Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.78 no.6 Johannesburg jul. 2023
http://dx.doi.org/10.17159/sadj.v78i06.16914
LITERATURE REVIEW
Aggressive odontogenic myxoma of the maxilla in a 9-year-old child. Report of a case and literature review
TC RaveleI; MMJ MasilelaII; IT DikgaleIII
IBDS, PG Dip Forensic Odontology. Sefako Makgatho Health Sciences University, Department of Oral and Maxillofacial Pathology, Pietersburg Academic Hospital, Oral Pathology Unit, South Africa. ORCID: 0009-0009-2932-1274
IIBDS, PG Dipl Dent (Oral Pathology), MDent (Oral Pathology). Sefako Makgatho Health Sciences University, Department of Oral and Maxillofacial Surgery, Pietersburg Academic Hospital, Oral Pathology Unit, South Africa. ORCID: 0000-0001-9702-5797
IIIBDT, BDS, MDent (MFOS), FC, Pietersburg Academic Hospital, Maxillofacial and Oral Pathology Unit, South Africa. ORCID: 0000-0001-6949-1811
ABSTRACT
Odontogenic myxoma is a rare, locally aggressive benign tumour of odontogenic ectomesenchyme origin. The tumour may cause significant facial disfigurement and has a negative psychological impact on a child. Odontogenic myxoma has predilection for females in the second and third decades of life. The mandibular molar region is the most frequently affected site. It is imperative to detect the tumour early to avoid radical surgery and reduce local recurrences. This case study reports a case of a 9-year-old female patient who presented with an expansile tumour that affected the entire left maxilla, perforated into the left maxillary sinus and completely occluded the sinus.
Keywords: Odontogenic myxoma, maxilla, aggressive.
INTRODUCTION
Odontogenic myxoma (OM) is an aggressive benign odontogenic neoplasm of ectomesenchymal origin that intimately resembles the dental papilla of a developing tooth microscopically. The tumour accounts for 2-5% of cases in Africa, China and the US.1 Two-thirds of OMs occur in the mandibular molar region whereas one-third occur in the maxilla, favouring the premolar-molar region. There is a female predilection within the second and third decades of life.1-7 Histologically the tumour is characterised by the spindle and stellate cells that are embedded in an abundant myxoid-rich stroma.1 This paper reports a case of a fast-growing maxillary OM in a 9-year-old female.
Case report
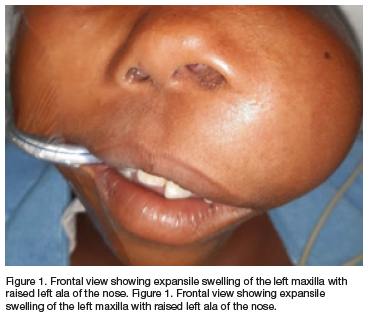
A 9-year-old female patient presented to Pietersburg Hospital, Maxillofacial and Oral Surgery clinic with the main complaint of a slightly painful mass of the left maxilla of approximately 2 years' duration. On examination, she had a large non-ulcerated swelling on the left maxilla measuring 7cmx12cm which raised the ala of the nose and flattened the alar groove (Figure 1). Intra-orally, there was evidence of both buccal and palatal bone expansion.
Both the orthopantomogram image as well as the computerised tomography image revealed a well-circumscribed soap-bubble to ground glass, expansile radiolucent maxillary tumour of about 4cmx3.3cm involving the unerupted and displaced tooth 25 and root resorption of tooth 24 (Figure 2a). The tumour extended into the left maxillary sinus causing complete occlusion of the sinus (Figure 2b). Clinical differential diagnoses included adenomatoid odontogenic tumour, ameloblastoma, ameloblastic fibroma and odontogenic myxoma. All these tumours are common in younger patients, cause bone expansion and are usually radiolucent.
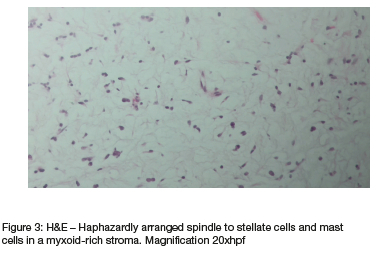
An incisional biopsy of the lesion was done and the specimen was sent for microscopic evaluation. The histological evaluation showed an infiltrating benign tumour composed of the spindle to stellate cells with eosinophilic cytoplasm in a myxoid-rich stroma with scattered vascular channels and sparse collagen fibrils. Numerous mast cells were also evident (Figure 3). The stromal cells stained diffusely and strongly positive for vimentin and Bcl-2 and patchy for smooth muscle actin (SMA) (Figure 4). There was no expression for h-Caldesmon. The proliferative index as detected by Ki-67 was less than 5%. The diagnosis of odontogenic myxoma was made.
Surgical management
Considering the extent of the tumour, a left hemi-maxillectomy was performed and could be classified according to the Brown classification system as vertical class II with a horizontal component b. Dieffenbach's modification of Weber Ferguson's approach was used to expose the tumour. A reconstruction plate was placed and secured with screws from the anterior part of the right maxilla extending to the left side of the zygomatic process to give more support to the remaining right maxilla. Soft tissue closure was achieved using polyglycolic 3/0 sutures on the mucosa and nylon 5/0 sutures on the skin (Figure 5).

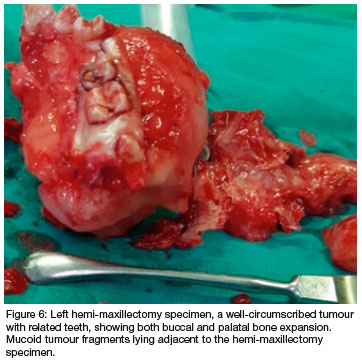
The left hemi-maxillectomy excision specimen showed a bony hard tumour with both buccal and palatal bone expansion and associated dentition. A well-circumscribed gelatinous tumour was noted (Figure 6). The histological diagnosis was consistent with the incision diagnosis of OM.
DISCUSSION
OM is a rare benign odontogenic tumour of ectomesenchymal origin, known for its local invasiveness and recurrence.2-4,8-9 Although OM is a rare tumour, its existence is well documented in the literature with the first case being reported in 1947.10 The tumour accounts for 2-5% of all odontogenic tumours3,11 and is the second most common odontogenic tumour after ameloblastoma.4,12-13 A study undertaken in 2017, which aimed to analyse the pattern of distribution of odontogenic tumours in sub-Saharan Africa, found that OM accounted for 4.9% of all odontogenic tumours. These included 67 cases from Nigeria, 55 from South Africa, 41 from Tanzania, 35 from Kenya and 6 from Uganda.13 In a 26-year retrospective study performed on odontogenic tumours manifesting in the first two decades of life in the South African rural population, OM was found to account for 4.7% of the cases.12 A range of 0.5-17% was also reported to prevail in Asia, Europe and America.2 The rarity of OM in the South African population is evidenced by studies undertaken in 2011 and 2016 whereby only 55 cases were reported over a period of 26 years and 29 over a period of 40 years respectively.12,14
OM is believed to arise from the ectomesenchyme and is perceived to be a tumour of dual fibroblastic-histiocytic origin with cells having myofibroblastic nature.15 The pathogenesis is not clear; however, HMGA2 rearrangement and HMGA2 protein overexpression may be associated with tumorigenesis.16 Recently, activating mutations in the MAPK/ERK signalling pathway have been identified in the tumour, which can serve as targets for pharmacological therapy.17 The invasive behaviour of the tumour is facilitated by MMP-9 while MMP-1 helps to remodel the extracellular matrix and facilitates the dissemination of the tumour through the bone.18-19
Bcl-2, an antiapoptotic protein, indicates the proliferative activity of the tumour cells. Intense Bcl-2 staining correlates with tumour aggressiveness whereas poor Bcl-2 staining indicates a lack of aggressiveness. 20 As an antiapoptotic protein, Bcl-2 helps to establish the persistence of the proliferative tumour cells.4 In our case, there was diffuse Bcl-2 staining of the stromal cells and a low proliferative index of 2-4% as indicated by Ki-67. These findings correlate with the aggressive nature of the case. Although resection with clear margins was achieved, the patient needs a close follow-up to guard against recurrence.
The scarcity of OM in children younger than 10 years has been observed in multiple studies. Although OM may occur in the age range of 1 to 80 years, most tumours are encountered in the second and third decades of life and shows a female predilection.3-5,9,11-12,15,21-23 OMs are most commonly encountered in the posterior mandible as compared to the maxilla and, when occurring on the maxilla, the posterior region is the most affected.2 No site predilection was observed in some studies.12 Our patient was remarkable for both her young age and the fact that the lesion occurred in the maxilla.
Generally, OMs are slow-growing painless tumours.14 Some of the reported major complaints are the presence of swelling and failure in tooth eruption.5 Small OMs are usually asymptomatic whereas larger lesions cause painless expansion.21 In our case, we found that the lesion was slightly painful, with both buccal and palatal bone expansions causing facial asymmetry. Perforation and obliteration of the maxillary sinus were also observed and have not been commonly reported before.
Radiologically, most OM appears radiolucent and may be unilocular or multilocular with well-defined to ill-defined borders. The most common finding in a conventional radiograph is a multilocular radiolucency exhibiting soap-bubble, honeycomb or tennis racquet appearances. These features help to differentiate OM from malignant tumours as they are very destructive without trabeculation and bone septae.1,6,11,24 The expansile nature of OMs commonly causes displacement of associated teeth instead of root resorption. Displaced teeth are usually vital.2,14,25 The radiological features of our current case are consistent with those reported in the literature even though the uncommon feature of root resorption was also observed. The radiographic differential diagnoses include ameloblastoma, ameloblastic fibroma, aneurysmal bone cyst, glandular odontogenic cyst and central giant cell granuloma.
There is a tendency for patients to delay seeking medical intervention and the key contributors to late consultation are inaccessibility to healthcare facilities, low socioeconomic status and lack of knowledge.14 Oral health education and proper screening cannot be overemphasised.
The gross examination of OM appears to be a greyish-white, homogenous to heterogeneous nodular mass with variable consistency and the cut surface exhibits a homogenous glistening gelatinous surface9,24 which was similar to our case.
Histopathologically, OM is relatively easy to diagnose and is generally characterised by abundant myxoid stroma with spindle to stellate to round-shaped cells embedded within it. In some cases, tiny capillaries and sparse collagen fibrils are present. When there is dense collagen, the term fibromyxoma is used.1,17,24,26 Mast cells may also be found and are believed to contribute to the degradation of extracellular matrix and differentiation of myofibroblasts in OM, favouring local invasion of the tumour.4 Numerous mast cells (Figure 3) and myofibroblasts as highlighted by SMA (Figure 4) possibly contributed to the local invasiveness and aggressive behaviour observed in our case.
The histologic features of OM resemble a normal dental papilla; however, the clinical and radiographic features help to establish the diagnosis of OM. Differential diagnosis to be considered for a case of myxoid-rich OM is myxoid neurofibroma, hyperplastic dental follicle and chondromyxoid fibroma.17 Myxoid neurofibroma tends to grow in fascicles, contains numerous mast cells and stains positive for S100. Chondrmyxoid fibroma has chondroid tissue within a myxoid stroma, unlike OM which is usually myxoid or has increased fibrous stroma.5 Our case was predominantly myxoid with loosely arranged spindle to stellate-shaped cells. The tumour cells stained positive for vimentin and focally for SMA, but negative for h-Caldesmon, suggesting the possible myofibroblast nature of the lesion.
Small lesions may be treated by curettage only but large lesions require wide surgical resection because OM are usually not encapsulated and have a tendency to infiltrate the surrounding bone.1'24,26 In the present case, the patient was treated with hemi-maxillectomy resection and a reconstruction plate was placed and secured with screws from the anterior part of the right maxilla extending to the left side of the zygomatic process to give more support to the remaining right maxilla. No prosthetic construction was done to allow the growth plate to close completely and to co-ordinate long-term maintainance to rule out recurrence.
Postoperative complications such as transient dysfunction of the marginal mandibular branch of the facial nerve and loss of the microvascular flap may occur.5 A recurrence rate of up to 25% may be seen26-27 and is more likely to occur in cases that were treated with curettage only. However, lesions may recur even post extensive resection.5 After a year, our patient remains disease free. Yet, despite the radical surgery, we continue to monitor the patient.
CONCLUSION
Odontogenic myxomas are rare, benign odontogenic tumours that can be aggressive and may cause facial disfigurement and have a negative psychological impact on a child. Early detection of these lesions can avoid radical surgery. In children with larger tumours, we recommend long-term follow-up to guard against recurrence. Prosthetic reconstruction can be done once growth is completed.
Informed consent
Informed consent was obtained from both the patient and the guardian to publish this case report. Ethics clearance was also obtained from the Ethics Committee with clearance number SMUREC/D/101/2023: (J) Journal.
Conflict of interest
None
REFERENCES
1. Odell EW, Adebiyi K. Odontogenic myxoma/myxofibroma. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PG, eds. WHO Classification of Head and Neck Tumours, 4th ed. Lyon, IARC, 2017: 229-30 [ Links ]
2. Noffke CE, Raubenheimer EJ, Chabikuli NJ, Bouckaert MM. Odontogenic myxoma: review of the literature and report of 30 cases from South Africa. Oral Surg Oral Med Oral Pathol Oral Radiol, and Endod. 2007; 104(1): 101-9 [ Links ]
3. Dotta JH, Miotto LN, Spin-Neto R, Ferrisse TM. Odontogenic Myxoma: Systematic review and bias analysis. Eur J Clin Invest. 2020; 50: e13214 [ Links ]
4. Effiom OA, Adewole RA, Odukoya O. Clinicopathological characteristics of odontogenic myxoma in Nigerians. WAJM. 2011; 30(4): 255-61 [ Links ]
5. Francisco ALN, Chulam TC, Silva FO, Robeiro GG, Pinto CAL, Gondak RO, et al. Clinicopathologic analysis of 14 cases of odontogenic myxoma and review of the literature. J Clin Exp Dent. 2017; 9 (4): e560-3 [ Links ]
6. Ramesh V, Dhanuja M, Sriram K, Balamurali PD. Odontogenic myxoma of the maxilla - A case report. J. Int Oral Health. 2011; 3(1): 59 - 63 [ Links ]
7. Sato H, Kurihara Y, Shiogama S, Saka K, Kurasawa Y, Itose M, Yaso A, Shirota T. Long-term follow-up after conservative surgical treatment of odontogenic myxoma: a case report and literature review. Case Reports in Dentistry. 2019; 1-6 [ Links ]
8. Chulam TC, Silva FO, Ribeiro DG, Gondak RO, Kowalski LP, Gonçalves-Filho J. Clinicopathologic analysis of 14 cases of odontogenic myxoma and review of the literature. J Clin Exp Dent. 2017; 9(4): e560 [ Links ]
9. Shivashankara C, Nidoni M, Patil S, Shashikala KT. Odontogenic myxoma: a review with report of an uncommon case with recurrence in the mandible of a teenage male. The Saudi dental journal. 2017; 29(3): 93-101 [ Links ]
10. Thoma KH, Goldman HM. Central myxoma of the jaw. American Journal of Orthodontics and Oral Surgery. 1947; 33(7): B532-40 [ Links ]
11. Singaraju S, Wanjari SP, Parwani RN. Odontogenic myxoma of the maxilla: A report of a rare case and review of the literature. J Oral Maxillofac Pathol. 2010; 14(1):19 [ Links ]
12. Mamabolo M, Noffke C, Raubenheimer E. Odontogenic tumours manifesting in the first two decades of life in a rural African population sample: A 26-year retrospective analysis. Dentomaxillofacial Radiology. 2011; 40: 331-7 [ Links ]
13. Ogundana OM, Effiom OA, Odukoya O. Pattern of distribution of odontogenic tumours in sub-Saharan Africa. International Dental Journal. 2017; 67: 308-17 [ Links ]
14. Titinchi F, Hassan BA, Morkel JA, Nortje C. Odontogenic myxoma: a clinicopathological study in a South African population. J Oral Pathol Med. 2016; 45(8):599-604 [ Links ]
15. Sivakumar G, Kavitha B, Saraswathi TR, Sivapathasundharam B. Odontogenic myxoma of maxilla. Indian J Dent Res. 2008;19: 62-5 [ Links ]
16. Gomes CC, Diniz MG, Duarte AP, Bernardes VF, Gomez RS. Molecular review of odontogenic myxoma. Oral Oncology. 2011; 47: 325-8 [ Links ]
17. Vered M, Wright JM. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Odontogenic and Maxillofacial Bone Tumours. Head and Neck Pathology.2022; 16: 63-75 [ Links ]
18. Miyagi SP Marunduba CM, de Sa Silva F, Marques MM. Dental pulp stem cells express proteins involved in the local invasiveness of odontogenic myxoma. Braz Oral Res. 2012; 26(2): 139-144 [ Links ]
19. Nonaka CF, Goulart Filho JA, da Costa Miguel MC, de Souza LB, Pinto LP Immunohistochemical expression of matrix metalloproteinases 1, 2, and 9 in odontogenic myxoma and dental germ papilla. Pathology-Research and Practice. 2009; 205(7): 458-65 [ Links ]
20. Godishala Swamy SR, Naag S, Bahl S, Priyadarshini E. Odontogenic myxoma: A causality dilemma-Report of a nonpareil case and review of literature. J Oral and Maxillofac Pathol. 2018; S2-6 [ Links ]
21. Wankhedkar D, Patankar S, Gokul S, Sharma S. Odontogenic myxoma in an 8-year-old girl: A case report with review of literature. J Oral Maxillofac Pathol. 2019; 23: S83-6 [ Links ]
22. Siriwardena BS, Crane H, O'Neill N, Abdelkarim R, Brierley DJ, Franklin CD, Farthing PM, Speight PM, Hunter KD. Odontogenic tumors and lesions treated in a single specialist oral and maxillofacial pathology unit in the United Kingdom in 1992-2016. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2019;127(2): 151- 66 [ Links ]
23. Taneja T, Saxena S, Reddy V, Goel A, Taneja N. Odontogenic myxoma: A rare case involving maxillary sinus with a brief review of the literature. Indian Journal of Oral Sciences. 2012; 3(2): 107 [ Links ]
24. Ramesh S, Govindraju P, Pachipalusu B. Odontogenic myxoma of posterior maxilla-A rare case report. J Fam Med Prim Care. 2020; 9(3): 1744-8 [ Links ]
25. Kheir E, Stephen L, Nortje C, van Rensburg LJ, Titinchi F. The imaging characteristics of odontogenic myxoma and a comparison of three different imaging modalities. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2013; 116(4): 492-502 [ Links ]
26. Chi AC, Neville BW, Damm DD, Allen CM. Oral and Maxillofacial Pathology-E-Book. Elsevier Health Sciences; 2017: 29 [ Links ]
27. Banasser AM, Bawazir MM, Islam MN, Bhattacharyya I, Cohen DM, Fitzpatrick SG. Odontogenic myxoma: A 23-year retrospective series of 38 cases. Head and Neck Pathology. 2020; 14(4): 1021-7 [ Links ]
 Correspondence:
Correspondence:
Name: Dr MMJ Masilela
Tel: 082 410 4225
Email: mmjmams@yahoo.com / Mokgobja.Masilela@dhsd.limpopo.gov.za
Author's contribution
1. TC Ravele 40% (first author)
2. MMJ Masilela 40%
3. TC Dikgale 20%














