Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.78 n.1 Johannesburg Feb. 2023
RESEARCH
Analysis of the Mental Foramen and Inferior Alveolar Canal pattern based on CBCT data
N VermaI; M KaushikII; S ElkantiIII; N MehraIV; A GeorgeV
IMDS, Senior Lecturer; Department of Conservative Dentistry and Endodontics Army College of Dental Sciences, Secunderabad, India 6304215714; Orcid ID - 0000-000-22247-5774; (nv89168@gmail.com)
IIMDS, Prof & Head; Department of Conservative Dentistry and Endodontics Army College of Dental Sciences, Secunderabad, India 9391010325; Orcid ID - 0000-0001-9518-8007; (mamkaushik@gmail.com)
IIIMDS, Reader; Department of Conservative Dentistry and Endodontics Army College of Dental Sciences, Secunderabad, India 8790986380; Orcid ID -0000-0001-6082-6873; (soujanyae.17@gmail.com)
IVMDS, Reader; Department of Conservative Dentistry and Endodontics Army College of Dental Sciences, Secunderabad, India; 9553149417; Orcid ID - 0000-0003-3759-8264; (dr.nehamehra86@gmail.com)
VMDS, Senior Lecturer; Department of Conservative Dentistry and Endodontics Army College of Dental Sciences, Secunderabad, India 9553358706; Orcid ID -0000-0002-8486-8186; (alvgeo09@gmail.com)
ABSTRACT
INTRODUCTION: The mental foramen is located in a position where certain dental procedures may cause inadvertent damage to the mental nerve and lead to disorders of sensory functions such as altered sensa-tion, complete numbness, and neuropathic pain, which are uncommon but severe treatment complications with significant medico-legal implications. Hence thorough knowledge of its anatomical relation to its surrounding structures is critical while undertaking dental procedures
AIM AND OBJECTIVE: To investigate the size, shape, and position of the mental foramen (MF), its distance from adjacent teeth and mandibular borders, and the pattern of the inferior alveolar canal using CBCT in the Indian subpopulation
DESIGN: This was a retrospective, cross-sectional study
METHODS: The study evaluated 310 CBCT scans (179 males, 131 females) in axial, sagittal, and coronal planes. CBCT scans were evaluated, mapped and measured for all the parameters listed above based on age and sex. Data were analyzed using ANOVA, independent't-test, and chi-square test
RESULTS AND CONCLUSION: The size of MF is independent of age and sex; the most frequent shape of MF was Type III (round); location was below the apex of the second premolar (p>0.05). The distance of MF from the nearest root apex decreased with an increase in age and more in females than males (p>0.05). Inferior Alveolar Nerve Canal (IAC) pattern was perpendicular, and linear patterns of exit at MF were more common than anterior loops in all age groups
Keywords: Anterior loop, CBCT, Mental Foramen, Pattern, Position
INTRODUCTION
The inferior alveolar nerve is the largest branch of the mandibular nerve, which traverses via the mandibular canal along with the inferior alveolar artery and terminates into the mental nerve (MN) and incisive nerve. The mental nerve, along with the mental artery and vein, exists through the mental foramen (MF), at the anterolateral surface of the body of the mandible. 2 It provides sensory innervation to the soft tissues of the chin, lower lip, labial mucosa, lower canines, and incisors. 2-5
The IAN exits at the mental canal (MeC), and splits into the incisive nerve and the MN. The exit path at the MF is seen in three different patterns; linear or straight, perpendicular or vertical, and anterior loop (AL). 6 7
The usual location of the MF is between the apices of the first and second premolars or just below the apex of the second premolar.3, 4 The accurate identification of the MF is essential for diagnostic, clinical, and surgical procedures of the mandible. To untrained eyes, the MF may be mistaken for radiolucent lesions around the apices of the mandibular premolars and lead to misdiagnosis and incorrect interventions.6 Dental procedures like regional anesthesia, flap elevation, osteotomy, insertion of dental implants, surgical removal of roots, teeth, cysts, tumour or orthognathic surgeries, fixation of bone fractures procedures, non-surgical and surgical endodontic procedures require the operator to have thorough knowledge about the MF, the exit pattern of the nerve and its relation to the surrounding area.2,4,6,8
Endodontic procedures such as cleaning and shaping may lead to over instrumentation, inadvertent extrusion of medicament, irrigants, or chemicals used for root canal treatment can lead to complications from pain and swelling to mental nerve paraesthesia.14 Gutta percha though an inert root filling material, can generate paraesthesia due to thermal irritation and nerve compression by overfilling thermoplastic guttapercha.15
The mental nerve is a sensory nerve, and because its anatomic location, any invasive procedure performed in this region may damage the neurovascular bundles2, causing altered sensation, complete numbness, and even neuropathic pain. These complications interference with speech, eating, drinking, shaving, or make-up application and have medico-legal implications.16
Therefore, the knowledge of the presence and location of the mental foramen is essential for all dental procedures in the mandibular premolar area. This study aimed to investigate the size, shape, and position of the mental foramen, its distance from adjacent teeth and mandibular borders, and the pattern of the inferior alveolar canal using cone-beam computed tomography (CBCT) data in an Indian subpopulation.
MATERIALS AND METHODS
Exempt status was obtained for the study by the Institutional Review Board (ACDS/IRB/13/JAN/2021). The study was a retrospective analysis, and 402 CBCT scans were retrieved. All the scans were shot at a voxel size of 150pm x150 µm x150 µm and exposure settings of and 90 kV, 15 mA, 14s with Care stream C S 8100 (CS 3D version suite 3.10.8.0) (Care Stream Dental LLC, Atlanta, GA). The scan centre takes a blanket consent from all patients to use their data for scientific purposes.
Inclusion criteria for the CBCT scans were: South Indian ethnicity (verified by surname), visibility of MF, presence of permanent mandibular premolars and first mandibular molars, age group 20 years or more, lack of lesion in the apical area of premolars, and MF, and lack of bone resorption. Exclusion criteria: patients under 20 years, with mixed dentition, supernumerary teeth in the mental foramen region, and CBCT scans with poor film quality, errors, and artifacts concealing visibility of structures in the mandible.
As this is an observational study, from a CBCT center in Secunderabad, where the ethnicity of the paients is South Indian. The sample size determined was based on previous studies.2, 6
All the scans were assessed for eligibility against selection criteria by a single observer to reduce bias. A total of 310 scans fulfilling the inclusion and exclusion criteria were included in the study and categorized into three age groups 20-45 years, 46-60 years, and more than 60 years.
The CBCT scans were screened in sagittal, coronal, and axial views, and various measurements and observations were recorded.
In the sagittal view (Figure 1), the anteroposterior position of MF was recorded as the following (Tebo and Telford:
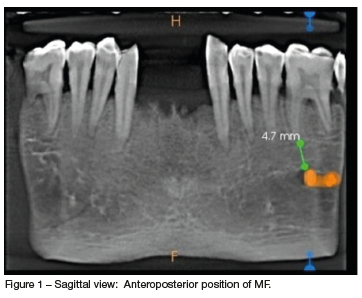
(a) Below 1st premolar
(b) Between 1st and 2nd premolar
(c) Below 2nd premolar
(d) Between 2nd premolar and 1st molar
(e) Below 1st molar
The distance between the superior margin of MF and the root apex of the nearest tooth (either premolar or mesial root of the mandibular first molar) was measured and recorded.
In the coronal view and axial view (Figure 2), the vertical [V] and horizontal [H] diameters of the MF were determined, respectively. The ratio (H: V) was used to classify the form of MF into three types based on previous studies 2 12, 13 -
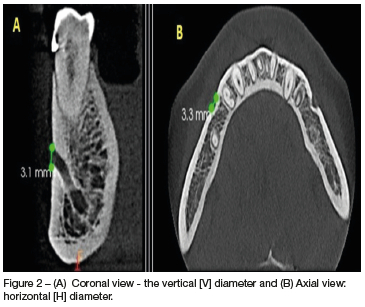
1. Oval horizontal form (Type I, H: V > 1.24)
2. Oval vertical form (Type II, H: V < 0.76)
3. Round form (Type III, when 0.76 < H: V > 1.24)
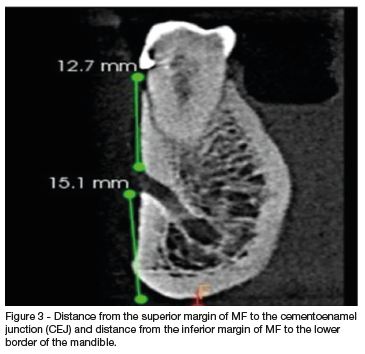
The distance from the superior margin of MF to the cementoenamel junction (CEJ) and distance from the inferior margin of MF to the lower border of the mandible was measured in the coronal view (Figure 3).
The inferior alveolar nerve canal (IAC) is classified based on its exit path into three patterns: linear, perpendicular, and anterior loop (Figure 4). The linear or straight pattern with the mental canal (MeC) shows a slight curve opening directly through the mental foramen.7 The perpendicular or vertical patterns with the mental canal bends (MeC) perpendicularly to the mental foramen.8 The anterior loop is an extension of the inferior alveolar nerve, anterior to the mental foramen, before exiting the canal, traversing inferiorly and anteriorly to it. 9-11

All the data was tabulated and recorded in an excel sheet (MS Office 2010).
STATISTICAL ANALYSIS
The data were subjected to analysis using Statistical Package for the Social Sciences (SPSS-20.0) software package (IBM, Chicago, USA). Results showing p< 0.05 as statistically significant.
One-way ANOVA test and Independent t-test were applied to compare the mental foramen size, the distance of MF from the nearest root apex, and distance from the lower mandibular border with age and sex. A Chi-square test was applied to compare the mental foramen type (based on its shape), the position of the mental foramen, and the prevalence of the Inferior Alveolar Canal pattern.
RESULTS
Descriptive analysis of the demographic data revealed the study participants as 179 male and 131 female. The distribution consisted of ages 20- 45 years, 46-60 years, and more than 60 years, with 228, 62, and 20 scans, respectively.
The size of the mental foramen in terms of its horizontal and vertical diameter varied with different age groups and sex. One-way ANOVA test and independent 't-test showed no significant differences (p>0.05) in values of the horizontal and vertical diameters as well as the H: V ratio (Table I) on both sides with the age and sex of participants. The shape of the MF was Type III (round) irrespective of age and sex (Table II).
The most common position of mental foramen apropos the adjacent teeth on the left and right side of the mandible was found to be below the second premolar irrespective of age and sex. (p>0.05) (Table III and Table IV).
The distance of MF from CEJ with side or sex did not significantly differ. However, its distance to the lower border of the mandibular showed a statistically significant difference on the right side concerning age (p< 0.05 and sex r (p<0.05) (Table V). The distance of MF from adjacent teeth decreased with age and more in females than males, the results were marginally different (p>0.05).
The most commonly observed IAC pattern was perpendicular in the age group 20-45 years, linear in 46-60 years, and for the age group >60 years, linear on the left side and perpendicular on the right side.
The anterior loop pattern was the least prevalent. These results were significant on the left side regarding age (p-value <0.05). Based on sex, the most common pattern in males and females on both sides was perpendicular, followed by a linear pattern with no statistically significant difference (Table VI).
DISCUSSION
The accurate identification of the MF is essential for diagnostic, clinical, and surgical procedures of the mandible. The analysis of the mental foramen and inferior alveolar canal can be done using techniques like manual palpation, direct visualization during surgery, cadaveric dissection, panoramic radiographs, periapical radiographs, magnetic resonance imaging (MRI), computed tomography (CT), ultrasound, and cone-beam computed tomography (CBCT).
17 Most techniques have limitations such as accuracy, cost, radiation exposure, and magnification.2
High-resolution CBCT is a promising and accurate technology for quantitatively determining the position of MF and the presence of AL. CBCT has the advantage of providing high-quality three-dimensional images without distortion and serves with a precise evaluation of the anatomical variations at much lesser radiation exposure than CT.9 For evaluation of the MF's location, size, and shape, a CBCT gives accurate estimates compared to an Orthopantogram.
In the present study, mental foramen has been studied in terms of its size, shape, position, distance from adjacent teeth and mandibular borders, and pattern of the inferior alveolar canal using CBCT. A lot of research is focussed on reading the MF and its relation to its size, anatomical position and IAN exit.2,3,4,6,7,9
However, this study is the first one to study the MF on CBCT and read the exit pattern; in the Indian Subpopulation (South Indian).
Horizontal diameter and vertical diameter values on the right side were higher in males as compared to the values observed in females. There was a marginal difference difference in the size of the MF with age and sex on both the left and right sides. These results are consistent with those found by Ewa Zmyslowska-Polakowska et al.,2
The value obtained by evaluating the ratio of the two diameters, i.e., horizontal diameter and vertical diameter, was helpful in the assessment of the shape of MF. The most frequent shape was a round shape (Type III), and the least was an oval horizontal (Type I). This was in contrast to the study by Ewa Zmyslowska-Polakowska et al., in the Polish population, where oval horizontal (Type I) was most frequent,2 and the study by Gershenson on dry mandibles, where the elliptical shape was more frequent.5
The results were similar to the CBCT studies reported by Shankar et al., Sekerci et al., and Alam et al., in the Indian, Turkish, and Arabic populations, respectively.18-20
Hence, the size and shape of the mental foramen vary among different populations.
The MF was located below the apex of the second premolar, followed by between the first and second premolar. These results were similar to the studies carried out by Ewa Zmyslowska-Polakowska et al., H. Mahlawy et al., Von Arx et al.,2,6,21
No significant difference was found between the distance between the MF and the apex of the nearest adjacent tooth with age and sex; however, the distance was slightly more on the left side in both males and females.
Distance from the mandibular lower border on the right side is maximum for age group>60 years, followed by 46-60 years, and the least for 20-45 years age group; the difference among these three groups was significant (p-value 0.018). This could be because there is resorption of alveolar bone with age, which places the MF near the superior border of the mandible.5
In severe cases of resorption, the MF, and the adjacent part of the mandibular canal are open at the superior margin of the body of the mandible.22
Distance from the mandibular lower border on the right side was significantly more in males than females (p-value 0.032). This difference in sex can be due to the lower development rate and bone growth of the craniofacial skeleton in females compared to males, which is governed by sexual hormones and local factors like masticatory forces and muscles, resulting in lesser bone deposition along the basal bone of the mandible. The result was similar to a study conducted by Rani et al.,23 There is no explanation for this observation, however, we did not read the presence or absence of teeth. A study by Pramstraller M Et.al has suggested that mandibular asymmetry as partially edentulous cases could result in resorption of alveolar bone more on one side and display a difference in the distance from the lower border. 24
The IAC pattern is categorized into linear, perpendicular, and anterior loop patterns. Identifying the anterior loop is essential for preventing neurosensory alterations during various surgical procedures in the MF region.
The most common pattern detected in the present study was the perpendicular pattern, followed by a linear pattern irrespective of sex, and the least common was the anterior loop. The incidence of anterior loop pattern was similar to a study conducted by H. Al-Mahalawy et al., in the Saudi population, in contrast with studies by Hu et al., and Apostolakis and Brown. 8,25 Whereas the difference among the three age groups was significant, the visibility of the anterior loop decreases with an increase in age, which may be due to reduced calcification of the cortex, which makes the bone remodeling slower. The increased cortical porosity and Haversian canals show resorption of bone, resulting in the bone marrow space enlargement and arrangement of the trabecular pattern in a disoriented manner, affecting the anterior loop of mental foramen visibility.26
Clinical significance of the present study-
1) Taking relevant radiographs for diagnostic and therapeutic procedures is essential.
2) Knowledge of the operator about the size, location, and position of the MF is of great clinical relevance for more accurate prediction of the success or failure of the dental procedures like successful anesthesia during nerve blocks, curettage, and root canal treatment. Misjudgments of the position may lead to paresthesia, bleeding, and inadvertent nerve damage.
3) I n the present study, the distance from the superior margin of MF to CEJ provides a stable and reliable reference point in patients with periodontal diseases that may cause resorption at the alveolar crest. This is clinically significant as it aids in avoiding iatrogenic errors while judging the precise position of the MF, which is important in preventing the damage to the neurovascular bundles exiting the MF during periapical surgeries.
4) Regarding the IAC pattern, in the present study, the perpendicular pattern was more common. However, AL has clinical relevance as identifying the anterior loop is important during various surgical procedures in the MF region like periapical surgery, orthognathic surgery, and hemorrhagic complications during the transoperative period of implant placement because individuals with an AL are more likely to suffer from neurosensory alterations. It is recommended to leave a '2mm Safety zone' between the coronal aspect of the nerve and the intended implant.27
The limitation of the study was that only one observer evaluated all the CBCT, thus, there could be some bias in the interpretation. However, the observer had a strict fixed parameter for reading and recording.
CONCLUSION
CBCT precisely determined the shape and location of mental foramen with the neighboring anatomical structures in the present study, and it was found that the size of MF varies with age and sex. The most frequent shape of MF was Type III (round), the location was below the apex of the second premolar, and the most common IAC pattern observed was the perpendicular pattern. Hence, knowledge of the anatomic proximity of the MF to adjacent root apices is essential during endodontic treatment and while performing various surgical procedures in the premolar area to avoid any injury or iatrogenic complications and achieve successful dental procedures.
REFERENCES
1. Singh B, Sharma K. Trigeminal Nerve-Anatomy, Testing & Diseases: A Review. Arch Neurol Neurol Disord. 2019; 2:112- 17. doi.org/10.1177%2F1744806920901890 [ Links ]
2. Zmyslowska-Polakowska E, Radwanski M, Ledzion S, Leski M, Zmyslowska A, Lukomska-Szymanska M. Evaluation of size and location of a mental foramen in the polish population using cone-beam computed tomography. BioMed Res Int.2019; 2019:1-8. doi: 10.1155/2019/1659476. PMID: 30719439 [ Links ]
3. Rezaei F, Bahrampour E, Alizadeh S, Imani MM. Assessment of Vertical and Horizontal Position of Mental Foramen in a Subpopulation of Kermanshah City by Panoramic Radiographs. J Medi Dent Sci. 2018; 6:459-65. doi.org/10.2174%2F1874210601509010297 [ Links ]
4. Mohammad ZK, Shadid R, Kaadna M, Qabaha A, Muhamad AH. Position of the Mental Foramen in a Northern Regional Palestinian Population. Int J Oral Craniofac Sci.2016; 2:057-064. doi.org/10.17352/2455-4634.000020 [ Links ]
5. Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: changes with age. Cells Tissues Organs.Acta Anat (Basel) 1986; 126:21-8. doi.org/10.1159/000146181 [ Links ]
6. Al-Mahalawy H, Al-Aithan H, Al-Kari B, Al-Jandan B, Shujaat S. Determination of the position of mental foramen and frequency of anterior loop in Saudi population. A retrospective CBCT study. Saudi Dent J. 2017; 29:29-35. doi.org/10.1016/j.sdentj.2017.01.001 [ Links ]
7. Iyengar AR, Patil S, Nagesh KS, Mehkri S, Manchanda A. Detection of anterior loop and other patterns of entry of mental nerve into the mental foramen: A radiographic study in panoramic images. J Dent Impl. 2013; 3:21. doi.org/10.1016%2Fj.sdentj.2017.01.001 [ Links ]
8. Hu KS, Yun HS, Hur MS, et a!,, Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg. 2007; 65:2288-94. doi: 10.1016/j.joms.2007.06.658. [ Links ]
9. Nair UP, Yazdi MH, Nayar GM, Parry H, Katkar RA, Nair MK. Configuration of the inferior alveolar canal as detected by cone beam computed tomography. J Conserv Dent. 2013; 16:518-21. doi.org/10.4103%2F0972-0707.120964 [ Links ]
10. Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodont. 2006; 77:1933-43. doi.org/10.1902/jop.2006.060197 [ Links ]
11. Vujanovic-Eskenazi A, Valero-James JM, Sánchez-Garcés MA, Gay-Escoda C. A retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and cone beam computerized tomography. Med Oral Pataol Oral Cir Bucal. 2015; 20:e239-245. doi: 10.4317/medoral.20026 [ Links ]
12. E. M. O. Junior, A. L. Araújo, C. M. Da Silva, C. F. Sousa-Rodrigues, and F. J. Lima, "Morphological and Morphometric Study of the Mental Foramen on the M-CP-18 JiachenjiangnPoint. Int J Morphol. Int. J. Morphol. , 2009; 27:231-238. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.880.2795&rep=rep1&type=pdf [ Links ]
13. L. Zhang and Q. Zheng, "Anatomic Relationship between Mental Foramen and Peripheral Structures Observed By Cone- Beam Computed Tomography. Anat Physiol. 2015; 5: 182. https://www.longdom.org/open-access/anatomic-relationship-betweenmental-foramen-and-peripheral-structures-observed-by-conebeam-computed-tomography-22501.html [ Links ]
14. Ahlgren FK, JohaaneFson AC, Hellem S. Displaced calcium hydroxide paste causing inferior alveolar nerve paraesthesia: report of a case. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2003; 96:734-7. doi.org/10.1016/j.tripleo.2003.08.018 [ Links ]
15. Ahonen M, Tjáderhane L. Endodontic-related paresthesia: a case report and literature review. J Endod. 2011; 37:1460-4. doi.org/10.1016/j.joen.2011.06.016 [ Links ]
16. Resnik RR. Neurosensory Deficit Complications in Implant Dentistry. Misch's Avoiding Complications in Oral Implantology. Elsevier.2018;3S9-63. [ Links ]
17. Aminoshariae, A., Su, A., Kulild, J.C. Determination of the location of the mental foramen: a critical review. J Endod.2014; 40; 471-75. doi.org/10.1016/j.joen.2013.12.009 [ Links ]
18. Sankar DK, Bhanu SP, Susan PJ. Morphometrical and morphological study of mental foramen in dry dentulous mandibles of South Andhra population of India Indian J Dent Res.2011. 22:542 https://www.ijdr.in/artide.asp?issn=09709290;year=2011;volume=22;issue=4;spage=542;epage=542;aulast=Sankar [ Links ]
19. A. Sekerci, H. Sahman, Y. Sisman, and Y. Aksu, "Morphometric analysis of the mental foramen in a Turkish population based on multi-slice computed tomography," J Oral Maxillofac Radiol.2013; 1: 2-7 doi.org/10.4103/2321-3841.111341 [ Links ]
20. M.K. Alam, S. Alhabib, B. K. Alzarea et al., "3D CBCT morphometric assessment of mental foramen in Arabic population andglobal comparison: imperative for invasive and non-invasive procedures in mandible," Acta Odontologica.2018; 76:98-104. doi.org/10.1080/00016357.2017.1387813 [ Links ]
21. Vop Arx T, Friedli M, Sendi P Lozanoff S, Bornstein MM. Location and dimensions of the mental foramen: a radiographic analysis by using cone-beam computed tomography. J Endod. 2013; 39:1522-28. doi.org/10.1016/j.joen.2013.07.033 [ Links ]
22. Suragimath A, Suragimath G, Murlasiddiah SK. Radiographic location of mental foramen in a randomly selected population of Maharashtra. J Indian Acad Oral Med Radiei 2016; 28:11-16. https://www.jiaomr.in/article.asp?issn=09721363;year=2016;volume=28;issue=1;spage=11;epage=16;aulast=Suragimath [ Links ]
23. Rani A, Kanjani V Kanjani D, Annigeri RG. Morphometric assessment of mental foramen for gender prediction using panoramic radiographs in the West Bengal population-A retrospective digital study. J. Adv. Clin. Res. Insights. 2019; 6:63-6. doi.org/10.15713/ins.jcri.262 [ Links ]
24. Pramstraller M, Schincaglia GP, Vecchiatini R, Farina R, Trombelli L. Alveolar ridge dimensions in mandibular posterior regions: a retrospective comparative study of dentate and edentulous sites using computerized tomography data. Surgical and Radiologic Anatomy. 2018 Dec;40(12):1419-28 [ Links ]
25. Apostolakis, D., Brown, J.E. The anterior loop of the inferior alveolar nerve: prsvolence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implan Res.2012; 23:1022-30. doi.org/10.1111/j.1600-0501.2011.02261.x [ Links ]
26. Sridhar M, Dhanraj M, Thiyaneswaran N, Jain AR. A retrospective radiographic evaluation of incisive canal and anterior loop of mental nerve using cone beam computed tomography. Drug Invention Today. 2018; 10:1656-60. https://healthdocbox.com/Dental_Care/112957124-A-retrospective-radiographic-evaluation-of-incisive-canal-and-anterior-loop-of-mental-nerve-using-cone-beam-computed-tomography.html [ Links ]
27. Hasan T. Mental foramen morphology: A must know in clinical dentistry. J Pak Dent Assoc. 2012; 21:00-00. https://www.researchgate.net/publication/233790049_Morphology_of_the_mental_foramena_must_know_in_clinical_dentistry [ Links ]
 Correspondence:
Correspondence:
Neha Verma
Army College of Dental Sciences, Jai Jawahar Nagar, Chennapur, CRPF Road Secunderabad, 500087
Phone numbers: 6304215714; E-mail address: nv89168@gmail.com
Author contribution
Dr N Verma 50%
Dr M Kaushik 30%
Dr E Soujanya 10%
Dr N Mehra 05%
Dr A George 05%














