Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.78 no.7 Johannesburg Ago. 2023
http://dx.doi.org/10.17159/sadj.v78i07.17071
RADIOLOGY CORNER
MAXILLOFACIAL RADIOLOGY
Nevoid Basal Cell Carcinoma Syndrome
L MerboldI; Z YakoobII
IBChD, PGDipDent (Radiology), MSc (Maxillofacial Radiology), Department of Oral and Maxillofacial Pathology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, South Africa ORCID: 0000-0003-4041-127X
IIBChD, PDD (Maxillofacial and Oral Radiology), MSc (Maxillofacial and Oral Radiology), PGDip General Management (GIBS Pret), Department of Oral and Maxillofacial Pathology, School of Dentistry, Faculty of Health Sciences, University of Pretoria, South Africa. ORCID: 0000-0003-1966-5574
CASE
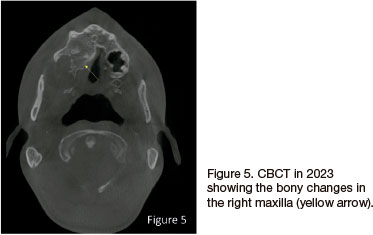
An 18-year-old male patient presented at our dental clinic in 2009 for a dental assessment. A panoramic radiograph was taken to evaluate dental crowning (Figure 1). An incidental finding was noted in the right maxilla, presenting as a well-demarcated, round, unilocular, radiolucent lesion with a corticated rim extending from the right maxillary tuberosity area to distal of the 16 causing impaction of the 18. A biopsy was taken and diagnosed as an odontogenic keratocyst (OKC) that was subsequently enucleated. In 2021 the patient returned and another panoramic radiograph (Figure 2) and a Waters view was taken where calcification of the falx cerebri was seen (Figure 3). On the panoramic radiograph an additional mandibular lesion was visible that presented as a well-demarcated, round, unilocular, radiolucent lesion with a corticated rim extending from distal of the 46 into the missing 47, 48 area. A CBCT was then taken to further analyse the lesions (Figure 4). A biopsy was taken in the right posterior mandible and diagnosed as an OKC. In 2023 the patient returned and a CBCT was taken. The right maxilla showed increased bone density adjacent to the enucleated lesion (Figure 5).
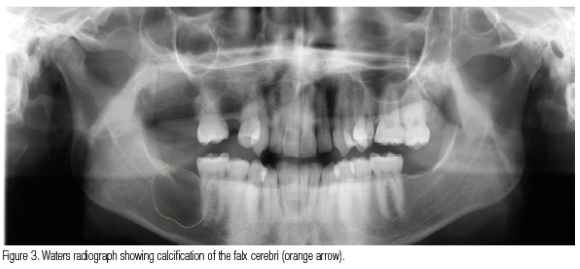
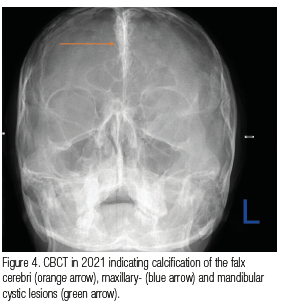
A diagnosis of Nevoid Basal Cell Carcinoma Syndrome (NBCCS) was made due to the multiple OKCs and calcification of the falx cerebri.
INTERPRETATION
Nevoid Basal Cell Carcinoma Syndrome (NBCCS), also known as Gorlin syndrome, is an autosomal dominant inherited condition1 with an equal gender distribution2 and a prevalence of 1 in 60,00O3 It is more common in the white population when compared to the black population, arising in the first to third decades of life3. It is caused due to a mutation in the patched (PTCH1) tumour suppressor gene on chromosome 9q22.3-q314, a component of the Hedgehog (Hh) pathway.5
The major diagnostic criteria for NBCCS are:3
• Multiple basal cell carcinomas (BCCs) of the skin
• Multiple odontogenic keratocysts of the jaws
• Calcification of the falx cerebri
• Bifid rib
• Palmar/planter pitting
The minor diagnostic criteria of NBCCS are:2
• Frontal and temporoparietal bossing
• Hypertelorism
• Mandibular prognathism
• Ovarian fibroma
• Medulloblastoma
A clinical diagnosis relies on specific criteria. NBCCS can be suspected with the presence of major and/or minor criteria, while a gene mutation analysis will confirm the diagnosis.2
The OKCs in patients with NBCCS differ from those in patients with isolated OKCs.4 The age when the first cyst presents is younger in the syndromic group. On radiographic examination, the OKCs in both groups have a similar presentation. The OKCs in patients with NBCCS are commonly associated with the crowns of impacted teeth and can be mistaken for dentigerous cysts.1
The OKCs in NBCCS usually present as uni- or multilocular radiolucencies and can be uni- or bilateral. In younger patients, the OKCs may be associated with an impacted tooth, leading to the displacement of teeth or less commonly causing root resorption. OKCs are usually locally destructive and can spread within the bone, rarely causing expansion.3 OKCs can be differentiated from other odontogenic cysts due to their non-expansive/minimal-expansive nature. Most benign odontogenic lesions expand the cortical borders of the jaws where OKCs extend along the long-axis or antero-posterior region of the jaws.6
The patient presented above did not have any of the other clinical features of NBCCS. However, if Basal Cell Carcinomas are present the treatment and prognosis depend on the behaviour of the skin lesions. The manifestations of NBCCS are generally not life-threatening; however, early diagnosis is important. Patients should take precautions to avoid ultraviolet sun exposure and radiation therapy. In rare instances, the skin lesions can cause tumour invasion into the brain and be fatal.1 The jaw cysts can be treated conservatively by enucleation. Removal of the cysts can lead to facial deformity and infection.1 The OKCs in patients with NBCCS have a higher recurrence rate and need more aggressive treatment.6 To detect early recurrences, the patient must be followed up with regular radiographs. Genetic counselling should be done for all patients with NBCCS.1 Early diagnosis and regular follow-up visits by a multidisciplinary team are important.3
AUTHORS' DECLARATION
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the University of Pretoria Ethics Committee (Reference no. 381/2023). All procedures followed the ethical standards of the Helsinki Declaration of 1975, as revised in 2008.
REFERENCES
1. Neville, BW, Damm, DD, Allen, CM, Chi, AC (2016). Oral and Maxillofacial Pathology. 4th Edition, WB Saunders, Elsevier, Missouri, 640-644 [ Links ]
2. Lo Muzio, L (2008). Nevoid basal cell carcinoma syndrome (gorlin syndrome). Orphanet Journal of Rare Diseases, 3, 32-32. https://doi.org/10.1186/1750-1172-3-32 [ Links ]
3. Manfredi, M, Vescovi, P, Bonanini, M, Porter, S (2004). Nevoid basal cell carcinoma syndrome: a review of the literature. International Journal of Oral & Maxillofacial Surgery, 33(2), 117-124. https://doi.org/10.1054/ijom.2003.0435 [ Links ]
4. Ambele, MA, Robinson, L, van Heerden, MB, Pepper, MS, van Heerden, WFP (2023). Comparative Molecular Genetics of Odontogenic Keratocysts in Sporadic and Syndromic Patients. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc, 36(1), 100002 https://doi.org/10.1016/j.modpat.2022.100002 [ Links ]
5. Bellei, B, Caputo, S, Carbone, A, Silipo, V, Papaccio, F, Picardo, M, Eibenschutz, L (2020). The role of dermal fibroblasts in nevoid basal cell carcinoma syndrome patients: an overview. International Journal of Molecular Sciences, 21(3). https://doi.org/10.3390/ijms21030720 [ Links ]
6. Unsal, G, Cicciu, M, Ayman Ahmad Saleh, R, Riyadh Ali Hammamy, M, Amer Kadri, A, Kuran, B, Minervini, G (2023). Radiological evaluation of odontogenic keratocysts in patients with nevoid basal cell carcinoma syndrome: a review. The Saudi Dental Journal. https://doi.org/10.1016/j.sdentj.2023.05.023 [ Links ]
 Correspondence:
Correspondence:
Zarah Yakoob
Email: zarah.yakoob@up.ac.za
Author's contribution
1. Lené Merbold (primary author) - 50%
2. Zarah Yakoob (secondary author) - 50%














