Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.79 n.1 Johannesburg Feb. 2024
http://dx.doi.org/10.17159/sadj.v79i01.16863
RESEARCH
https://doi.org/10.17159/sadj.v79i01.16863
Root and canal morphology of the maxillary first molar: A micro-computed tomography-focused review of literature with illustrative cases. Part 1: External root morphology
CH JonkerI; PJ van der VyverII; AC OettléIII
IBChD, Dip Odont (Endo), MSc (Endo), PGCert (ClinEd), AFHEA, PhD student in Anatomy (University of Pretoria), Faculty of Health, Peninsula Dental School, University of Plymouth Ground, Truro Dental Education Facility, Knowledge Spa, Royal Cornwall Hospital, Truro, UK ORCID: 0000-0002-9110-5208
IIBChD, PG Dip Dent (Endo), PG Dip Dent (Aesthet Dent), MSc, PhD, Department of Odontology, School of Dentistry, School of Health Sciences, University of Pretoria, Pretoria 0031, South Africa ORCID: 0000-0003-1951-6042
IIIPhD, Department of Anatomy and Histology, School of Medicine, Sefako Makgatho Health Sciences University, Pretoria, South Africa ORCID: 0000-0002-9389-057X
ABSTRACT
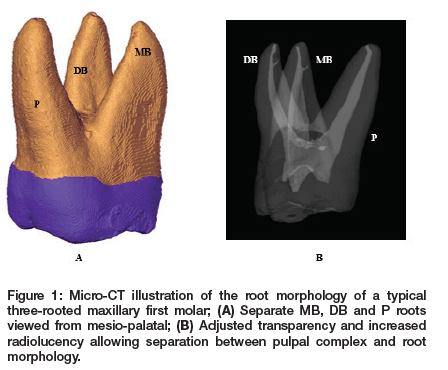
Cleaning and shaping of the root canal are profoundly affected by the complexity of root and canal morphology. Undiscovered roots or canals may lead to a reduced prognosis of a treated tooth as hidden causative organisms and their by-products can cause re-infection. Most maxillary first molars have three roots, namely mesio-buccal (MB), disto-buccal (DB) and palatal (P). They can be separate or fused, with incidences varying between populations. Anomalies have also been documented that include single-rooted, double-rooted, four and even five-rooted teeth. Additional roots are mostly in the form of additional palatal roots and are known as either a radix mesiolingualis (RML) or radix distolingualis (RDL). This paper is the first of two giving an overview, focused on micro-CT, of available literature on various aspects of the root and canal morphology of the maxillary first permanent molar. The aim of this paper is to provide an overview of relevant aspects of the external root morphology in different populations. The content is supported by illustrative micro-CT images and case reports of rare morphological findings on maxillary first molars.
Keywords: Micro-CT, number of roots, radix mesiolingualis, radix distolingualis, root fusion, taurodontism
INTRODUCTION
Once a tooth becomes irreversibly inflamed, endodontic treatment is required. This involves removing infected tissues from the root canal system in a series of mechanical and chemical disinfection steps and eventual three-dimensional sealing of the prepared root canal spaces.1,2 Cleaning and shaping of the root canal are profoundly affected by the complexity of root and canal morphology. Undiscovered roots or canals may lead to a reduced prognosis of a treated tooth, as causative organisms and their by-products can cause re-infection.2,3 n addition to a complex internal structure, the external morphology of this tooth can be bizarre. In most cases, three roots are present: mesio-buccal (MB), disto-buccal (DB) and palatal (P).4 Roots can be separate or fused, with incidences varying between populations.5-9 Variations in the number of roots have also been noted, including single-rooted, double-rooted,10-12 four and even five-rooted teeth13,14 These additional roots are mostly palatal.14
Recent technological developments, such as cone-beam tomography (CBCT) and micro-computed tomography (micro-CT), have made it possible to identify many of the complexities and anatomical variations of the roots and root canals of molar teeth in three dimensions that were often hidden in the two-dimensional view of conventional radiographs.15-17 More specifically, micro-CT enables the observation of fine detail and the identification of complexities in a segmentation process known as the watershed. During segmentation each component of a tooth is virtually separated from the others using modern software (for example Avizo18). Different colours can be assigned to enamel, dentine or the pulp, images can be magnified, and a tooth can be rotated in multiple planes18-20
The aim of this paper is to provide an overview of available literature on the external root morphology of the maxillary first molar, supported by illustrative clinical cases and micro-CT images. Studies have identified several investigative methodologies, and morphological findings differ from population to population. However, the focus is on micro-CT reports.
Number of roots
Several papers report on the number of roots in different populations and, in most, CBCT was used. The consensus is that the maxillary first molar has predominantly three roots but variations, including root fusions, have also been noted.5,21-26 Many authors have described the number of roots in different populations, which vary between one, two, three or four-rooted first molars. Findings from available literature are shown in Table I. Figure 1 shows a typical three-rooted maxillary first molar with separated roots viewed through micro-CT and Avizo software. No studies that reported on the number of roots using micro-CT methodology were identified.
Radix mesiolingualis (RML) and radix distolingualis (RDL)
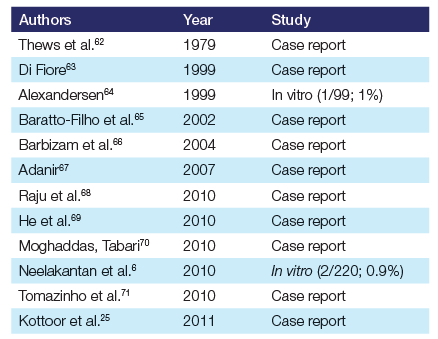
Additional roots can be present on either the mesio-palatal side (RML) or on the disto-palatal side (RDL).13 Most of the reports on RML and RDL are case reports, but there are a few cross-sectional studies investigating the prevalence of RML and RDL. In a Danish study authors found a prevalence of 8.6% of RML in maxillary first molars using visual inspection. No RDL were identified.13 Christie et al.61 observed patients in vivo who displayed additional palatal roots and found a prevalence of 12.5% for a fourth root.61 No studies reporting specifically on the RML or RDL in African or South African populations using micro-CT were identified, but a Ugandan investigation found no teeth with more than three roots. The same was reported in other African or South African populations.5,28,55
Figure 2 illustrates a case report of a South African who presented with a rare case of combined RML and RDL. The patient, a 54-year-old male, presented with irreversible pulpitis on his left maxillary first molar that had previously been restored with a large occlusal amalgam. A periapical radiograph provided limited diagnostic information and no additional roots could be observed between the MP and DB roots. However, CBCT images revealed the presence of two buccal and two palatal roots (RML and RDL). The defective amalgam restoration was removed and the pulp was exposed. Clinically, the crown of the tooth appeared enlarged compared to the contralateral first molar and was asymmetrical in shape. The pulp chamber floor was quadrangular in shape, with four distinct canal orifices arranged in each corner. The mesio-palatal and disto-palatal canal orifices were positioned more mesial and distal to the chamber floor than where a single palatal canal orifice would normally be. The four root canal systems were prepared after determining length and establishing glide path using the ProTaper Universal System (Dentsply Sirona).
Other reports of four-rooted first molars are included in Table II but unfortunately the specifics and location of the fourth root were not given.
Root fusion
Although most maxillary first molars display a separate three-rooted configuration, fusion can occur between some or all the roots. The findings between populations differ. For example, in a Korean study, 0.7% of teeth in the sample displayed root fusion.7 This is similar to the case of a North American population where 0.9% of fusion between roots occurred in the sampled teeth.60 Both these figures are lower than the 2.2% that was observed in a Chinese group.38 In a Portuguese population, a larger number of teeth with fused roots were identified (7.1%).8 Some populations in China, Burma, Iran, Poland and Taiwan had no teeth with fused roots in their samples.6,32,33,48,52,57 The incidence of fusion in other populations is 1.3% in an Iranian population,46 2.1 % in a Greek population,43 0.7% in a Spanish population,56 2.4% in another Iranian population,47 1.4% in China,9 11% in Ireland,50 2.1 % in South China35 and 7% in Saudi Arabia.72 Rwenyonyi et al.5 found fusion in 4.1% of teeth in Uganda. A prevalence of 9% of fused roots was found in a South African study. Unfortunately, no mention is made which population groups were included.55 However, the Ugandan study contained individuals of African descent.5 As South Africans are a diverse group of people it is difficult to make predictions for other groups. Nevertheless, the relatively higher prevalence noted is important to consider in the South African context. CBCT was the method used in most investigations, while micro-CT studies were limited (if any). Figure 3 shows a maxillary first molar that was isolated by segmentation using Avizo from a South African individual of African descent.
Figure 4 illustrates a case report of a 38-year-old South African female who presented with a non-vital right maxillary first molar with a large periapical radiolucency. A highresolution CBCT scan revealed that the distobuccal and palatal roots were fused. The fused root contained two root canal systems that joined into one large apical foramen in the apical third of the root and the mesio-buccal root only had one root canal system. After root canal preparation with the ProTaper Ultimate system (Dentsply Sirona) it was noted that the apex was open where the two canals joined in the fused root. The open apex was closed with ProRoot MTA (Dentsply Sirona) before the mesio-buccal and remaining parts of the root canals in the fused root were obturated using AH Plus Bioceramic cement (Dentsply Sirona) and gutta-percha cones.
Taurodontism
In this type of root morphology a tooth often displays shortened roots and an elongated body where the pulp floor and root furcations are displaced apically, resulting in a large pulp chamber.74 First described by Arthur Keith, a tooth with taurodontic traits has the appearance of a bull.75 The reported prevalence ranges between 0.57% and 4.37%76,77 but can be as high as 60%.78,79 Prevalence between different population groups has been reported. In a Senegalese study involving individuals of African descent, panoramic radiographs were used to investigate maxillary first and second molars. The authors found that 18.8% of the teeth showed taurodontism with a higher prevalence in second molars.80 In an early South African study, a researcher reported a prevalence of 30% in all molars after investigating skulls from different races including those from African descent. The prevalence in first molars was not specified but the author stated that taurodontism was more common in second and third molars.81 Most available reports are case reports using radiographic examinations. The use of micro-CT in cross-sectional studies to report on the prevalence of taurodontism in maxillary first molars is scarce (if any). Figure 5 depicts an example of a maxillary first molar that was isolated with segmentation using Avizo in micro-CT from a South African of African descent.
DISCUSSION
It is apparent that root and root canal morphology can differ among population groups and it has been determined that the anatomy of molars has a relation to genetic control.82 The anatomy of the roots of molar teeth can also be influenced by geographic location or perhaps socioeconomic status.83,84 It is important that treating clinicians are aware of any variations. Roots and their root canals that remain undiscovered increase the risk of treatment failure as infections can recur.2,85
The external morphology of the maxillary first molar predominantly shows three separate roots. Most studies identified in this paper reported three roots in 90% of teeth (Table 1). It is interesting to note that different population groups within a country can display varied root morphologies and number of roots. In China, for example, eight CBCT studies were identified on individuals who displayed differences in the number of one-rooted, two-rooted, three-rooted and four-rooted teeth. Perhaps geographic factors or genetic make-up determined the differences between findings. Nearly all studies that reported on the number of roots used CBCT in their methodology. Micro-CT studies on root numbers are scarce and it appears that this technology has mainly been used to investigate complex internal morphology rather than to calculate the number of roots or macroscopic investigation of external root morphology. Although authors have determined that root morphological differences can be attributed to genetics or other factors,17,21-23 it seems that the specific reasons why the number of roots differs between populations is not clear. Single-rooted (0% to 3.9%), double-rooted (0% to 13.6%), four-rooted (0%-6%) and five-rooted (mainly by case reports) teeth in different populations are less common (Tables 1 and 2). Teeth with root morphological anomalies outside the expected norm can create treatment challenges. Additional roots can easily be overlooked during root canal treatment14 and may also cause difficulties during extractions such as fracture of roots. The aetiology of additional roots is not completely understood but it has been speculated that disease, trauma, ethnicity, genetics and external pressure on the developing tooth could contribute to its formation.86-89 Additional roots can form either by splitting or folding of the Hertwig's root sheath (HERS), thereby forming independent roots with a variety of morphological features.90 The highest incidence of a fourth root, 6%, was reported in Saudi Arabia.10 As mentioned earlier, an additional palatal root can be present on the mesio-palatal and is referred to as RML. In teeth where the additional root is present on the disto-palatal, it is referred to as RDL. These root morphologies have been described and classified by various authors.61,91
The case report described earlier depicts a rare case where both a RML and RDL were present. A thorough radiographic investigation is required to identify landmarks that might alert a clinician to the presence of additional roots or variations in root morphology. The use of magnification in the form of the dental operating microscope may assist in the location of hidden root canals. Specialised diagnostic tools such as CBCT provide a three-dimensional view and assist in the diagnosis of root canal configurations and variations in root morphology.14 It is important that clinicians follow a methodical approach to identify this type of root morphology and use specialised diagnostic tools and equipment. Although it is appreciated that dental practices may have limited access to specialised tools, they can increase the rate of endodontic success if correctly applied.2
The same can be said for teeth displaying taurodontism. Careful examination of pre-operative radiographs including panoramic views is needed, as taurodontic traits may not exhibit any significant clinical characteristics.92 Magnification can be very beneficial in identifying orifices on an apically displaced pulpal floor.
Maxillary first molars can also display fusion of different roots. According to Zhang et al.,73 roots can display six types of fusion. The MB root can be fused to the DB root (Type 1); the MB root to the P root (Type 2); the DB root to the P root (Type 3); the MB root to the DB root and either the MB or DB root to the P root (Type 4); the P root with the MB and DB roots (Type 5); and the MB, DB and P roots all fused into a cone shape (Type 6). As with calculating the number of roots, CBCT has mainly been used to report on fused roots. Root fusion is created when the HERS fails to develop or fuses in the region of the root furcation, or it can form with increased age when more and more cementum is deposited, joining roots.72 This is some of the most complex root canal morphology and often root canals are merged. It has been established that merged root canals can be present in 4.5% to 27.9% of teeth.5,6,8 Authors have also stated that root fusion in maxillary molars is more complex than in mandibular molars as two or three can be fused, altering both internal and external morphology.8,73 Clinicians should be aware that fused morphology can be present and diagnostic tools such as CBCT are valuable in establishing its presence. Even if a clinician does not have access to CBCT technology, a proper investigation of pre-operative radiographs is vital. It may alert a treating clinician to abnormal root and canal morphologies. Clinical observation during access cavity preparation is of paramount importance to identify any additional root canal orifices and roots.2
In conclusion, the external root morphology of the maxillary first molar can be diverse and the number of roots, root fusion, additional roots and taurodontism vary among populations. Investigations in African and South African populations are limited, as is the use of micro-CT in investigations. Findings in different populations are important for pre-operative diagnosis, the clinical management of affected teeth and the management of morphological root variants.
Declaration
The authors declare that there is no financial interest in this paper and that this paper has not been submitted elsewhere for publication. All authors agree with the content of the manuscript. This manuscript did not receive any funding from funding agencies in the public, commercia, or not-for-profit sectors.
Conflict of interés
We declare that there is no conflict of interest.
REFERENCES
1. Wu M-K, Wesselink PR, Walton RE. Apical terminus location of root canal treatment procedures. Oral Surg Oral Med Oral Pathol Oral Rad Endod. 2000; 89: 99-103. DOI: 10.1016/S1079-2104(00)80023-2 [ Links ]
2. Vertucci FJ. Root canal morphology and its relationship to endodontic procedures. Endod Topics. 2005; 10: 3-29. DOI: 10.1111/j.1601-1546.2005.00129.x [ Links ]
3. Van der Vyver PJ, Vorster M. Radix entomolaris: Literature review and case report. S Afr Dent J. 2017; 72: 113-7 [ Links ]
4. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984; 58: 589-99. DOI: 10.1016/0030-4220(84)90085-9 [ Links ]
5. Rwenyonyi CM, Kutesa AM, Muwazi LM, Buwembo W. Root and canal morphology of maxillary first and second permanent molar teeth in a Ugandan population. Int Endod J. 2007; 40: 679-8 [ Links ]
6. Neelakantan P, Subbarao C, Ahuja R, Subbarao CV Gutmann JL. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod. 2010; 36: 1622-7 [ Links ]
7. Kim Y Lee SJ, Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: Variations in the number of roots and canals and the incidence of fusion. J Endod. 2012; 38: 1063-8 [ Links ]
8. Martins JN, Mata A, Marques D, Caramês J. Prevalence of root fusions and main root canal merging in human upper and lower molars: A cone-beam computed omography in vivo study. J Endod. 2016; 42: 900-8 [ Links ]
9. Tian X, Yang X, Qian L, Wei B, Gong Y Analysis of the root and canal morphologies n maxillary first and second molars in a Chinese population using cone-beam computed tomography. J Endod. 2016; 42: 696-701 [ Links ]
10. Alrahabi M, Zafar MS. Evaluation of root canal morphology of maxillary molars sing cone-beam computed tomography. Pak J Med Sci. 2015; 31: 426-30. DOI: 10.12669/pjms.312.6753. DOI: 10.12669/pjms.312.6753 [ Links ]
11. Altunsoy M, Ok E, Nur BG, Aglarci OS, Gungor E, Colak M. Root canal morphology nalysis of maxillary permanent first and second molars in a southeastern Turkish opulation using cone-beam computed tomography. J Dent Sci. 2015; 10: 401-7. DOI: 10.1016/j.jds.2014.06.005 [ Links ]
12. Felsypremila G, Vinothkumar TS, Kandaswamy D. Anatomic symmetry of root and root canal orphology of posterior teeth in an Indian subpopulation using cone-beam computed tomography: A retrospective study. Eur J Dent. 2015; 09: 500-7. DOI: 10.4103/1305-7456.172623 [ Links ]
13. Alexandersen OC. Radix mesiolingualis and radix distolingualis in a collection of permanent maxillary molars. Acta Odontol Scand. 2000; 58: 229-3 [ Links ]
14. Ahmed H, Abbott P. Accessory roots in maxillary molar teeth: A review and endodontic considerations: Accessory roots in maxillary molars. Aust Dent J. 2012; 57: 123-31. DOI: 10.1111/j.1834-7819.2012.01678.x [ Links ]
15. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007; 33: 1121-32. DOI: 10.1016/j.joen.2007.06.011 [ Links ]
16. Nielsen RB, Alyassin AM, Peters DD, Carnes DL, Lancaster J. Microcomputed tomography: An advanced system for detailed endodontic research. J Endod. 1995; 1: 561- [ Links ]
17. Buchanan GD, Gamieldien MY, Fabris-Rotelli I, Van Schoor A, Uys A. Root and canal orphology of maxillary second molars in a Black South African subpopulation using cone-beam computed tomography and two classifications. Aust Endod J. 022; 00: 1-1 [ Links ]
18. Westenberger P. Avizo - Three-dimensional visualization framework. In: Proceedings f the eoinformatics 2008 - Data to knowledge, USGS, 2008, 1-- [ Links ]
19. Meyer F, Beucher S. Morphological segmentation. J Vis Commun Image Represent. 990; 1: 21-4 [ Links ]
20. Roerdink JBTM, Meijster A. The watershed transform: Definitions, algorithms and arallelization strategies. Fundam Inform. 2000; 41: 187-22 [ Links ]
21. Alavi AM, Opasanon A, Ng YL, Gulabivala K. Root and canal morphology of Thaimaxillary molars. Int Endod J. 2002; 35: 478-8 [ Links ]
22. Zheng Q, Wang Y, Zhou X, Wang Q, Zheng G, Huang D. A cone-beam computed omography study of maxillary first permanent molar root and canal morphology in a hinese population. J Endod. 2010; 36: 1480-4. DOI: 10.1016/j.joen.2010.06.01 [ Links ]
23. Lee JH, Kim KD, Lee JK, et al. Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Rad Endod. 2011; 111: 785-91. DOI: 10.1016/j.tripleo.2010.11.026 [ Links ]
24. Versiani MA, Sousa-Neto MD, Basrani B. The root canal dentition in permanent dentition, 1st ed. Heidelberg: Springer, 2018: 89-24 [ Links ]
25. Kottoor J, Velmurugan N, Ballal S, Roy A. Four-rooted maxillary first molar having C-shaped palatal root canal morphology evaluated using cone-beam computerized tomography: A case report. Oral Surg Oral Med Oral Pathol Oral Rad Endod 2011; 111: e41-e4 [ Links ]
26. Barbizam JVB, Ribeiro RG, Filho MT. Unusual anatomy of permanent maxillary molars. J Endod. 2004; 30: 668-71. DOI: 10.1097/01.DON.0000121618.45515.5A [ Links ]
27. Thomas RP, Moule AJ, Bryant R. Root canal morphology of maxillary permanent first molar teeth at various ages. Int Endod J. 1993; 26: 25--67. DOI: 10.1111/J.1365-2591.1993.tb00570.x [ Links ]
28. Martins JNR, Alkhawas MAM, Altaki Z, et al. Worldwide analyses of maxillary first molar second mesiobuccal prevalence: A multicenter cone-beam computed tomographic study. J Endod. 2018; 44: 1641-9. DOI: 10.1016/j.joen.2018.07.027 [ Links ]
29. Silva EJNL, Nejaim Y Silva AIV Haiter-Neto F, Zaia AA, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone- beam computed tomographic imaging: An in vivo study. J Endod. 2014; 40: 173-6. DOI: 10.1016/j.joen.2013.10.00 [ Links ]
30. Lyra CM, Delai D, Pereira KCR, Pereira GM, Pasternak Júnior B, Oliveira CAP. Morphology of mesiobuccal root canals of maxillary first molars: A comparison of CBCT scanning and cross-sectioning. Braz Dent J. 2015; 26: 525- [ Links ]
31. Estrela C, Bueno MR, Couto GS, et al. Study of root canal anatomy in human permanent teeth in a subpopulation of Brazil's center region using cone-beam computed tomography - Part 1. Braz Dent J. 2015; 26: 53-- [ Links ]
32. Ng YL, Aung TH, Alavi A, Gulabivala K. Root and canal morphology of Burmese maxillary molars. Int Endod J. 2001; 34: 620-30. DOI: 10.1046/J.1365-2591.2001.00438.x [ Links ]
33. Zhang R, Yang H, Yu X, Wang H, Hu T, Dummer PMH. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J. 2011; 44: 162-9. doi:10.1111/j.1365-2591.2010.01826.x [ Links ]
34. Jing Y, Ye X, Liu D, Zhang Z, Ma X. Cone-beam computed tomography was used for study of root and canal morphology of maxillary first and second molars. Beijing Da Xue Xue Bao Yi Xue Ban. 2014; 46: 958-6 [ Links ]
35. Wang H, Ci B, Yu H, et al. Evaluation of root and canal morphology of maxillary molars in a Southern Chinese subpopulation: a cone-beam computed tomographic study. Int J Clin Exp Med. 2017; 10: 7030-. [ Links ]
36. Zhang Y, Xu H, Wang D, et al. Assessment of the second mesiobuccal root canal in maxillary first molars: A cone-beam computed tomographic study. J Endod. 2017; 43: 199--6. DOI: 10.1016/j.joen.2017.06.021 [ Links ]
37. Martins JNR, Gu Y, Marques D, Francisco H, Caramês J. Differences on the Root and Root Canal Morphologies between Asian and White Ethnic Groups Analyzed by Cone-beam Computed Tomography. J Endod. 2018; 44: 1096-104. DOI:10.1016/j.joen.2018.04.00 [ Links ]
38. Gu Y Wang W, Ni L. Four-rooted permanent maxillary first and second molars in a northwestern Chinese population. Arch Oral Biol. 2015; 60: 811-7 [ Links ]
39. Ghobashy AM, Nagy MM, Bayoumi AA. Evaluation of root and canal morphology of maxillary permanent molars in an Egyptian population by cone-beam computed tomography. J Endod. 2017; 43: 108-92. DOI: 10.1016/j.joen.2017.02.014 [ Links ]
40. Salem SAB, Ibrahim SM, Abdalsamad AM. Prevalence of second mesio-buccal canal in maxillary first and second molars in an Egyptian population using CBCT (A cross-sectional study). Acta Sci Dent Sci. 2018; 2: 64-8 [ Links ]
41. Monsarrat P, Arcaute B, Peters OA, et al. Interrelationships in the variability of root canal anatomy among the permanent teeth: A full-mouth approach by cone-beam CT. PLoS ONE. 2016; 11: 1-13. DOI: 10.1371/journal.pone.016532910.1371/ journal.pone.0165329 [ Links ]
42. Beshkenadze E, Chipashvili N. Anatomo-morphological features of the root canal system in a Georgian population - cone-beam computed tomography study Georgian Med News. 2015; 247: 7-1 [ Links ]
43. Nikoloudaki GE, Kontogiannis TG, Kerezoudis NP. Evaluation of the root and canal morphology of maxillary permanent molars and the incidence of the second mesiobuccal root canal in a Greek population using cone-beam computed tomography. Open Dent J. 2015; 9: 26--72. DOI: 10.2174/1874210601509010267 [ Links ]
44. Shenoi RP Ghule HM. CBVT analysis of canal configuration of the mesio-buccal root of maxillary first permanent molar teeth: An in vitro study. Contemp Clin Dent. 2012; 3: 277-8 [ Links ]
45. Khademi A, Zamani Naser A, Bahreinian Z, Mehdizadeh M, Najarían M, Khazaei S. Root Morphology and canal configuration of first and second maxillary molars in a selected Iranian population: A cone-beam computed tomography evaluation. Iran Endod J. 2017; 12: 28--92. DOI: 10.22037/iej.v12i3.13708 [ Links ]
46. Naseri M, Safi Y Akbarzadeh Baghban A, Khayat A, Eftekhar L. Survey of anatomy and root canal morphology of maxillary first molars regarding age and gender in an Iranian population using cone-beam computed tomography. Iran Endod J. 2016; 11: 298-303. DOI: 10.22037/iej.2016.8 [ Links ]
47. Rouhani A, Bagherpour A, Akbari M, Azizi M, Nejat A, Naghavi N. Cone-beam computed tomography evaluation of maxillary first and second molars in an Iranian population: A morphological study. Iran Endod J 2014; 9: 19-- [ Links ]
48. Faramarzi F, Vossoghi M, Shokri A, Shams B, Vossoghi M, Khoshbin. Cone-beam computed tomography study of root and canal morphology of maxillary first molar in an Iranian population. Avicenna J Dent Res. 2015; 7: 1- [ Links ]
49. Ghoncheh Z, Zade BM, Kharazifard MJ. Root morphology of the maxillary first and second molars in an Iranian population using cone-beam computed tomography. J Dent (Tehran). 2017; 14: 115-2 [ Links ]
50. Shalabi RMA, Omer JG OE, Jennings M, Claffey NM. Root canal anatomy of maxillary first and second permanent molars. Int Endod J. 2000; 33: 40--14. DOI: 10.1046/j.1365-2591.2000.00221.x [ Links ]
51. Plotino G, Tocci L, Grande NM, et al. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: A cone-beam computed tomography study in vivo. J Endod. 2013; 39: 154--8. DOI: 10.1016/j.joen.2013.09.012 [ Links ]
52. Olczak K, Pawlicka H. The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Polish population. BMC Med Imaging 2017; 17: 1-7. DOI: 10.1186/s12880-017-0243-3 [ Links ]
53. Martins JNR, Marques D, Mata A, Caramês J. Root and root canal morphology of the permanent dentition in a Caucasian population: A cone-beam computed tomography study. Int Endod J. 2017; 50: 101--26. DOI: 10.1111/iej.12724 [ Links ]
54. Razumova S, Brago A, Khaskhanova L, Barakat H, Howijieh A. Evaluation of anatomy and root canal morphology of the maxillary first molar using the cone-beam computed tomography among residents of the Moscow region. Contemp Clin Dent 2018; 9: S133-S13 [ Links ]
55. Irhaim AA. Evaluation of the root and canal morphology of permanent maxillary first molars cone beam computed tomography in a sample of patients treated at the Wits Oral Health Centre. Dissertation, University of Witwatersrand, 2016: 1-5 [ Links ]
56. Pérez-Heredia M, Ferrer-Luque CM, Bravo M, Castelo-Baz P, Ruíz-Piñón M, Baca P Cone-beam computed tomographic study of root anatomy and canal configuration of molars in a Spanish population. J Endod. 2017; 43: 151--6. DOI: 10.1016/j. joen.2017.03.026 [ Links ]
57. Lin YH, Lin HN, Chen CC, Chen SS. Evaluation of the root and canal systems of maxillary molars in Taiwanese patients: A cone-beam computed tomography study. Biomed. J. 2017; 40: 232-8. DOI: 10.1016/j.bj.2017.05.003 [ Links ]
58. Ratanajirasut R, Panichuttra A, Panmekiate S. A Cone-beam computed tomographic study of root and canal morphology of maxillary first and second permanent molars in a Thai population. J Endod. 2018; 44: 5--61. DOI: 10.1016/j.joen.2017.08.020 [ Links ]
59. Altunsoy M, Ok E, Nur BG, Aglarci OS, Gungor E, Colak M.Root canal morphology analysis of maxillary permanent first and second molars in a southeastern Turkish population using cone-beam computed tomography. J Dent Sci. 2015; 10: 401-7. DOI: 10.1016/j.jds.2014.06.005 [ Links ]
60. Guo J, Vahidnia A, Sedghizadeh P, Enciso R. Evaluation of root and canal morphology of maxillary permanent first molars in a North American population by cone-beam computed tomography. J Endod. 2014; 40: 635-9. DOI: 10.1016/j.joen.2014.02.002 [ Links ]
61. Christie WH, Peikoff MD, Fogel HM. Maxillary molars with two palatal roots: A retrospective clinical study. J Endod. 1991; 17: 80-4. DOI: 10.1016/S0099-2399(06)81613-4 [ Links ]
62. Thews ME, Kemp WB, Jones CR. Aberrations in palatal root and root canal morphology of two maxillary first molars. J Endod. 1979; 5: 94-6 [ Links ]
63. Di Fiore PM. Complications of surgical crown lengthening for a maxillary molar with four roots: A clinical report. J Prosthet Dent. 1999; 82: 266-9 [ Links ]
64. Alexandersen OC. Radix paramolaris and radix distomolaris in Danish permanent maxillary molars. Acta Odontol Scand. 1999; 57: 283-9 [ Links ]
65. Baratto-Filho F, Fariniuk LF, Ferreira EL, Pecora JD, Cruz-Filho AM, Sousa-Neto MD. Clinical and macroscopic study of maxillary molars with two palatal roots. Int Endod J. 2002; 35: 796-801. DOI: 10.1046/j.1365-2591.2002.00559.x [ Links ]
66. Barbizam JVB, Ribeiro RG, Filho MT. Unusual anatomy of permanent maxillary molars. J Endod. 2004; 30: 668-71. DOI: 10.1097/01.DON.0000121618.45515.5A [ Links ]
67. Adanir N. An unusual maxillary first molar with four roots and six canals: A case report. Aust Dent J. 2007; 52: 333- [ Links ]
68. Raju RC, Chandrasekhar V, Singh CV, Pasari S. Maxillary molar with two palatal roots: Two case reports. J Conserv Dent. 2010; 13: 58-61 [ Links ]
69. He W, Wei K, Chen J, Yu Q. Endodontic treatment of maxillary first molars presenting with unusual asymmetric palatal root morphology using spiral computerized tomography: A case report. Oral Surg Oral Med Oral Pathol Oral Rad Endod. 2010; 109: e55-e59 [ Links ]
70. Moghaddas H, Tabari ZA. Palatal cervical enamel projection in a four-rooted maxillary first molar: A case report. Res J Biol Sci. 2010; 5: 508-11 [ Links ]
71. Tomazinho FS, Baratto-Filho F, Zaitter S, Leonardi DP, Gonzaga CC. Unusual anatomy of a maxillary first molar with two palatal roots: A case report. J Oral Sci. 2010; 52: 149-53 [ Links ]
72. Mashyakhy M, Chourasia HR, Jabali A, Almutairi A, Gambarini G. Analysis of fused rooted maxillary first and second molars with merged and C-shaped canal configurations: Prevalence, characteristics and correlations in a Saudi Arabian population. J Endod. 2019; 45: 1209-1 [ Links ]
73. Zhang Q, Chen H, Fan B, Fan W, Gutmann JL. Root and root canal morphology in maxillary second molar with fused root from a native Chinese population. J Endod 2014; 40: 871-5 [ Links ]
74. Jafarzadeh H, Azarpazhooh A, Mayhall JT. Taurodontism: A review of the condition and endodontic treatment challenges. Int Endod J. 2008; 41: 375-8 [ Links ]
75. Tsesis I, Steinbock N, Rosenberg E, Kaufman AY. Endodontic treatment of developmental anomalies in posterior teeth: Treatment of geminated/fused teeth - report of two cases. Int Endod J. 2003; 36: 372-9. DOI: 10.1046/j.1365- 2591.2003.00666.x [ Links ]
76. Jayashankara CM, Shivanna AK, Sridhara KS, Kumar PS. Taurodontism: A dental rarity. J Oral Maxillofac Pathol. 2013; 17: 47 [ Links ]
77. Hasan M. Taurodontism Part 1: History, aetiology and molecular signalling, epidemiology and classification. Dent Update. 2019; 46: 158-65 [ Links ]
78. Barker BCW. Taurodontism: The incidence and possible significance of the trait. Aust Dent J. 1976; 21: 272-6 [ Links ]
79. MacDonald-Jankowski DS, Li TT. Taurodontism in a young adult Chinese population. Dentomaxillofac Radiol. 1993; 22: 140-4 [ Links ]
80. Toure B, Kane AW, Sarr M, Wone MM, Fall F. Prevalence of taurodontism at the level of the molar in a black Senegalese population 15 to 19 years of age. Odontostomatol Trop. 2000; 23: 36- [ Links ]
81. Shaw JM. Taurodont teeth in South African races. J Anat. 1928; 62: 476-9 [ Links ]
82. Cleghorn BM, Christie WH, Dong CCS. Root and root canal morphology of the human permanent maxillary first molar: A literature review. J Endod. 2006; 32: 813-2 [ Links ]
83. Kuzekanani M, Najafipour R. Prevalence and distribution of radix paramolaris in the mandibular first and second molars of an Iranian population. J Int Soc Prev Community Dent. 2018; 8: 240-4 [ Links ]
84. Buchanan GD, Gamieldien MY Tredoux S, Vally ZI. Root and canal configurations of maxillary premolars in a South African subpopulation using cone-beam computed tomography and two classification systems. J Oral Sci. 2020; 62: 93-7. DOI: 10.2334/josnusd.19-0160 [ Links ]
85. Cantatore G, Berutti E, Castellucci A. Missed anatomy: Frequency and clinical impact. Endod Topics. 2006; 15: 3-31 [ Links ]
86. Tratman EK. Three-rooted lower molars in man and their racial distribution. Br Dent J. 1938; 64: 264-74 [ Links ]
87. Kocsis GS, Marcsik A. Accessory root formation on a lower medial incisor. Oral Surg Oral Med Oral Pathol 1989; 68: 644-5 [ Links ]
88. Midtbø M, Halse A. Root length, crown height, and root morphology in Turner syndrome. Acta Odontol Scand. 1994; 52: 303-14 [ Links ]
89. Kannan SK, Santharam H. Supernumerary roots. Indian J Dent Res. 2002; 13: 116-9 [ Links ]
90. Türp JC, Alt KW. Anatomy and morphology of human teeth. In: Alt KW, Rösing FW, Teschler-Nicola M. eds. Dental anthropology. Vienna: Springer, 1998: 71-94 [ Links ]
91. Baratto-Filho F, Fariniuk LF, Ferreira EL, Pecora JD, Cruz-Filho AM, Sousa-Neto MD. Clinical and macroscopic study of maxillary molars with two palatal roots. Int Endod J. 2002; 35: 796-801. DOI: 10.1046/j.1365-2591.2002.00559.x [ Links ]
92. Bürklein S, Breuer D, Schäfer E. Prevalence of taurodontic and pyramidal molars in a German population. J Endod. 2011; 37: 158-62 [ Links ]
 Correspondence:
Correspondence:
Name: Dr CH Jonker
Email: casper.jonker@plymouth.ac.uk
Tel: +44 1872 258104
Author's contribution
1 . Casper H Jonker: Principal author, manuscript layout and write-up - 60%
2 . Peet J van der Vyver: Treated patients and clinical images, manuscript layout and proofreading - 25%
3 . Anna C Oettlé: Proofreading and layout - 15%
Acknowledgements
The corresponding author would like to extend his gratitude towards Dr Charlotte Theye for technical support in preparation of the manuscript.














