Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Science
versión On-line ISSN 1996-7489
versión impresa ISSN 0038-2353
S. Afr. j. sci. vol.112 no.7-8 Pretoria 2016
http://dx.doi.org/10.17159/sajs.2016/20150470
RESEARCH ARTICLE
Osteogenic tumour in Australopithecus sediba: Earliest hominin evidence for neoplastic disease
Patrick S. Randolph-QuinneyI, II, *; Scott A. WilliamsII, III; Maryna SteynI; Marc R. MeyerIV; Jacqueline S. SmilgII, V, VI; Steven E. ChurchillII, VII; Edward J. OdesI, II; Tanya AugustineI; Paul TafforeauVIII; Lee R. BergerII, IX
ISchool of Anatomical Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIEvolutionary Studies Institute, School of Geosciences, University of the Witwatersrand, Johannesburg, South Africa
IIICenter for the Study of Human Origins, Department of Anthropology, New York University, New York, New York, USA
IVDepartment of Anthropology, School of Social & Behavioral Sciences, Chaffey College, Rancho Cucamonga, California, USA
VSchool of Radiation Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIDepartment of Radiology, Charlotte Maxeke Academic Hospital, Johannesburg, South Africa
VIIDepartment of Evolutionary Anthropology, Duke University, Durham, North Carolina, USA
VIIIEuropean Synchrotron Radiation Facility, Grenoble, France
IXDST/NRF South African Centre of Excellence in Palaeosciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
We describe the earliest evidence for neoplastic disease in the hominin lineage. This is reported from the type specimen of the extinct hominin Australopithecus sediba from Malapa, South Africa, dated to 1.98 million years ago. The affected individual was male and developmentally equivalent to a human child of 12 to 13 years of age. A penetrating lytic lesion affected the sixth thoracic vertebra. The lesion was macroscopically evaluated and internally imaged through phase-contrast X-ray synchrotron microtomography. A comprehensive differential diagnosis was undertaken based on gross- and micro-morphology of the lesion, leading to a probable diagnosis of osteoid osteoma. These neoplasms are solitary, benign, osteoid and bone-forming tumours, formed from well-vascularised connective tissue within which there is active production of osteoid and woven bone. Tumours of any kind are rare in archaeological populations, and are all but unknown in the hominin record, highlighting the importance of this discovery. The presence of this disease at Malapa predates the earliest evidence of malignant neoplasia in the hominin fossil record by perhaps 200 000 years.
Keywords: Malapa; palaeopathology; neoplasia; taphonomy; osteoma; malignant
Introduction
A neoplasm ('new-growth' or tumour) is defined as a mass of localised tissue growth, the cellular proliferation of which is no longer subject to the effects of normal growth-regulating mechanisms.1-3A neoplasm may be benign or malignant. Malignant tumours are often referred to colloquially as cancer, although the term 'malignant neoplasia' is more clinically appropriate.1 In the developed world, death from malignancy is second only to cardiovascular disease and is often perceived as a disease of modernity.4Neoplastic disease would have been prevalent in the past (e.g. Odes et al.5), but most likely occurred at much lower levels of incidence than today, given the shorter life expectancy for victims1,6,7 and the differing environmental context. Both these factors strongly influence the incidence and prognosis of any cancer.3,8 The preserved signatures of neoplasms of any kind are rare in archaeological populations, and are all but unknown in the hominin record. Here we present the earliest fossil evidence for neoplastic disease in the human lineage, with a detailed description and diagnosis of a tumorous lesion affecting the spine of a juvenile male Australopithecus sediba, Malapa Hominin 1 (MH1).9,10 This species has been postulated as a possible ancestor of the genus Homo.9The clinical and evolutionary implications of the diagnosed condition are discussed.
The Malapa hominin site
The Malapa site is one of several hominin-bearing Plio-Pleistocene cave deposits located within the Cradle of Humankind World Heritage Site to the northwest of Johannesburg, South Africa. The region includes sites such as Sterkfontein11, Swartkrans12, Kromdraai13, Gladysvale14 and Rising Star15. The fossil deposits in these caves were formed in roughly similar fashion as debris cone accumulations deposited beneath vertical cave openings, which formed phreatically within the dolomites of the Malmani Subgroup.15,16 At Malapa, the main hominin-bearing deposits have been dated using uranium-lead dating of flowstones, combined with palaeomagnetic and stratigraphic analyses of flowstones and underlying sediments, to 1.977 ± 0.002 million years ago (Ma).17 The cave deposits comprise five sedimentary facies, termed A to E, from stratigraphically lowest to highest.
Facies A and B occur below a central flowstone sheet, and are overlain by an erosion remnant (facies C), which in turn is overlain by the main hominin-bearing breccia, facies D. This has yielded well-preserved macro- and micro-mammal fossils (such as carnivores, equids and bovids18), including the fossilised remains of at least six hominins. Two of these, MH1 and MH2, have been reported in the literature as representatives of a new hominin species, Australopithecus sediba9. Taphonomically the site has been interpreted as a complex cave system with open deep vertical shafts that operated as death traps for animals on the surface of the landscape. This death-trap scenario might have been the process by which the Malapa hominins entered the cave system17,18, as evidenced by peri-mortem damage on the skeletons of MH1 and MH2, consistent with a fatal fall19. Furthermore, both skeletons present partial anatomical articulation consistent with rapid incorporation into the cave sediments early in the decomposition process.18
Case study: Vertebra U.W. 88-37
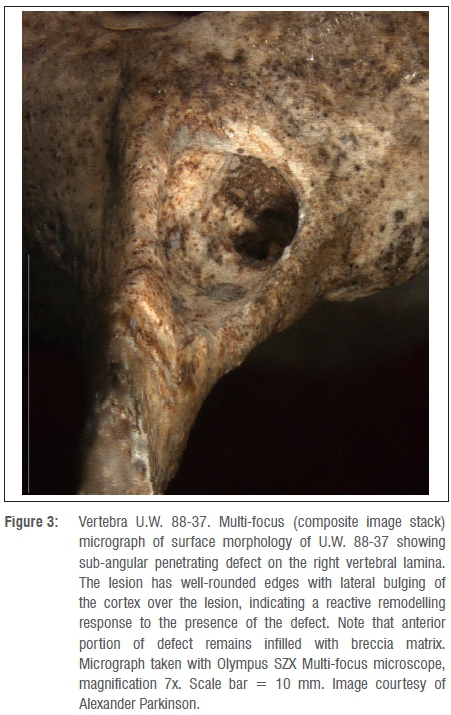
A pathological lesion affects the spine of Malapa Hominin 1 (MH1), the type specimen of Australopithecus sediba. This individual (Figure 1) was male, and at death he was at a developmental stage equivalent to that of a human child aged 12 to 13 years9. The pathological specimen (U.W. 88-37) is a complete vertebra originally assigned to T5-T710, now considered to represent the sixth thoracic vertebra10. The dorsal surface of the right-side lamina exhibits a rounded penetrating defect (Figure 2), measuring approximately 6.7 mm supero-inferiorly and 5.9 mm medio-laterally.

The defect presents as a lytic lesion that extends ventrally into the lamina for much of its length, the most anterior portion of which remains infilled with breccia matrix (Figure 3). On the surface, the lesion has well-rounded edges with a somewhat sclerotic appearance. There is no evidence of periosteal or reactive bone formation on the cortex of the specimen. Viewing the right lamina from above, it appears thicker than the left lamina and bulges laterally over the lesion, indicating a reactive remodelling response to the presence of the defect.
The lesion initially widens directly under the oval opening, but then narrows as it progresses anteriorly. The base of the lesion appears smooth and sclerotic under microscopic evaluation insofar as the presence of residual breccia allows. The spinous process deviates slightly to the right, but appears in keeping with slight asymmetry noted elsewhere in the surviving thoracic vertebrae. This deviation falls within normal variation; we do not consider it significant enough to cause scoliosis or other vertebral misalignment, and it is unlikely that this asymmetry was related to the pathology.
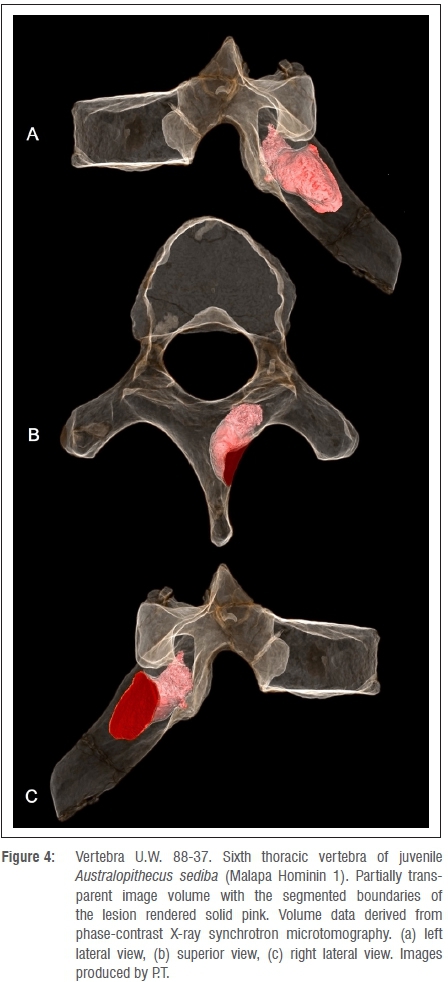
Because of the presence of breccia within the lesion, the internal morphology of the specimen was assessed using phase-contrast X-ray synchrotron microtomography (performed at the European Synchrotron Radiation Facility, ESRF) and a specific acquisition protocol applied for high-quality imaging of large fossils (see Supplementary Appendix materials and methods). From the microtomographic volume, the maximum long axis of the lesion in the transverse plane measures 11.8 mm x 4.9 mm along the minor axis, with a cross-sectional area of 45.6 mm, and in the sagittal plane the lesion measures 14.7 mm x 7.9 mm, with a cross-sectional area of 68.6 mm. The internal linear dimensions are consistently less than 20 mm in diameter, which has important implications for final diagnosis.
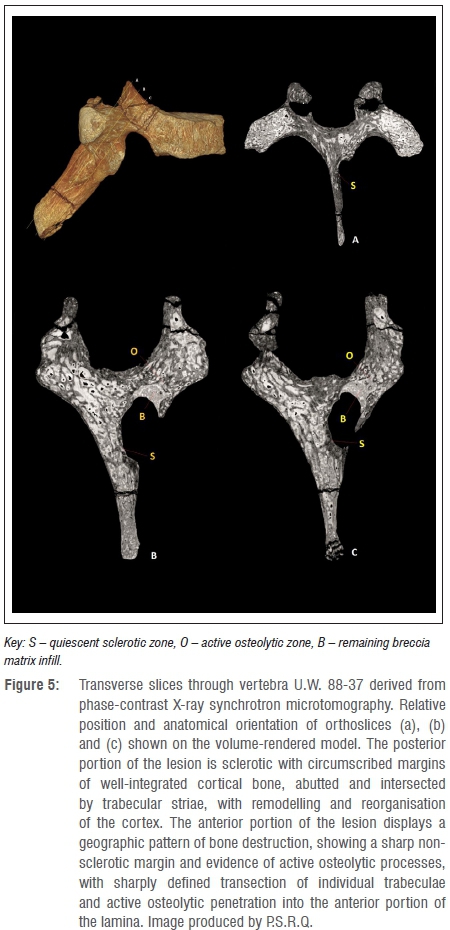
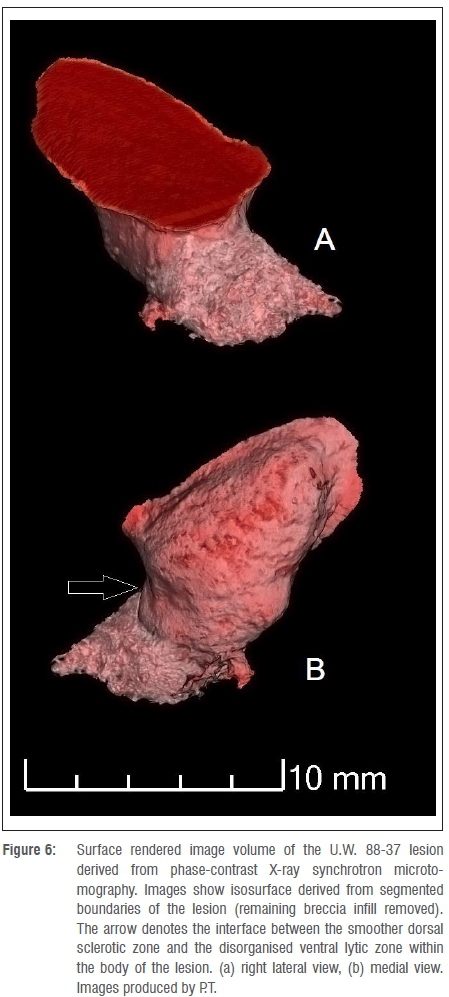
Figure 4 shows the microtomographic imaging, with a semi-transparent volume-rendered image row. The imaging indicates that the lesion is highly penetrative and extends ventrally within the right-side of the spinous process, penetrating the lamina before terminating at the approximate level of the superior articular facet. The internal morphology shows no involvement of the transverse process or pedicle, and the lesion does not penetrate the vertebral canal. No mineralised focal point or nidus was discerned. The edges of the first two-thirds of the lesion (moving dorsal to ventral) display sclerotic characteristics, with circumscribed margins of well-integrated cortical bone, abutted and intersected by trabecular striae (Figure 5 and Supplementary Appendix). This pattern is indicative of a slow-forming bony process, with remodelling and reorganisation of posterior aspects of the lesion. The shape of a lesion is indicative of its growth rate, with lesions that are long and oriented with the long axis of a bone indicating a nonaggressive benign process. The ventral third of the lesion, however, displays a geographic pattern of bone destruction, showing a sharp non-sclerotic margin and evidence of active osteolytic processes, with sharply-defined transection of individual trabeculae, and active osteolytic penetration into the anterior portion of the lamina. A volume-rendered negative surface model of the lesion (Figure 6) demonstrates the clear distinction between the dorsal sclerotic zone and the ventral lytic zone within the body of the active lesion.
Differential diagnosis
Diagnosis was undertaken using palaeopathological and clinical diagnostic criteria1'2,20-34. The accumulated evidence for osteolytic and osteosclerotic processes indicates that the disease process was both chronic and active at the time of death of MH1 (as mentioned, at a developmentally equivalent stage to a modern human child of 12 to 13 years of age). The lesion was less than 15 mm at the largest diameter, extending deep into the right side of the spinous process and involving only the vertebral lamina. The presence of reorganised sclerotic bone indicates a reactive ante-mortem process, and the lesion can therefore not be attributed to taphonomic, diagenetic or pathology-mimicking effects or processes1.
The morphology of the lesion externally and internally is inconsistent with vertebral osteomyelitis. The absence of a proliferative cortical inflammatory response (such as periosteal and/or endosteal bone hypertrophy) or secondary lytic lesions across both the U.W. 88-37 vertebra and the surviving cranial and post-cranial elements of MH1 excludes a diagnosis of specific or non-specific systemic infection, such as brucellosis, nonspecific osteitis, haematogenous osteomyelitis or treponemal osteitis. There is no evidence of deformation or callus formation associated with skeletal trauma such as a healed fracture, and the lesion does not present morphology consistent with post-traumatic processes such as cortical hypertrophy or the development of a cloaca. It is therefore most likely that this condition represents a primary osteogenic or osseous tumour of the spine. These are rare lesions with a much lower incidence than metastases, multiple myeloma or lymphoma.1,2,20,21,23,27,32 Based on age at death, sex, anatomical location of the lesion, and specific patterns of expression and skeletal involvement, conditions such as osteosarcoma, chondrosarcoma or Ewing's sarcoma can be excluded; these neoplasms are often more aggressive, with destruction of the cortex1,21,23.
Included in the differential diagnosis as the most likely cause of the observed lesion are osteoid osteoma, osteoblastoma, giant cell tumour and aneurysmal bone cyst. A number of secondary diagnoses are possible, specifically enostosis (compact bone island), fibrous cortical defect (fibroxanthoma), plasmacytoma, eosinophilic granuloma, and hydatid cyst infection. The range of possible differential diagnoses and primary diagnostic criteria are detailed in Table S1 (Supplementary Appendix).
Based on the observed pathological, morphological, and life-history criteria, the two most likely diagnoses are osteoid osteoma and osteoblastoma. Taking the demographic data for these two tumour types into account, both options seem possible: both are primary bone-forming tumours, osteoblastic in nature; benign; have a predilection for males; and show the highest prevalence in juveniles and adolescents. Osteoid osteoma resembles the observed lesion in terms of size, as these tumours are usually less than 20 mm in diameter, with well-circumscribed margins and being round or oval in form23.
McCall22 notes that computed tomography is the most valuable method to investigate this type of lesion. Under CT imaging of osteoid osteoma a small lucency is often recorded, which may have a central high attenuation as a result of mineralisation, and surrounding sclerotic bone is noted with some thickening of the lamina or pedicle. These are features seen in MH1 (Figure 4). On plain radiographs, most osteoid osteomas are osteosclerotic, with or without a visible nidus. By contrast, Kan and Schmidt35 suggest that osteoblastomas are predominantly lucent or lytic in roughly 50% of cases, sclerotic in 30% of cases, and mixed in the remaining 20% of cases. On plain radiographs, osteoblastomas are typically expansile with a scalloped or lobulated appearance, and their margins are well-defined, with a sclerotic rim evident in approximately 30% of patients. A sclerotic rim is therefore much more common in osteoid osteomas than in osteoblastomas. The smooth, sclerotic, well-defined posterior margins of the lesion we studied are fully consistent with a resolving osteoid osteoma. However, the skeletal distribution of osteoid osteoma might argue against this being the most likely diagnosis, as osteoid osteomas are most commonly found in the lower extremities; occurrence in the spine is less likely than that exhibited in osteoblastoma22.
To quantifiably assess the differential diagnosis, we applied Bayes Theorem of conditional probability to the diagnosis of osteoid osteoma and osteoblastoma. Using absolute clinical incidence data of osteoid osteoma36-38 and osteoblastoma25,37-42 to calculate prior and conditional probabilities of the disease expression in the vertebral column (as opposed to elsewhere in the skeleton), a conditional probability of 0.214 was derived for the likelihood of osteoid osteoma, and 0.068 for osteoblastoma. These results indicate a 3.75-fold higher likelihood that osteoid osteoma was represented in this case than osteoblastoma (see supplementary online material Table S2 for discussion of Bayes parameters and probability functions used). Given the morphological and pathological similarities between the two tumour types, and the age and nature of the specimen under analysis, the results suggest osteoid osteoma firstly and osteoblastoma secondly as the most likely diagnoses of what was clearly a benign entity of abnormal nature.
Discussion
MH1 suffered from a primary osteogenic tumour, which affected the right lamina of the sixth thoracic vertebra. The neoplastic lesion was chronic and was still active at the time of his death. From modern clinical studies36-38 it is likely that osteoid osteoma may have taken months, rather than years, to develop. This neoplastic condition may involve neurological deficits, although this is unlikely as the lesion did not penetrate the neural canal, and no scoliosis was noted. However, the position of the lesion may have affected normal musculoskeletal function and movement of both the shoulder-blade and the upper right quadrant of the back. The tumour may have invoked a number of physiological responses including acute or chronic pain, muscular disturbance and pain-provoked muscular spasm, as discussed in clinical case studies.21,36-38,40 A close association exists between the affected region and overlaying or closely inserting muscles such as trapezius, erector spinae, and rhomboid major, and this might have led to limitations on normal movement, given the likely arboreal component in the locomotor repertoire of A. sediba.9,43
The presence of a primary bone-forming tumour of the spine presents a number of considerations with regard to both the life-history of Australopithecus sediba, and evidence for neoplasia elsewhere in the deep past. Evidence for neoplastic disease is not unknown in the fossil, archaeological and historical records1,8,44. However, preservational factors limit the study of neoplasms to the skeleton (with the rare exception of naturally and artificially mummified bodies that may preserve pathological soft tissues) from which the confident diagnosis of tumours has been problematical45. The earliest skeletal evidence for neoplastic disease comes from pre-Cenozoic contexts, with purported cases of neoplasm found in fossil fish from the Upper Devonian. The earliest unequivocal case dates from 300 Ma, with evidence of benign osteoma with focal hyperostosis affecting the skeleton of Phanerosteon mirabile from the North American Lower Carboniferous3. Later terrestrial cases include diagnoses of benign haemangioma and eosinophilic granuloma in Jurassic dinosaurs; benign osteoma in mosasaurs; and haemangioma, metastatic cancer, desmoplastic fibroma and osteoblastoma in Cretaceous hadrosaurs.46,47 In the more recent past, benign osteoid osteoma and osteoblastoma have been identified in European mammoths dating from 24 000 to 23 000 years ago (ka).48
The presence of neoplastic disease in the hominin fossil record is highly contentious. Until recently, the earliest purported evidence was suggested to be from a mandible of archaic Homo from Kanam, Kenya. This fossil is generally thought to derive from the Lower or Middle Pleistocene, and expresses pathological growth in the symphysial region. The lesion has been attributed to osteosarcoma, bone keloid, or Burkitt's lymphoma, although some researchers have diagnosed it as osteomyelitis resulting from a facial fracture49-52. The first substantive evidence for malignant neoplasia in hominins is derived from the SK7923 metatarsal fragment, dated to 1.8 to 1.6 Ma, from the site of Swartkrans, South Africa; a bony cortical exostosis together with osseous infilling of the medullary cavity of the shaft of the bone has been attributed by Odes and colleagues to osteosarcoma5.
The next significant evidence for near-human neoplastic disease is suggested by Monge and colleagues, who present a case of fibrous dysplasia in a rib of Homo neanderthalensis dated to 120 ka from the European site of Krapina.53 The Middle Pleistocene site of Atapuerca (Sima de los Huesos) evidenced small benign osteoid osteomata affecting the orbital roof of crania AT-777 and the endocranial surface of Cranium 4.54 Other evidence comes from the Vogelherd (Stetten) II parietal bone, initially thought to represent a 35-ka-old Neanderthal, but now known to be Neolithic in origin55; in this specimen new bone formation has been linked to a possible meningioma although the final diagnosis remains equivocal56. The most significant evidence for neoplastic disease in antiquity derives from the bio-archaeological record of the recent Holocene (and the last four millennia in particular) and is detailed in a number of historical reviews and texts1-3,46 to which the reader is directed.
As noted above, neoplastic disease in various forms, including osteoid osteoma and osteoblastoma, is an ancient phenomenon. It first appeared during the Palaeozoic and Mesozoic in extinct fish and members of the Dinosauria respectively.3,46,47 However, the fact that reports of cancers or neoplasms remain exceedingly rare in the fossil record of almost any geological epoch1,3,8,46,47,53 may be due to a number of factors, exacerbated by the relative disjunction between osseous tumours and all other forms of neoplasms. Primary bone tumours are rare compared with other neoplasms and account for around 7% of all soft and hard tissue cancers.22 Neoplasms are historically reported to be rare in wild living mammals, with only 1.8% of deaths in chimpanzee communities reportedly resulting from cancer.3 A mere handful of neoplastic cases have been recorded based on observational studies of camels, deer, gibbons, tigers, kangaroos, pacaranas, fur seals, ferrets, killer whales, harbour seals, sea lions and harp seals.3 However, recent reviews of neoplasms in wild non-human primates57 have shown that neoplastic disease might be far more widespread than previous studies suggest, in both monkeys and great apes; however, the vast majority of such cases involve benign soft tissue rather than malignant tumours. When bone tumours have been noted, they have tended to present as small benign growths such as button osteomata, which have been observed in both gorilla subspecies but have not been seen in either chimpanzees or orangutans57. An isolated case of benign osteochondroma was observed in the Gombe chimpanzee 'Old Female'.58 Whilst these rare cases of neoplasia in non-human primates share morphological homology with human disease expression, it is unclear whether they share a common genetic basis or evolutionary history.
With regard to osteoid osteoma in humans, cytogenetic chromosomal studies indicate some degree of a genetic basis. This includes the involvement of chromosome 22, 22q monosomy and trisomy aberrations59; aberrant expression of transcription factors Runx2 and Osterix, both of which are master regulators of osteoblastic lineage differentiation60; and duplications and deletions at 22q13.159, the locus of which reflects genes that play a role directly in osteogenesis (PDGF-B and ATF-4). The involvement of the latter suite of genes may suggest a degree of evolutionary conservatism, which warrants further investigation across primate taxa. As noted by Odes et al.5, whilst the expression of neoplasia is rare in prehistory, the capacity for neoplastic disease (as evidenced by both fossil evidence and oncogenes) was present in deep-time.
It is no surprise that metastatic bone tumours are rare or absent in the archaeological and fossil records, because of the limited life expectancies of our ancestors6,7 and the low incidence generally of skeletally forming or affecting neoplasms1,3,20,23,46. It is well known that primary bone tumours mostly occur in younger individuals1,20,21,27,37,40, and it can therefore be expected that such tumours would have been present and have a similar prevalence to what is observed among modern individuals. It seems likely that neoplastic disease was as prevalent in ancient hominin populations as that expressed today in wild primate groups, but for various reasons it left little fossil trace. One reason might be the sheer paucity of individuals recovered from the hominin record, which would represent an issue of epidemiological sampling6.
With regard to the earliest evidence for neoplastic disease in the hominin fossil record reported here, the fact that primary bone neoplasms are so rare makes this an important discovery. Whilst we consider it unlikely that neoplastic disease would have played a major role in the evolutionary forces operating on the Homininae, this case provides a unique glimpse into the individual life experience of a single extinct hominin. MH1 provides a window onto the expression and evolution of neoplastic disease in the human lineage, and highlights the utility of multidisciplinary clinical studies applied to the understanding of the evolution and development of disease in the human lineage.
Acknowledgements
We would like to acknowledge the assistance and help of the following people in the production of this research: Bonita de Klerk, Wilma Lawrence and Jennifer Randolph-Quinney. S.A.W. would like to acknowledge the help of Morgan Hill and Eric Mazelis from the Microscopy and Imaging Facility, and Neil Duncan and Eileen Westwig of the Department of Mammalogy at the American Museum of Natural History. Further support in scanning time was given by the European Synchrotron Radiation Facility and by the Department of Radiology at Charlotte Maxeke Academic Hospital in Johannesburg. The research was funded by grants to L.R.B. from the National Geographic Society, the National Research Foundation of South Africa and the DST/NRF South African Centre of Excellence in Palaeosciences. Additional direct support for E.J.O. was received from the National Research Foundation of South Africa and the DST/NRF South African Centre of Excellence in Palaeosciences. M.S. was supported by the National Research Foundation of South Africa.
Authors' contributions
P.S.R.Q. coordinated the research and wrote the original draft of the manuscript, incorporating additional case notes and observational data on U.W. 88-37 as provided by S.A.W., M.S., M.R.M., J.S.S., S.E.C. and L.R.B. Detailed discussion of oncogenetics was provided by T.A, and E.J.O. provided detailed discussion of the historical data on early hominin palaeopathology. P.T. undertook the synchrotron scanning of the specimen, and primary reconstruction, segmentation and imaging. All authors contributed equally to data acquisition and analysis, and to editing.
References
1. Ortner DJ. Tumors and tumor-like lesions of bone. In: Ortner DJ, editor. Identification of Pathological Conditions in Human Skeletal Remains. Amsterdam: Academic Press; 2003. p. 503-544. http://dx.doi.org/10.1016/B978-012528628-2/50057-0 [ Links ]
2. Aufderheide AC, Rodríguez-Martin C. The Cambridge encylopedia of human paleopathology. Cambridge: Cambridge University Press; 1998. [ Links ]
3. Capasso LL. Antiquity of cancer. Int J Cancer. 2005;113(1):2-13. http://dx.doi.org/10.1002/ijc.20610 [ Links ]
4. Jemal A, Bray F, Center M, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69-90. http://dx.doi.org/10.3322/caac.20107 [ Links ]
5. Odes EJ, Randolph-Quinney PS, Steyn M, Throckmorton Z, Smilg JS, Zipfel B, et al. Earliest hominin cancer: 1.7-milllion-year-old osteosarcoma from Swartkrans Cave, South Africa. S Afr J Sci. 2016;112(7/8), Art. #2015 0471, 5 pages. http://dx.doi.org/10.17159/sajs.2016/20150471 [ Links ]
6. Chamberlain AT. Demography in archaeology. Cambridge: Cambridge University Press; 2006. http://dx.doi.org/10.1017/CBO9780511607165 [ Links ]
7. Mann A. Paleodemographic aspects of the South African australopithecines. Philadelphia: University of Pennsylvania; 1975. [ Links ]
8. Retief FP Cilliers L. Breast cancer in antiquity. S Afr Med J. 2011;101(8):513- 515. [ Links ]
9. Berger LR, de Ruiter DJ, Churchill SE, Schmid P Carlson KJ, Dirks PHGM, et al. Australopithecus sediba: A new species of Homo-like australopith from South Africa. Science. 2010;328(5975):195-204. http://dx.doi.org/10.1126/science.1184944 [ Links ]
10. Williams SA, Ostrofsky KR, Frater N, Churchill SE, Schmid P Berger LR. The vertebral column of Australopithecus sediba. Science. 2013;340(6129). http://dx.doi.org/10.1126/science.1232996 [ Links ]
11. Berger L, Lacruz R, De Ruiter D. Revised age estimates of Australopithecus-bearing deposits at Sterkfontein, South Africa. Am J Phys Anthropol. 2002;119:192-197. http://dx.doi.org/10.1002/ajpa.10156 [ Links ]
12. Brain CK. Structure and stratigraphy of the Swartkrans Cave in the light of the new excavations. In: Brain CK, editor. Swartkrans. Pretoria: Transvaal Museum Monograph 8; 1993. p. 23-34. [ Links ]
13. Berger LR, Menter CG, Thackeray JF. The renewal of excavation activities at Kromdraai, South Africa. S Afr J Sci. 1994;90:209-210. [ Links ]
14. Lacruz RS, Brink JS, Hancox J, Skinner AS, Herries A, Schmidt P et al. Paleontology, geological context and paleoenvironmental implications of a Middle Pleistocene faunal assemblage from the Gladysvale Cave, South Africa. Paleontologia Africana. 2002;38:99-114. [ Links ]
15. Dirks PHGM, Berger LR, Roberts EM, Kramers JD, Hawks J, Randolph-Quinney PS, et al. Geological and taphonomic context for the new hominin species Homo naledi from the Dinaledi Chamber, South Africa. eLife. 2015;4, Art. #e09561. http://dx.doi.org/10.7554/eLife.09561 [ Links ]
16. Dirks P, Berger L. Hominin-bearing caves and landscape dynamics in the Cradle of Humankind, South Africa. J Afr Earth Sci. 2012;78:109-131. http://dx.doi.org/10.1016/j.jafrearsci.2012.09.012 [ Links ]
17. Dirks PHGM, Kibii JM, Kuhn BF, Steininger C, Churchill SE, Kramers JD, et al. Geological setting and age of Australopithecus sediba from Southern Africa. Science. 2010;328(5975):205-208. http://dx.doi.org/10.1126/science.1184950 [ Links ]
18. Val A, Dirks PHGM, Backwell LR, d'Errico F, Berger LR. Taphonomic analysis of the faunal assemblage associated with the hominins (Australopithecus sediba) from the Early Pleistocene cave deposits of Malapa, South Africa. PLoS ONE. 2015;10(6), Art. #e0126904. http://dx.doi.org/10.1371/journal.pone.0126904 [ Links ]
19. LAbbé EN, Symes SA, Pokines JT, Cabo LL, Stull KE, Kuo S, et al. Evidence of fatal skeletal injuries on Malapa Hominins 1 and 2. Sci Rep. 2015;5, Art. #15120. http://dx.doi.org/10.1038/srep15120 [ Links ]
20. Bahk Y-W. Combined scintigraphic and radiographic diagnosis of bone and joint diseases. New York: Springer; 2007. http://dx.doi.org/10.1007/978-3-540-68732-0_4 [ Links ]
21. Khurana JS. The surgical pathology of bone tumors and tumor-like lesions. In: Khurana JS, editor. Bone pathology. London: Humana Press; 2009. p. 285-345. http://dx.doi.org/10.1007/978-1-59745-347-9_19 [ Links ]
22. McCall IW. Radiology and pathological correlations of bone tumours of the spine. In: Gourtsoyiannis NC, Ros PR, editors. Radiologic-pathologic correlations from head to toe: Understanding the manifestations of disease. Berlin: Springer; 2005. p. 721-742. http://dx.doi.org/10.1007/3-540-26664-X_32 [ Links ]
23. Vigorita VJ. Orthopaedic pathology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. [ Links ]
24. Baba H, Maezawa Y, Furusawa N, Wada M, Kokubo Y, Imura S, et al. Solitary plasmacytomas of the spine associated with neurological complications. Spinal Cord. 1998;36(7):470-l75. http://dx.doi.org/10.1038/sj.sc.3100572 [ Links ]
25. Berry M, Mankin H, Gebhardt M, Rosenberg A, Hornicek F. Osteoblastoma: a 30-year study of 99 cases. J Surg Oncol. 2008;98:179-183. http://dx.doi.org/10.1002/jso.21105 [ Links ]
26. Betsy M, Kupersmith LM, Springfield DS. Metaphyseal fibrous defects. J Am Acad Orthop Surg. 2004;12(2):89-95. http://dx.doi.org/10.5435/00124635-200403000-00004 [ Links ]
27. Binning M, Klimo Jr P Gluf W, Goumnerova L. Spinal tumors in children. Neurosurg Clin N Am. 2007;18(4):631-658. http://dx.doi.org/10.1016/j.nec.2007.07.001 [ Links ]
28. McLain RF, Weinstein JN. Solitary plasmacytomas of the spine: A review of 84 cases. J Spinal Disord. 1989;2(2):69-74. http://dx.doi.org/10.1097/00002517-198906000-00001 [ Links ]
29. Mendenhall WM, Zlotecki RA, Scarborough MT, Gibbs CP, Mendenhall NP. Giant cell tumor of bone. Am J Clin Oncol. 2006;29(1):96-99. http://dx.doi.org/10.1097/01.coc.0000195089.11620.b7 [ Links ]
30. Celik C, Münevver FS, Ucan H. Spinal hydatid cyst: Review. Türkiye Klinikleri J Med Sci. 2010;30(3):1073-1077. http://dx.doi.org/10.5336/medsci.2009-13722 [ Links ]
31. Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: Concept, controversy, clinical presentation, and imaging. Am J Roentgenol. 1995;164(3):573-580. http://dx.doi.org/10.2214/ajr.164.3.7863874 [ Links ]
32. Osborn AG. Tumors, cysts, and tumorlike lesions of the spine and spinal cord. In: Osborn AG, editor. Diagnostic neuroradiology. St. Louis: Mosby; 1994. p. 876-918. [ Links ]
33. Kuruvath S, O'Donovan DG, Aspoas AR, David KM. Benign fibrous histio-cytoma of the thoracic spine: Case report and review of the literature. J Neurosurg Spine. 2006;4(3):260-264. http://dx.doi.org/10.3171/spi.2006.4.3.260 [ Links ]
34. Kaye JJ, Freiberger RH. Eosinophilic granuloma of the spine without vertebra plana: A report of two unusual cases. Radiology. 1969;92(6):1188-1191. http://dx.doi.org/10.1148/92.6.1188 [ Links ]
35. Kan P Schmidt MH. Osteoid osteoma and osteoblastoma of the spine. Neurosurg Clin North Am. 2008;19(1):65-70. http://dx.doi.org/10.1016/j.nec.2007.09.003 [ Links ]
36. de Souza Dias L, Frost HM. Osteoid Osteoma-Osteoblastoma. Cancer. 1974;33(4):1075-1081. http://dx.doi.org/10.1002/1097-0142(197404)33:4<1075::AID-CNCR2820330427>3.0.CO;2-4 [ Links ]
37. Azouz EM, Kozlowski K, Marton D, Sprague P Zerhouni A, Asselah F. Osteoid osteoma and osteoblastoma of the spine in children: Report of 22 cases with brief literature review. Pediatr Radiol. 1986;16(1):25-31. http://dx.doi.org/10.1007/BF02387501 [ Links ]
38. Saccomanni B. Osteoid osteoma and osteoblastoma of the spine: A review of the literature. Curr Rev Musculoskelet Med. 2009;2(1):65-67. http://dx.doi.org/10.1007/s12178-009-9047-6 [ Links ]
39. Lucas DR. Osteoblastoma. Arch Pathol Lab Med. 2010;134:1460-1466. [ Links ]
40. Amacher AL, Eltomey A. Spinal osteoblastoma in children and adolescents. Child Nerv Syst. 1985;1(1):29-32. http://dx.doi.org/10.1007/BF00706727 [ Links ]
41. Aszódi K. Benign osteoblastoma: Quantitative histological distinction from osteoid osteoma. Arch Orthop Unfallchir. 1977;88(3):359-368. http://dx.doi.org/10.1007/BF00416625 [ Links ]
42. Boriani S, Capanna R, Donati D, Levine A, Picci P Savini R. Osteoblastoma of the spine. Clin Orthop Relat Res. 1992;278:37-45. http://dx.doi.org/10.1097/00003086-199205000-00006 [ Links ]
43. Churchill SE, Holliday TW, Carlson KJ, Jashashvili T, Macias ME, Mathews S, et al. The upper limb of Australopithecus sediba. Science. 2013;340(6129), Art. #1233477. http://dx.doi.org/10.1126/science.1233477 [ Links ]
44. Eshed V Latimer B, Greenwald CM, Jellema LM, Rothschild BM, Wish-Baratz S, et al. Button osteoma: Its etiology and pathophysiology. Am J Phys Anthropol. 2002;118(3):217-230. http://dx.doi.org/10.1002/ajpa.10087 [ Links ]
45. Rothschild BM, Rothschild C. Comparison of radiologic and gross examination for detection of cancer in defleshed skeletons. Am J Phys Anthropol. 1995;96(4):357-363. http://dx.doi.org/10.1002/ajpa.1330960404 [ Links ]
46. Rothschild BM, Martin LD. Paleopathology: Disease in the fossil record. Boca Raton, FL: CRC Press; 1993. [ Links ]
47. Rothschild BM, Tanke DH, Hebling M, Martin LD. Epidemiologic study of tumors in dinosaurs. Naturwissenschaften. 2003;90(11):495-500. http://dx.doi.org/10.1007/s00114-003-0473-9 [ Links ]
48. Leshchinsky SV. Paleoecological investigation of mammoth remains from the Krakow Spadzista Street (B) site. Quartern Int. 2012;276-277:155-169. http://dx.doi.org/10.1016/j.quaint.2012.05.025 [ Links ]
49. Phelan J, Weiner MJ, Ricci JL, Plummer T, Gauld S, Potts R, et al. Diagnosis of the pathology of the Kanam Mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(4), Art. #e20. http://dx.doi.org/10.1016/j.tripleo.2006.12.041 [ Links ]
50. Tobias PV. The Kanam jaw. Nature. 1960;185:946-947. http://dx.doi.org/10.1038/185946a0 [ Links ]
51. Tobias PV. A re-examination of the Kanam mandible. In: Mortelmans G, Nenquin J, editors. Actes du IVe Congres Panafricain de Préhistoire et de l'Étude du Quaternaire, Sections I and II. Tervuren, Belgique: Annales Ser. Qu-8o, Sciences Humaines 40; 1962. p. 341-350. [ Links ]
52. Stathopoulos G. Kanam mandible's tumour. Lancet. 1975;305(7899). p. 165. http://dx.doi.org/10.1016/S0140-6736(75)91462-2 [ Links ]
53. Monge J, Kricun M, Radovcic J, Radovcic D, Mann A, Frayer DW. Fibrous dysplasia in a 120,000+ year old Neandertal from Krapina, Croatia. PLoS ONE. 2013;8(6), Art. #e64539. http://dx.doi.org/10.1371/journal.pone.0064539 [ Links ]
54. Pérez P Gracia A, Martinez I, Arsuaga J. Paleopathological evidence of the cranial remains from the Sima de los Huesos Middle Pleistocene site (Sierra de Atapuerca, Spain). Description and preliminary inferences. J Hum Evol. 1997;33(2):409-421. http://dx.doi.org/10.1006/jhev.1997.0139 [ Links ]
55. Conard NJ, Grootes PM, Smith FH. Unexpectedly recent dates for human remains from Vogelherd. Nature. 2004;430:198-201. http://dx.doi.org/10.1038/nature02690 [ Links ]
56. Czarnetzki A. Pathological changes in the morphology of the Young Paleolithic skeletal remains from Stetten (South-west Germany). J Hum Evol. 1980;9(1):15-17. http://dx.doi.org/10.1016/0047-2484(80)90037-8 [ Links ]
57. Lovell NC. Patterns of injury and illness in Great Apes. Washington, DC: Smithsonian Press; 1990. [ Links ]
58. Jurmain R. Trauma, degenerative disease and other pathologies among the Gombe chimpanzees. Am J Phys Anthropol. 1989;80(2):229-237. http://dx.doi.org/10.1002/ajpa.1330800211 [ Links ]
59. López-Terrada D, Hicks JM. Genetics and molecular biology of bone and soft tissue tumors. In: Khurana JS, editor. Bone pathology. Dordrecht: Humana Press; 2009. p. 91-124. http://dx.doi.org/10.1007/978-1-59745-347-9_6 [ Links ]
60. Dancer J, Henry S, Bondaruk J, Lee S, Ayala A, de Crombrugghe B, et al. Expression of master regulatory genes controlling skeletal development in benign cartilage and bone forming tumors. Hum Pathol. 2010;41(12):1788- 1793. http://dx.doi.org/10.1016/j.humpath.2010.06.008 [ Links ]
 Correspondence:
Correspondence:
Patrick Randolph-Quinney
School of Forensic and Applied Sciences, University of Central Lancashire
Preston, Lancashire, PR1 2HE, UK
prandolph-quinney@uclan.ac.uk
Received: 11 Dec. 2015
Revised:16 Mar. 2016
Accepted: 17 Mar. 2016
* Current address: School of Forensic and Applied Sciences, University of Central Lancashire, Preston, Lancashire, United Kingdom














