Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Onderstepoort Journal of Veterinary Research
On-line version ISSN 2219-0635
Print version ISSN 0030-2465
Onderstepoort j. vet. res. vol.81 n.2 Pretoria Feb. 2014
PROCEEDINGS
The quest for One Health: Human Resource training aspects
Angwara Kiwara; Ave-Maria Semakafu; Gasto Frumence
School of Public Health and Social Sciences, Muhimbili University of Health and Allied Sciences, Tanzania
ABSTRACT
Appropriately trained Human Resources for Health (HRH) are key inputs into One Health. '... more than 50% of all infectious diseases of humans originate from animals and that, of the emerging diseases about 75% could be traced back to animal origin' (Rweyemamu et al. 2006). A comprehensive understanding of the social determinants of health, through an appropriate training model for HRH, is a key input. This study aimed to explore if human and veterinary medical schools were using such a model or providing time for this model in their curricula. Specific objectives were to: determine the time that human and veterinary medical schools' curricula provide for subjects or courses related to the social determinants of health; analyse the curricula contents to establish how they relate to the social determinants of health; and explore how a bio-medical model may influence the graduates' understanding and practice of One Health. A review of human and veterinary graduate-level medical schools' curricula in East Africa was performed in April 2013 and May 2013. The findings were: in the curricula, SDH contents for knowledge enhancement about One Health are minimal and that teaching is Germ Theory model-driven and partisan. Out of the total training time for physicians and veterinarians, less than 10% was provided for the social determinants of health-related courses. In conclusion, the curricula and training times provided are inadequate for graduates to fully understand the social determinants of health and their role in One Health. Furthermore, the Germ Theory model that has been adopted addresses secondary causes and is inappropriate. There is a need for more in-depth model. This article suggests that a vicious cycle of ill-health model must be taught.
Introduction
International Public Health experts are now focusing their attention on innovative ways of realising better health in all countries through an improved framework; this is because previous approaches have not delivered the expected results (Solar et al. 2010; WHO 2010). Despite sustained efforts by health experts and policy makers, ill health still exists for both animals and humans (WHO 2006). The One Health approach has overwhelmed most of the debates (Coker et al. 2011). These debates are justified given that 'it has been established that more than 50% of all infectious diseases of humans originate from animals and that of the emerging diseases about 75% could be traced back to animal origin,' (Rweyemamu et al. 2006). It is further argued, and plausibly so, that the social and environmental ecology drives the social determinants of health, which researches have proven over time to be of primary importance in both animal and human health (WHO 2006; World Bank 2010).
Objectives
This article sought to contribute to an important aspect of enriching a One Health approach, with a specific focus on analysing the key aspects of the training of health workers. It set out to specifically:
• Determine the time that human and veterinary medical schools' curricula provide for subjects or courses related to the social determinants of health (SDH).
• Analyse curricula contents and how they relate to the SDH.
• Examine how the curricula contents may influence the graduates' understanding and practice of One Health.
Methodology and marterials
The curricula of five university-level human and veterinary medical schools in East Africa were reviewed. The aim was to establish how much time was allocated to courses related to the SDH taught at the medical schools. These courses included: Nutrition, Community health sociology and Development studies. Other courses included the classical subjects at medical and veterinary schools such as: Parasitology; Microbiology; Virology; Pathology; Pharmacology; and Management of diseases. Current curricula were obtained from the respective universities and schools in the region and analysed by desk review. The total times provided for the SDH-related subjects (Nutrition, Community health sociology and Development studies) were compiled. Likewise, the total times provided for the classical subjects were compiled. A thorough examination of the classical subjects was undertaken to decipher and categorise the contents as to whether they were related in any way with the SDH. Finally, ten group discussions were held with final-year veterinary and human medicine students in conveniently selected schools.
For the focus-group discussions, three questions guided the discussions. These questions were:
• How do you understand One Health?
• Would you work as one team after graduation?
• Would you facilitate joint training if you had the means to do so?
Results
It was established that students studying to become physicians or veterinarians spend on average ten semesters at university. This totals 6382 hours; out of this time, only 639 hours or 10% is spent on subjects that are directly related to the SDH. The rest of the time is spent on the classical subjects. Compartmentalisation and isolated, specific moulding takes place very early on before the graduate goes out to practice.
It was also established that the contents of the classical subjects present microorganisms to be the primary causes of ill health in animals and human beings. Students are taught that these microorganisms exist and act in their own right, independent of the social and environmental ecology, to cause ill health. They are taught that the direct management of these microorganisms can overcome the problem of ill health in animals with disregard to the social and environmental ecology. Given the established compartmentalisation during training and the disregard for the social and environmental ecology, One Health is thus seriously threatened.
The curricula of the veterinary and medical schools put the Germ Theory Model as the lead model in the training of veterinarians and human medical doctors. This centralisation is not in favour of a One Health approach. It also creates and reinforces the fatal culture among medical and veterinary students of despising social sciences as a tool in One Health. Furthermore, it has come to acquire unquestionable legitimacy in dealing with diseases in both human beings and animals for reasons to be further raised below.
During the focus group discussions, responses were transcribed and themes grouped together in a qualitative analysis. It was established that the final-year human and animal health students at the institutions studied minimally understand One Health. All of the ten focus group discussions had similar conclusions. In an attempt to search deeper, written explanations about what One Health meant were given to all groups.
Regarding working as one team for One Health, the responses were mixed. These future animal and human health experts were of the view that such collective work should be done during epidemic outbreaks affecting human beings and animals. Otherwise they see themselves as holding specific authorities, each in their own discipline and area of work.
In relation to joint training, where certain core courses like Anatomy and Physiology are provided on one campus and in one school with provision for separate training in senior years, the views were very clear. The position was that no joint training can or should be done. It seems that stereotypes have already caught up with the future animal and human health experts.
Discussion
Appropriately trained Human Resources for Health - a critical input in One Health
Sub-Saharan African countries are locked up in a fatal dilemma. They have a double-hump epidemiological transition (WHO 2006). Unlike the developed world, they have the increasing problem of non-communicable diseases whilst still suffering from high levels of infectious diseases. The high burden of infectious diseases is more than 50% of animal origin (Rweyemamu et al. 2006). This is why the region's HRH need to be trained with this fact born in mind. That is why, more than in any other region of the world, One Health matters most in Sub-Saharan Africa and needs to be strengthened (WHO 2008). What are the issues?
Infectious Diseases: the Future Report (2006) noted that critical issues in Sub-Saharan Africa include an overwhelming presence of infectious diseases in the region, which poses a serious threat to the lives of both animals and humans (Rweyemamu et al. 2006). These diseases attack humans and animals, causing morbidity, mortality and death from starvation. The implications of this, in the form of economic losses, social instability and a resultant downward spiral in livelihood, are immediate (Brazier et al. 2007). Ultimately, these countries are locked in a vicious cycle of poverty that is hard to escape from. This has serious economic and health implications given the fact that livestock agriculture represents 25% of the region's Gross Domestic Product (Rweyemamu et al. 2006).
Both the economic and political reforms that have taken place in the region have worsened the spread of contagious diseases affecting both animals and humans. For example, the structural adjustment programmes have intensified movement of both humans and animals in the region, making it easier for infections to spread faster and further. Larger-scale farming activities have been extended to new areas, increasing contact with wild stock and the possibility of new and fatal infections (World Bank 2010). Documented examples include Ebola and a variety of hemorrhagic fevers.
The direct effects of zoonoses and multiplicity of other diseases among animals and humans, who are continuously interacting, has lead to the economic and social decline. Understanding the importance of these factors by health workers, among others, is necessary in the quest for One Health in the region (Winding 2007).
Civil wars and refugee crises have been driven by poor governance and have displaced large numbers of animals and humans into remote areas. At such times, control of movement is not possible. This facilitates spread of infectious diseases from one area to another and from animals to humans. Under such conditions, infectious diseases of animal origin easily spread among the human population because of poor hygiene, over congestion, poor nutrition and lack of proper accommodation (Drummond et al. 2005).
A deepened understanding of the direct effects of HRH practices is necessary in both animal and human health. Such practices include irrational prescription of antibiotics. This leads to emergence of resistant microorganisms. The many unregistered pharmaceutical outlets in the region and the use of incomplete doses enhance this practice (Rweyemamu 2006). Due to liberalisation of the economy, uncontrolled importation and sale of drugs is widespread. These drugs are often ineffective because they lack the active ingredients that are necessary. Others have expired, but they are sold for use to uninformed consumers. In both instances, emergence of resistant organisms is a consequence. The resulting prolonged morbidity has a negative impact on the economy.
Many systemic factors have contributed substantially to a decline of both animal and human health, thus minimising the chances of realising One Health. They are:
• Weak health care systems, which cannot perform proper diagnosis and disease management.
• Weak rural economies, which tend to push people to migrate to urban areas where life without employment and income is a recipe for behaviours that may lead to drug use and sexually transmitted infections, including HIV and AIDS.
• Inadequate government budgets, which are often dependent on development partner support. This may have unfavourable conditionality or may not be received as expected.
• Weak government-level veterinary services, which are mainly available in urban areas where demand is higher.
• Frequent policy and structural changes.
• Uncontrolled animal movement within the country or from neighbouring countries.
For the East African region this last factor is a major threat. Each year, wild animals move across the national boundaries in large numbers. Likewise, pastoralists migrate across the region looking for better pastures for their livestock. These movements facilitate movement of old and new pathogens (Rweyemamu et al. 2006)
Why consideration of social determinants of health matter - lessons for One Health
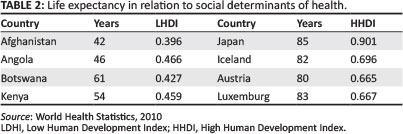
The training of HRH for One Health must facilitate an objective understanding of One Health and health in general as a multisectoral or multifactorial product of the interplay of socio-economic factors. Such understanding will enable the trained HRH to objectively appreciate that establishment of One Health is driven by human behaviour, social policies, economics, culture and more. The best tool that indicates the role of SDH in health is the Human development index. The Human development index (HDI) is a tool developed by the United Nations to measure and rank countries' levels of social and economic development (WHO 2010). The direct link between socio-economic factors and health is clearly indicated when life expectancy and maternal mortality rates are examined in countries ranked by HDI (Table 1). The results of such ranking are indicated in the tables below.

The analysis of life expectancy and maternal mortality rate in different countries has shown that the higher the HDI (favourable socio-economic conditions), the lower the maternal mortality rate (Table 2). Likewise, the higher it is, the higher the life expectancy. On the other hand, the lower the HDI (unfavourable socioeconomic conditions), the higher the maternal mortality rate and the lower the life expectancy.
Production of Human Resource for Health-appropriate training models
Cocker et al. (2011) and Solar et al. (2010) concurred with the findings of this research that an appropriate model for the training of Human Resources for One Health is necessary and must draw its contents from a multisectoral framework. This premise is a key factor, which determines how effective the produced human resources will be after training as a One Health core team. A major prerequisite, however, is the presence of political will - this will enable the training centres, particularly those at the higher levels, to get enough funds to guide development of appropriate training models that they can implement. The models developed should be able to respond to the needs of One Health in specific situations. An effective HRH must be prepared to understand the primary causes rendering the concept and practice of One Health to be marginalised. As the curricula analysis above showed, only 10% of the training time is related to social determinants of disease. An attempt will now be made to unravel this puzzle by revisiting the origins of the Germ Theory of disease.
The Germ Theory model
For centuries, this model has dominated conceptualisation of disease, approach to curing disease and, particularly, what is taught at medical and veterinary schools. It is interesting to note the span of years over which the germ theory has remained a leading model in the training of health care professionals despite its lack of objectivity and dynamism as a major shortcoming. This shortcoming is proven by the epidemiological transition, which has manifested itself in the developed world where infectious diseases have been controlled. This phenomenon deserves urgent scientific enquiry. Training through this model focuses on managing isolated episodes of animal or human illness. The view that any particular episode is not independent of the social or environmental ecology is not considered. Treatment of cholera, for example, is by administering antibiotics and other drugs. A primary solution, like improvement of hygiene through better water supplies, which is a lasting solution, is emphasised the least by most clinical physicians and often it is not even included in the management plan. Likewise, the treatment of trypanosomiasis invariably does not consider the environmental ecology.
The Germ Theory, however, has left the developing countries with a legacy of the 'magic bullets' (antibiotics and other drugs) as a 'panacea' to diseases that are purely of social origin. The problem is not only the legacy but also the production of professionals who cannot conceptualise illness within its social context and so, in turn, empower the affected population to become healthier through appropriate advocacy of social approaches. The Germ Theory has deep roots: briefly, it was founded in two epochs: the race for the Germ Theory and what has been termed as the beginning of a new era, which is briefly revisited below.
The race for the Germ Theory
Before James Henle's 1840 essay on 'Miasmata and Contagion', in which he formulated the modern germ theory, understanding of ill health or disease was speculative and predominantly secular (Barry 2005). At the beginning of 500 BC, medicine became largely secular. It was believed that disease was an outcome of some imbalance in the body and that balance could be restored by intervention (Warner 1992). This speculative era was replaced as society became more inquisitive.
The beginning of a new era
By 1500, methods of medicine were challenged. Parcelius declared investigation of nature 'Not by following that which the old taught, but by our own observation of nature, confirmed by experiment and by reasoning thereon' (Barry 2005). Later, Vaselius dissected human corpses and concluded that Galen's findings had come from animals and were flawed (Barry 2005). Fracastorius hypothesised that diseases had specific causes and that contagion passes from one thing to another and is originally caused by infection of the imperceptible particle'. In 1628, came Edward Jenner's work with cowpox on vaccination and immunisations. These were major landmarks in human and veterinary medicine (Barry 2005).
In 1860, Pasteur proved that living things, not a chemical reaction, caused fermentation (Warner 1992). The proof of Pasteur's work was by Joseph Lister who applied these findings to surgery. Subsequently, Robert Koch's groundbreaking work established the complete life circle of the anthrax bacillus, which showed that it formed spores that could lie dormant in the soil for years. In 1882, Koch's discovery of the tubercle bacillus - the cause of tuberculosis in animals and human beings - further confirmed the Germ Theory. Later on in early 1900, while working at Ocean Road Hospital in Tanzania, Koch discovered the malaria parasite for the first time (Richard et al. 1964). These events and breakthroughs gave the Germ Theory authenticity and unprecedented power. What was theory became 'fact', the social origin of disease paradigm lost face and it suffered a major convulsion. The discovery of antibiotics incarcerated almost irreversibly the idea that social and environmental ecology were the primary origins of ill health in animals and humans.
Antibiotics
With the discovery of antibiotics in the 1940s and their effect on infections, the Germ Theory attained an unprecedented authority and power. The dramatic effects of antibiotic prescriptions (penicillin and sulpha drugs) on syphilis, yaws, anthrax and other infections gave the theory fame and outright acceptance as the answer to 'all diseases'. Unquestionably, it assumed a central position in the health care professional's training. The 'magic' power of antibiotics cast darkness on the sanitary movement, the epidemiological transition and emerging lessons.
The epidemiological transition and unlearned lessons
As the Germ Theory evolved, great lessons of public health importance accumulated. The sanitary movement matured in England through its impact in reducing morbidity and mortality caused by the Black Death and cholera epidemics (Basch 1999). Virchow publicly advocated that medicine (in animals and humans) was a social science and that medical professionals and veterinarians needed to have social science knowledge (Basch 1999). Chadwick was literally prosecuted for standing behind the sanitary revolution in England. McKeon wrote prolifically about how the decline in morbidity and mortality preceded the advent of antibiotics and other curative work (McKeown et al. 1974). It is a small wonder how the training of health professionals has managed to marginalise these lessons and focus almost exclusively on the Germ Theory as a major tool in training. The Germ Theory is ill informed and is turned upside down by the realities of the epidemiological transition. In this transition many societies have overcome infectious diseases (bacterial, viral or parasitic) through socio-economic measures. They are now confronted by non-communicable diseases, which the Germ Theory cannot understand. Given these developments, the Germ Theory should have suffered its first fatal convulsion, however, it did not. What is the way out of this impasse? A proposal is presented below.
A proposed new model for the training of veterinarians and medical doctors
The most frequent human health problems, in both the developed and developing countries, have social determinants as their primary cause. Typically, the top five disease categories in the developing countries include: infectious diseases (bacterial, parasitic, viral or fungal); nutrition-related diseases; drugs; alcoholism; and degenerative disorders (diabetes, cancers or cardiovascular diseases). All of these have social determinants as their primary cause. In the developed world, the major categories of diseases in order of importance are: degenerative disorders (cancers, work-related health problems, heart diseases and diabetes); road traffic accidents; alcoholism; and suicide. These also have social determinants as their primary causes. Likewise, major veterinary challenges in the developing countries, such as foot-and-mouth disease, rinderpest (controlled, but with recurrences), tick fever, trypanosomiasis, rabies, rift valley fever, anthrax and bovine tuberculosis have policy-related, social and environmental ecology as their primary factors. If these are not understood One Health will be a mirage.
As such, the proposed training model must clearly show that social determinants of health are the primary cause of health or ill health. At the same time, the curricula in medical and veterinary schools need to build capacity for all health workers to understand health and ill health in that context and that micro organisms, as presented by the Germ Theory, are secondary causes. Such a model must show a dynamic link between social determinants and health or ill health. It must also show, within the dynamic process, the role of the Germ Theory model-produced professionals and its outcomes, such as the vicious cycle of ill-health, chronic ill-health and death.
What is the essence of this model?
The model, as shown in Figure 1, shows that those who succumb to ill health often adopt a wait-and-see approach or self medicate. This happens for both livestock and human illnesses. Eventually when it does not work they consult health care experts. The health care experts under their Germ Theory training provide prescriptions for medications like antibiotics. Some of the animals or patients recover, but some will acquire a chronic status and others will die. Those animals that recover often survive on low scale morbidity and are a liability to farmers because their productivity (milk, meat, eggs) is low and are not good for nutrition or the market. These intensify the downward spiral of poverty. For humans, those who respond to medication are discharged out of the management regime and resume life in the society where they caught the previous ill-health problem. Because the social determinants of health, which caused the previous ill-health problem, are still unaddressed, those who were cured by the antimalarials or antibiotics, for example, and even many more new ones, will become sick again and get locked up in the vicious cycle of ill health. The diagram below illustrates this movement in a cycle, as determined by exposure to social determinants of health for both animals and humans.

This suggested training model will strongly underline that analysis and understanding of health and disease by all health professionals not only public health professionals, at all levels of training, is essential. It must begin with a detailed understanding of the social determinants of health (SDH) - society, social relations, economic well-being - and the development trends, as the primary causes of disease or ill health. Bacteria, parasites, viruses and more are only secondary causes of ill health. The struggles focused at vertical elimination of bacteria, viruses and parasites through use of drugs alone have not succeeded anywhere and no country in the world has done this to date or should ever do it in future.
Health workers count
Due to the immense power bestowed on them by society and their acceptability, health care professionals in human medicine and veterinarians can be significant advocates of social change. These professionals, through the model above, can be trained to understand that the majority of ill-health is due to SDH and that it is possible to change society so that ill-health becomes history. A number of countries have controlled rinderpest or malaria because they have been able to nurture political will and intervene through social determinants, and made it possible for universal accessibility so that such diseases have been controlled. A voice coming from medical doctors and veterinarians will reach many individuals in the consultation room, households and communities within this context and break the vicious cycle of ill health through favourable SDH (Figure 2). By intervening at the level of social determinants of health, as the cycle in the diagram below shows, more and more will remain healthy and ill health will be minimised.

Conclusion
For a long time it has been assumed that the graduate HRH would productively take the role in realisation of One Health. However, the nature of their knowledge on the link between SDH and animal or human health and how the medical schools shape this knowledge has been a grey area and given minimum attention.
The curriculum review referred to above has shown that the medical and veterinary schools use the Germ Theory model in training. This model, however, does not facilitate a deep understanding of the importance of SDH in healthcare, and the courses related to SDH are provided by only 10% of the graduates' training time.
The level of impact of HRH on One Health will be determined by how veterinarians and human medicine professionals comprehensively understand the social determinants of health as the primary causes of ill health or health. The model used in training affects this understanding. The Germ Theory presents microorganisms as the primary causes of ill health. However, the microorganisms are outcomes of the social and environmental ecology. These outcomes are rife in the developing world and can only be fully understood by HRH who have been trained on the vicious cycle of ill health. Such health workers will be the agents for change, as they will be able to objectively empower individuals and communities to actively participate in pursuit and defence of their own health and that of animals.
This study recommends the vicious cycle of ill health as a model with which to enrich training of HRH in order to enable better performance in One Health.
Acknowledgements
The authors thank the Swedish International Development Agency for providing the required support to undertake the fieldwork, which has led to this article. They also thank the Muhimbili University of Health and Social Sciences for giving them time from their regular activities to undertake this review.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
A.W., A-M.S. and G.F. (all from Muhimbili University of Health and Allied Sciences) jointly guided preparation of research tools, supervised data collection, analysis and manuscript preparation.
References
Barry, J.M., 2005, The Great Influenza, The story of the deadliest Pandemic in History, Penguin Books, New York. [ Links ]
Basch, P.F., 1999, Textbook of International Health, Oxford University Press, New York. [ Links ]
Brazier, J., Ratcliffe, J., Salomon, J.A. & Tsutchiya, A., 2007, Measuring and Valuing health benefits for economic evaluation, Oxford University Press, Oxford. [ Links ]
Coker, R., Rushton, R., Mounier-Jack, S., Karimuribo, R., Lutumba, P., Kambarage, D. et al., 2011, 'Towards a conceptual framework to support one-health research for policy on emerging zoonoses' The Lancet Infectious Diseases 11, 326-331. [ Links ]
Drummond, M.F., Sculpher, M.J., Torrace, G.W., O'Brien, B.J. & Stoddart, G.L., 2005, Methods for the economic evaluation of health care programmes, 3rd edn., Oxford University Press, Oxford. [ Links ]
McKeown, T. & Lowe, C.R. (eds.), 1974, An Introduction to Social Medicine, 2nd edn., Blackwell Scientific, Oxford. [ Links ]
Richard, M., Titmuss, Abel-Smith, B., Macdonald, G., William, A. & Wood, C., 1964, The Health Services of Tanganyika, Pitman Medical Publishing Company, London. [ Links ]
Solar, O. & Irwin, A., 2010, Conceptual framework for action on the Social determinants of health, Discussion Paper two (Policy and Practice), WHO, Geneva, Switzerland. [ Links ]
Rweyemamu, M., Otim-Nape, W. & Serwadda, D., 2006, Foresight: Infectious Diseases: Preparing for the Future Africa, Office of Science and Innovation, London. [ Links ]
Warner, J.H., 1992, The Fall and Rise of Professional Mystery in Laboratory Revolution in Medicine, Penguin Publishers, New York. [ Links ]
Winding, W., 2007, 'One health: Pulling animal health and public health together', Federation of Veterinarians of Europe, viewed 30 May 2011, from http://search.babylon.com/?q=%E2%80%9COne+Health%E2%80%9D+pulling+Animal+ Heal th+and+Public+Health+together+Brussels%2C+3+October+2007&babsrc=HP_ ss&s=web&as=0. [ Links ]
WHO, 2006a, 'The control of neglected zoonotic diseases: A route to poverty alleviation', in Report of a Joint WHO/DFID-AHP Meeting with the Participation of FAO and OIE, Geneva, 20-21 September, viewed 31 May 2013, from http://whqlibdoc.who.int/publications/2006/9789241594301_eng.pdf [ Links ]
WHO, 2008, 'Closing the gap in a generation: Health equity through action on the social determinants of health', in Final Report of the Commission on Social Determinants of Health, WHO and Commission on Social Determinants of Health, Geneva. [ Links ]
WHO, 2010, 'World Health Statistics 2010' viewed 27 June 2013, from http://www.who.int/whosis/whostat/EN_WHS10_Full.pdf [ Links ]
World Bank, 2010, People, Pathogens and our Planet, Volume 1: Towards a One Health Approach for Controlling Zoonotic Diseases. Report No. 50833-Glb, World Bank: Agriculture and rural development health, nutrition and population, Washington DC, viewed 27 June 2013, from http://siteresources.worldbank.org/INTARD/Resources/PPP_Web.pdf [ Links ]
 Correspondence:
Correspondence:
Angwara Kiwara
PO Box 35147
Dar-es-Salaam, Tanzania
angwarakiwara@yahoo.com
Note: Proceedings of the 2nd One Health Conference in Africa. Jointly organised by the Southern African Centre for Infectious Disease Surveillance and the Tanzania National Institute for Medical Research, held at the Snow Crest Hotel in Arusha, Tanzania from 16th to 19th April 2013: http://www.sacids.org/kms/frontend/index.php?m=119.














