Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.78 n.3 Johannesburg Apr. 2023
RESEARCH
Factors that affected the efficacy of nonsurgical periodontal treatment carried out by postgraduate periodontology students
M AbdallaI; MT PeckII; C RaynerIII; F Kimmie-DhansayIV; A JefthaV
IDepartment of Oral Medicine and Periodontology, Faculty of Dentistry. University of the Western Cape. ORCID: 0000-0002-3083-7974
IISpecialist in Oral Medicine and Periodontology. Private Practice, Cape Town. ORCID: 0000-0002-4755-0574
IIIDepartment of Oral Hygeine. Faculty of Dentistry. University of the Western Cape. ORCID: 0000-0002-8057-0956
IVResearch support unit, Faculty of Dentistry. University of the Western Cape. ORCID: 0000-0003-2919-6193
VDepartment of Oral Medicine and Periodontology, Faculty of Dentistry. University of the Western Cape. ORCID: 0000-0003-0910-5899
ABSTRACT
BACKGROUND: The training of postgraduate students in periodontology has a significant clinical impact. The overall assessment of the efficacy of non-surgical treatment of periodontitis, has value to inform training protocols as well as assess the quality of clinical service delivery. Furthermore, obstacles to successful treatment can be identified
AIM: The aim of the study was to determine the effectiveness of non-surgical periodontal treatment, as well as the factors that may determine treatment outcome at the postgraduate clinic in the Periodontology Department at the University of the Western Cape, Tygerberg Dental Hospital, between 2016 and 2018
METHODS: A cross-sectional record-based study of 100 patients was conducted. Demographic, social, clinical, treatment data were obtained from the hospital files. Periodontal parameters including bleeding index (BI), Pocket Probing depth (PPD), Plaque index (PI), and clinical attachment level (CAL), were recorded at the initial visit (Pre-treatment) and follow-up visits (Post-treatment), and the final treatment outcomes were calculated based on the differences of these parameters' values between the initial visit and the last follow-up visit. Data were presented as mean and range for continuous variables and as a frequency for categorical variables. Statistical analyses were performed to determine if there was a relationship between the varied factors and treatment outcome with p < 0.05 as statistically significant
RESULTS: The results showed that all 100 patients demonstrated a marked reduction in PPD, PI, BI, and loss of CAL. The overall mean PPD reduction was 0.32 (0.5), the mean reduction in PI and BI were 37.2 (24.08) and 34.61 (22.78), respectively, and the mean clinical attachment gain was 0.42 (0.97) mm. Treatment outcome showed no difference in PPD, PI, BI, and CAL between females, smokers, and patients with systemic conditions compared to males, nonsmokers, and patients without systemic conditions. On the other hand, patients who underwent more maintenance treatment visits over a period longer than 2 months duration had significantly better outcomes compared to patients who had less than two months of duration of treatment
CONCLUSION: This study proved the effectiveness of the non-surgical surgical periodontal treatment at the postgraduate periodontal clinic. Treatment duration and frequency of recall visits were the most influential factor impacting the treatment outcome
Keywords: Periodontal disease. Periodontitis. Non-surgical Periodontal therapy. Treatment efficacy. Treatment outcome. Postgraduate Students. Tygerberg Dental Hospital. Influential factors.
INTRODUCTION
Periodontal disease is the sixth most prevalent disease globally1,2,3,4. A new classification of periodontal disease was proposed in June 2018 based on the World Workshop on Classification of Periodontal and Peri-Implant Diseases and Conditions held in Chicago in November 2017. According to the pathophysiology, this workshop classified periodontal disease into three categories: necrotizing periodontitis, periodontitis as a manifestation of a systemic disease, and periodontitis. Periodontitis is further characterized by the staging and grading system that relies on the severity of the disease and the rate of disease progression, respectively.5
Investigations have shown that periodontitis is linked to over 50 systemic diseases and conditions.6 Although no clear causative association has been established, it has been found that periodontal therapy is not only crucial for maintaining proper oral health, but can also improve the overall systemic health of periodontally involved individuals.7 Periodontal therapy aims to restore the natural dentition, periodontium, and peri-implant tissue, as well as to restore function, aesthetics, health, and comfort.8 Generally, there are four phases associated with periodontal therapy: the systemic phase, the initial non-surgical phase, the constructive surgical phase, and the supportive periodontal phase. The initial non-surgical phase is the most critical component of periodontal therapy with the main objective to reduce or eliminate gingival inflammation.9
Treatment outcome is the evaluation carried out to assess the results of treatment to determine the efficiency, effectiveness, safety, and practicability of the treatment in each case.10 The American Academy of Periodontology reported the desired outcome of periodontal therapy as a significant resolution of clinical signs of gingival inflammation, reduction of pocket depths, clinical attachment gains (or at least stabilization of the attachment level), and the progress toward reduction of plaque to a level compatible with gingival health.11 Periodontal treatment outcome is considered clinically successful with the absence of pocket depth (> 5mm) and bleeding on probing of < 15%. The treatment outcome is defined as beneficial when the mean clinical attachment level and the mean probing pocket depth outcomes were improved.12,13
The aim of the study was to determine the effectiveness of non-surgical periodontal treatment, as well as the factors that affected the clinical outcome at the postgraduate clinic in the Periodontology Department at the University of the Western Cape, Tygerberg Dental Hospital, between 2016 and 2018.
MATERIALS AND METHODS
The present study was an analytic, cross-sectional, record-based study of patients who had visited the postgraduate clinic at the Periodontal Department at Tygerberg Dental Hospital between 2016 and 2018 for the treatment of periodontitis. The study was approved by the the Biomedical Research Ethics Committee of the University of the Western Cape (Ethics Reference Number: BM19/2/6).
Inclusion criteria were patients between 18 and 80 years, patients diagnosed with periodontitis, patients treated by a postgraduate student, and patients who had follow-up visits. Exclusion criteria were patients who had no record of follow-up visit, pregnant women or breastfeeding mothers, and patients with missing data.
Data collection
More than 700 files for patients treated by different students at the postgraduate department during the years 20162018, were analyzed. This study included a convenient sample of 100 patients who met the inclusion criteria. Patient data were obtained from the hospital files. Age, sex, smoking history and medical history were acquired from the patient profiles. In addition, treatment data such as type of treatment provided, whether chlorhexidine mouthwash has been prescribed, and treatment duration were also obtained. Furthermore, the periodontal parameters data were also extracted. These include (BI), (PPD), and (PI). These parameters were recorded at six sites per tooth (mesiobuccal, mid buccal, distobuccal, mesiolingual, mid lingual, and distolingual). In addition to that (CAL), which was measured by the distance from the cementoenamel junction to the base of the periodontal pocket was also obtained. The mean values of all these parameters were recorded at the initial visit (Pre-treatment) and follow-up visits (post-treatment), and the final treatment outcomes were calculated based on the differences of these parameters' values between the initial visit and the last follow-up visit.
Statistical analysis
Statistical analysis was performed using Stata Corp (2017) Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. Data were presented as mean and range for continuous variables and as a frequency for categorical variables. Statistical analyses were performed using a t-test to determine if there was a relation between the varied factors and treatment outcome. A P-value of p < 0.05 was considered statistically significant.
RESULTS
The study population consisted of 100 patients with periodontitis. The patients' mean age was 51.1 (23.24) years old (range 22-81 years). The sample consisted of 48 males and 52 females with a ratio of 0.9:1. Smoking history was present in 70 patients. Systemic conditions were present in 53 patients (26 patients with diabetes mellites, 6 patients with HIV, and 21 patients with other conditions). The overall mean PPD reduction was 0.31 (0.4), the mean reduction in PI and BI were 37.2 (24.08) and 34.61 (22.78), respectively, and the mean clinical attachment gain was 0.42 (0.97)mm. Treatment outcome showed greater decrease in PPD, PI, and BI, as well as greater increase in CAL in females, smokers, and patients with systemic conditions compared to males, non-smoker, and patients without systemic conditions. However, this finding was not statistically significant. Results are shown in Table 1.
Results also showed that as the number of dental visits increased by 1 visit, the probing depths decreased by -0.37 units, the plaque index decreased by -0.414 units and the CAL increased by 0.038 units. However, these findings were statistically insignificant.
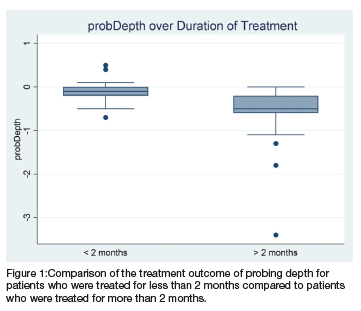
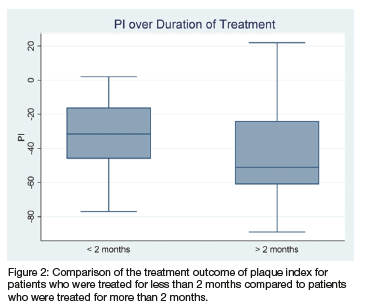
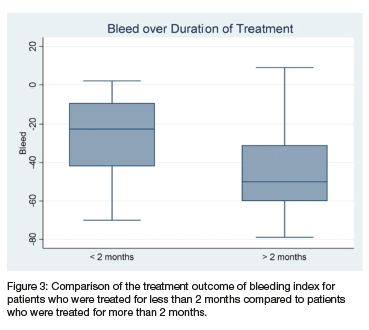
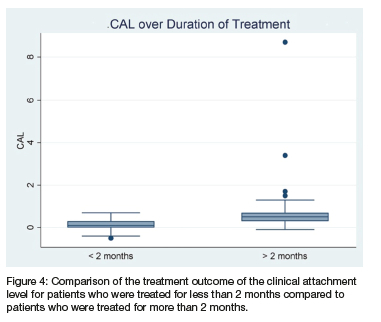
All patients were given oral hygiene instructions (OHI) and chlorhexidine (CHX) prescriptions. Ninety six percent (96 patients) were treated with scaling and root planing, while only 4% (4 patients) were treated with scaling only. Antibiotics were prescribed for 28% (28 patients). Fifty percent (50 patients) were treated for more than two months and 50% (50 patients) were treated for less than 2 months. Treatment outcome showed a greater decrease in PPD, PI, BI, as well as increase in CAL in patients who underwent more than 2 months of treatment compared to patients who had less than two months of treatment. This finding was statistically significant. Results are shown in Figures 1-4.
DISCUSSION
The goal of the current study was to determine the effectiveness of non-surgical periodontal treatment, as well as the factors that affect this efficacy. Although not statistically significant, this study showed that all patients demonstrated a marked reduction in PPD, PI, BI and an increase in the CAL. The overall mean PPD reduction was 0.31 (0.4), the mean reduction in PI and BI were 37.2 (24.08) and 34.61 (22.78), respectively, and the mean clinical attachment gain was 0.42 (0.97) mm. In a study with a large Chinese population that included 10,789 patients, the overall mean PPD reduction was 0.6mm.14 Cobb et al,. reported that the mean PPD reduction for pockets was 1.29 mm, with a net gain in clinical attachment level of 0.55 mm.15
Patient-related factors
Males had higher pre-treatment PPD, PI, BI and clinical attachment loss compared to females. However, only CAL was statistically significant. This proposes that females had better oral hygiene behavior than males. This result conforms to several studies conducted in the past decades that compared oral hygiene behavior between males and females. Strauss et al., also found that females practice daily interdental cleaning more often than men.16 However, in the present study improvement in the periodontal parameters after treatment in both males and females were observed, however, the effectiveness of treatment was not affected by sex factor.
Smokers had a higher pre-treatment PPD, PI, BI, and clinical attachment loss compared to non-smokers. Although, none of these findings were statistically significant. This finding is similar to a cross-sectional study in India, which evaluated the periodontal health status among cigarette smokers and non-smokers. The study showed that deep pockets of > 6mm were found in 41% of smokers and 26% of nonsmokers, and the difference between the two groups was statistically significant.17 Petrovic et al., found a statistically higher plaque index in smokers compared to non-smoker.18 Haffajee et al., also found that current smokers had greater attachment loss than past smokers or those who never smoked.19 Smoking status did not significantly affect treatment outcome in this population.
Patients with systemic conditions had a higher pre-treatment pocket depth and plaque index compared to patients without systemic conditions. Several studies support the relationship between systemic diseases and periodontal disease. A study in Sweden found that the prevalence of periodontal pockets > 5mm was associated with established hypertension or high blood pressure readings,20 while Botero et al., found that patients with both periodontitis and diabetes mellitus have greater clinical attachment loss than non-diabetic periodontitis patients.21
The findings of this study revealed that the improvement in BI, PI and CAL was not affected by the medical condition of the patient. However, the mean PPD was different between participants with and without a systemic condition at base line.
Treatment-related factors
The present study found that treatment duration of more than two months was more beneficial in reducing PPD, PI, and BI, as well as increasing CAL compared to treatment of less than two months duration. This finding is in agreement with a study conducted in Israel in 2003 which evaluated probing pocket depth changes following 2 years of periodontal maintenance therapy. The study included 595 patients, whereby all participants showed a continuous decrease in pocket depth of 0.95 over the 2 year.22 A similar outcome was reported in a study that examined periodontal and dental conditions in individuals after periodontal therapy in private practice in Geneva. They found that longer treatment duration (i.e., the more frequent the recall visits), was associated with a greater reduction in probing pocket depth (23). Worth mentioning is the duration of treatment and frequency of periodontal maintenance visits, which may reflect the patient compliance and dedication to treatment, as patients with longer duration of treatment are usually more dedicated to their periodontal treatment, which positively impacts the periodontal treatment outcome.24, 25
The main limitations of this study were that the study was file-based, which made it inherently vulnerable to bias, as well as the relatively limited sample size, which influenced the statistical significance.
CONCLUSION
This is the first reported study of its kind to investigate the periodontal treatment outcome in a local South African dental hospital, which confirmed the effectiveness of non-surgical periodontal treatment in the Postgraduate Periodontal Clinic at Tygerberg Dental Hospital. The overall reduction in PPD, BI, PI, and clinical attachment gain was reported in all patients. The most significant factor to impact treatment outcome is treatment duration and frequency of recall visits; greater success is achieved if treatment is rendered over more than two months with increased frequency of recall visits.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest nor any financial interest in this study. Furthermore, we declare that the study does not have any commercial value and is done purely to add to the current pool of knowledge.
Author's contribution:
Dr M Abdalla 35%
Supervisor: Dr A Jeftha 25%
Co supervisor: Mrs C.Rayner 20%
Co Supervisor: Dr. M.T.Peck 10%
Statisticians: Dr F. Kimmie- Dhansay 10%
REFERENCES
1. Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe periodontitis in 1990.2010: a systematic review and meta. regression. Journal of dental research. 2014 Nov;93(11):1045.53. [ Links ]
2. Frencken JE, Sharma P, Stenhouse L, Green D, Laverty D, Dietrich T. Global epidemiology of dental caries and severe periodontitis-a comprehensive review. Journal of clinical periodontology. 2017 Mar;44: S94.105. [ Links ]
3. Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. International journal of health sciences. 2017 Apr;11(2):72. [ Links ]
4. Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. Journal of clinical periodontology. 2017 May;44(5):456.62. [ Links ]
5. Caton JG, Armitage G, Berglundh T, Chapple IL, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M, Tonetti MS. A new classification scheme for periodontal and peri-implant diseases and conditions-Introduction and key changes from the 1999 classification. Journal of periodontology. 2018 Jun;89:S1.8. [ Links ]
6. Beck JD, Papapanou PN, Philips KH, Offenbacher S. Periodontal medicine: 100 years of progress. Journal of dental research. 2019 Sep;98(10):1053.62. [ Links ]
7. Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. International journal of health sciences. 2017 Apr;11(2):72. [ Links ]
8. Mariotti A, Hefti AF. Defining periodontal health. BMC oral health. 2015 Dec;15(1):1.8. [ Links ]
9. Azouni KG, Tarakji B. The trimeric model: A new model of periodontal treatment planning. Journal of Clinical and Diagnostic Research: JCDR. 2014 Jul;8(7):ZE17. [ Links ]
10. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research. 2011 Mar 1;38(2):65.76. [ Links ]
11. Walter C, Rodriguez FR, Taner B, Hecker H, Weiger R. Association of tobacco use and periapical pathosis-a systematic review. International endodontic journal. 2012 Dec;45(12):1065.73. [ Links ]
12. Van der Velden U, Sanz M. Postgraduate periodontal education. Scope, competences, proficiencies and learning outcomes: Consensus report of the 1st European workshop on periodontal education-position paper 3 and consensus view 3. European Journal of Dental Education. 2010 May; 14:34.40. [ Links ]
13. Sanz I, Alonso B, Carasol M, Herrera D, Sanz M. Nonsurgical treatment of periodontitis. Journal of Evidence.Based Dental Practice. 2012 Sep 1;12(3):76.86. [ Links ]
14. Jiao J, Shi D, Cao ZQ, Meng HX, Lu RF, Zhang L, Song Y Zhao JR. Effectiveness of non-surgical periodontal therapy in a large Chinese population with chronic periodontitis. Journal of clinical periodontology. 2017 Jan;44(1):42.50. [ Links ]
15. Cobb CM. Non-surgical pocket therapy: Mechanical. Annals of periodontology. 1996 Nov;1(1):443.90. [ Links ]
16. Strauss, S.M. and Stefanou, L.B. Interdental cleaning among persons with diabetes: relationships with individual characteristics. International journal of dental hygiene.2014; 12(2), pp.127.132. [ Links ]
17. Gautam, D.K., Jindal, V., Gupta, S.C., Tuli, A., Kotwal, B., and Thakur, R. Effect of cigarette smoking on the periodontal health status: A comparative, cross.sectional study. Journal of Indian Society of Periodontology.2011;15(4), p.383 [ Links ]
18. Petrovic, M., Kesic, L., Obradovic, R., Savic, Z., Mihailovic, D., Obradovic, I., Avdic. Saracevic, M., Janjic.Trickovic, O., and Janjic, M.. Comparative analysis of smoking influence on periodontal tissue in subjects with periodontal disease. Materia socio. medica. 2013; 25(3), p.196. [ Links ]
19. Haffajee, A.D. and Socransky, S.S. Relationship of cigarette smoking to attachment level profiles. Journal of Clinical Periodontology. 2001;28(4), pp.283-295. [ Links ]
20. Engström, S., Gahnberg, L., Högberg, H., and Svärdsudd, K.. Association between high blood pressure and deep periodontal pockets. Upsala journal of medical sciences. 2007;112(1), pp.95.103. [ Links ]
21. Botero, J.E., Yepes, F.L., Roldán, N., Castrillón, C.A., Hincapie, J.P., Ochoa, S.P., Ospina, C.A., Becerra, M.A., Jaramillo, A., Gutierrez, S.J., and Contreras, A. Tooth and periodontal clinical attachment loss are associated with hyperglycemia in patients with diabetes. Journal of periodontology. 2012;83(10), pp.1245.1250. [ Links ]
22. Soskolne WA, Proskin HM, Stabholz A. Probing depth changes following 2 years of periodontal maintenance therapy including adjunctive controlled release of chlorhexidine. Journal of periodontology. 2003 Apr;74(4):420.7. [ Links ]
23. Müller Campanile V Megally A, Campanile G, Gayet-Ageron A, Giannopoulou C, Mombelli A. Risk factors for recurrence of periodontal disease in patients in maintenance care in a private practice. Journal of clinical periodontology. 2019 Sep;46(9):918-26. [ Links ]
24. Carvalho VF, Okuda OS, Bernardo CC, Pannuti CM, Georgetti MA, De Micheli G, Pustiglioni FE. Compliance improvement in periodontal maintenance. Journal of Applied Oral Science. 2010 Jun;18(3):215.9. [ Links ]
25. Oliveira Costa F, Miranda Cota LO, Pereira Lages EJ, Medeiros Lorentz TC, Soares Dutra Oliveira AM, Dutra Oliveira PA, Costa JE. Progression of periodontitis in a sample of regular and irregular compliers under maintenance therapy: a 3-year follow-up study. Journal of periodontology. 2011 Sep;82(9):1279-87. [ Links ]
 Correspondence:
Correspondence:
M Abdalla
Rm D4 Tygeberg Hosp- U W C Dental School,Francie Van Zijl Drive, Parow, Cape Town,7500.
Email: 3820881@myuwc.ac.za; Cell: 0840316566














