Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.77 n.10 Johannesburg Nov. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no10a6
CASE REPORT
Actinomycosis osteomyelitis of the mandible in a 71-year-old patient: A Case Report
N KhanI; G MhlangaII
IDepartment of Maxillo-Facial and Oral Surgery, Unversity of Pretoria. ORCID: 0000-0002-4110-6595
IIDepartment of Maxillo-Facial and Oral Surgery, Unversity of Pretoria. ORCID: 0000-0002-0663-7235
ABSTRACT
We herein present the treatment of an actinomycosis osteomyelitis case. A 71-year-old female with a dental history of multiple tooth extractions two years prior who subsequently developed chronic osteomyelitis. Previous treatment included 10 sessions of hyperbaric oxygen and pentoxifylline tocopherol protocol as well as debridement of the lesion that had resulted in a subsequent midline pathological fracture of the mandible. The fracture was treated by intra-bony wiring. The clinical extra-oral presentation was that of severe pain, recurrent swelling of the submandibular areas bilaterally and draining fistulae. Our treatment included antibiotic therapy: guided by Microscopy Culture and Sensitivity and a segmental mandibulectomy with the placement of a reconstruction plate. The outcome of the therapeutic management was successful. Histopathology results confirmed chronic osteomyelitis with bacterial colonies in keeping with actinomycosis. At the six-week post-operative appointment, the patient was healing well.
Keywords: Osteomyelitis, Actinomycosis, Segmental mandibulectomy
BACKGROUND
Osteomyelitis is inflammation of bone and marrow.1 It frequently occurs as a primary isolated focus of disease or can be secondary to systemic infection.1 Although any microorganism may cause osteomyelitis, bacteria is the most common etiologic agent.2 The infection caused by the microorganism compromises the blood supply to the bone.3 By compromising the blood supply to the bone, it also hinders the inflammatory response needed to clear the disease, promoting disease progression.3 In the head and neck region, infections of the mandible can be introduced through an extraction socket or direct trauma to the mandible resulting in an open fracture.4 Actinomycosis is a normal commensal microorganism of the oral cavity, thus when the mandible is exposed, either from the extraction socket or trauma, it can enter and cause osteomyelitis.4 Mandibular actinomycosis infections commonly present with Arm soft tissue swellings and multiple abscesses, making it difficult to distinguish from inflammatory conditions, neoplastic processes or trauma.4
Three main types of osteomyelitis are acute, primary chronic, and chronic osteomyelitis. Acute and chronic osteomyelitis are similar in presentation, however, separated by the duration of time since the onset of the disease. The former has a duration of fewer than 4 weeks and latter lasts for more than 4 weeks.5 Chronic osteomyelitis is common in communities with poor socio-economic conditions presenting with poor oral hygiene.6 Chronic osteomyelitis is a debilitating condition, requiring adequate antimicrobial treatment, and or surgical management.7 Due to bacteria being the most common cause of osteomyelitis, empiric antibiotic therapy is often selected.8 However, definitive antimicrobial therapy should be based on final microscopy culture and sensitivity (MC&S) results.9 MC&S results also help in avoiding multidrug resistance and lead to a favourable treatment outcome.8
CASE PRESENTATION
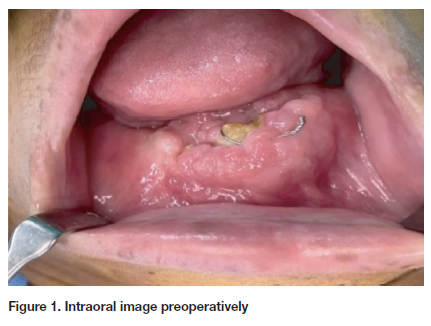
A 71-year-old female with hypertension and osteoarthritis was referred to the Maxillo-Facial and Oral Surgery Department at the Oral and Dental Hospital. She presented with multiple sinus tracts of the anterior mandible. Her dental history revealed multiple tooth extractions two years prior with subsequent development of chronic osteomyelitis. Before the presentation, she received sessions of hyperbaric oxygen complimented by a pentoxifylline tocopherol protocol. Subsequently, she developed a pathologic fracture which was treated and reduced with an internal fixation wire. On examination, there was bilateral submandibular soft tissue swellings and draining fistulae. Intraorally, necrotic exposed bone was noted in the anterior mandible with exposed wire. Upon palpation, the surrounding tissues were friable and tender (Figure 1).
Investigations
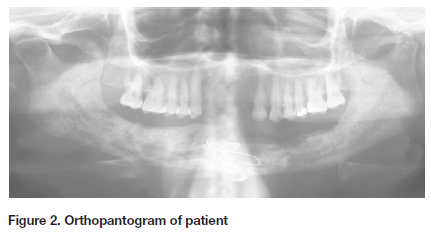
Special investigations included an Orthopantomogram (OPG) radiograph which showed multiple areas of ill-defined, moth-eaten mixed radiolucent/radiopaque lesions extending from the left parasymphaseal area of the mandible to the symphysis (Figure 2). A pathological fracture was noted in the midline of the mandible that had been reduced and fixed with wire. Microscopy, culture, and sensitivity (MC&S) results that accompanied the patient from a private laboratory, showed multiple drug resistance. The list included resistance to penicillin and beta-lactamase.
Treatment
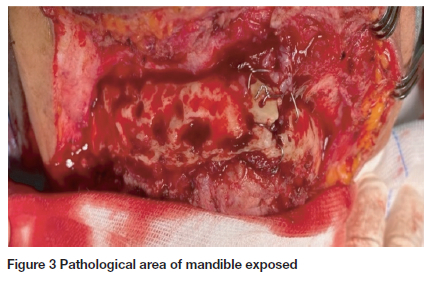
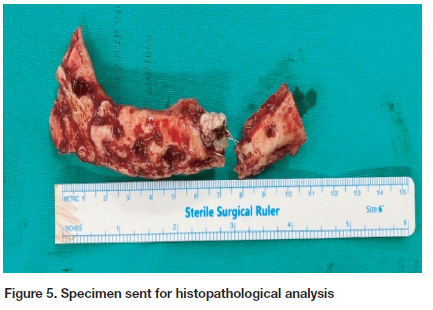
A segmental mandibulectomy of the necrotic bone (Figure 3) with the placement of a construction plate was the treatment of choice (Figure 4). The specimen was sent for histopathological analysis and tissue was also submitted for MC&S (Figure 5).
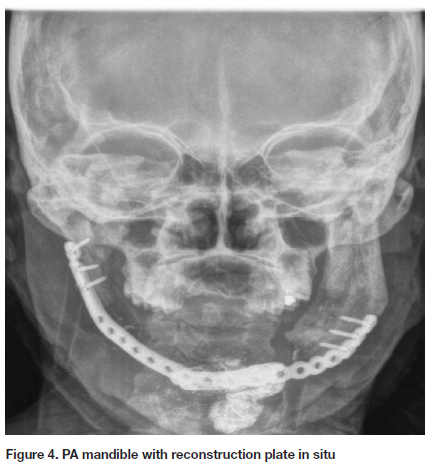
Histopathological examination confirmed chronic osteomyelitis with Actinomycosis bacterial colonies. MC&S confirmed bacterial organisms sensitive to Vancomycin. Vancomycin 1g IV was given as a daily dose in the hospital for 2 weeks. Trough levels were measured to ensure antibiotic levels were in the therapeutic range.
DISCUSSION
Actinomycosis is a commensal of the oral cavity however, a history of trauma from either dental extractions or facial fractures, especially of the mandible, can result in disease as seen in this case. If a patient presents with radiopaque lesions of the mandible with multiple fistulas and a pathological fracture, mandibular osteomyelitis should be considered. The management should include a biopsy and MC&S to confirm the possible diagnosis. Bacterial colonies form distinct actinomycotic granules, referred to as sulphur granules. These granules are composed of dense aggregates of filamentous bacteria.10
Treatment of cervicofacial actinomycosis includes a surgical approach in combination with IV antibiotics.11 First-line antibiotics include parenteral administration of penicillin G (50-75mg/kg/day IV in four daily divided doses) for 4 to 6 weeks. This may be followed by peroral penicillin V (30-60mg/kg/day administered in four divided doses) until complete resolution of the disease is noted.12 Older literature advocated long-term antibiotic usage of 6 to 12 months duration.12 In this case, the patient had multiple mandibular debridements along with various antibiotics, hyperbaric oxygen therapy, and tocopherol therapy, all with no resolution of the disease. She then had multidrug resistance and was hospitalised for surgical treatment as well as with Vancomycin 1g IV daily for 2-weeks in the hospital. At the six-week follow-up appointment, the bone had healed well with no evidence of sepsis on examination and her function was restored.
Learning objective
Due to impoverished, poor socio-economic conditions, one must consider the possibility of actinomycosis osteomyelitis after a non-healing extraction socket or other Maxillo-Facial trauma. Mandibular actinomycosis may have a similar presentation to neoplastic processes, as noted by the presence of multiple fistulas, thus should be included in the list of differential diagnoses. Of critical importance, treatment must include microbial culture and sensitivity to optimize antimicrobial usage. Thus, avoiding multidrug resistance and leading to a favourable treatment outcome.
Patient consent
Patient consent was obtained verbally and in writing and submitted and approved by RESCOM and ethics prior to publication.
Disclosure of interest-The authors declare that they have no competing interests.
REFERENCES
1. Kumar V, Abbas AK, Aster JC. Robbins basic pathology e-book. Elsevier Health Sciences; 2017 Mar 8. p 773 [ Links ]
2. Urs AB, Singh H, Mohanty S, Sharma P. Fungal osteomyelitis of maxillofacial bones: rare presentation. Journal of oral and maxillofacial pathology. 2016 Sep;20(3):546. [ Links ]
3. Mercuri LG. Acute osteomyelitis of the jaws. Oral and maxillofacial surgery clinics of North America. 1991 May 1;3(2):355-65. [ Links ]
4. Sasaki Y, Kaneda T, Uyeda JW, Okada H, Sekiya K, Suemitsu M, Sakai O. Actinomycosis in the mandible: CT and MR findings. American Journal of Neuroradiology. 2014 Feb 1;35(2):390-4. [ Links ]
5. Agarwal A, Kumar N, Tyagi A, De N. Primary chronic osteomyelitis in the mandible: a conservative approach. Case Reports. 2014 Apr 3;2014: bcr2013202448. [ Links ]
6. Gaetti-Jardim E, Landucci LF, de Oliveira KL, Costa I, Ranieri RV, Okamoto AC, Schweitzer CM. Microbiota associated with infections of the jaws. International journal of dentistry. 2012 Jul 8;2012. [ Links ]
7. Pincus DJ, Armstrong MB, Thaller SR. Osteomyelitis of the craniofacial skeleton. Seminars in plastic surgery 2009 May (Vol. 23, No. 02, pp. 073-079). [ Links ]
8. Dym H, Zeidan J. Microbiology of acute and chronic osteomyelitis and antibiotic treatment. Dental Clinics. 2017 Apr 1;61(2):271-82. [ Links ]
9. Miloro M. Peterson's principles of oral maxillofacial surgery. 3rd ed. New York: McGraw-Hill Medical; 2011. [ Links ]
10. Lerner PI. The lumpy jaw: Cervicofacial actinomycosis. Infectious disease clinics of North America. 1988 Mar 1;2(1):203-20. [ Links ]
11. Moghimi M, Salentijn E, Debets-Ossenkop Y, Karagozoglu KH, Forouzanfar T. Treatment of cervicofacial actinomycosis: a report of 19 cases and review of literature. Medicina oral, patologia oral y cirugia bucal. 2013 Jul;18(4): e627. [ Links ]
12. Oostman O, Smego RA. Cervicofacial actinomycosis: diagnosis and management. Current infectious disease reports. 2005 Jun;7(3):170-4. [ Links ]
 Correspondence:
Correspondence:
Dr. Nazia Khan
Department of Maxillofacial and Oral Surgery
University of Pretoria
South Africa
E-mail: Nazia.khan@up.ac.za
Te: +27798784996
Author contributions:
1 . Dr Nazia Khan: 50%
2 . Dr Gugulethu Mhlanga: 50%














