Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.78 no.9 Johannesburg Out. 2023
http://dx.doi.org/10.17159/sadj.v78i09.16651
RESEARCH
Patient satisfaction with complete dentures received from an urban district hospital
K NaiduI; CP OwenII
IDepartment of Oral Rehabilitation, School of Oral Health Science, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa. ORCID: 0009-0004-6130-8284
IIProfessor Emeritus, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa. ORCID: 000-0002-9565-8010
ABSTRACT
PURPOSE: To assess some of the factors that may contribute to patient satisfaction with a complete denture service provided by a district hospital in South Africa.
METHOD: The participants were patients who had received mucosa-borne complete dentures at least one year previously. A questionnaire recorded demographics and treatment details either in person or telephonically. All patients were also asked to score a variety of factors related to satisfaction on a validated visual analogue scale. Associations were sought between patient demographics, treatment procedures and satisfaction.
RESULTS: Sample size analysis required a sample size of 180 to detect at least a medium effect size, and 76 to detect large effect sizes. However, it was not possible to increase the sample size beyond 157 in the time available. Several associations were observed that were statistically significant, but most were of small effect. Even though 75% were upset at having lost their teeth, 64% reported that they had not minded wearing dentures. Overall there were high levels of satisfaction, irrespective of the treatment procedures used. There were few meaningful associations between patient characteristics and satisfaction scores.
CONCLUSION: It was clear that the patients had adapted well to their dentures. Patient satisfaction and patient adaptability are subject to many factors, and how patients cope, and what factors help remains unknown. It is clear the provision of this complete denture service in the public sector improved these patients' quality of life and that patients can adapt to mucosa-borne dentures provided in a public setting.
Keywords: Complete dentures, patient satisfaction
INTRODUCTION
Edentulousness impairs a patient's ability to chew and perform other oral functions, resulting in a wide range of health and oral health-related quality of life impacts that can be minimised by different types of fixed and/or removable prosthodontic treatment. Implant-retained overdentures have been proposed as the standard of care1,2 for the edentulous mandible but this has been questioned on humanitarian,3 socioeconomic and prosthodontic grounds.4 Moreover, this applies to less than 1% of the world's population, who are estimated to have received implant therapy.5 In addition, health, psychological, anatomical and economic constraints preclude implant therapy for many elderly patients.
For most edentulous patients, mucosa-borne dentures will be their only choice, provided they have access to this care; in many developing countries, including South Africa, there is a high demand but a limited supply of treatment from public dental clinics. Despite their limitations, though, complete dentures can greatly improve the quality of life for edentulous patients.6,7
Appearance, comfort, the ability to masticate and to speak without encumbrance are some of the factors which determine the success or failure of the denture.8 Denture hygiene and care, the rate of resorption of the alveolar bone ridges, and the frequency with which dentures are replaced are also important factors influencing the satisfaction of dentures. Some patients adapt easily to wearing and using dentures while others may not. Thus, in addition to physical and physiological factors, the psychological traits of the patient and the relationship between the patient and clinician all play important roles in determining the level of satisfaction with complete dentures.6,9-14 In addition, the dentist's experience has also been related to satisfaction.15 While the literature has identified several factors affecting patient satisfaction with complete dentures, some of which may be beyond the control of the clinician, it is nevertheless considered important to continue to assess patient satisfaction, to identify those factors which might result in an improvement in a denture service, especially in the public sector. Barriers to access such as the location of patients relative to the hospital or clinic and the means of travelling may also influence patient acceptance and satisfaction. In South Africa, many patients travel from far outlying areas to their nearest public dental health facility for treatment which includes fabrication of complete dentures. Due to the time it takes them to reach the hospital, and the cost, many do not return for follow-up visits once they have received their denture. Patients may accept their dentures even though some may be dissatisfied with them because of the barriers to attending again.
The purpose of this study was to survey patients who have received complete dentures from a public clinic at least one year post insertion, to determine their satisfaction with their complete dentures and to investigate any associations between clinical data, patient satisfaction and the demographic characteristics of the patients.
METHODS AND MATERIALS
Ethical approval was granted by the Human Research Ethics Committee of the University of the Witwatersrand (clearance number M160734) and permission was obtained from the regulatory health authority of the Department of Health of the province. This study was conducted at the Dental Department of King Dinuzulu Hospital Complex, Springfield, Durban.
The sample size was based on the association between satisfaction scores on the one hand and sociodemographic and clinical factors on the other. For the detection of small, medium and large effect sizes (f=0.10, 0.25 or 0.40, respectively) with 80% power at the 5% significance level, sample sizes of 1096, 180 or 76 are required.16 Although at least a medium effect size would be ideal, the actual sample size of 157 was thus slightly smaller than desired, but it was found not possible to increase this number of participants. Assessment of each patient was carried out by the same clinician to ensure standardisation and consistency of observations. The following demographic data were recorded:
• Age
• Gender
• Place of residence
• Mode of transport to the clinic
• Cost to get to the clinic
• Time taken to get to the clinic
• Ease or difficulty in getting to the clinic
• Medication
• Educational level
• Ability to write and read
• Wearing dentures at night
• Cleaning dentures
• Use of fixative
• Relationship with the dentist
• Attitude towards losing their teeth
• Attitude toward wearing dentures
The patient satisfaction dimensions measured were:
• Pain - upper
• Pain - lower
• Comfort - upper
• Comfort - lower
• Appearance - upper
• Appearance - lower
• Function - upper
• Function - lower
• Stability - upper
• Stability - lower
• Speech quality
• Cleaning difficulty - upper
• Cleaning difficulty - lower
• Overall satisfaction - upper
• Overall satisfaction - lower
The full questionnaires used are available from the authors.
A Visual Analogue Scale and the McGill Pain Questionnaire17,18 were modified to assess denture comfort and patient satisfaction. The two pain scores were reverse scored so that all 15 satisfaction scores ranged from 0 (low satisfaction) to 100 (high satisfaction). The patients were given an information letter explaining the study, or it was read out to those patients only available telephonically, and they were asked to give their consent. A translator was used as necessary and, to prevent bias, the questionnaire was applied by a single administrator. If the patients were unable to attend the clinic, then telephonic contact was made and instead of a visual analogue scale, the patients were asked to score according to the expression "on a scale of 1 to 100". Patients who were able to attend the clinic were also asked to score according to this expression to provide some correlation between the two methods.
Because the fabrication of the dentures was carried out by six different clinicians based at the hospital, patient records were obtained and the procedures used as well as the number of visits were noted.
A clinical evaluation of the dentures was not carried out, because there is consensus in the literature that there is little or no correlation between such a normative assessment of complete dentures and patient satisfaction.9,19-23
Statistical analysis
The relationship between pairs of satisfaction scores was assessed by Spearman's rank correlation coefficient since the data did not meet the assumptions of Pearson's correlation coefficient. The strength of the associations was measured by interpreting the absolute value of the correlation coefficient. The following scale of interpretation was used:24
0.50 and above large effect
0.3 to 0.49 moderate effect
Below 0.3 small effect
The relationships between patient satisfaction and sociodemographic and clinical variables were assessed by the Wilcoxon rank sum test (or the Kruskal-Wallis test for more than two categories). The following scale of interpretation was used:24
0.80 and above large effect
0.50 to 0.79 moderate effect
0.20 to 0.49 small effect
below 0.20 near zero effect
The χ2 test was used to assess the relationships between procedures and the number of post-insertion visits. Fisher's exact test was used for 2 x 2 tables or where the requirements for the X2 test could not be met. The strength of the associations was measured by Cramer's V and the phi coefficient respectively. The following scale of interpretation was used:24
0.50 and above high/strong association
0.30 to 0.49 moderate association
0.10 to 0.29 weak association
below 0.10 little, if any, association
Data analysis was carried out using SAS (version 9.4 for Windows). The 5% significance level was used.
RESULTS
Because there were no baseline data, the end-point satisfaction scores for the various dimensions were compared and not the percentage difference/gain/loss in satisfaction. A total of 157 patients who received complete dentures completed the VAS survey, 62% on paper and 38% telephonically. For those who completed the scores on paper, there were no differences between where they placed their mark and when subsequently asked to score verbally on a scale of "one to a hundred", thus validating the telephonically derived scores.
Associations between demographic variables and satisfaction scores
The mean age of the patients was 71 years with a range of 60 to 91. The proportion of female patients (66%) was almost twice that of male patients (34%). Only 7% of the patients had matriculated from school, 5% had a diploma, and 11% were illiterate. Sixty-nine percent of the participants were on medication for hypertension and 48% for diabetes. There were no meaningful associations between any of the satisfaction scores and age, gender, education and medication.
In terms of their attitude toward wearing dentures, 75% were upset at having lost their teeth, and 64% reported that they had not minded wearing dentures. There were no significant or meaningful relationships to any of the satisfaction scores.
The statistical analysis did reveal some associations between some of the satisfaction scores and some of the demographic variables (Table 1) but the effect sizes were small or very small and so it is unlikely that any of these variables influenced satisfaction.
Relationship with the dentist
This was marked on a 5-point scale where 1 = poor and 5 = excellent. Patients generally had a good relationship with the dentist who made their dentures, with 87% rating a 4 or 5. No patients rated 1, 7 rated 2, and 14 rated 3. For associations, categories 1-3 were combined, because of the small group sizes (13%). Many of the scores were significantly lower in the few patients whose relationship with the dentist was reported as poor, but there were only two medium effect sizes (comfort and function of the upper denture), the rest being small.
Procedures used
The procedures used for fabricating dentures and the percentages are shown in Table 2.
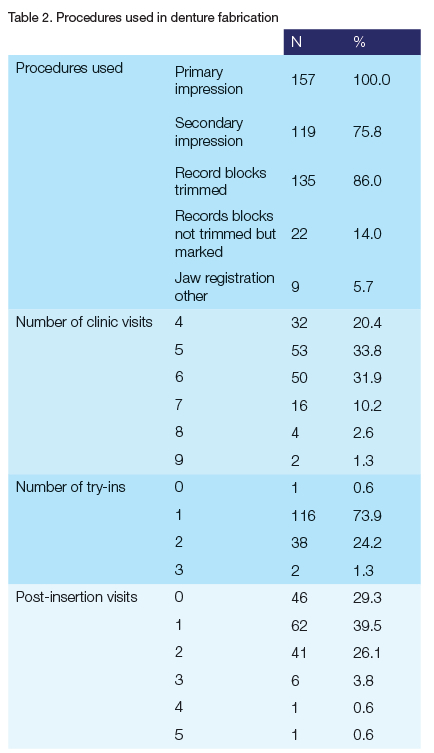
For analysis, because of small group sizes it was necessary to make groupings as follows:
Number of clinic visits: 7 or more visits were grouped.
Number of try-ins: 2 and 3 were grouped, and 0 was omitted.
Number of post-insertion visits: 2 or more visits were grouped.
The only statistically significant difference to emerge was, not surprisingly, between whether or not a secondary impression was made and the number of clinic visits. Associations were then sought to enquire if any of the procedure variables were associated with any of the satisfaction scores. Statistically significant differences were found only for secondary impressions (appearance, stability of the mandibular denture, speech and cleaning) and jaw registrations when the record lock was not trimmed (appearance of the maxillary denture). In all cases the effect sizes were small.
Overall patient satisfaction scores
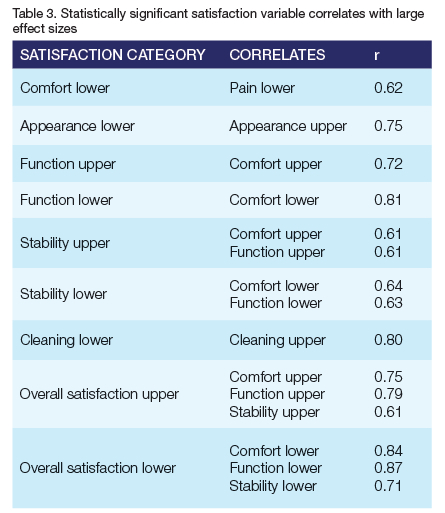
Correlations coefficients were calculated between the patient satisfaction variables, and several large effect sizes were found, all at p < 0.0001 (Table 3).
DISCUSSION
Patient satisfaction
Patient satisfaction is the ultimate goal in dental treatment. Conventional complete dentures are the only practical treatment option for most edentulous patients. However, a patient's satisfaction with denture use hinges on a variety of factors such as aesthetics, speech, retention, comfort and function, as well as dentist-patient communication.14,25
Visual analogue scales (VAS) were used for assessing patient satisfaction, and these have been validated in several studies. The results showed that the correlations observed were all entirely logical; for example, discomfort was correlated with pain, stability with comfort and function and overall satisfaction with comfort, function and stability.
In a questionnaire-based study, Marinus (1990)26 stressed the mutual benefits of the patient-dentist relationship concerning satisfaction, attitude and expectations from their new dentures. Santos et al (2015)27 found that the establishment of a friendly and respectful relationship between patients and dentists during denture-making may result in higher satisfaction. The participants in this study reported an overwhelmingly good relationship with their dentist, with 87% scoring 4 or 5 on a 5-point poor-to-excellent scale. The patients' satisfaction scores affected most variables except stability of the mandibular denture, but with small effect sizes. Moderate effect sizes were, however, noted for comfort (r = 0.53) and for function (r = 0.50) of the maxillary denture. These results would generally imply and confirm that the psycho-social element in the making of complete dentures is an important one.
The satisfaction variable correlates were all logical, and overall patient satisfaction was high, with a mean score for all scores of 75 (SD 17). The overall satisfaction score with the maxillary denture was 75 and 68 with the mandibular denture. It was clear, therefore, that these patients were able to adapt well to their dentures and all were using them satisfactorily for at least a year post-insertion. Although patients were able to function well with their dentures, a limitation of the procedures was that it appears that nutrition counselling was not a routine. It has been shown that this is necessary as the mere presence of a prosthesis does not necessarily change food choices without targeted interventions to improve dietary habits.28,29
Patient demographics
The age and gender distribution was not dissimilar to those reported elsewhere, as was the fact that there was no association between these and satisfaction scores,13,22,25,30-32 although there have been associations shown of a higher satisfaction score for aesthetics in women denture wearers.27,33,34
Many medications and combinations of medication can contribute to adverse intra-oral conditions such as depleted and poor saliva (which contributes to difficulty with denture wearing), but there were no significant associations between any of the satisfaction scores and medication. It is unclear why this should be the case among these participants, and it may reflect their adaptability.
Although there were some associations between some of the satisfaction scores and some of the demographic variables, the effect sizes were small or very small and so it is unlikely that any of these variables influenced satisfaction. This may have been a measure of the fact that in this sample only moderate or large effects would be significant, but other studies have not reported consistent associations and most relied purely on probability values without calculating effect sizes.
It was interesting to note that the most common method of cleaning their dentures was soaking in water alone, although this was mostly after either brushing with soap or toothpaste. This has not been reported in the literature. An advantage of following up patients and recalling them is that aspects such as denture cleaning can be reinforced, as some reported using bleach (which adversely affects the appearance), and abrasives such as the use of bicarbonate of soda and coarse salt. Although no clinical examinations were performed, it is important to emphasise appropriate cleaning methods because of the well-known association with denture stomatitis.
It was also of some concern to find a relatively large number of patients who slept with their dentures at night (23% and 15% wore maxillary and mandibular dentures, respectively). A recent systematic review35 reported mean values of nocturnal denture wearing varying from 11% to 31%. The concern is mainly with the association between nocturnal denture wearing and candidiasis36 as well as a possible association with sleep disorders. The clinical advice is always for patients to leave their dentures out at night, especially those with denture stomatitis. There were some associations: scores for pain, comfort, function and speech were significantly higher for those who wore their dentures at night, compared with those who did not but so were the scores for overall satisfaction, which is not logical, and perhaps explains why the effect sizes were small.
Only 5% and 8% of the patients reported that they used a fixative for their maxillary and mandibular dentures respectively. No prevalence studies on the use of fixatives could be found. Although the effect sizes were small, it was logical to observe higher scores for the stability, overall satisfaction and speech for those using fixatives in the maxillary denture and comfort, function, stability, overall satisfaction and speech for the mandibular denture. It has been suggested that denture fixatives may improve the dietary behaviour of complete denture wearers37 and, for patients who can afford these, this could be encouraged If they have difficulty wearing complete dentures which are technically correct.
Procedures used during the making of complete dentures
The literature has been equivocal about the link between certain procedures used in the construction of complete dentures and subsequent patient satisfaction. Several recent systematic reviews (eg Sanjeevan et al (2021)38 have shown similar outcomes using abbreviated techniques when compared with conventional multivisit techniques and some studies have found some links such as between fewer post-delivery adjustments and higher patient satisfaction scores (eg Gaspar et al 2013).6
In this study, it was not possible to infer that those who had more than one try-in were correlated with the procedures used, due to the low numbers. It was also not possible to determine the reasons for the variety in post-insertion visits (40% had one visit, but 29% did not return at all). It would appear that, in keeping with the literature on abbreviated or "simplified" techniques, the procedures used did not influence patient satisfaction in the participants of this study.
Limitations
The sample size was a limitation of this study as only small effect sizes could be detected. The influence of previous denture wearing was also not determined and this could have had a bearing on patient adaptability and therefore of satisfaction. Nevertheless, the information gave valuable insight into the multiple aspects that can affect patient satisfaction, as well as the need for follow-up in terms of oral hygiene and nutrition advice.
CONCLUSION
Within the limitations of this study, and despite the great variety among the participants, their overall satisfaction scores with their complete dentures were such that, in comparison with other international studies, they had adapted well to denture-wearing.
Although there were several associations between satisfaction scores and some characteristics of the participants, the low sample size precluded definitive correlations. Patient satisfaction and patient adaptability are subject to a multitude of factors, and just how patients cope, and what factors assist this process, remains unknown. The provision of this mucosa-borne complete denture service in a public sector hospital has provided these patients with improved function as they were able to adapt well to their dentures. However, denture hygiene and nutritional counselling should become a routine part of all removable prosthodontic service provision. It is therefore recommended that national and provincial health departments provide sufficient funds so that edentulous patients may have the health benefits of being able to chew and therefore improve their nutritional status and, at the same time, improve their appearance.
ACKNOWLEDGEMENTS
Thanks are due to the hospital management, the nursing staff and, in particular, the participants, as well as the dentists who had provided the dentures. We are grateful to Dr P Gaylard for the statistical analysis.
This research was originally successfully submitted for an MScDent degree.
Funding/conflict of interest
The research received no funding and the authors declare no conflict of interest.
REFERENCES
1. Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, et al. The McGill Consensus Statement on Overdentures. Int J Prosthodont 2002; 15: 413-4 [ Links ]
2. Thomason JM, Kelly SA, Bendkowski A, Ellis JS. Two implant retained overdentures - a review of the literature supporting the McGill and York consensus statements. J Dent 2012; 40: 22-34. doi: 10.1016/j.jdent.2011.08.017 [ Links ]
2. Owen CP. Standards of care: good or evil? Int J Prosthodont. 2008; 22: 328-330 [ Links ]
3. Fitzpatrick B. Standard of care for the edentulous mandible: a systematic review. J Prosthet Dent. 2006; 95(1): 71-8. doi: 10.1016/j.prosdent.2005.11.007 [ Links ]
4. Carlsson GE. Critical review of some dogmas in prosthodontics. J Prosthodont Res. 2009; 53(1): 3-10. doi: 10.1016/j.jpor.2008.08.003 [ Links ]
5. Gaspar MG, Dos Santos MBF, Dos Santos JFF, Marchini L. Correlation of previous experience, patient expectation and the number of post-delivery adjustments of complete dentures with patient satisfaction in a Brazilian population. J Oral Rehab. 2013; 40: 590-594. doi: 10.1111/joor.12070 [ Links ]
6. Omar R, Al-Tarakemah Y, Akbar J, Al-Awadhi S, Behbehani Y, Lamontagne P Influence of procedural variations during the laboratory phase of complete denture fabrication on patient satisfaction and denture quality. J Dent 2013; 41: 852-860. doi: 10.1016/j.jdent.2013.07.013 [ Links ]
7. Fenlon MR, Sherriff M, Newton JT. The influence of personality on patients' satisfaction with existing and new complete dentures. J Dent 2007; 35(9): 744-8. doi: 10.1016/j.jdent.2007.06.003 [ Links ]
8. Van Waas MAJ. The influence of clinical variables on patients' satisfaction with complete dentures. J Prosthet Dent 1990; 63: 307-310. doi: 10.1016/0022-3913(90)90202-n [ Links ]
9. Garrett NR, Kapur KK. Effects of improvements of poorly fitting dentures and new dentures on patient satisfaction. J Prosthet Dent 1996; 76(4): 403-413. doi: 10.1016/s0022-3913(96)90546-6 [ Links ]
10. Brunello D L, Mandikos MN. Construction faults, age, gender, and relative medical health: Factors associated with complaints in complete denture patients. J Prosthet Dent 1998; 79(5): 545-554. doi: 10.1016/s0022-3913(98)70176-3 [ Links ]
11. Fenlon MR, Sherriff M, Walter JD. An investigation of factors influencing patients' use of new complete dentures using structural equation modelling techniques. Community Dent Oral Epidemiol 2000; 28(2): 133-140. doi: 10.1034/j.1600-0528.2000.028002133.x [ Links ]
12. Bilhan H, Geckili O, Ergin S, Erdogan O, Ates G. Evaluation of satisfaction and complications in patients with existing complete dentures. J Oral Sci. 2013; 55(1): 29-37. doi: 10.2334/josnusd.55.29 [ Links ]
13. Chen JH, Huang HL, Lin YC, Chou TM, Ebinger J, Lee HE. Dentist-Patient Communication and Denture Quality Associated with Complete Denture Satisfaction Among Taiwanese Elderly Wearers. Int J Prosthodont. 2015; 28(5): 531-7. doi: 10.11607/ijp.4223 [ Links ]
14 Kimoto S, Kimoto K, Kitamura A, Saita M, Iijima M, Kawai Y. Effect of dentist's clinical experience on treatment satisfaction of a complete denture. J Oral Rehabil. 2013; 40: 940-947. doi: 10.1111/joor.12108 [ Links ]
15. Faul F, Erdfelder E, Lang A.-G, Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39(2): 175-91. doi: 10.3758/bf03193146 [ Links ]
16. Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975; 1(3): 277-299. doi: 10.1016/0304-3959(75)90044-5 [ Links ]
17. Ohnhaus EE, Adler R. Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain. 1975; 1(4): 379-384. doi: 10.1016/0304-3959(75)90075-5 [ Links ]
18. Langer A, Michman J, Seifert I. Factors influencing satisfaction with complete dentures in geriatric patients. J Prosthet Dent 1961; 11: 1019-1031 [ Links ]
19. Berg E. The influence of some anamnestic, demographic and clinical variables on patient acceptance of new complete dentures. Acta Odontol Scand 1984; 42: 119-273. doi: 10.3109/00016358409035249 [ Links ]
20. Heyink J, Heezen J, Schaub R. Dentist and patient appraisal of complete dentures in a Dutch elderly population community. Dent Oral Epidemiol 1986; 14: 323-6. doi: 10.1111/j.1600-0528.1986.tb01083.x [ Links ]
22. Awad MA and Feine JS. Measuring patient satisfaction with mandibular prostheses. Community Dent Oral Epidemiol. 1998; 26(6): 400-5. doi: 10.1111/j.1600-0528.1998.tb01978.x [ Links ]
23. Fenlon MR, Sherriff M, Walter JD. Agreement between clinical measures of quality and patients' rating of fit of existing and new complete dentures. J Dent. 2002; 30(4): 135-9. doi: 10.1016/s0300-5712(02)00016-7 [ Links ]
24. Cohen J. Statistical power and analysis for the behavioral sciences (2nd ed.), 1988; Hillsdale, NJ, Lawrence Erlbaum Associates, Inc. [ Links ]
25. Al-Omiri MK, Sghaireen MG, Al-Qudah AA, Hammad OA, Lynch CD ynch E. Relationship between impacts of removable prosthodontic rehabilitation on daily living, satisfaction and personality profiles. J Dent. 2014; 42(3): 366-72. doi: 10.1016/j.jdent.2013.12.010 [ Links ]
26. Van Waas MA. The influence of psychologic factors on patient satisfaction with complete dentures. J Prosthet Dent. 1990; 63(5): 545-548. doi: 10.1016/0022-3913(90)90073-1 [ Links ]
27 . Santos BF, dos Santos MB, Santos JF, Marchini L. Patients' evaluation of complete denture therapy and their association with related variables: A pilot study. J Prosthodont. 2015; 24(5): 351-357. doi: 10.1111/jopr.12286 [ Links ]
28. Bradbury J, Thomason JM, Jepson NJ, Walls AW, Allen PF, Moynihan PJ. Nutrition counseling increases fruit and vegetable intake in the edentulous. J Dent Res. 2006; 85(5): 463-468. doi: 10.1177/154405910608500513 [ Links ]
29. Hamdan NM, Gray-Donald K, Awad MA, Johnson-Down L, Wollin S, Feine JS. Do implant overdentures improve dietary intake? A randomized clinical trial. J Dent Res. 2013; 92(12 Suppl): 146S-53S. doi: 10.1177/0022034513504948 [ Links ]
30. Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: Revisiting the shared treatment decision-making model. Soc Sci Med 1999; 49: 651661. doi: 10.1016/s0277-9536(99)00145-8 [ Links ]
31. Al Quran F, Clifford T, Cooper C, Lamey PJ. Influence of psychological factors on the acceptance of complete dentures. Gerodontology. 2001; 18: 35-40. doi: 10.1111/j.1741-2358.2001.00035.x [ Links ]
32. Celebic A, Knezovic-Zlataric D, Papic M, Carek V, Baucic I, Stipetic J. Factors Related to Patient Satisfaction with Complete Denture Therapy. J Gerontol A Biol Sci Med Sci. 2003; 58(10): M948-53. doi: 10.1093/gerona/58.10.m948 [ Links ]
33. de Lima EA, dos Santos MB, Marchini L. Patients expectations of and satisfaction with implant-supported fixed partial dentures and single crowns. Int J Prosthodont.2012; 25: 484-490 [ Links ]
34. da Cunha MC, Santos JF, Santos MB, Marchini L. Patients expectations before and satisfaction after full arch fixed implant-prosthesis rehabilitation. J Oral Implantol. 2015; 41(3): 235-239. doi: 10.1563/AAID-JOI-D-12-00134 [ Links ]
35. Emami E, Nguyen HP, Rompré P, Lavigne GJ, Huynh NT. The effect of nocturnal wear of dentures on the sleep quality: a systematic review and meta-analysis. Sleep Breath. 2017; 21(1): 9-18. doi: 10.1007/s11325-016-1369-1 [ Links ]
36. Compagnoni MA, Souza RF, Marra J, Pero AC, Barbosa DB. Relationship between Candida and nocturnal denture wear: quantitative study. J Oral Rehabil. 2007; 34(8): 600-605. doi: 10.1111/j.1365-2842.2007.01754.x [ Links ]
37. Bartlett DW, Maggio B, Targett D, Fenlon MR, Thomas J. A preliminary investigation into the use of denture adhesives combined with dietary advice to improve diets in complete denture wearers. J Dent. 2013; 41(2): 143-7. doi: 10.1016/j.jdent.2012.10.012 [ Links ]
38. Sanjeevan V, Rajagopal P, Venkitachalam R, Aras M. Efficiency of simplified versus traditional denture fabrication methods: A systematic review and meta-analysis. J Prosthet Dent. 2021; 126(3): 377-385. doi: 10.1016/j.prosdent.2020.07.003. [ Links ]
 Correspondence:
Correspondence:
Prof CP Owen
Tel: +27 83 679 2205
Email: peter.owen@wits.ac.za
Author's contribution:
1 . K Naidu - 70%
2 . CP Owen - 30%














