Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.78 no.2 Johannesburg mar. 2023
LITERATURE REVIEW WITH AN ILLUSTRATIVE CASE
Proteus Syndrome - A one in a million occurrence
LM SykesI; C BradfieldII
IBSc, BDS, MDent, FCD(SA), IRENSA, Dip Forensic Path, Dip ESMEA, FCD (CD), Head of Department of Prosthodontics, University of Pretoria
IIB Tech, BChD, Dip Aesthetics; Registrar Department of Prosthodontics,
ABSTRACT
The syndrome is named after the Greek sea-god Proteus, who could change his shape.
Proteus Syndrome (PS) is a rare condition with an incidence of less than 1 in 1 million people. It is characterized by variable, multifocal overgrowth of bones, skin, or other tissue derived from any of the three germinal layers. It is generally not apparent at birth, but signs develop rapidly from as early as 6 months and get more severe with age. Craniofacial deformities are less frequent but overgrowth of facial bones leads to disfigurement, malocclusion and a number of other oral and dental anomalies. The following case report of a young boy with PS was written for three reasons. Firstly, it will describe this unusual condition to colleagues who have never encountered patients with the syndrome. It then stresses the importance of a holistic approach to treatment planning. This entails addressing the immediate needs, and then basing the definitive treatment on considerations of possible short- and longterm, patient-related developments. Finally, it illustrates how a complex case was treated successfully with conservative management using modifications of standard clinical procedures.
Keywords: Proteus Syndrome; Craniofacial Deformity; Akt1 Gene Mutation
INTRODUCTION
Proteus Syndrome (PS) is a sporadic condition caused by the AKT1 gene mutation, and characterized by highly variable, multifocal, disproportionate and asymmetric overgrowth of the bones, skin, or any other tissues, derived from any of the three germinal layers.1, 2 3 The affected organs and tissues grow faster than the surrounding areas leading to both sizeable physical distortion as well as impaired and / or limited movement. It is compounded by the fact that growth is generally asymmetrical and affects the right and left sides of the body differently. It may affect almost any part of the body, but the most common sites are the bones in the limbs, skull, and spine, followed by the skin1. The pattern of enlargement varies greatly, especially in the skin where it presents with a characteristic feature known as cerebriform connective tissue nevi, which are thick, raised, and deeply grooved lesions. These usually occurs on the soles of the feet and are rarely ever seen in any other condition, as well as epidermal nevi, vascular malformations, and dysregulated adipose tissue.1,3 Other common manifestations include macrodactyly (partial gigantism of hands or feet), vertebral abnormalities, asymmetric muscle and limb growth with length discrepancies, hyperostosis, and restricted movement.1,2,3 Some people with PS have neurological abnormalities, including intellectual disability, seizures, brain malformations and vision loss.1,3,4 Many also display distinctive facial features such as dolichocephaly / long faces, down-slanting palpebral fissures on the outer corners of the eyes, ptosis, low nasal bridges with wide or anteverted nares, and an open-mouth expression.1 It appears that these characteristics are more commonly seen in those who also have neurological symptoms, but the reason for this is not known. It is also unclear how or why these features are related to the abnormal growth.1
Craniofacial deformities are less frequent than the skeletal abnormalities, and are associated with exostoses and overgrowth of membranous bones (30% of patients), leading to dentofacial disfigurement and often malocclusion.4 The dentition is reported to be involved in approximately 18.6% of patients, with the most common features being tooth agenesis, ectopia, gingival hypertrophy, crowding, malocclusion, multiple frenula, high arched palate, asymmetrical hypertrophied tongue and enamel hyperplasia.4
INCIDENCE AND PRESENTATION AT BIRTH
Proteus Syndrome is a rare condition of unknown aetiology, with an incidence of less than 1 in 1 million people, thus very few cases have been reported in the literature.3 It is generally not apparent at birth, with less than 17.5% of neonates showing any early signs of asymmetry, however these develop rapidly in early childhood.3 Overgrowth becomes apparent between the ages of 6 and 18 months and gets more severe with age, although in some cases it has been seen to stabilize in adolescence.1,2,3 It has a male to female sex ratio of 1.9:1.3 Of interest is that the change is not inherited but occurs randomly in one cell during the early stages of foetal development, as such, it does not run in families.1 The condition is postulated to arise as a result of a mutation in the AKT1 gene, where some cells will have the mutation and other cells will not. This finding of a mixture of cells in the absences of a genetic mutation, is known as mosaicism.1 The AKT1 gene helps regulate cell growth, division, proliferation, and death, thus if an abnormality in this gene disrupts the cell's ability to regulate its own growth, it could then grow and divide abnormally leading to the characteristic features seen in patients with PS.1
SIMILAR CONDITIONS AND DIAGNOSIS
Proteus syndrome may be over diagnosed, or misdiagnosed, as individuals with other conditions featuring unilateral overgrowth such as ossifying fibroma, osseous dysplasia, fibrous dysplasia, neurofibromatosis type 1, Kippel-Trénaunay syndrome, hemihyperplasia-multiple lipomatosis, familial lipomatosis, symmetric lipomatosis, epidermal nevus, Maffucci syndrome, and Bannayan-Riley-Ruvalcaba syndromes have often been mistakenly diagnosed as Proteus syndrome.1,2,4,5 There are strict guidelines to follow in order to make a definitive diagnosis of PS, and all of these need to be present to confirm the classification. These include: mosaic distribution of lesions; sporadic occurrence; progressive course; and rapid asymmetric and disproportionate overgrowth. It also needs to have additional specific criteria from the categories (A, B and C), of which there must be at least 1 feature from category A, or two from B or three from C.3
The recommended diagnostic tests for patients with suspected PS include clinical photographs, initial skeletal surveys and follow up comparisons. Tests should consist of radiographs of affected areas, magnetic resonance imaging (MRI) of the chest, abdomen and pelvis (to exclude aggressive intra-abdominal lymphomas), dermatological evaluation and biopsies if indicated. Additional MRIs of the central nervous system may help identify neurological abnormalities that can be associated with mental deficiencies and / or seizures.1,2,3 Chest X-rays, Computed tomography (CT) imaging, pulmonary function tests, and selected genetic tests aid in identification of other genetic disorders. Treatment may involve orthopaedic consultation and operations where needed, continuous paediatric management and referral to family counselling and support groups.2,3,5 The different skeletal problems may be addressed by various surgical procedures such as "epiphyseodesus for asymmetrical epiphyseal growth, reduction osteotomies to shorten or straighten long bones, shoe lifts for mild leg length discrepancies, prosthetic joint replacement, and spinal fusion to prevent development of kyphoscoliosis".3 A further complicating factor associated with the rapid overgrowth of long bones is that they have abnormally thin cortices, and deficiencies of the overlying soft tissue which do not grow at the same rate, and adds to the restricted mobility.3
A recent systematic review of maxillofacial manifestations of PS (2021) found 14 papers that reported on patients with PS.4 Most of them were case reports of single patients, and focused specifically on the imaging modalities used to help in the diagnosis.4 Conventional panoramic radiographs were generally used as they provide a large amount of information such as the presence of impactions, tooth agenesis, root dilacerations, resorption, ectopic eruption, asymmetric dental maturation and asymmetric enlargement of the alveolar bones.4 Lateral cephalometric radiographs and CT scans were used for treatment planning or when any form of intervention was envisaged. Intraoral findings in the 14 cases included the following: malocclusion (2 patients); dental crowding (2); crossbite (2); dental ectopia, rotations, enamel hypoplasia, tooth agenesis, impactions (2); high arched palate, unilaterally enlarged alveolar bone (2); gingival hyperplasia (3); unilateral enlargement of the tongue (3); maxillary or mandibular prominence (4); jaw atresia (1); anterior open bite, teeth in infraocclusion (2); tilted occlusal plane, enlarged zygoma (1), delayed eruption, deviated midline, osteomas, unilateral enamel hypoplasia (1). Most of the papers reported that the teeth present were normal in size and shape.4
POTENTIAL COMPLICATIONS
Patients with PS have an increased risk of developing various types of benign tumours and blood clots, most notably thromboembolism. If these become dislodged from the limb vessels they may travel to the lungs causing respiratory complications and pulmonary emboli. The latter are a common cause of premature death in these patients due to the compounded burden of vascular malformations, frequent surgical procedures, and restricted mobility.1,2 Antithrombotic prophylaxis is recommended for any surgical interventions to try prevent this.3
CASE REPORT
A 29-year old male patient who had been diagnosed with PS by molecular genetic testing at the age of 3 years, presented to the dentist requesting a new denture. The old one was not fitting him anymore.
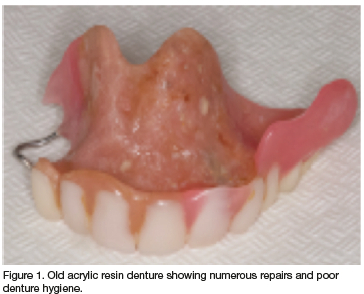
The old denture was reportedly more than 10 years old, badly stained, covered with plaque, and had signs of previous repairs (Figure 1). It was difficult to assess the denture fit due to his restricted mouth opening, however once it was inserted it was clear that this prosthesis would never fit due to the numerous bony overgrowths, undercut areas and exostoses that had developed. Further intraoral examination revealed that he had very few remaining teeth (14 and 15 in the maxilla, and 31-34 and 42-44 in the mandible) with a 19 mm diastema between the 42 and 31 (Figures 2 and 3). The other teeth had been extracted over the years, but neither he, nor his mother could elaborate on how many teeth had been lost to establish if he had developed a full complement of teeth initially.
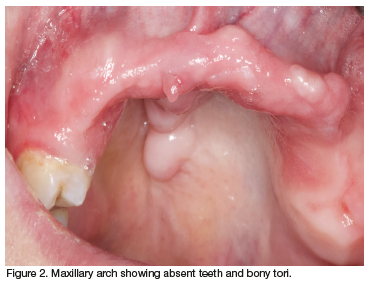
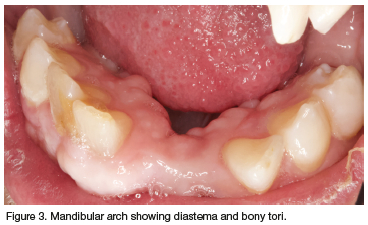
His mother could also not give any accurate details regarding time of eruption or eruption patterns. The remaining teeth all appeared normal in size and structure, but it was not possible to assess their roots, bony support or internal morphology as the restricted mouth opening and bony interferences hindered the insertion of a radiograph sensor and the possibility of capturing any meaningful images. An additional obstacle was his larger than normal tongue with this characteristic enlargement of the fungiform papillae.
Attempts at taking a panoramic radiograph or CBCT also met with no success as he had a large hump on his posterior neck / upper back that obstructed the moving arm of the machines (*see related comments). An appointment was made for him to have a Lodox X-Ray, however on the day he had a severe migraine** and this had to be cancelled. It was never rescheduled as the clinicians did not feel it justified to subject him to the stress and radiation exposure merely for the sake of their interest and records. Furthermore, the final treatment selected could be carried out adequately without having these images performed.
Extra-oral examination showed the classical facial features of dolichocephaly, downward slanting palpebral fissures on the outer corners of his eyes, ptosis, low nasal bridge with wide or anteverted nares, and an open-mouth expression.1 He also had numerous soft tissue "blebs" around the eyelids. The patient also had deformities of his hands, arms, legs, feet, back and spine. The former two accounted for his difficulty with oral hygiene measures, while the latter made walking, and sitting in the dental chair / x-ray units a struggle*. A further complication was that he experienced frequent severe headaches and migraines (**see related comments), resulting in many of his scheduled appointments being cut short or cancelled.
TREATMENT OPTIONS AND RESPECTIVE LIMITATIONS
Due to the rarity of the condition, there was very little dental literature to consult when debating the various treatment options. The thought processes and arguments below were based on personal clinical experiences through treating other patients with similar bone or soft tissue abnormalities and atypical growth patterns.
The first consideration in any patient's treatment plan should be to determine if any clinical intervention is needed and possible to perform. Except for emergency care, no treatment is always an option. However, in this case the missing teeth were in the anterior region of the maxilla and needed to be replaced for speech, aesthetics, mastication and to prevent the opposing mandibular teeth from over-erupting. The most conservative choice was to fabricate a removable acrylic resin partial denture. These are quick and relatively inexpensive to make, require minimal tooth preparation, and are easy to insert and remove for oral hygiene purposes.
A chrome cobalt partial denture would ordinarily have been preferred in young patients if they have enough healthy abutment teeth. They are stronger, less damaging to the dentition and gingival tissues, easier to keep clean and reportedly more comfortable to wear. However, in this situation, the patient only had two remaining maxillary teeth, and the added hindrance of constant and unpredictable bone growth in the jaws. An acrylic resin denture was more suitable as it would be easier to adapt and modify to accommodate the ever-changing denture bearing foundation. It was essential to stress to the patient and his mother the need for regular review visits so that the dentist could monitor his condition and adjust the dentures when necessary to avoid them impinging or causing pressure and ulcerations on areas of growth. Denture modifications are relatively simple to perform in acrylic resin dentures, but almost impossible with chrome cobalt.
A further option considered was to manufacture an acrylic resin denture and line its fitting surface with a resilient material such as Molloplast® (Buffalo Dental manufacturing Inc.) or GC Reline ® (GC Australasia) which may be more accommodating of the ever-changing denture bearing area. However additional resilient layers make the denture bulkier, and the resin layer thinner and weaker. They are seldom used in partial dentures. The extra thickness would also have encroached on the interalveolar space, which was already limited due to the excess bone growth in both his jaws. Furthermore, it would have been more difficult to insert and remove due to his restricted mouth opening, they are less easy to clean and adjust, and are more prone to microorganism contamination.
Fixed bridgework was contraindicated due to the long span that crossed the midline, lack of abutment teeth in the second quadrant, and poor condition of the remaining two maxillary teeth. Even if there had been enough teeth to support a bridge, any bone growth could potentially affect their position, which in turn would create stresses within the bridge framework. This may result in bone loss, tooth loosening, debonding, bridge fracture, and perhaps altered occlusion. On the other hand, if the growth was slow, there was a possibility that the functional units would adapt and there would be no adverse consequences. However, there was no way of predicting the future and the question would be if it was a justifiable risk to take.
Implants were considered as there appeared to be enough bone and the patient was relatively healthy. However, there were far too many factors that ruled against this option. Firstly, the clinicians would have to find a way of taking radiographs to assess bone quality, quantity and to plan for implant placement*. Furthermore, the same concerns about splinting teeth together in bridgework would apply to implants regarding the possibility of bone growth altering their position or angulation. An alternative may have been to keep the implants separate and use them to retain a partial overdenture.
This option was ruled out due to the additional space requirements of the latter. Literature recommends a minimum of 15 mm per arch inter-alveolar space to accommodate an implant-supported prosthesis.6,7 This patient had only 10mm in the second quadrant and would thus need to undergo surgical bone reduction either prior to or at the time of the implant placement. They could also later become submerged if bone grew around the cervical areas, and would need periodic peri-implant alveoplasty to keep their margins exposed. This would risk damaging the threads or the surface of the implant bodies in their most critical area. Implants also need to be positioned at the same height, parallel to the alveolar ridge and equidistant from the midline in order to limit the lateral forces exerted during mastication and to maintain prosthesis stability. If this is not accomplished there will be torsional forces and stresses on the abutments and / or the superstructure leading to prosthesis fracture and possible implant loss.6,7 With his limited dexterity, and mouth opening, both placement and restoration of the implants as well as subsequent maintenance and oral hygiene were a major concern.
A final consideration is that patients with PS often suffer from vascular complications. Surgery and new bone formation may impinge on vital blood vessels. This in turn may lead to reduced bone turnover and compromise osseointegration. It may add to the already increased risk of venous thrombi, with dire consequences.
DEFINITIVE DENTAL TREATMENT
The patient was accustomed to wearing an acrylic resin removable partial maxillary denture, and based on the above consideration, it was decided that a new one would be the best option for his current needs. The primary impression turned out to be very difficult to take due to his limited mouth opening and atypical ridge shape. (All dental visits were difficult as the patient could not sit comfortably in the dental chair*, had frequent migraines** / panic attacks during the session necessitating them being aborted, and struggled opening his mouth and keeping it open.) After numerous attempts with various modified trays (Figure 4) the dentist decided to make use of his current denture as a special tray. This was trimmed down on the fitting surface to create a space over the areas where his ridges had grown as well as for the impression material. The borders were built up with green stick modelling compound (Kerr Impression compound®, Henry Shein Inc.) and an impression was taken using an irreversible hydrocolloid (Blueprint impression material®, Dentsply Inc).

To limit the number of visits needed, bite blocks were fabricated on the primary cast and at the following visit a mandibular impression was taken along with a jaw relation recording and tooth selection. At the next session the waxed denture was tried in and adjusted at the chairside until all parties were satisfied with the fit, tooth position, speech and aesthetics. The dentist then used this trial denture as a special tray and took a "pick up impression" in it with a light bodied silicone (Coltene President® Silicon impression material Light body, Whaledent Affinis) to capture an accurate secondary impression and pour the final cast (Figure 5). If this procedure is carried out, the clinician must identify and mark the post dam area on the palate, ensure it is transferred onto the intaglio surface of the impression, and scribe it onto the master cast.

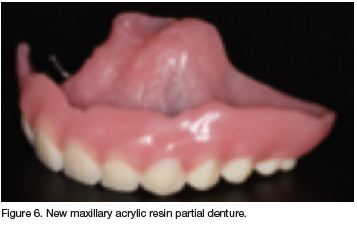
Clasp were added to engage the 14,15 and the denture was processed and delivered (Figure 6). The patient was ecstatic with his "new look" as well as all the attention he had received from the treating team (Figure 7).

He was taught how to insert and remove his dentures, and given instructions on cleaning. A large soft scrubbing brush was adapted by adding a "Velcro" strap to it. This made it easier for him to hold and he was advised to use it in place of the smaller toothbrush to clean his denture.
His mother was counselled on the need to help him maintain intra-oral hygiene and to bring him back for regular maintenance prophylaxis and denture adjustments.
DISCUSSION AND CONCLUSIONS
After 2 months, the patient returned for a recall visit. He was managing well inserting, removing and functioning with his new prosthesis and was overjoyed with the positive feedback he had received from family and friends. The clinicians were still eager to view radiographs of his remaining teeth, and the patient, who was now used to having a prosthesis in his mouth, agreed to another attempt at this. The effort and outcome proved to be more valuable than anticipated. The radiographs confirmed that the 15 and 25 were fully formed and of normal structure (Figure 8).
The second view revealed an impacted / submerged 16 which was not evident clinically (Figure 9). The intriguing feature was that the tooth appeared to have not erupted, and was surrounded by bone and soft tissue, yet it had an inexplicable occlusal radiopacity which resembled a restoration. A possible explanation was that this tooth may have erupted normally and been restored at some time in the patient's past. The tissues could then have grown over the tooth resulting in it now being embedded, and thus seemingly impacted. The superior position may have resulted if the 14 and 15 were carried downwards with the growing bone. Another explanation was that it may have been an artefact due to superimposition of the cusps. A CBCT was performed with a metal marker (the ball clasp on his new denture) in the patient's mouth for reference. It showed the radiopacity clearly in a number of views, and in many it was more opaque than the metal (Figure 10).

This case presented a young man suffering from PS who had many dental and skeletal limitations. It highlights the need for clinicians to have a holistic and compassionate approach towards management of all persons under their care. They need to spend time assessing each new patient carefully and thoroughly at the initial consultation. Thereafter the treatment options and definitive plan must be based on an appraisal of the individual's needs, desires, physical / oral condition, time, finances, and physical limitations, and maintenance requirements, as well as their own skills, facilities, capabilities and ethical values. In this way they will not only be practicing in a caring and compassionate manner, but will also benefit from the peace of mind that comes with knowing they have done their best.
ETHICAL STATEMENT
The patient was asked if his case and illustrations could be used for publication purposes. He was assured of confidentiality and anonymity, and that all illustrations would conceal his identity. Both he and his mother gave full consent to this.
REFERENCES
1. Biesecker L. The challenges of Proteus Syndrome: Diagnosis and management. Eu J Hum Genet; 2006. 14(11):1151-7. [ Links ]
2. Jamis-Dow CA., Turner J, Biesecker LG and Choyke PL. Radiologic manifestations of Proteus syndrome. Radiographics. 2004. Vol 23(4):1051-1068. [ Links ]
3. Cohen MJ. 2005. Proteus Syndrome: An Update. Am J of Med Genet; 137C:38-52 [ Links ]
4. Mun Munhoz L, Arita ES, Nishimura DA, et al,. Maxillofacial manifestations of Proteus syndrome: a systemic review with a case report. Oral Radiol.2021. 37: 2-12. [ Links ]
5. Biesecker LG, Happle R, Mulliken JB, et al,. Proteus syndrome: diagnostic criteria, differential diagnosis, and patient evaluation. Am J Med Genet.1999 Jun 11;84(5):389-95. Review. [ Links ]
6. Misch CE, Goodacre CJ, Finley JM, et al,. Consensus conference panel report: crown-height space guidelines for implant dentistry-part 1. Implant dentistry. 2005;14(4):312-318. [ Links ]
7. Tosi LL, Sapp JC, Allen ES, O'Keefe RJ, et al,. Assessment and management of the orthopedic and other complications of Proteus syndrome. J Children's Ortho: Official J of Eur Paed Orthopaedic Soc (epos). 2011;5(5):319-327. doi:10.1007/s11832-011-0350-6. [ Links ]
 Correspondence:
Correspondence:
Leanne Sykes
Orchid: https://orcid.org/0000-0002-2002-6238
Email: Leanne.sykes@up.ac.za
Authors contributions
LM Sykes Primary author 50%
C Bradfield Second author 50%














