Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Science
On-line version ISSN 1996-7489
Print version ISSN 0038-2353
S. Afr. j. sci. vol.114 n.9-10 Pretoria Sep./Oct. 2018
http://dx.doi.org/10.17159/sajs.2018/4451
RESEARCH ARTICLE
Alcohol and other drug use among women seeking substance abuse treatment in the Western Cape, South Africa
Siphokazi DadaI; Nadine Harker BurnhamsI, II; Ria LaubscherIII; Charles ParryI, IV; Bronwyn MyersI, V
IAlcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Cape Town, South Africa
IISchool of Public Health, University of Cape Town, Cape Town, South Africa
IIIBiostatistics Unit, South African Medical Research Council, Cape Town, South Africa
IVDepartment of Psychiatry, Stellenbosch University, Cape Town, South Africa
VDepartment of Psychiatry and Mental Health, University of Cape Town, Cape Town, South Africa
ABSTRACT
Despite a high prevalence of alcohol and other drug use (AOD) in South Africa, little is known about AOD use among women, including those in treatment centres, and changes in use over time. This knowledge is important for the development of gender-sensitive interventions for the prevention and treatment of AOD problems. We aimed to describe changes in patterns of AOD use among women who accessed specialist AOD treatment centres in the Western Cape Province of South Africa. Data were collected from 51 specialist AOD treatment centres participating in the South African Community Epidemiology Network on Drug Use between 2000 and 2013. A total of 74 368 treatment episodes were recorded for the period, of which 22% involved women. The proportion of women seeking treatment increased from 4% to 11% over time. The most common primary substance of abuse among this sample was alcohol, followed by methamphetamine. Multinomial logistic regression analyses showed that young coloured (mixed race) women were almost 18 times more likely than other women to report methamphetamine as their primary substance of abuse (RRR=17.80; 95% CI=13.18-24.04). More than a quarter of women reported poly-substance abuse. Women treated for heroin were significantly more likely to be white and younger than 25 years old (RRR=1.62; 95% CI=1.19-2.21). These data portray an increasing use of AOD treatment services by women; particularly for alcohol and methamphetamine use disorders. Additional investigations into the service needs of women utilising AOD treatment is warranted.
Significance:
• The study provides the prevalence of AOD use disorders among women in substance abuse treatment facilities in the Western Cape.
• The study reflects treatment admissions for poly-substance abuse and severe AOD problems among these women.
• The findings highlight the importance of women-specific treatment programmes to encourage utilisation of substance abuse treatment services.
Keywords: female; alcohol and other drug treatment; poly-substance abuse; readmissions; barriers
Background
Since its transition to democracy in 1994, South Africa has experienced a dramatic increase in the use of a variety of different substances of abuse.1 According to the South African Stress and Health Survey, a large population-based mental health survey conducted in 2002-2003, the lifetime prevalence of alcohol and other drug (AOD) use disorders among South African adults was as high as 13.3%, with past year prevalence of AOD use disorders being 5.8%.2 Among these 12-month prevalent cases, approximately 30.9% had a severe AOD use disorder,2 with this condition being more likely among male than female individuals. Over the last decade, several studies point to lifetime use of alcohol or drugs being higher among men than women.3 For example, the 2003/2004 South African Demographic and Health Survey reported prevalence rates for alcohol use of 70.3% for men and 39.2% for women over the age of 15.3 However, findings on the prevalence of binge drinking among men relative to women suggest that, among current drinkers, problem-drinking rates are higher among women relative to men. For example, the Survey reported that rates for binge drinking on weekends were higher among women (25%) than men (23%).3 Similarly, a community-based study on access to treatment reported more daily use of alcohol among women than among men.4 Drinking may be more common among men, but these findings suggest that women drinkers have more problematic patterns of use relative to men.
While alcohol is still the most commonly used substance in South Africa, other substances such as cannabis and methamphetamine are widely used among women.5,6 A study conducted by Myers4 found that levels of methamphetamine use among men and women were very similar. In fact, 28% of female substance users reported daily use of methamphetamine compared to 22% of their male counterparts.4 Wechsberg et al.7 also reported very high levels of methamphetamine use among female substance users participating in an HIV-risk reduction intervention study. While these studies, like others, have mostly found that prevalence rates are consistently higher among men than women3,8, the data suggest a narrowing of this gender gap in many countries9,10, particularly among young women. Research conducted in treatment centres has also shown that for certain substances of abuse, such as over-the-counter and prescription medicines, the demand for treatment is greater for female users.11 Despite overall lower prevalence rates when compared to men, AOD use is important to address among women as women have shorter trajectories to developing AOD use disorders than men.12 Women with AOD problems are also more likely to experience health problems such as liver disease13, osteoporosis14, fertility problems and breast cancer15 than women without these problems. Additionally, women who use AODs problematically are also less likely to practise safe sex consistently with their partners7 and may trade sex in exchange for AODs, placing them at risk for acquiring HIV and other sexually transmitted infections7,16. Research has suggested that women who use AODs are also more vulnerable to intimate partner violence and exposure to other forms of violence than the general population.17,18
Although AOD use is an important health concern for women, there has been limited South African research on this topic, including on those women who seek and access addiction treatment centres. The last few years have seen advances in local studies investigating AOD use among women in South Africa7,19; however, much of the available information on prevalence has come from once-off, cross-sectional, and intervention research studies, often conducted in specific locations. As a result, AOD use trends among women have been hard to identify. Given the harmful effects of problem AOD use for women, accurate data on patterns of AOD use among women are necessary to help guide the formation and implementation of effective substance abuse policies and interventions targeting women. Through this paper, we hope to address this gap by describing trends in the nature and extent of AOD use among women who used specialist AOD treatment centres in the Western Cape between 2000 and 2013.
Methods
The South African Community Epidemiology Network on Drug Use (SACENDU) is a network of researchers, practitioners and policymakers from six sentinel sites in South Africa who meet bi-annually to provide community-level public health surveillance information about substance use related trends, including for the Western Cape. All AOD treatment centres are requested to join the network and participation within the network is voluntary. Data were collected from 51 AOD treatment sites in the Western Cape, which participate in SACENDU, representing 80% of the available treatment sites in the province. In order to be admitted to a specialist AOD treatment centre, patients are required to meet diagnostic criteria for an AOD use disorder. A standardised one-page data collection form was completed for each patient enrolled in a participating treatment centre during a 6-month period; the form consisted of 22 forced-choice questions.
Data collection form
The data collection form contains questions about socio-demographic characteristics; referral sources; type of treatment received (inpatient or outpatient); primary and secondary substances of use (mode and frequency of use); prior treatment experiences; non-medical use of codeine-containing products; non-communicable disease diagnosis; tobacco use; HIV testing in the past 12 months, as well as service payment. Typically, the case manager completes the form a few days after the patient has been enrolled into the programme. Treatment centres are able to complete an electronic or paper form. To ensure data quality, completed forms are checked for possible miscodes and missing information before data analysis. Ethical approval for this study was provided by Stellenbosch University's Health Research Ethics Committee (N10/08/253).
Analysis
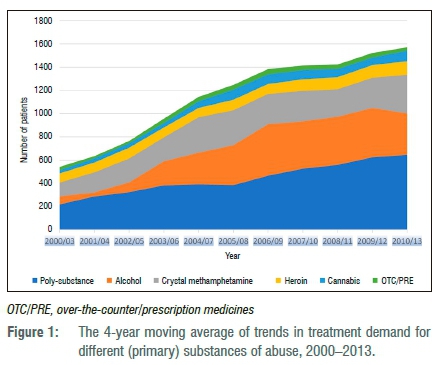
Cochran-Armitage trend tests were used to determine significant changes in female admissions to treatment between 2000 and 2013 (Figure 1). For the trend analysis, alcohol was used as a reference category. Descriptive analyses were used to describe demographic data. Chi-squared tests were performed to assess the strength of associations between participant demographic characteristics (race, marital status, education level, age category, employment status) and types of substance use (all drugs, alcohol, methamphetamine, heroin, cannabis, over-the-counter or prescription medicines and poly-substance use) of women admitted to specialist treatment centres (Table 1). A multinomial logistic regression was performed to examine the type of substance use of women with different demographic characteristics and treatment history (inpatient versus outpatient, and previous treatment). The Asian race category was excluded from this analysis because of the low number of Asians admitted to treatment centres. The variable 'type of treatment received' was used as an outcome, with 'alcohol' as the reference category. Results are presented as relative risk ratios (RRR) with 95% confidence intervals (Table 2). All statistical analyses were conducted using Stata 1320 and SAS Version 9.421; p<0.05 was indicative of statistical significance.
Results
Demographic profile and differences in patterns of substance use
From January 2000 to December 2013, 74 368 forms were collected, of which 16 656 (22.4%) were for female patients. Table 1 presents the demographic characteristics of the sample. In this data collection period, the age of female patients ranged between 10 and 85 years, with the mean age being 29.5 years (s.d.=11.80). The majority (63.3%) of patients were coloured, followed by white patients (28.3%) and black African patients (6.3%). In relation to employment status, 54.8% of women reported that they were unemployed at the time of admission, and 24.9% reported full-time employment. Of the 16 656 female patients, 71.6% had completed high school (Grade 12), with a further 13.5% patients having had tertiary education. Of the female patients enrolled during this period, 50.5% were admitted as outpatients and were referred for treatment mostly by family or friends (22.4%) or sought treatment themselves (22.8%). A total of 26% of female patients reported having received previous treatment for an AOD problem. The majority (59.1%) of patients had never been married.
Changes in substance abuse treatment admission trends for women
The number of women admitted to AOD treatment centres increased significantly between 2000 and 2013 (Figure 1). There was a gradual increase in the proportion of admissions for alcohol-related problems from 2000 (34.1%) to 2009 (37.3%), although the proportion of alcohol-related admissions decreased and remained stable from 2011. Methamphetamine admissions saw a rapid growth from 20.4% of admissions in 2000 to 34.2% of admissions in 2004, with a significant decline in 2008 (22.2%; z=12.25; p=0.001), plateauing in the last 3 years. Over time, the proportion of heroin-related admissions increased significantly, from 4.8% in 2000 to 5.6% in 2013 (z=11.52; p<0.001). Trend analysis showed a significant increase in the proportion of cannabis admissions from less than 1.9% of admissions in 2000 to 8.3% in 2013 (z=5.17; p=0.001). Data suggest a significant increase in the proportion of women reporting poly-substance abuse (use of more than one substance), from 26.6% of admissions in 2000 to 42.3% of admissions in 2013 (z=-8.30; p<0.001).
Differences in types of substance use
Multinomial logistic regression analyses revealed similarities and differences in the types of substance use among female patients of different demographic characteristics (Table 2). When compared to black African patients, coloured (RRR=3.62; 95% CI=2.05-4.31) and white (RRR=3.43; 95% CI=2.83-4.16) patients were three times more likely to be admitted for poly-substance abuse than for alcohol-related problems.
Patients between the ages of 26 and 35 and those 36 years of age and older were significantly more likely to have alcohol as their primary substance of abuse (RRR=0.33; 95% CI=0.26-0.42 and RRR=0.15; 95% CI=0.12-0.20, respectively) when compared with their younger counterparts, and therefore less likely to be admitted for poly-substance abuse. Women abusing poly-substances were also more likely to be unemployed than employed (RRR=1.89; 95% CI = 1.70-2.10; Table 2) and were more likely to have had a previous treatment episode (RRR=1.36; 95% CI=1.22-1.50) than women abusing alcohol.
In relation to methamphetamine use, coloured women were nearly 18 times more likely to have methamphetamine as their primary substance of abuse (RRR=17.80; 95% CI=13.18-24.04), followed by white patients (RRR=5.24; 95% CI=3.75-7.33). Compared to patients admitted for alcohol problems, those with methamphetamine problems were twice as likely to be unemployed (RRR=2.43; 95% CI=2.10-2.81). They were also more likely to have secondary or tertiary education than those admitted for alcohol-related problems (Table 2). Those admitted with methamphetamine as their primary substance of abuse were less likely to have received inpatient treatment relative to alcohol abuse patients (RRR=0.48; 95% CI=0.42-0.55).
Women admitted for heroin treatment were significantly more likely to be white (RRR=33.37; 95% CI=18.84-59.10) when compared to patients admitted for alcohol abuse; heroin abuse patients were more likely to be between the ages of 19 and 25 or younger (RRR=1.62; 95% CI=1.19-2.21) than their alcohol using counterparts. Patients admitted for heroin abuse were four times more likely to be unemployed compared to patients admitted for alcohol abuse (RRR=4.54; 95% CI=3.70-5.59). Heroin abuse patients were also three times more likely to have a tertiary education when compared to alcohol abuse patients. Patients admitted for cannabis use were predominantly younger than 19 years of age. They were significantly less likely to be in the 19-25 years (RRR=0.38; 95% CI=0.27-0.52); 26-35 years (RRR=0.11; 95% CI=0.07-0.15) or older than 36 years of age categories (RRR=0.04; 95% CI=0.03-0.06). Furthermore, they were four times more likely to be learners (RRR=4.31; 95% CI=2.97-6.25) than persons with alcohol as their primary substance of abuse.
Patients admitted with over-the-counter and prescription medications as their primary substance of abuse, were eight times more likely to be white (RRR=8.77; 95% CI=4.02-19.11) and have a tertiary education (RRR=3.40; 95% CI=2.10-5.51), when compared to patients admitted for alcohol-related problems. These patients were also less likely to have had a previous treatment admission (RRR=0.41; 95% CI=0.30-0.55).
Discussion
Our study is among the first to explore AOD trends among women in treatment for an AOD use disorder in the Western Cape. Our findings suggest that while fewer women relative to men access specialist substance abuse treatment facilities, over time there has been a gradual increase in the proportion of women utilising these services in the Western Cape. This finding is encouraging as prior studies have documented that women with substance use disorders experience many barriers to accessing treatment, including stigma, geographical, financial, childcare and other barriers.22-24 Additionally, it is also thought that available treatment services are not always appropriate for the unique needs of women who use substances.25 This gradual increase in women's use of treatment services is likely as a result of multiple factors, including increasing rates of substance use among women in Western Cape communities, efforts to help women overcome barriers to initiating substance abuse treatment,23,26 and efforts to expand the availability of services for women, including the introduction of several women-specific treatment programmes.
While our findings suggest that women seek treatment for both alcohol- and drug-related problems, it is evident that alcohol is the most common substance of abuse among women who access treatment. Findings indicate that the proportion of female admissions where alcohol was the primary substance of abuse increased significantly over the last decade. An increase in the utilisation of AOD treatment services by people with alcohol-related problems could be attributed to alcohol-related awareness campaigns run in primary health clinics and within communities that may have increased women's awareness of when alcohol use is problematic and how to access services. Additionally, it is also not unlikely that liquor industry action, such as improved marketing initiatives, has increased women's use of alcohol which may have led to greater need for and use of AOD treatment services by women. Despite the increased utilisation of treatment services by women with alcohol problems, more needs to be done to expand access to alcohol treatment for women. One option for expanding access to care would be to identify women with problematic patterns of alcohol use in community and health settings through screening, further providing women at risk for alcohol-related problems with brief interventions to increase their motivation to engage with treatment before referring them to care. Apart from programmes that seek to identify women who may benefit from treatment and link them to care, it is also imperative that treatment services consider whether their programmes are adequately meeting the needs of their female patients, particularly given that only a quarter of the treatment population are female.
Findings also point to more women accessing treatment for methamphetamine and heroin-related problems in the Western Cape. A third of the sample reported methamphetamine as their primary substance of abuse. These patients were slightly younger than patients receiving treatment for alcohol problems. This finding is not surprising as the time from first use to treatment for people with methamphetamine problems is generally shorter than that for people using other drugs. Methamphetamine abusers cannot as easily avoid seeking help from specialist treatment centres as persons who abuse alcohol, as methamphetamine is associated with major physical harm, cardiovascular complications and disability in mental health functioning, leading to psychoses, anxiety disorders and suicidal ideation.27,28 Since 2004, the Western Cape in particular has seen a surge in methamphetamine admissions to specialist treatment centres. Issues like gangsterism and organised crime, increased marketing, availability and low price have been associated with high levels of methamphetamine use in this region.29,30 This surge in use remains a concern, particularly as people abusing this drug are significantly more likely to report severe health, family and financial problems compared to people who abuse other drugs.28,30,31 For instance, women with methamphetamine use disorders have more symptoms of poor mental health relative to women who use other drugs23 and women who use methamphetamine are more likely to have been victims of sexual abuse and intimate partner violence.17,18 If the numerous physical and mental health needs of women who use methamphetamine are not addressed within the context of AOD treatment, it is unlikely that women will view these services as appropriate, acceptable or effective. Given findings from prior research25,32, these negative beliefs about the appropriateness and effectiveness of treatment may hamper women's use of AOD treatment services23.
Admissions for heroin abuse among women were lower than for some of the other substances but have gradually increased over the 13-year period. Similar to findings from other studies33, women using heroin were on average younger and white. Given the high number of heroin re-admissions when compared to other substances of abuse, and multiple harms associated with heroin use (both to the individual and broader society), some consideration should be given to whether the current available treatment regimens for heroin problems are effective. Furthermore, harm-reduction interventions such as medically assisted treatment should be made available for heroin users in long-term treatment facilities, including public healthcare facilities.
Poly-substance abuse in this study was also common among patients. Our findings suggest that women who use multiple substances had more occupational problems and more severe AOD problems, as reflected in their multiple treatment episodes. This is in line with studies from other contexts, which suggest that the use of multiple illegal substances increases the likelihood of the emergence of severe psychological problems, and impacts on a plethora of social concerns both directly and indirectly.
In addition, poly-substance use has been found to lead to intentional and unintentional injuries, death and disability as well as multiple health problems including but not limited to cardiovascular disease, diabetes and the acquisition of infectious diseases such as tuberculosis and HIV.34 Given these associations, women who are admitted to treatment with poly-substance abuse problems should be carefully screened for co-occurring health and mental health difficulties and provided with access to relevant preventative and curative health services.
Our findings also show that over half of the patients reporting cannabis use as their primary substance of abuse were younger than 18 years and were students or learners. The high prevalence of cannabis-related problems among young people mirrors similar findings from South African studies of drug use among high school students.35,36 As early cannabis use has implications for healthy brain development from childhood to young adulthood37, and could lead to poor academic functioning and school dropout, evidence-based interventions aimed at delaying and preventing the initiation of cannabis use among young women are urgently needed.
Over time, fewer women were admitted for poly-substance abuse, methamphetamine and heroin-related problems relative to alcohol use problems. One of the reasons for this finding is the stigma associated with illicit drug use by women, which is often linked to risky sexual behaviour such as trading sex in exchange for drugs and inconsistent condom use with their partners.7,32 Therefore, when women seek treatment, they may be more likely to report alcohol abuse compared to other drugs in fear of this perceived judgemental attitude by treatment providers.
There are several limitations to this study. First, data were only collected from specialist substance abuse treatment centres and are unlikely to represent the magnitude of AOD use disorders among women in the Western Cape. Given the limited availability of services and limited use of treatment services by women,26 the number of patients recorded in this study is likely to be a significant underestimate of the actual number of women with AOD problems. In addition, data collected from these specialist treatment centres are limited to those centres that provide the data consistently. We were not able to control for double counting across centres within particular time periods and this may have slightly inflated the number of patients receiving treatment and may have biased the data towards those patients who seek AOD treatment across more than one treatment centre. Future epidemiological studies should consider adopting a more multifaceted approach to assessing the prevalence and trends in the extent of AOD use disorders among women over time, including using other more direct measures such as general household surveys as well as indirect estimation techniques.
In conclusion, our study shows that there has been a relative increase in the use of AOD treatment by women in the Western Cape over time, particularly for poly-substance and methamphetamine use disorders. Further research is needed to better understand whether treatment programmes largely designed for, and utilised mainly by, men (who typically comprise about 80% of persons in treatment) are appropriate for the increasing number of women who access these services and are perceived to be helpful for addressing women's service needs.
Acknowledgements
We wish to acknowledge the National Department of Health (Mental Health & Substance Abuse Directorate) for its longstanding financial support of SACENDU, and staff from participating treatment centres for their continued support in providing data. The research reported in this publication was also supported by the South African Medical Research Council, which supported the salaries of all the authors.
Authors' contributions
S.D. was the lead author. S.D., N.H.B., B.M. and C.P. all contributed conceptually. S.D. collected data. N.H.B. and R.L. performed analysis. All authors contributed towards the final write-up.
References
1. Parry CDH, Pithey AL. Risk behaviour and HIV among drug using population in South Africa. Afr J Drug Alcohol Stud. 2006;5:139-156. [ Links ]
2. Herman AA, Stein DJ, Seedat S, Heeringa SG, Moomal H, Williams DR. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. S Afr Med J. 2009;99(5 Pt 2):339-344. [ Links ]
3. South African Department of Health, Medical Research Council, OrcMacro. South Africa Demographic and Health Survey 2003. Pretoria: Department of Health; 2007. [ Links ]
4. Myers B. Access to substance abuse treatment for historically underserved communities in the Cape Town Metropole. Cape Town: Medical Research Council; 2007. [ Links ]
5. Dada S, Burnhams N, Erasmus J, Parry C, Bhana A, Timol F, et al. Monitoring alcohol and drug abuse treatment admissions in South Africa: July-December 2015 (Phase 39). Cape Town: Medical Research Council; 2016. [ Links ]
6. Van Heerden MS, Grimsrud AT, Seedat S, Myer L, Williams DR, Stein DJ. Patterns of substance use in South Africa: Results from the South African Stress and Health study. S Afr Med J. 2009;99(5 Pt 2):358-366. [ Links ]
7. Wechsberg WM, Luseno WK, Karg RS, Young S, Rodman N, Myers B, et al. Alcohol, cannabis, and methamphetamine use and other risk behaviours among Black and Coloured South African women: A small randomized trial in the Western Cape. Int J Drug Policy. 2008;19(2):130-139. https://doi.org/10.1016/j.drugpo.2007.11.018 [ Links ]
8. Stein DJ, Seedat S, Herman A, Moomal H, Heeringa SG, Kessler RC, et al. Lifetime prevalence of psychiatric disorders in South Africa. Br J Psychiatry. 2008;92:112-117. https://doi.org/10.1192/bjp.bp.106.029280 [ Links ]
9. Wagner FA, Anthony JC. Male-female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug Alcohol Depend. 2007;86(2-3):191-198. https://doi.org/10.1016/j.drugalcdep.2006.06.003 [ Links ]
10. Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G. Gender and alcohol consumption: Patterns from the multinational GENACIS project. Addiction. 2009;104(9):1487-500. https://doi.org/10.1111/j.1360-0443.2009.02696.x [ Links ]
11. Myers B, Siegfried N, Parry CD. Over-the-counter and prescription medicine misuse in Cape Town - Findings from specialist treatment centres. S Afr Med J. 2003;93(5):367-370. [ Links ]
12. Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010;33(2):339-355. https://doi.org/10.1016/j.psc.2010.01.004 [ Links ]
13. Myers B, Vythilingum, B. Substance use and abuse in South Africa: Women and alcohol. In: Ellis G, Stein D, Meintjies E, Thomas K, editors. Substance use and abuse in South Africa: Insights from brain and behavioural sciences. Cape Town: UCT Press; 2012. p. 71-86. [ Links ]
14. Sampson HW. Alcohol and other factors affecting osteoporosis risk in women. Alcohol Res Health. 2002;26(4):292-298. [ Links ]
15. Schneider M, Norman R, Parry C, Bradshaw D, Pluddemann A, Group SACRAC. Estimating the burden of disease attributable to alcohol use in South Africa in 2000. S Afr Med J. 2007;97(8 Pt 2):664-672. [ Links ]
16. Parry CD, Dewing S, Petersen P, Carney T, Needle R, Kroeger K, et al. Rapid assessment of HIV risk behavior in drug using sex workers in three cities in South Africa. AIDS Behav. 2009;13(5):849-859. https://doi.org/10.1007/s10461-008-9367-3 [ Links ]
17. Gass JD, Stein DJ, Williams DR, Seedat S. Gender differences in risk for intimate partner violence among South African adults. J Interpers Violence. 2011;26(14):2764-2789. https://doi.org/10.1177/0886260510390960 [ Links ]
18. Wechsberg WM, Myers B, Reed E, Carney T, Emanuel AN, Browne FA. Substance use, gender inequity, violence and sexual risk among couples in Cape Town. Cult Health Sex. 2013;15(10):1221-1236. https://doi.org/10.1080/13691058.2013.815366 [ Links ]
19. Wechsberg WM, Myers B, Kline TL, Carney T, Browne FA, Novak SP. The relationship of alcohol and other drug use typologies to sex risk behaviors among vulnerable women in Cape Town, South Africa. J AIDS Clin Res. 2012;S1, Art. #15, 8 pages. https://doi.org/10.4172/2155-6113.S1-015 [ Links ]
20. StataCorp. Stata statistical software: Release 13. College Station, TX: StataCorp; 2013. [ Links ]
21. SAS Institute Inc. SAS 9.4 software. Cary, NC: SAS Institute Inc; 2013. [ Links ]
22. Myers B, Louw J, Pasche SE. Gendered barriers to substance abuse treatment utilization among disadvantaged communities in Cape Town, South Africa. Afr J Psychiatry. 2011;14:146-153. https://doi.org/10.4314/ajpsy.v14i2.7 [ Links ]
23. Myers B, Kline TL, Doherty IA, Carney T, Wechsberg WM. Perceived need for substance use treatment among young women from disadvantaged communities in Cape Town, South Africa. BMC Psychiatry. 2014;14, Art. #100, 10 pages. https://doi.org/10.1186/1471-244X-14-100 [ Links ]
24. World Health Organization. Global status report on alcohol and health 2014. Geneva: WHO; 2014. [ Links ]
25. Reed E, Emanuael AN, Myers B, Johnson K, Wechsberg W. The relevance of social contexts and social action in reducing substance use and victimization among women participating in an HIV prevention intervention in Cape Town, South Africa. Subst Abuse Rehabil. 2013;4:55-64. [ Links ]
26. Myers BCT, Wechsberg WM. 'Not on the agenda': A qualitative study of influences on health services use among poor young women who use drugs in Cape Town, South Africa. Int J Drug Policy. 2016;30:52-58. https://doi.org/10.1016/j.drugpo.2015.12.019 [ Links ]
27. Darke S, Kaye S, McKetin R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008;27(3):253-262. https://doi.org/10.1080/09595230801923702 [ Links ]
28. Meade CS, Towe SL, Watt MH, Lion RR, Myers B, Skinner D, et al. Addiction and treatment experiences among active methamphetamine users recruited from a township community in Cape Town, South Africa: A mixed-methods study. Drug Alcohol Depend. 2015;152:79-86. https://doi.org/10.1016/j.drugalcdep.2015.04.016 [ Links ]
29. Hobkirk AL, Watt MH, Myers B, Skinner D, Meade CS. A qualitative study of methamphetamine initiation in Cape Town, South Africa. Int J Drug Policy. 2016;30:99-106. https://doi.org/10.1016/j.drugpo.2015.10.006 [ Links ]
30. Kimani SM, Watt MH, Merli MG, Skinner D, Myers B, Pieterse D, et al. Respondent driven sampling is an effective method for engaging methamphetamine users in HIV prevention research in South Africa. Drug Alcohol Depend. 2014;143:134-140. https://doi.org/10.1016/j.drugalcdep.2014.07.018 [ Links ]
31. Watt MH, Myers B, Towe SL, Meade CS. The mental health experiences and needs of methamphetamine users in Cape Town: A mixed methods study. S Afr Med J. 2015;105(8):685-688. https://doi.org/10.7196/SAMJnew.7910 [ Links ]
32. Myers B, Fakier N, Louw J. Stigma, treatment beliefs, and substance abuse treatment use in historically disadvantaged communities. Afr J Psychiatry. 2009;12(3):218-222. https://doi.org/10.4314/ajpsy.v12i3.48497 [ Links ]
33. Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821-826. https://doi.org/10.1001/jamapsychiatry.2014.366 [ Links ]
34. Harker Burnhams N, Laubscher R, Howell S, Shaw M, Erasmus J, Townsend L. Using respondent-driven sampling (RDS) to recruit illegal poly-substance users in Cape Town, South Africa: Implications and future directions. Subst Abuse Treat Prev Policy. 2016;11, Art. #31, 12 pages. https://doi.org/10.1186/s13011-016-0074-1 [ Links ]
35. Morojele N, Myers B, Townsend L, Lombard C, Plüddemann A, Carney T, at el. Survey on substance use, risk behaviour and mental health among Grade 8-10 learners in Western Cape Provincial Schools, 2011. Cape Town: South African Medical Research Council; 2013. [ Links ]
36. Reddy SP, James S, Sewpaul R, Sifunda S, Ellahebokus A, Kambaran NS, at el. Umthente Uhlaba Usamila - The 3rd South African National Youth Risk Behaviour Survey 2011. Cape Town: South African Medical Research Council; 2013. [ Links ]
37. Jacobus J, Tapert SF. Effects of cannabis on the adolescent brain. Curr Pharm Des. 2014;20(13):2186-2193. https://doi.org/10.2174/13816128113199990426 [ Links ]
 Correspondence:
Correspondence:
Siphokazi Dada
Email: sdada@mrc.ac.za
Received: 17 May 2017
Revised: 16 Jan. 2018
Accepted: 16 May 2018
Published: 11 Sep. 2018
FUNDING: South African Department of Health; South African Medical Research Council














