Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Social Work
versión On-line ISSN 2312-7198
versión impresa ISSN 0037-8054
Social work (Stellenbosch. Online) vol.60 no.1 Stellenbosch 2024
http://dx.doi.org/10.15270/60-1-1245
ARTICLES
Should the Covid-19 pandemic be considered a traumatic stressor? Some concerns for mental health professionals
Ashraf Kagee
Stellenbosch University, Department of Psychology, Stellenbosch, South Africa https://orcid.org/0000-0003-1241-2566 skagee@sun.ac.za
ABSTRACT
This opinion article argues that it may not be appropriate to regard the Covid-19 pandemic as a traumatic stressor. Persons diagnosed with Covid-19 have typically been concerned about events that might have occurred in the future such as severe illness, hospitalisation and death, access to treatment, the welfare of dependents, and stigma and discrimination. Their concerns are thus future-oriented rather than anchored to a past traumatic event, which is the requirement for a diagnosis of PTSD. If the criteria for what is considered a traumatic stressor are widened, there is a risk that the concept of trauma may become so diluted that many events, even mildly distressing ones, may be regarded as traumatic. Social workers and other health professionals should take these matters into account when attending to the emotional and psychological needs of persons affected by the Covid-19 pandemic.
Keywords: Covid-19; distress; pandemic; post-traumatic stress; trauma
INTRODUCTION
Various authors have argued that the Covid-19 pandemic has been a stressor of such magnitude that it is appropriate to conceptualise it as a traumatic stressor (e.g. Jukes, Fowler-Watt & Rees, 2022; Masiero, Mazzocco, Harnois, Cropley & Pravettoni, 2020). This opinion article argues that such a conceptualisation may be inappropriate. The Covid-19 illness trajectory usually follows the course of infection and the experience of symptoms such as fever, cough, or loss of sense of smell (anosmia) or taste (ageusia) (Struyf et al., 2022). Some infected persons require hospitalisation, usually involving ventilation, when symptoms do not abate (Möhlenkamp & Thiele, 2020). Recovery may take days or months and, in some cases, death occurs (Jordan, Adab & Cheng, 2020). When people recover, most resume normal functioning in time, although for some the condition known as "long Covid" can be an enduring experience (Yong, 2021). As of this writing, of the nearly 600 million recorded cases of Covid 19, there have been approximately 6.8 million deaths worldwide (CSSE: Center for Systems Science and Engineering, 2023). Some authors have suggested that post-traumatic stress should be included to help make sense of the public mental health crisis that may follow the pandemic (Horesh & Brown, 2020). Indeed, Vanaken and colleagues have argued that trauma-related stress symptoms are an important aspect of the psychological impact of Covid-19 pandemic (Vanaken, Scheveneels, Belmans, & Hermans, 2020). It has been argued that the pandemic involves characteristics that pertain to "mass traumatic events" with sequelae such as hypervigilance, avoidance and intrusive thoughts related to health status (Horesh & Brown, 2020).
In South Africa, similar to most countries around the globe, the Covid-19 lockdown protocols forced millions of citizens to change their work and school routines and social lives. Strict rules required all persons to remain at home except for essential purposes. The lockdown caused considerable disruption to individuals, families, households, communities, and the national economy (Arndt et al., 2020).
RESEARCH ON MENTAL HEALTH EFFECTS OF COVID 19
Among 84 Canadian respondents, 61% reported psychological distress related to depression, anxiety, or post-traumatic stress disorder (PTSD). Of this sample, 43% reported anxiety-related symptoms, 33% reported depression-related symptoms, and 6% had PTSD-related symptoms (Gill et al., 2022). In a study of 10,000 participants in various countries, the pandemic was experienced as moderately stressful for most people, and 11% reported high levels of stress (Gloster et al., 2020). Depression was reported by 25% of the sample. Predictors of good mental health were high levels of social support, education level and psychological flexibility while limited finances and insufficient resources predicted poorer outcomes. In a meta-analysis of 19 studies among pregnant women, the overall prevalence estimates of anxiety and depression during COVID-19 were 42% and 25%, respectively (Fan et al., 2021), with younger participants being more vulnerable to anxiety. Much of the literature suggests that the experience of the Covid-19 pandemic has been severely stressful for large numbers of people across the world.
COVID 19 AS A TRAUMATIC EXPERIENCE
According to the Diagnostic and Statistical Model of Mental Disorders (DSM5) (American Psychiatric Association, 2013) and the International Classification of Diseases (ICD-11) (World Health Organisation, 2019:271), a traumatic stressor involves:
exposure to actual or threatened death, serious injury, or sexual violence in ways that include directly experiencing the event; witnessing the event as it occurred to others; learning that the event(s) occurred to a close family member or close friend; or experiencing repeated or extreme exposure to aversive details of the traumatic event.
Typical events that are considered traumatic stressors include exposure to war, threatened or actual physical assault or sexual violence, being kidnapped, being taken hostage, a terrorist attack, torture, incarceration as a prisoner of war, natural or human-made disasters, and severe motor vehicle accidents. Importantly, a life-threatening illness or debilitating medical condition is not necessarily considered a traumatic event.
There has also been an argument that Covid-19 is a new type of traumatic stressor and is unique because of its "uncontrolled invisibility" (Kira et al., 2021). Kira et al. (2021) have argued that COVID-19-related traumatic stress is not necessarily related to actual infection with COVID-19, but pertains to the perceived or actual threat of an uncontrolled virus and the various economic and social consequences of actions taken by different agencies to mitigate its effects. It has been suggested that the condition of "Covid Stress Syndome" be conceptualised to account for distress associated with Covid (Taylor et al., 2020). However, as noted by Norrholm et al. (2021), there are nosological problems with creating new mental disorders that are associated with specific types of events. Indeed, these authors suggest that clinicians and researchers adhere to a specific and narrow interpretation of the DSM5 criteria rather than a broader approach, as the latter risks diluting the PTSD diagnosis (Norrholm et al, 2021).
On the other hand, Masiero et al. (2020) suggest that COVID-19 may be conceptualised as the cause of individual and collective traumas that should be the focus of research. These authors cite four potential sources of trauma, namely moral injury among healthcare professionals who were required to make triaging decisions about which patients to ventilate, traumatic grief among persons who experienced loss of loved ones, loss of roles and identity, and social divisions related to economic shutdown. Their article was published quite early in the pandemic trajectory when there was considerable uncertainty about the nature of the Covid-19 virus and its effects on global health.
The Covid-19 Traumatic Stress Scale, a 12-item instrument, was developed to assess trauma responses to the Covid-19 pandemic (Kira et al., 2021). Items on the scale include "I am afraid of the coronavirus", "I am stressed around other people because I worry I'll catch the coronavirus", and "Thinking about the coronavirus makes me feel threatened". An index event of infection is not required as an anchor for the scale items. Instead, the index event is the experience of the pandemic in general, rather than a specific event such as hospitalisation and intubation. Also, most of the items do not map onto symptoms of traumatisation as specified in the DSM-5 (American Psychiatric Association, 2022). Instead, they relate to concerns about being infected with the virus, losing one's job, and feeling isolated because of the lockdown. Thus, while the scale measures emotional distress, it is unlikely to be a valid measure of trauma.
THEORISING PTSD
Various theories such as Mowrer's two-factor theory and Foa's emotional processing theory have been proposed to explain the occurrence of symptoms following exposure to a traumatic stressor. Mowrer's two-factor theory suggests that classical and instrumental conditioning can explain symptoms such as fear and anxiety (Smith & Suda, 1999). Emotional processing theory developed by Foa and colleagues suggests that emotional disorders reflect the presence of emotion structures such as fear in memory (Foa & Kozak, 1986). These fear structures include representations of stimuli related to emotional responses, the meanings associated with these stimuli and responses, and the associations among these representations. When someone encounters information that matches some of the information represented in the fear structure, this fear structure is activated which results in the spread of activation to associated representations. In this way cognitive, behavioural and physiological reactions are produced. A fear structure becomes maladaptive or pathological when associations among representations of stimuli do not accurately represent reality (Foa & Kozak, 1986). Thus, a harmless stimulus may be erroneously associated with a threat. There are areas of overlap between emotional processing theory and conditioning theories of PTSD. However, emotional processing theory incorporates associations between stimuli and responses and focuses on the meanings associated with them. According to emotional processing theory, PTSD involves an event that occurred in the past and thus the actual threat related to the event is also past-oriented. However, in cases of chronic PTSD, people process the traumatic stressor and its sequelae consequences in such a way that there is a continued sense of current threat. A related theory, schema theory, suggests that core beliefs are held by most people, for example, that the world is benign and meaningful, that the self is worthy, and that people are trustworthy. These assumptions are altered following a traumatic event (Janoff-Bulman, 1989).
CONCEPTUALISING COVID-19 AS A TRAUMA
A diagnosis of PTSD requires there to have been exposure to actual or threatened death, serious injury or sexual violence by directly experiencing the traumatic event. The ensuing symptoms of PTSD anchored to the traumatic event fall into symptom clusters (discussed below). The DSM-5 states that a life-threatening illness or debilitating medical condition is not necessarily considered a traumatic event. Medical incidents that qualify as traumatic events involve sudden, catastrophic events such as waking during surgery and anaphylactic shock (American Psychiatric Association, 2022).
It is reasonable to assume that a response to receipt of information that one is infected with COVID can potentially be accompanied by intense fear, feelings of helplessness, and horror (Criterion A1), especially if the news is unexpected. Yet with large numbers infected around the world, infection was unlikely to be a surprise for most people. Nonetheless, with receipt of information about a positive Covid-19 test result as the anchoring traumatic event, the symptoms of intrusion, avoidance and hyperarousal warrant examination.
The requirement for a traumatic stressor is exposure to actual or threatened violent or accidental death, serious injury, or sexual violence by directly experiencing the traumatic event(s); witnessing the event as it occurred to others; learning that it occurred to a close family member or close friend; or experiencing repeated or extreme exposure to aversive details of the event. Symptoms of intrusion (B criteria) include recurrent and intrusive distressing memories of the traumatic event(s); distressing dreams; psychological distress at exposure to cues related to the event; and physiological reactions to cues about the event. Symptoms of avoidance (C criteria) relate to efforts to avoid distressing thoughts or feelings and reminders about the event. Negative alterations in cognitions and mood (D criteria) involve an inability to remember important aspects of the event; exaggerated negative beliefs or expectations; distorted cognitions about the event; a persistent negative emotional state; and diminished interest in significant activities. Alterations in arousal and reactivity (E criteria) include irritability, hypervigilance and startle shock response.
The B criteria and C criteria are most problematic from a nosological perspective. For a diagnosis of PTSD, these symptoms need to be anchored to the event, which may be either receipt of a positive Covid-19 test result, experiencing symptoms of Covid-19, or hospitalisation involving intubation. The question arises whether one may indeed experience receipt of a positive test result as a disorder of memory rather than as a threat to one's future health and possible mortality. The meaning attributed to a positive Covid-19 test result by most people is likely to be future rather than past-oriented. Distress experienced by persons with a positive result is unlikely to stem from disturbing memories, but rather from concern about likely future events such as illness, hospitalisation and death.
In an online survey of 2,025 adults in the United Kingdom, elevated levels of anxiety, depression and symptoms of traumatisation were reported at the beginning of the pandemic, compared to previous population studies (Shevlin et al., 2020). These researchers used the International Trauma Questionnaire to assess symptoms of re-experiencing, avoidance and sense of threat to an index stressor which was defined as "in relation to your experience of the COVID-19 pandemic" (Shevlin et al., 2020). However, this index stressor does not conform to the DSM5 criterion A for PTSD and should be more specific, for example, receipt of a Covid-19 test result, having severe symptoms, or hospitalisation including intubation.
A second concern is that a diagnosis of PTSD requires symptoms to occur consequent to a past event. When receiving a positive Covid-19 test result, concerns about hospitalisation, intubation and possible death would thus not qualify as stressors, because these events exist as possibilities in the future. There is a risk of confusion between an anchoring event that did occur thus precipitating symptoms of trauma, and future possible events that have not occurred and that may be the source of concern or worry.
To counter this view, Addis has presented three arguments that remembering and imagining are "fundamentally the same process" (Addis, 2020). First, this author argues that both remembering and imagining involve a simulation system that draws on elements of experience that include detailed descriptions, conceptual information and mental schemas about how the world is constructed. Second, both remembering and imagining operate according to the same rules, namely the construction of schemas, the representation of the event itself, and the interaction between the two. Third, both involve the same brain system that drives cognitions (Addis, 2020). However, while these three factors may indeed be common to memory and imagining, they are uniquely separate phenomena. Memory is anchored to an event that has already occurred, while imagining is applied to events that have never occurred, but that may or may not occur in the future. It is therefore inaccurate to conflate the two mental experiences and assume that they approximate the same mental processes. Memory is encoded based on experience, while imagining is not.
It is a slippery slope that can lead to conceptual bracket creep if it is argued that imagining future events can provoke symptoms of traumatisation, for example, among soldiers before they set off to war, or persons whose loved ones are likely to die in the near future (Bridgland et al., 2021). Conceptual bracket creep occurs when ordinary stressors that may hitherto have been distressing are, as a result of a shifting definition, deemed capable of producing PTSD. By this logic imagining any unpleasant or horrifying experience can be classified as a traumatic stressor, thus rendering the term meaningless. In their internet-based study of over 1,000 participants in the United States, United Kingdom, Canada, Australia and New Zealand, Bridgland and colleagues modified the PTSD Checklist to measure symptoms related to "Covid-19 experiences" (p. 5) and asked respondents to state if each trauma-related symptom was associated with an event that occurred in the past, present or "might occur in the future" (Bridgland et al., 2021). Based on this method 13.2% of respondents were classified as "PTSD positive", of whom 60.6% were not exposed to the virus. More participants who had been directly exposed to the virus were "PTSD positive" than those who had not been exposed: 16.5% versus 11.6%.
There are two problems with Bridgland's study. First, the index events included 32 possible Covid-19-related events that included "someone I know has tested positive for Covid-19", "My workplace has closed but I am still earning a salary", "My or my partner's workplace has reduced working hours", and "I have been working studying from home". Participants were asked how much these events bothered them. It has been argued that the Covid-19 pandemic is a multiple complex trauma that consists of a fear of infection and possible death (Ornell et al., 2020), economic hardship that may accompany job loss, business failure and a distressed economy (McKibbin & Fernando, 2020). The stresses of lockdown, social isolation, disrupted routines created ruptures in family and social life (Brooks et al., 2020). Lockdowns in most countries created conditions for emotional distress and most people around the world would have in some way been affected by at least some of these events. Thus, stating that they were bothered by them is a very low threshold for constituting an index event for traumatic stress. Working or studying from home, working and still earning a salary, and having a partner who has reduced working hours can hardly be considered as traumatic stressors.
Second, in Bridgland's study the term "PTSD positive" refers to persons scoring > 33 on the PTSD Checklist for DSM5 (PCL-5), which is the cut-off for clinical significance (Bridgland et al., 2021). The PCL-5 is a 20-item questionnaire that corresponds to the DSM-5 symptom criteria for PTSD. This method of determining traumatisation does not refer to caseness for post-traumatic stress disorder, as the PCL-5 is a screening rather than a diagnostic instrument. The PCL-5 has limited sensitivity and specificity when compared to a gold standard diagnostic assessment instrument such as the Structured Clinical Interview for the DSM5 (Kagee et al., 2022). In their study among users of antiretroviral therapy, Kagee et al. found that the PCL-5 identified positive cases 56.3% of the time using the SCID-5 as the diagnostic gold standard for PTSD (Kagee et al., 2022).
Taken together, the argument that PTSD-like responses may occur in response to past, present and future events is therefore spurious. McNally has called attention to a conceptual bracket creep in how trauma is defined, so that what would typically be considered an ordinary stressor is now regarded a traumatic stressor (McNally, 2006). Bracket creep is a concerning development for at least three reasons. First, expanding the definition of trauma may limit the scope to identify the underlying psychobiological processes that lead to PTSD. Second, a broad concept of trauma limits the extent to which the stressor can be said to be the cause of the ensuing psychological symptoms as preexisting personal vulnerability factors are more likely to play an important role. A shift away from the stressor and towards predisposing factors as a cause of the person's reaction would then eliminate the rationale for PTSD. Third, conceptualising most events that are part of life as traumatic risks medicalising normal human distress to stressful events (McNally, 2006).
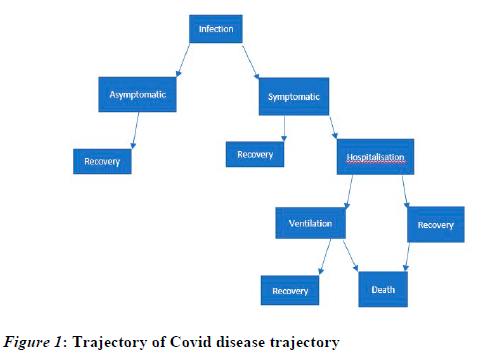
Figure 1 displays the Covid-19 disease trajectory. Of most consequence to mental health professionals, including social workers, are the mental health consequences of infection, being symptomatic, hospitalisation and death. To examine the potential for the Covid-19 experience to qualify as an index event, it is useful to divide the experience into two components, namely, infection with Covid-19 and the ensuing experience of mild to moderate symptoms, and hospitalisation in the event of severe symptoms.
Common symptoms associated with Covid-19 infection are: fatigue, shortness of breath, muscle pain, joint pain, headache, cough, chest pain, altered smell, altered taste and diarrhoea (Aiyegbusi et al., 2021). Other symptoms include cognitive impairment, loss of memory, anxiety and sleep disturbance, and worry about the possibility of hospitalisation and death (Muñoz-Navarro et al., 2021). Yet none of these experiences approximates a traumatic event as specified by DSM5 criteria as delineated above.
Hospitalisation for a Covid-19 has been described as a "potential trigger for PTSD" (Martínez-Caballero et al., 2021). Hospitalisation for severe symptoms associated with Covid-19 infection may include pain from endotracheal intubation, limited ability to communicate, and feelings of loss of control, all of which may be associated with fear of death from Covid-19.
The meaning of a Covid-19 test result varied as the pandemic progressed. In early 2020 when the pandemic was a new experience and was associated with numerous deaths, infection represented potential severe illness and death. Later in 2020 as epidemiological data became available, it became apparent that deaths and severe infection occurred in a minority of infected persons (Ceylan, 2020). When vaccines were developed and introduced (Rudan et al., 2022), the number of cases of severe symptoms, hospitalisation and deaths declined dramatically (Andrews et al., 2022). The changing nature of the Covid-19 pandemic has had implications for how people responded psychologically. It is to be expected that distress associated with the risk of infection may be alleviated following vaccination.
DOES A POSITIVE COVID-19 TEST RESULT IN PSYCHOLOGICAL TRAUMA?
To argue that a positive Covid 19 test result is not traumatic is not to deny its potentially emotionally distressing nature. A positive Covid-19 test result was likely to be psychologically disturbing for most people, especially before the availability of vaccines, potentially leading to feelings of despondency, fear, worry and concern about the future. However, distress is different from PTSD, which has specific diagnostic criteria. While social support and supportive counselling may be indicated for emotional distress, best practice treatment for PTSD includes cognitive therapy (Hembree & Foa, 2000) and anti-anxiety medication (Boehnlein & Kinzie, 2007). Conceptualising someone's psychological status in terms of PTSD is likely to be inaccurate and may lead to inappropriate approaches to intervention.
HOSPITALISATION FOR SEVERE SYMPTOMS OF COVID-19
A possible exception to the application of diagnostic criteria for PTSD to the Covid-19 experience is hospitalisation for severe symptoms of Covid-19, which may include endotracheal intubation, and can be associated with pain, inability to communicate and consequent feelings of loss of control (Asimakopoulou & Madianos, 2015). Research on the psychological sequelae associated with intensive care treatment in general suggests that elevated distress is common, especially among women and young persons (Girard et al., 2007; Jones et al., 2001). In five hospitals around Athens, Greece, Asimakopoulou and Madianos found the prevalence of PTSD to be 35.3% among ICU patients and 13.5% among non-ICU patients, with 11.6% meeting the criteria for both major depression and PTSD (Asimakopoulou & Madianos, 2014).
The treatments used in ICU care in and of themselves commonly result in anxiety, pain and traumatic symptoms (Girard et al., 2007). Yet, in addition, critical illness including severe injury are reasons for people to be admitted to ICU, which then could be considered the index event rather than experiences in ICU such as intubation. For example, in Girard's study, even though PTSD was not assessed at admission to ICU, some study participants may have had pre-existing PTSD (Girard et al., 2007). On the other hand, Patel and colleagues found that approximately 10% of ICU survivors experienced ICU-related PTSD, i.e. related to their critical illness in the twelve months following hospitalisation (Patel et al., 2016), even though preexisting PTSD and depression were strongly associated with ICU-related PTSD. Nonetheless, it is reasonable to conclude that mechanical ventilation and intubation, with their attendant experiences of feeling out of control, are both highly distressing for most patients who receive them and potentially traumatic for some.
THE IMPACT OF EVENT SCALE AND COVID-19
The Impact of Event Scale Covid-19 (IES-COVID19) was developed from the Impact of Event Scale (IES) in the Netherlands, with higher scores indicating "a higher psychological impact of the situation with regard to COVID-19" (Vanaken et al., 2020). The authors state that the IES-Covid-19 items were largely kept similar to the original 15-item IES, except that references to past events were changed to match present experiences as data collection occurred during the pandemic. By means of confirmatory factor analysis, the factor structure of the IES-COVID-19 was found to be like the original IES. Two latent factors were found, namely, intrusion and avoidance (Vanaken et al., 2020).
There are several concerning matters pertaining to both the original IES and the adapted Covid-19 version that require mention. Firstly, the items are general and can be seen to reflect "variations in normal functioning" (Coyne, 2011). Coyne (2011) has observed that cancer patients have high scores on the IES-R not because of symptoms of traumatisation but as a result of vigilance about new symptoms of their condition. The same argument may be made of persons who are or have been worried about Covid-19 infection or worsening of symptoms, such as loss of taste or difficulty breathing. Thus, the IES may detect vigilance that is appropriate in the context of a pandemic rather than symptoms such as intrusion and rumination.
Secondly, Coyne (2011) argues that the scores on the IES may produce misleading results. Lees-Haley and colleagues asked students to complete the IES with the index stressor being "the worst movie or television show they had seen recently" (Lees-Haley et al., 2001) and found elevated scores typically associated with symptoms of traumatisation. To this end it would appear that the IES may also detect valence-free aspects of events such as memorability or cognitive accessibility rather than trauma (Lees-Haley et al., 2001). A high IES score is thus open to interpretation in more than one way, including reaction to a non-threatening event. Even if infection with Covid-19 is considered a threatening event, the stressor is then fear of infection rather than the Covid-19 pandemic itself. As indicated above, as the pandemic progressed and with new information about the risk of mortality and the introduction of various vaccinations, the threat eventually abated for most people.
The IES also has some ambiguous items. The item "I thought about it when I didn't mean to " is essentially valence free. A thought that occurred unintentionally is not necessarily distressing and this item does not suggest a negative emotion or cognition. The item "I avoided letting myself get upset when I thought about it or was reminded of it" can be interpreted as being a positive experience as becoming upset is avoided. Similarly, the item "I tried to remove it from my thoughts" can also be seen as positive as the noxious stimulus, namely the Covid-19 pandemic, no longer has a distressing effect. The item "I tried not to talk about it" appears to assume that talking about a distressing event is necessarily a positive activity to reduce emotional distress. Yet several studies have shown that psychological expression can have iatrogenic effects. For example, a Cochrane review of 15 trials suggests that critical incident stress debriefing can result in people retaining negative psychological symptoms compared to those who receive no intervention (Rose et al., 1996). Some people may cope better by not speaking about distressing events and speaking about a problem does not in all cases ameliorate distress. Finally, the item "I tried not to think about it" may also be a positive phenomenon. Making attempts not to think about a distressing event may be a positive way of coping. Whether these attempts are successful or not is a separate matter, but success in not thinking about a stressful event is not assessed by the item, only making such an attempt. In sum, the IES as it is applied to the Covid-19 pandemic as an index event may yield information that does not necessarily map onto symptoms of traumatisation as specified in the DSM-5.
In the study by Vanaken et al. (2020) the mean IES-R scores among Belgian students on the IES-Covid-19 were 24.84 in March and 22.02 in April 2020 (Vanaken et al., 2020). Considering the discussion above, these findings should be interpreted with caution as they may not necessarily mean a response to the Covid-19 pandemic as a traumatic event, but instead reflect a way of coping or managing a challenge in living circumstances.
CONCLUDING REMARKS
As has been shown above, both the Traumatic Stress Scale and the Impact of Event Scale Covid-19 are flawed when applied to the Covid-19 pandemic as a traumatic stressor. The items on both measures map imperfectly onto the symptoms of traumatisation as specified in the DSM-5 criteria for posttraumatic stress. Contrary to the argument of Addis (2020), remembering and imagining are discrete cognitive entities. There may be some overlap between these two psychological experiences but remembering requires an event to have occurred in the past whereas imagining does not. Conceptual bracket creep remains a concern for trauma researchers. An ever-widening set of criteria for index stressor risks diluting the concept of trauma so that relatively trivial distressing events may be regarded as traumatic. Specifically, Bridgland and colleagues' modified PTSD Checklist that frames working or studying from home or having reduced working hours as a potential traumatic stressor is likely to be an example of this phenomenon (Bridgland et al., 2021). Such experiences are certainly different in terms of substance and magnitude from intubation or admission to ICU. Thus "Covid-19-related experiences" are not a plausible traumatic stressor in the same way that a threat to physical safety may be. In any case elevated scores on a self-report measure such as the PCL-5 does not mean "PTSD positive" as Bridgeland and colleagues argue, given suboptimal concordance between elevated scores and caseness for the condition.
It is necessary to distinguish between distress and trauma. Distress is usually a time-limited experience that involves emotional discomfort but is ameliorated with social and psychological support or positive coping methods. PTSD is a psychiatric condition that has potentially long-term negative consequences on mental health and quality of life. PTSD symptoms are usually ameliorated with evidence-informed interventions such as exposure therapy. This article argues against conceptualising psychological reactions to the Covid-19 pandemic as traumatic. To do so inappropriately pathologises people who experience normal emotional distress in response to challenges associated with the Covid-19 pandemic. This is a matter for the social work profession to take into account.
Implications for social work practice
As social workers are mental health professionals and provide counselling and mental health services to individuals and families dealing with emotional and psychological problems, it is necessary that the profession appropriately conceptualises Covid-19-related distress in ways that are in keeping with accepted definitions of trauma and thus yield optimal mental health outcomes. To this extent the support and resources provided by social workers to individuals and families should be tailored to meet the actual experiences of people. Social workers can thus assist patients and their families in navigating the healthcare system, including accessing mental health services as these pertain to their needs. In both community and educational settings social workers may support clients and students who have difficulties by means of assessment of their mental health needs rather than an assumption of traumatisation that may be inappropriate. In this way social workers can develop programmes and advocate for policies that address the psychological, social and economic challenges that people experience in the aftermath of the pandemic.
REFERENCES
Addis, D. R. 2020. Mental time travel? A neurocognitive model of event simulation. Review of Philosophy and Psychology, 11, 233-259. [ Links ]
Aiyegbusi, O. L., Hughes, S. E., Turner, G., Rivera, S. C., McMullan, C., Chandan, J. S., Haroon, S., Price, G., Davies, E. H., & Nirantharakumar, K. 2021. Symptoms, complications and management of long COVID: A review. Journal of the Royal Society of Medicine, 114(9): 428-442. [ Links ]
American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders. 5th ed. [Online] Available: https://doi.org/10.1176/appi.books.9780890425596. [ Links ]
Andrews, N., Stowe, J., Kirsebom, F., Toffa, S., Rickeard, T., Gallagher, E., Gower, C., Kall, M., Groves, N. & O'Connell, A. M. 2022. Covid-19 vaccine effectiveness against the Omicron (B. 1.1. 529) variant. New England Journal of Medicine, 386(16): 1532-1546. [ Links ]
Arndt, C., Davies, R., Gabriel, S., Harris, L., Makrelov, K., Robinson, S., Levy, S., Simbanegavi, W., van Seventer, D. & Anderson, L. 2020. Covid-19 lockdowns, income distribution, and food security: An analysis for South Africa. Global Food Security, 26: 100410. [ Links ]
Asimakopoulou, E. & Madianos, M. 2014. The prevalence of Major Depression-PTSD comorbidity among ICU survivors in five general hospitals of Athens: A cross-sectional study. Issues in Mental Health Nursing, 35(12): 954-963. [ Links ]
Asimakopoulou, E. & Madianos, M. 2015. Posttraumatic stress disorder after discharge from intensive care units in greater Athens area. Journal of Trauma Nursing, 22(4): 209-217. [ Links ]
Association, A. P. 2022. Diagnostic and Statistical Manual of Mental Disorders Fifth Edition Text Revision-DSM-5-TR. American Psychiatric Association: Washington, DC, USA. [ Links ]
Boehnlein, J. K. & Kinzie, J. D. 2007. Pharmacologic reduction of CNS noradrenergic activity in PTSD: The case for clonidine and prazosin. Journal of Psychiatric Practice, 13(2): 72-78. [ Links ]
Bridgland, V. M. E., Moeck, E. K., Green, D. M., Swain, T. L., Nayda, D. M., Matson, L. A., Hutchison, N. P. & Takarangi, M. K. T. 2021. Why the COVID-19 pandemic is a traumatic stressor. PloS One, 16(1): e0240146. [ Links ]
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N. & Rubin, G. J. 2020. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227): 912-920. [ Links ]
Ceylan, Z. 2020. Estimation of COVID-19 prevalence in Italy, Spain, and France. Science of The Total Environment, 729:138817. [ Links ]
Coyne, J. C. 2011. Did Americans suffer virtual trauma from television coverage. Psychology Today, The Skeptical Sleuth. [Online] Available: https://www.psychologytoday.com/us/blog/the-skeptical-sleuth/201109/september-11-2001-did-americans-suffer-virtual-trauma-from [ Links ]
CSSE: Center for Systems Science and Engineering. 2022. Covid 19 Dashboard. CSSE: Center for Systems Science and Engineering. [Online] Available: https://www.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6 [ Links ]
Fan, S., Guan, J., Cao, L., Wang, M., Zhao, H., Chen, L. & Yan, L. 2021. Psychological effects caused by COVID-19 pandemic on pregnant women: A systematic review with meta-analysis. Asian Journal of Psychiatry, 56: 102533. [ Links ]
Foa, E. B. & Kozak, M. J. 1986. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1): 20. [ Links ]
Gill, P. K., Du, C., Khan, F., Karimi, N., Sabharwal, K. & Agarwal, M. 2022. The psychological effects of COVID-19 spread in young Canadian adults. International Journal of Social Psychiatry, 68(1): 216-222. [ Links ]
Girard, T. D., Shintani, A. K., Jackson, J. C., Gordon, S. M., Pun, B. T., Henderson, M. S., Dittus, R. S., Bernard, G. R. & Ely, E. W. 2007. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: A prospective cohort study. Critical Care, 11(1): 1-8. [ Links ]
Gloster, A. T., Lamnisos, D., Lubenko, J., Presti, G., Squatrito, V., Constantinou, M., Nicolaou, C., Papacostas, S., Aydın, G. & Chong, Y. Y. 2020. Impact of COVID-19 pandemic on mental health: An international study. PloS One, 15(12): e0244809. [ Links ]
Hembree, E. A. & Foa, E. B. 2000. Posttraumatic stress disorder: Psychological factors and psychosocial interventions. Journal of Clinical Psychiatry, 61, 33-39. [ Links ]
Horesh, D. & Brown, A. D. 2020. Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4): 331. [ Links ]
Janoff-Bulman, R. 1989. Assumptive worlds and the stress of traumatic events: Applications of the schema construct. Social Cognition, 7(2): 113-136. [ Links ]
Jones, C., Griffiths, R. D., Humphris, G. & Skirrow, P. M. 2001. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Critical Care Medicine, 29(3): 573-580. [ Links ]
Jordan, R. E., Adab, P. & Cheng, K. 2020. Covid-19: risk factors for severe disease and death. In Bmj (Vol. 368). British Medical Journal Publishing Group. BMJ 2020;368:m1198 DOI: 10.1136/bmj.m1198. [ Links ]
Jukes, S., Fowler-Watt, K. & Rees, G. 2022. Reporting the Covid-19 pandemic: Trauma on our own doorstep. Digital Journalism, 10(6): 997-1014. [ Links ]
Kagee, A., Bantjes, J., Saal, W. & Sterley, A. 2022. Predicting posttraumatic stress disorder caseness using the PTSD Checklist for DSM-5 among patients receiving care for HIV. Journal of Traumatic Stress, 35(1): 13-21. [ Links ]
Kira, I. A., Shuwiekh, H. A. M., Ashby, J. S., Elwakeel, S. A., Alhuwailah, A., Sous, M. S. F., Baali, S. B. A., Azdaou, C., Oliemat, E. M. & Jamil, H. J. 2021. The impact of COVID-19 traumatic stressors on mental health: Is COVID-19 a new trauma type. International Journal of Mental Health and Addiction, 21(1): 51-70. [ Links ]
Lees-Haley, P. R., Price, J. R., Williams, C. W. & Betz, B. P. 2001. Use of the Impact of Events Scale in the assessment of emotional distress and PTSD may produce misleading results. Journal of Forensic Neuropsychology, 2(2): 45-52. [ Links ]
Martínez-Caballero, C. M., Cárdaba-García, R. M., Varas-Manovel, R., García-Sanz, L. M., Martínez-Piedra, J., Fernández-Carbajo, J. J., Pérez-Pérez, L., Madrigal-Fernández, M. A., Barba-Pérez, M. Á., Olea, E., Durantez-Fernández, C. & Herrero-Frutos, M. T. 2021. Analyzing the impact of COVID-19 trauma on developing post-traumatic stress disorder among emergency medical workers in Spain. International Journal of Environmental Research and Public Health, 18(17): 9132. https://doi.org/10.3390/ijerph18179132 [ Links ]
Masiero, M., Mazzocco, K., Harnois, C., Cropley, M. & Pravettoni, G. 2020. From individual to social trauma: Sources of everyday trauma in Italy, the US and UK during the COVID-19 pandemic. Journal of Trauma & Dissociation, 21(5): 513-519. [ Links ]
McKibbin, W. & Fernando, R. 2020. The economic impact of COVID-19. In: Baldwin, R. & Weder di Mauro, B. (eds.). Economics in the Time of COVID-19. (Vol. 45). CEPR Press Centre for Economic Policy Research London. [ Links ]
McNally, R. J. 2006. The expanding empire of posttraumatic stress disorder. Medscape General Medicine, 8(2): 9. [ Links ]
Möhlenkamp, S. & Thiele, H. 2020. Ventilation of COVID-19 patients in intensive care units. Herz, 45(4): 329-331. [ Links ]
Muñoz-Navarro, R., Malonda, E., Llorca-Mestre, A., Cano-Vindel, A. & Fernández-Berrocal, P. 2021. Worry about COVID-19 contagion and general anxiety: Moderation and mediation effects of cognitive emotion regulation. Journal of Psychiatric Research, 137: 311-318. [ Links ]
Norrholm, S. D., Zalta, A., Zoellner, L., Powers, A., Tull, M. T., Reist, C., Schnurr, P. P., Weather, F. & Friedman, M. J. 2021. Does COVID-19 count? Defining Criterion A trauma for diagnosing PTSD during a global crisis. Depression and Anxiety, 38(9): 882-885. [ Links ]
Ornell, F., Schuch, J. B., Sordi, A. O. & Kessler, F. H. P. 2020. "Pandemic fear" and COVID-19: Mental health burden and strategies. Brazilian Journal of Psychiatry, 42: 232-235. [ Links ]
Patel, M. B., Jackson, J. C., Morandi, A., Girard, T. D., Hughes, C. G., Thompson, J. L., ... & Pandharipande, P. P. 2016. Incidence and risk factors for intensive care unit-related post-traumatic stress disorder in veterans and civilians. American Journal of Respiratory and Critical Care Medicine, 193(12): 1373-1381. [ Links ]
Rose, S. C., Bisson, J., Churchill, R., Wessely, S. & Group, C. C. M. D. 1996. Psychological debriefing for preventing post-traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews, 2010(1). [ Links ]
Rudan, I., Adeloye, D. & Sheikh, A. 2022. COVID-19: Vaccines, efficacy and effects on variants. Current Opinion in Pulmonary Medicine, 28(3): 180-191. [ Links ]
Shevlin, M., McBride, O., Murphy, J., Miller, J. G., Hartman, T. K., Levita, L., Mason, L., Martinez, A. P., McKay, R. & Stocks, T. V. A. 2020. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open, 6(6): e125. [ Links ]
Smith, P. O. & Suda, K. T. 1999. Mowrer's two factor model: Applications to disaster mental health services. Traumatology, 5(2): 26-32. [ Links ]
Struyf, T., Deeks, J. J., Dinnes, J., Takwoingi, Y., Davenport, C., Leeflang, M. M. G., Spijker, R., Hooft, L., Emperador, D. & Domen, J. 2022. Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19. Cochrane Database of Systematic Reviews, 5(5): CD013665. Doi: 10.1002/14651858.CD013665.pub3. [ Links ]
Taylor, S., Landry, C. A., Paluszek, M. M., Fergus, T. A., McKay, D. & Asmundson, G. J. G. 2020. Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders, 72:102232. https://doi.org/10.1016/j.janxdis.2020.102232 [ Links ]
Vanaken, L., Scheveneels, S., Belmans, E. & Hermans, D. 2020. Validation of the impact of event scale with modifications for COVID-19 (IES-COVID19). Frontiers in Psychiatry, 11: 738. [ Links ]
World Health Organization. 2019. International Classification of Diseases, Eleventh Revision (ICD-11), (WHO) 2019/2021. [Online] Available: https://icd.who.int/browse11. [ Links ]
Yong, S. J. 2021. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infectious Diseases, 53(10): 737-754. [ Links ]
Article received: 05/07/2023
Article accepted: 18/08/2023
Article published: 26/03/2024
AUTHOR BIOGRAPHY
Ashraf Kagee is a Distinguished Professor of Psychology and co-director of the Alan Fisher Centre for Public Mental Health. He previously served as a member of a World Health Organisation working group to develop diagnostic guidelines on stress-related disorders for the International Classification of Diseases 11th Edition. He developed the ideas for this paper after the Covid-19 pandemic.














