMIC institutions in important ways: first, partnering with HIC institutions for such research can enhance funding opportunities; and, second, it can lead to the transfer of knowledge and best practices that might not otherwise be transferred in strictly clinical engagement.
There are several limitations to this study. Most importantly, published literature is not wholly representative of surgical care delivery. There are likely institutions performing cardiac surgery that do not contribute to the peer-reviewed literature, and our results should not be interpreted as depicting the entirety of care available in the region. For example, in South Africa, just 7 of 48 centres offering cardiac surgical care are academic in nature. While these seven centres serve some nearly 90% of the population, they serve only 20% of cardiac cases each year and are the only institutions contributing to our data. Thus, generalising operative volume or scope by working solely from the assembled literature would lead to a distorted portrait of ongoing cardiac care. This bias is perhaps most evident in the context of surgical indication. If interpreted as a representative sample, our data would suggest that rheumatic heart disease, even when coupled with valve stenosis and regurgitation, accounts for just 36.4% of cases. Those currently practising in Africa are likely to recognise this figure as a significant underrepresentation. Secondly, there is a great deal of heterogeneity in the type and quality of data reported in this literature, complicating the analysis of mortality, morbidity and HRQL measures. The diversity of the reported data emphasises the need for improved standardisation of reporting practices in the region.
Despite the discrepancy of published literature and true service delivery, research output is still one of the final indicators of cardiac surgical services and the role of academia. This review is an important first step toward understanding the scope of cardiac surgery currently practised in the region, and the type and quality of research surrounding this care. While these results provide an initial glance, the picture that emerges is still incomplete. It is imperative that the global surgery and cardiac surgery communities continue efforts to understand ways to best approach ironing out the profound inequity in access to care and research capacity.
Authors' contributions
Y.L. and R.M.B. were responsible for project management, design of methodology, conceptualisation, curation of data, analysis and interpretation of data, production of the initial draft, revisions, supervision of students, dissemination of results, and validation of work. B.M.T., S.Y., J.S.D., and K.T. contributed to curation of data, analysis and interpretation of data, and revision of the manuscript. N.L. and P.Z. supported data analysis and interpretation, and revision of the manuscript. All authors reviewed drafts of the manuscript and approved the final version for publication.
References
1.Higashi H, Barendregt JJ, Kassebaum NJ, Weiser TG, Bickler SW, Vos T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: Cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child. 2015;100(3):233-238. https://doi.org/10.1136/archdischild-2014-306175 [ Links ]
2.Bernier PL, Stefanescu A, Samoukovic G, Tchervenkov CI. The challenge of congenital heart disease worldwide: Epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2010;13(1):26-34. https://doi.org/10.1053/j.pcsu.2010.02.005 [ Links ]
3.Carapetis JR, Steer AC, Mulholland KE, Weber M. The global burden of Group A streptococcal diseases. Lancet Infect Dis. 2005;5(11):685-694. https://doi.org/10.1016/S1473-3099(05)70267-X [ Links ]
4.Zuhlke LJ, Steer AC. Estimates of the global burden of rheumatic heart disease. Glob Heart. 2013;8(3):189-195. https://doi.org/10.1016/j.gheart.2013.08.008 [ Links ]
5.Zühlke LJ, Beaton A, Engel ME, Hugo-Hamman CT, Karthikeyan G, Katzenellenbogen JM, et al. Group A streptococcus, acute rheumatic fever and rheumatic heart disease: Epidemiology and clinical considerations. Curr Treatment Options Cardio Med. 2017;19(2), Art. #15, 23 pages. https://doi.org/10.1007/s11936-017-0513-y [ Links ]
6.Ellis J, Martin R, Wilde P, Tometzki A, Senkungu J, Nansera D. Echocardiographic, chest X-ray and electrocardiogram findings in children presenting with heart failure to a Ugandan paediatric ward. Trop Doct. 2007;37(3):149-150. https://doi.org/10.1258/004947507781524665 [ Links ]
7.Mocumbi A, Ferreira M, Sidi D, Yacoub MH. A population study of endomyocardial fibrosis in a rural area of Mozambique. New Engl J Med. 2008;359(1):43-49. https://doi.org/10.1056/NEJMoa0708629 [ Links ]
8.Mocumbi AO, Falase AO. Recent advances in the epidemiology, diagnosis and treatment of endomyocardial fibrosis in Africa. Heart. 2013;99(20):1481-1487. https://doi.org/10.1136/heartjnl-2012-303193 [ Links ]
9.Sliwa K, Acquah L, Gersh BJ, Mocumbi AO. Impact of socioeconomic status, ethnicity, and urbanization on risk factor profiles of cardiovascular disease in Africa. Circulation. 2016;133(12):1199-1208. https://doi.org/10.1161/CIRCULATIONAHA.114.008730 [ Links ]
10.Keates AK, Mocumbi AO, Ntsekhe M, Sliwa K, Stewart S. Cardiovascular disease in Africa: Epidemiological profile and challenges. Nat Rev Cardiol. 2017;14(5):273-293. https://doi.org/10.1038/nrcardio.2017.19 [ Links ]
11.Saidi O, Ben Mansour N, O'Flaherty M, Capewell S, Critchley JA, Ben Romdhane H. Analyzing recent coronary heart disease mortality trends in Tunisia between 1997 and 2009. PLoS One. 2013;8(5), e63202, 10 pages. https://doi.org/10.1371/journal.pone.0063202 [ Links ]
12.Ogeng'o JA, Gatonga P, Olabu BO. Cardiovascular causes of death in an East African country: An autopsy study. Cardiol J. 2011;18(1):67-72. [ Links ]
13.Essien OE, Andy J, Ansa V, Otu AA, Udoh A. Coronary artery disease and the profile of cardiovascular risk factors in South South Nigeria: A clinical and autopsy study. Cardiol Res Pract. 2014;2014, Art. #804751, 7 pages. https://doi.org/10.1155/2014/804751 [ Links ]
14.Zilla P, Bolman R, Yacoub M, Beyersdorf F, Sliwa K, Zühlke L, et al. The Cape Town Declaration on Access to Cardiac Surgery in the Developing World. Asian Cardiovasc Thoracic Ann. 2018;26(7):535-539. https://doi.org/10.1177/0218492318791359 [ Links ]
15.The World Bank. World Bank Country and Lending Groups [webpage on the Internet]. c2018 [cited 2018 Dec 13]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [ Links ]
16.Pauyo T, Debas HT, Kyamanywa P, Kushner AL, Pankaj GJ, Lavy C, et al. Systematic review of surgical literature from resource-limited countries: Developing strategies for success. World J Surg. 2015;39(9):2173-2181. https://doi.org/10.1007/s00268-015-3102-9 [ Links ]
17.Pagel PS, Hudetz JA. A bibliometric analysis of geographic publication variations in the journal of cardiothoracic and vascular anesthesia from 1990 to 2011. J Cardiothorac Vasc Anesth. 2013;27(2):208-212. https://doi.org/10.1053/j.jvca.2012.08.022 [ Links ]
18.Sliwa K, Zilla P. Rheumatic heart disease: The tip of the iceberg. Circulation. 2012;125(25):3060-3062. https://doi.org/10.1161/CIRCULATIONAHA.112.114199 [ Links ]
19.Ng-Kamstra JS, Riesel JN, Arya S rad Weston, Tino Kreutzer, John G. Meara, . Surgical non-governmental organizations: Global surgery's unknown nonprofit sector. World J Surg. 2016;40(8):1823-1841. https://doi.org/10.1007/s00268-016-3486-1 [ Links ]
20.Nguyen N, Jacobs JP, Dearani JA, Weinstein S, Novick WM, Jacobs ML. Survey of nongovernmental organizations providing pediatric cardiovascular care in low- and middle-income countries. World J Pediatr Congenit Heart Surg. 2014;5(2):248-255. https://doi.org/10.1177/2150135113514458 [ Links ]
21.Glass RI, Razak M, Said M. The importance of research in the MEPI Program: Perspectives from the National Institutes of Health. Acad Med. 2014;89(8):S9-S10. https://doi.org/10.1097/ACM.0000000000000351 [ Links ]
22.Olapade-Olaopa E, Baird S, Kiguli-Malwadde E, Kolars JC. Growing partnerships: Leveraging the power of collaboration through the medical education partnership initiative. Acad Med. 2014;89(8): S19-S23. https://doi.org/10.1097/ACM.0000000000000345 [ Links ]
23.Omaswa F, Kiguli-Malwadde E, Donkor P, Hakim J, Derbew M, Baird S, et al. Medical education partnership initiative gives birth to AFREhealth. Lancet Glob Health. 2017;5(10):Pe965-e966. https://doi.org/10.1016/S2214-109X(17)30329-7 [ Links ]
24.Zilla P, Yacoub M, Zühlke L, Beyersdorf F, Sliwa K, Khubulava G, et al. Global unmet needs in cardiac surgery. Glob Heart. 2018;13(4):293-303. https://doi.org/10.1177/0218492318791359 [ Links ]
25.Dzudie A, Sliwa K. Addressing the shortage of research capacity in cardiovascular disease in Africa via leadership training. Heart Asia. 2017;9(1):96-98. http://dx.doi.org/10.1136/heartasia-2016-010834 [ Links ]
26.Krishnaswami S, Stephens C, Yang G, Nwomeh B, Swaroop M, Nadler E, et al. An academic career in global surgery: A position paper from the Society of University Surgeons Committee on Academic Global Surgery. Surgery. 2018;163(4):954-960. https://doi.org/10.1016/j.surg.2009.02.015 [ Links ]
27.Krishnaswami S, Perkins S, Frost M, Nwomeh B, Simeone D, Nadler E, et al. International surgical efforts within U.S academic institutions: Results of a survey by the AAS/SUS Joint Committee on International Academic Surgery. J Surg Res. 2010;158(2):180. https://doi.org/10.1016/j.jss.2009.11.041 [ Links ]
28.Meara J, Leather A, Hagander L, Alkire B, Alonso N, Ameh E, et al. Global surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-624. https://doi.org/10.1016/S0140-6736(15)60160-X [ Links ]
29.Ramsay R. African health researchers unite. Lancet. 2002;360:1665-1666. https://doi.org/10.1016/S0140-6736(02)11654-0 [ Links ]
30.Shuchman M, Wondimagegn D, Pain C, Alem A. Partnering with local scientists should be mandatory. Nat Med. 2014;20(1):12. https://doi.org/10.1038/nm0114-12 [ Links ]
31.Ezeh A, Izugbara C, Kabiru C, Fonn S, Kahn K, Manderson L, et al. Building capacity for public and population health research in Africa: The consortium for advanced research training in Africa (CARTA) model. Glob Health Action. 2010;3(1), Art. #5693, 7 pages. https://doi.org/10.3402/gha.v3i0.5693 [ Links ]
32.Cox JL. Presidential address: Changing boundaries. J Thorac Cardiovasc Surg. 2001;122(3):413-418. https://doi.org/10.1067/mtc.2001.118489 [ Links ]
33.Dearani JA, Jacobs JP, Bolman RM III, Swain JD, Vricella LA, Weinstein S, et al. Humanitarian outreach in cardiothoracic surgery: From setup to sustainability. Ann Thorac Surg. 2016;102(3):1004-1011. https://doi.org/10.1016/j.athoracsur.2016.03.062 [ Links ]
34.Nguyen N, Leon-Wyss J, Iyer KS, Pezzella AT. Paediatric cardiac surgery in low-income and middle-income countries: A continuing challenge. Arch Dis Child. 2015;100(12):1156-1159. https://doi.org/10.1136/archdischild-2015-308173 [ Links ]
35.Jacobs JP, Horowitz MD, Mavroudis C, Siegel A, Sade RM. Surgical tourism: The role of cardiothoracic surgery societies in evaluating international surgery centers. Ann Thorac Surg. 2013;96(1):8-14. https://doi.org/10.1016/j.athoracsur.2013.02.058 [ Links ]
 Correspondence:
Correspondence:
Yihan Lin
yihan.lin@ucdenver.edu
Received: 12 June 2019
Revised: 10 Oct. 2019
Accepted: 28 Oct. 2019
Published: 29 Jan. 2020
Editor: Pascal Bessong
Funding: None
* joint first authorship
Supplementary Material
The supplementary file is available in pdf: [Supplementary file]














