Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.78 no.2 Johannesburg mar. 2023
CASE REPORT
An innovative digital workflow for the fabrication of a prosthetic ear: A case report
N NetshilindiI; W Asia-MichaelsII; R MaartIII
IBChD, MChD Prosthodontist, OHCS, SA Military Health Services neonetshilindi@gmail.com
IIBChD, MChD; Senior Lecturer/Specialist Restorative Dentistry University of the Western Cape Tel. +27 21 937 3005 Fax. +27 21 931 2287 Private Bag X01 Tygerberg 7505. wasiamichaels@uwc.ac.za
IIIBChD, FDD, MPhil, PhD; Stomatologist /Senior Lecturer Restorative Dentistry University of the Western Cape. Tel. +27 21 937 3181; Fax. +27 21 931 2287, Private Bag X01, Tygerberg 7505. rmaart@uwc.ac.za
ABSTRACT
The aim of maxillofacial rehabilitation is to provide suitable prostheses for patients with oro-facial defects, and enable them to resume their roles in society. Recent advances in bionics and prosthetics have combined different techniques to help in the production of aesthetic and functional prostheses. Technology can now supplement the freehand sculpting skills of the clinician by capturing accurate images of the soft tissues from both the defect and non-defect areas, and using these to digitally recreate the desired templates.
This case report describes the digital steps used to capture necessary data for the design and fabrication of an auricular template, and final ear prosthesis. Results from this case study suggested that the digital method is: 1) more accurate; 2) less time-consuming than traditional methods; and 3) less invasive, and thus more accepted by patients.
Keywords: Maxillofacial prosthetics, Auricular prosthesis, Digital impression, Computer-aided design/computer-aided manufacturing (CAD/CAM), Rapid prototyping, Standard Tessellation Language (STL)
INTRODUCTION
Facial deformity can be emotionally traumatising and could affect the social behaviour of an individual.1 Maxillofacial prosthetics is defined as the art and science of restoring a malformed or missing part of the human body through artificial means.2 A prosthesis may be the appropriate treatment when surgical reconstruction is unsuitable or not possible.3 Maxillofacial prosthodontics aims to provide functional and/or aesthetically pleasing prostheses for patients with facial defects so that they may feel comfortable working and interacting with others in their daily lives.1 Lifelike facial and body prostheses rely on accurate reproduction of the shape and colour of the missing part, and need to blend well with the surrounding structures in order to make them as inconspicuous as possible.4 An auricular prosthesis is a removable appliance that offers an alternative to surgical rehabilitation of a missing ear.5 These have generally been fabricated by means of modelling a template of the missing ear by hand using direct measurements from the dimensions of the opposing ear as a guide. In some cases, impressions of ears from healthy "donor volunteers" have also been used to aid the clinician. The template (usually wax) is then positioned and adjusted at the chairside to ensure it is in the correct alignment with the remaining ear, and of the desired size, shape and extent of protrusion.6 This process requires a certain amount of artistic skill, to sculpt and carve human anatomy, and can take time to develop and perfect.4 The final template is then processed into a shade matched silicone prosthesis which may be attached with adhesives, via mechanical means (such as spectacle frames) or with bone-anchored implants.7
The conventional way of fabricating an auricular prosthesis is tedious, time-consuming, and relies on the artistic dexterity or the clinician or technician. Two key processes of production are used to record accurate impressions and produce an inverted copy of the patient's normal ear that will fit over the defect.8 As the process of impression taking of the defective surface is technique sensitive, it may be uncomfortable for the patient.9 Potential errors include the distortion of the facial soft tissues during the impression taking process.10
Recent advances in bionics and prosthodontics have combined different techniques to help with the fabrication of aesthetically pleasing and / or functional prostheses, of which ear prostheses are an example of progress in this area.12 Technology can now supplement the freehand sculpting skills by capturing accurate images of the opposing structures and replicating them in an inverse form.13
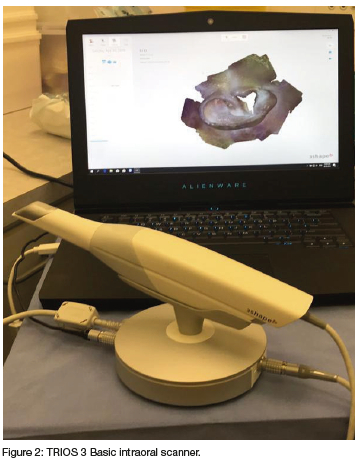
Digital impression techniques have also been described using sophisticated laser scanning technology. However, the use of magnetic resonance imaging (MRI) and computed tomography (CT) to acquire digital models may expose the patient to unnecessary radiation.9 Nevertheless, computer aided design and rapid prototyping have recently been used to fabricate an inverted copy of an ear.7 Moreover, there are claims that the application of computer-aided design/computer-aided manufacturing (CAD/CAM) processes can reduce or eliminate errors. With these CAD/ CAM processes, some analogue steps are still required.7,14 More recently, the process of capturing and reproducing a mirror image of a human ear digitally using an intraoral scanner (TRIOS 3, 3Shape) and digital software were explored.7 In the latter study, Ballo et al,.7 introduced a new technique for direct digital impressions of the ear using the TRIOS 3 intraoral scanner and an external marker as an alternative to the traditional method. The digital scan was performed on a volunteer who had two intact ears and no defect.7 Although capturing and reproducing an ear has been well described, literature related to the reproducibility of these procedures is limited. Therefore, the aim of this case report is to describe the digital steps taken to ensure a reproducible method in capturing necessary data and fabrication of an auricular template.
CASE REPORT
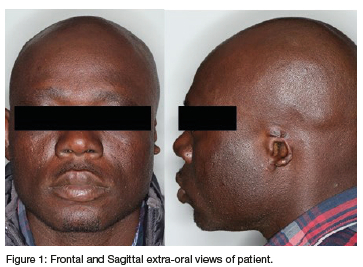
A 34-year-old male was referred to the Maxillofacial Prosthodontic Clinic at Tygerberg Hospital in 2019 for fabrication of a left ear prosthesis (Figure 1). The patient lost his left ear due to trauma. There was no additional damage to the internal ear and the patient's auditory function was unaffected, and he was medically fit.
METHODS AND MATERIALS
1. Digital scanning of the normal ear and affected side with the defect.
A digital intraoral scanner (3 Shape TRIOS 3 Basic, Copenhagen, Denmark) (Figure 2) was used to capture data of both the normal ear on the contralateral side and the affected side in a Standard Tessellation Language (STL) format (Figure 3). The position of an artificial marker (Suremark radiographic stickers, Danville, WA) was placed on the tragus of both the normal ear and the left side of the defect. The tragus was chosen as the landmark for the marker as this was the only anatomical landmark still present on the affected side. The scanning procedure was adopted from the study by Ballo et al,.7
2. Acquired data processing to produce the inverted copy of the normal ear.
The two STL files were obtained and exported into the Autodesk Meshmixer 3-dimensional (3D) modelling software (Meshmixer v2.1, Autodesk, Inc). The software was used to invert the normal ear on the contralateral side (Autodesk Meshmixer).
3. 3D printing of the ear template.
Once the final design was meshed and the final margins merged with the surrounding area, the design was extracted and imported into a 3D printing machine (Phrozen LCD resin 3D printer). An inverted copy of the normal ear was 3D printed in resin (3D Rapid, Monocure) (Figures 4 & 5). The 3D printed ear template was fitted onto the defect area and photographs were taken to verify the fit and position (Figures 4 & 5).
At this stage, the 3D printed ear template was compared with the template that had been traditionally produced via conventional impression (Alginate, Blueprint, Dentisply) and wsxcarving (Dental modelling wax, Kemdent). Comparison of accuracy fit and anatomic representation was done via direct visualisation of how the different templates fit clinically, photographically and comments from the patients.
No modifications of the digital template were required. The final design of the prosthesis was completed digitally and moulds were designed for the fabrication of the prosthesis which was done manually.
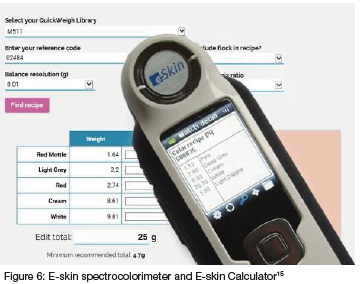
4. Digital skin colour matching & silicon mixing.
An e-Skin spectrocolorimeter and e-Skin calculator15 was used for colour matching (Figure 6). Three areas on the skin, namely the surrounding area of the defect, the forehead, and the nose, were measured and logged into the e-skin meter. E-Skin uses a digital library of nearly 22,000 skin tones to match to patient skin for prosthetic applications. The e-Skin instrument measures skin colour and instantly retrieves and displays on its screen a matching colorant recipe from its database, or the recipe can be retrieved from the online calculator that also saves the data automatically for future reference. The recipe provides the weights of the Part A and Part Β Platinum Silicon 51115 that are required to be mixed with the colours (Figures 7 & 8). The colour was confirmed to match the patient's skin before mixing the silicon.
5. Fabrication of final prosthesis
The mixed silicon and colourants were poured into the mould and which was then invested, processed and the final prosthesis was finished and trimmed. It was then tried on, adjusted where needed and secured in place with medical adhesive (Secure Medical adhesive, Technovent) (Figures 9 & 10). The patient was given home care advice for placement, removal and cleaning of the prosthesis and skin area.
DISCUSSION
Maxillofacial prosthetics is a unique and challenging field in dentistry. Patients afflicted by congenital or acquired maxillofacial defects experience immense psychological anguish as a result of functional and aesthetic deficits. They generally require treatment from a multidisciplinary team in order to select the most appropriate treatment plan, and to execute the rehabilitation in a well-planned and meticulous manner in order to provide them with the best possible functional and aesthetic outcomes. Optimal rehabilitation may be limited by patient-specific issues; however, the main aim is to address both their physical and psychosocial needs and return them to a state of near to normalcy as possible.
Advanced digital technologies (ADTs) at the turn of the millennium showed great promise to the field of maxillofacial prosthetics. The multidisciplinary team embraced ADTs, transforming their approach from an analogue to the integration of such technologies in the rehabilitation of maxillofacial defects. The digital era in which we find ourselves today sees ADTs as securing their place in maxillofacial prosthetics, considerably improving treatment planning and manufacture of maxillofacial prostheses.
This clinical report describes the use of ADT to produce an accurately fitting auricular prosthesis for a patient who lost his ear due to trauma. This technology could decrease the amount of technical skill required to make an ear template. The use of digital software can also decrease laboratory time required and chairside adjustments required.
With the digital scanning phase of the methodology, also known as visualisation or data acquisition, the data of maxillofacial defects may be visualised or acquired by means of medical and non-medical imaging technologies. Nonmedical imaging techniques utilising lasers or intense light beams include intraoral scanners, laser surface scanners, and 3D photogrammetry systems.4,7,16 In this case, the data required to fabricate the ear template was captured using an intraoral scanner (3 Shape). Visualisation may also be accomplished by means of medical imaging including CT, cone beam computed topography (CBCT), and MRI.7,17
Unlike non-medical imaging which only captures surface data, the medical imaging allows for deeper visualisation of the defect; thus, both types of data acquisition are sometimes necessary. According to Ballo et al.,7 only a few studies have incorporated intraoral scanners to make a direct impression of maxillofacial defects; this might be due to the difficulty in stitching the captured images from the intraoral scanners due to lack of clear landmarks on extra-oral soft tissues.7
However, for other digitising systems, data may be directly saved as a STL. Several types of design software are offered by manufacturers for the design of maxillofacial prostheses with extensive design and sculpting tool sets.This allows the virtual clay models to be sculpted with all necessary anatomical details into any form needed.18,17 Commercial and open-source software are available. Once the prosthesis is designed it may be saved as a STL file format or matched virtually to the defect model and appraised prior to manufacturing.
Manufacturing is commonly known as 3D printing or rapid prototyping (RP). Azari and Nikzad19 refer to RP as a "layer by layer technique". This unique layering feature of RP allows for ease of managing formation and production of intricate shapes with internal detail and undercut areas, hence becoming more appealing to prosthodontics. There are several reports in the literature of the efficacy of RP techniques in maxillofacial prosthetics.20,21,22 These techniques can be used for direct and indirect RP. Direct RP refers to "the process of directly printing out the prosthesis or template", while indirect RP refers to "printing out a mould and manually injecting prosthesis material into it".23
The final design of the prosthesis was completed digitally and moulds were designed for the fabrication of the prosthesis which was done manually. The time reported to design and produce the inverted copy of the normal ear digitally using the Autodesk Meshmixer programme took approximately 30 minutes. The time required for fabrication of the 3D printed ear template was approximately 2.5 hours. This is the main advantage of using this current approach to fabricate an auricular prosthesis, namely the shortened time required for the process. The time7 Not only does computer-aided design and CAD/CAM significantly reduce the work time but also the number of appointments.3
In the current case, data of the normal ear as well as the defect, were successfully captured using the TRIOS 3 Basic (3 Shape) intraoral scanner. The digitized ear was inverted and reverse engineered to fit over the defect. In the Ballo et al.,7 study, the digital scan was performed on a volunteer who had two intact ears and no defect. The scarcity of such case reports was initially referenced in a review by Farook et al.,23, and later, echoed by Suresh et al.,25. In both systematic reviews, the Balo et al.,7 study was the only study mentioned, that included the use of intraoral scanning technology, while other similar published literature used either desktop type or commercial laser scanners. To date, limited use of intraoral scanners to fab ricate a prosthetic ear/defect has been reporter. In this case report, the impression taking process was completely digital. Sykes et al,.26, demonstrated the accuracy of a digitally produced ear template by obtaining ratings from blinded observers and by superimposing the 3Dprinted and wax carved templates over each other and measuring volumetric changes.
The normal ear on the contralateral side was accurately inverted and merged with the affected side (the negative volume effect) using the Autodesk Meshmixer software. The prosthesis template was successfully printed using a Phrozen 3D printer. The template was tried-in clinically. It fitted accurately and could be reproduced when required. Tam, McGrath and Ho et al,.24 found that out of 6 ear templates produced via indirect processing, 4 of the 6 had good marginal accuracy and retention, while 6 of the 6 showed symmetry and had good position. In this case, although comparison was not the main objective, the clinicians and the patient preferred the 3D printed template over the wax carved template in terms of appearance and accuracy of fit.
CONCLUSION
This case report describes the use of intraoral scanners to make a digital impression and template of an ear for a patient with a missing ear. The TRIOS 3 Basic (3Shape) intraoral scanner successfully captured the anatomy of the normal ear and the affected ear. The 3D printed ear template resulted in an accurate anatomical representation. Two of the authors have clinical experience of fabricating maxillofacial prosthesis using the traditional method with some experience of the newer digital technology as described in this case report. From the successful outcome of this described treatment, they agreed that this digital method is: 1) more accurate; 2) less time-consuming than traditional methods; and 3) less invasive, and thus more accepted by patients. Further exploration of the incorporation and use of digital methods for the full range of maxillofacial rehabilitation is recommended.
ACKNOWLEDGEMENTS
The authors acknowledge the clinical guidance of Drs Sandile Mpungose & Ian Gründling.
No conflict of interest to declare.
REFERENCES
1. Singh A, Ghosh S, Kar S, Ahmed I. Silicone prosthesis for a patient with unilateral ear defect: A Clinical case report. Eur J Gen Dent. 2013; 2: 315-9. [ Links ]
2. Hatamleh M, Haylock C, Watson J, Watts D. Maxillofacial prosthetic rehabilitation in the UK: A survey of maxillofacial prosthetists' and technologists' attitudes and opinions. Int J Oral Maxillofac Surg. 2010; 39: 1186-92. [ Links ]
3. Bi Y Zhou M, Wei H. Digital workflow for auricular prosthesis fabrication with a negative mold. J Prosthet Dent. 2022. [ Links ]
4. Watson J, Hatamleh M. Complete integration of technology for improved reproduction of auricular prostheses. J Prosthet Dent. 2014; 111: 430-36. [ Links ]
5. Wang RR, Andres CJ. Hemifacial microsomia and treatment options for auricular replacement: a review of the literature. J Prosthet Dent. 1999; 82: 197-204. [ Links ]
6. Coward TJ, Richards R, Scott BJ. Development of a Morphing Technique for Predicting the Position and Size of an Artificial Ear in Hemifacial Microsomia Patients, Int J Prosthodont. 2014; 27(5): 451-57. [ Links ]
7. Ballo AM, Nguyen CT, Lee VS. Digital workflow of auricular rehabilitation: A technical report using an intraoral scanner. 2019. J Prosthodont 28: 596-600, [ Links ]
8. Taylor TD, editor. Clinical maxillofacial prosthetics, Volume 1. Chicago: Quintessence; 2000. [ Links ]
9. Mohammed IM, Tatineni J, Cadd B, Peart G, Gibson I. Advanced Auricular Prosthesis Development by 3D Modelling and ΜuIti-material Printing. InDesTech 2016: Proceedings of the International Conference on Design and Technology 2017; 37-43. [ Links ]
10. Hooper SM, Westcott T, Evans PLL, Bocca AR Jagger DC. Implant-supported facial prostheses provided by a maxillofacial unit in a U.K. regional hospital: Longevity and patient opinions. J Prosthodont. 2005; 14(1): 32-8. [ Links ]
11. Mathews MF, Sutton AJ, Smith RM. The auricular impression: An alternate technique. J Prosthodont. 2000; 9(2): 106-9. [ Links ]
12. Suaste-Górnez Ε, Roldan GR, Cruz HR, Jimenez OT. Developing an ear prosthesis fabricated in polyvinyl id ene flouride by a 3D Printer with sensory intrinsic properties of pressure and temperature. Sensors. 2016; 16(3): 332 [ Links ]
13. Coward, TJ, Watson, RM, Wilkinson, IC. Fabrication of a wax ear by rapid-process modeling using stereolithography. Int J Prosthodont. 1999; 12(1): 20-7, [ Links ]
14. AI Mardini M, Ercoli C, Graser GN. A technique to produce a mirror-image wax pattern of an ear using rapid prototyping technology. J Prosthet Dent. 2005; 94(2): 195-98. [ Links ]
15. Technovent. Spectromatch Systems. Technovent Catalogue [Internet]. 2020; www.technovent.com Accessed [ Links ]
16. Liu H, Bai S, Yu X, Zhao Y. Combined use of a facial scanner and intraoral scanner to acquire a digital scan for the fabrication of an orbital prosthesis. J Prosthet Dent, 2019; 121(3): 531-34. [ Links ]
17. Elbashti ME, Sumita Yl, Kelimu S, Aswehlee AM, Awuti S, Hattori M, Taniguchi H, Application of digital technologies in maxillofacial prosthetics literature: A 10-year observation of five selected prosthodontics journals. Int J Prosthodont. 2019; 32(1): 45-50. [ Links ]
18. Kim M, Lee J, Shin S. Fabricating an obturator using rapid prototyping to design the framework: A case report. Int J Prosthodont. 2014; 27(5): 439-41. [ Links ]
19. Azari A, Nikzad S. The evolution of rapid prototyping in dentistry: A review. Rapid Prototyp J. 2009; 15(3): 216-25. [ Links ]
20. Eggbeer D. The computer aided design and fabrication of facial prostheses [thesis], Cardiff, UK: University of Wales Institute; 2008. [ Links ]
21. Taniguchi H, Sumita Yl, Otomaru T, Minamisawa N, Inohara K. Maxillofacial prosthodontics-current treatment and research. Prosthodont Res Prac. 2008; 7: 132-34. [ Links ]
22. Soriano CM, Vega PC, Devesa AE, Salas EJ, López JL. Frequency and type of digital procedures used for the intraoral prosthetic rehabilitation of patients with head and neck cancer: A systematic review. J Prosthet Dent. 2022 [Epub 2021 January 09]; 127(5): 811-15. [ Links ]
23. Farook TH, Jamayet NB, Abdullah JY Rajion ZA, Alam MK. A systematic review of the computerised tools and digital techniques applied to fabricate nasal, auricular, orbital and ocular prostheses for facial defect rehabilitation. J Stomatol Oral and Maxillofac Surg. 2020; 121: 268-77. [ Links ]
24. Tam CK, McGrath CP, Ho SMY, Pow EHN, Luk HWK, Cheung LK. Psychosocial and quality of life outcomes of prosthetic auricular rehabilitation with CAD/CAM technology. Int J Dent. 2014. [ Links ]
25. Suresh N, Janakiram C, Nayar S, Krishnapriya VN, Mathew A. Effectiveness of digital data acquisition technologies in the fabrication of maxillofacial prostheses-A systematic review. Journal of Oral Biology and Craniofacial Research. 2022 Jan 1;12(1):208-15. [ Links ]














