Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.77 n.10 Johannesburg Nov. 2022
http://dx.doi.org/10.17159/2519-0105/2022/v77no10a3
RESEARCH
Self-reported oral health status: Perspectives of patients undergoing therapy for cancer of the head and neck region, in the eThekwini District, KZN
BS Bauluck-NujooI; S SinghII
IBDS (SSR Medical College-University of Mauritius), M.MEDSc (UKZN), School of Health Sciences, University of KwaZulu-Natal, South Africa. ORCID Number: 0000-0002-71575122
IIB.OH, M.Sc (Dent), PhD (UWC), PG Dip Heal Res Ethics (Stell), PhD (Clin and Res Ethics (Stell) Professor: Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal, South Africa. ORCID Number: 0000-0003-4842-602
ABSTRACT
BACKGROUND: There is a dearth of published evidence related to understanding oral health needs for patients undergoing therapy for cancer of the head and neck region in South Africa
Aim and objectives: This study aimed to assess perceived oral health status of patients undergoing therapy for cancer of the head and neck region, in eTthekwini district, KwaZulu-Natal.
METHODS: This was a cross-sectional case study using quantitative data to determine patients' perspectives of oral health status and need. The study population comprised 235 voluntary patients (aged between 20-70 years old), undergoing treatment or follow up for cancer therapy of the head and neck region, in a public tertiary referral hospital in the eThekwini district, KwaZulu-Natal. Purposive sampling technique was used for participant selection. The research instrument comprised a combination of two previously validated questionnaires: a core questionnaire (EORTC QLQ-C30, Version 3.0) and the head and neck cancer specific module (EORTC H&N-35). Data was analysed using the statistical package for software sciences (SPSS), version 24
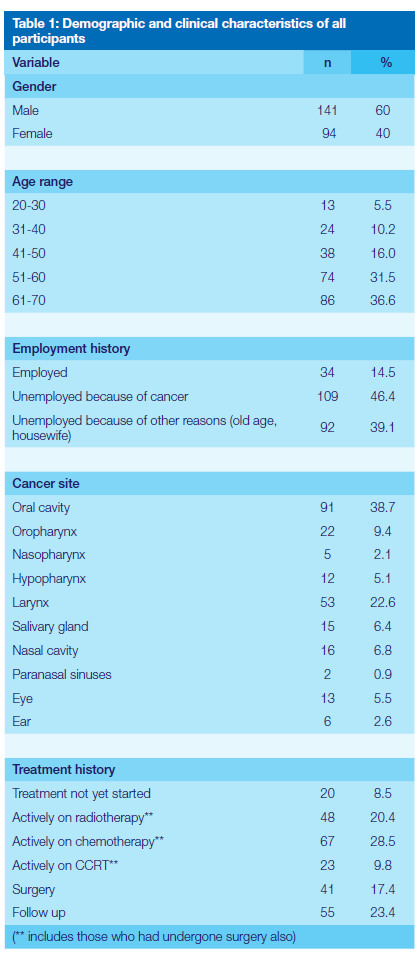
RESULTS: More than half of the study population were male (60%; n= 141). The mean age was 54.38 (SD= 12.30). The results indicate that 14.5% (n=34) were employed, 46.4% (n=109) were unemployed because of cancer and 39.1% (n=92) were unemployed due to other reasons (old age, housewife). Oral cavity cancer was the most common (n=91; 38.7%), followed by laryngeal cancer (n= 53; 22.6%) among all the other head and neck cancers. Males (n=50; 21.3%) were more affected by oral cavity cancer as compared to females (n=41; 17.4%). With reference to treatment, 20.4% (n=48) were on radiotherapy, 28.5% (n=67) were on chemotherapy and 9.8% (n=23) were on CCRT, 17.4% (n=41) had surgery, 8.5% (n=20) were recently diagnosed with cancer of the head and neck and 23.4% (n=55) were on follow up. Oral health-related symptoms were experienced to varying degree by the participants
The majority of participants (n=125; 53.2%) did not report any pain and discomfort. More female participants (n=7; 7.4%) in the age group of 41-60 reported of severe difficulty in swallowing liquids than males of the same age group. Most participants (n=148; 63.0%) had difficulty in swallowing solid foods. Similarly, the majority of participants experienced problems with their teeth (n=162; 69.0%), reported xerostomia (n=159; 67.7%). With reference to trismus, a higher proportion of females (n=27; 28.7%) reported severe trismus compared to male participants (n=33; 23.4%). With reference to increased viscosity of saliva, 34.0% (n=32) of females reported extremely sticky saliva as compared to 29.8% males (n=42).
CONCLUSION: It is apparent from the findings that oral health-related complications are present in varying degrees in the study participants with head and neck cancer. It is important to educate patients to seek treatment for these complications. It is equally important that dentists and dental health care providers with specific skills-mix, assess and manage such complications efficiently and timely so as to improve the quality of life of patients with head and neck cancer.
INTRODUCTION
The head and neck region is a complex anatomical structure1. This region and its physiological functions are both affected by cancer or its multimodality treatment1. Head and neck cancer (HNC) is a complex disease extending from the skull base to the clavicles, comprising different subsites namely, pharynx (including hypopharynx, nasopharynx and oropharynx), larynx, paranasal sinuses and nasal cavity, minor and major salivary glands, oral cavity (including lip, alveolar ridge, buccal mucosa, gingiva, oral tongue, retromolar trigone and floor of mouth), ear, skin and neck2, 3. Cancer of the eye was also included besides that of oral cavity, pharynx, larynx, nasal cavity, paranasal sinuses and salivary glands since it is also found in the head and neck region4.
Radiotherapy (RT), chemotherapy (CT), concurrent chemoradiotherapy (CCRT), and surgery are the different treatment modalities employed in the management of head and neck cancer 5. The oral cavity, its subsites and dental hard tissues are some of the vital structureswhich get affected either directly or indirectly by effects of radiotherapy, chemotherapy, concurrent chemoradiotherapy and surgery of any head and neck cancer 6. Thus, oral health support and maintenance is of dynamic importance before, during and even after therapy since multimodal treatment-related oral complications like radiation caries, oral mucositis, xerostomia, osteoradionecrosis, periodontal disease, trismus, hypersensitivity and infections, pose a challenge for optimum oral health care 7. The motor functions including mastication, deglutition, speech and sensory functions of the gustatory, olfactory and auditory systems are disturbed 8. Disfigurement of the facial appearance is also a challenging complication because of the highly conspicuous nature of this region 9.
Poor oral health is linked to poorer quality of life and increased mortality 10. Therefore, assessment of the oral health of patients with cancer of the head and neck is an important form of support in oral health care since the head and neck region comprise of vital organs which, when affected, unfavourably impact on the overall well-being.
Oral health services are delivered via the public and private sector in South Africa 11. The public sector caters for 80% of the population of South Africa by providing primary preventive and restorative care 11. The rural areas of KwaZulu-Natal comprise of almost 62% of the total population. However, an unequal distribution of services is present since the urban areas are more privileged in terms of oral health care access12. Inadequate and unequal distribution of dental health care providers and dental professionals is one of the reason contributing to this unequal trend in service delivery11,12. Delivering oral health care through an integrated approach is incessantly and persuasively mentioned in policy planning documents but research demonstrated that this approach is not fully translated into actions and hence a lack in meaningful content is observed13. A qualitative component of this present study also showed that there is a significant gap in service delivery for patients undergoing treatment for head and neck cancer since there is no specific oral health policy for this population group.
This study arose as a need to assess the perceived overall well-being and oral health status of patients undergoing therapy for cancer of the head and neck so as to empower patients to identify their own needs which will subsequently provide a contribution to provincial oral health planning.
For ease of analysis, cancer of the lip, buccal mucosa, anterior two thirds of tongue, floor of mouth, maxilla, mandible, hard palate, gingiva and retromolar trigone were grouped under oral cavity cancer 4, 14. Similarly, cancer of the base of the tongue, soft palate and tonsils were categorised under oropharyngeal cancer 14. Salivary gland cancer consisted of only parotid and submandibular gland cancer. There were no other cancers of the salivary gland like sublingual gland and minor salivary gland cancer.
METHODS
This was a descriptive cross-sectional case study conducted between April to August 2017 to determine the perceptions of overall well-being and oral health status in patients undergoing treatment for head and neck cancer using quantitative methods. The study site was a public tertiary central referral hospital for the management of cancer, located in the Ethekwini Metropolitan Municipality within the province of KwaZulu-Natal. The sample population consisted of 235 voluntary adult patients of both sexes who were undergoing therapy exclusively for cancer of the head and neck region (active treatment, prior to treatment, or follow up). Purposive sampling technique was used for participant selection.
The sample size was calculated by taking into consideration the proportion of population in KZN, using a uniform distribution to have an estimate of the head and neck cancer cases in KZN and assuming that 65% of head and neck cancer patients attend public hospitals. The required sample size according to the calculation was 147. However, it was agreed that 250 participants would be included in the study instead of 147 so as to have more conclusive and accurate results and increase the statistical power. However, the final sample size was 235, given that fifteen patients did not consent. A total of 250 patients were approached either from the waiting room or radiotherapy or chemotherapy departments of the Oncology Unit of the hospital and explicit information about the study and time commitments were given verbally. All interested persons were given a participant information sheet to allow voluntary informed decisions to be made before consenting. The information sheets contained full details about the nature, purpose and any potential benefits and risks of the study in a simple, concise and easily understandable language. Participants were also informed of their right to withdraw from the study at any time they wish so without incurring any penalty or loss of treatment benefits to which they are entitled to receive. The inclusion criteria were histologically diagnosed head and neck cancer participants undergoing therapy, aged between 20-70 years old.
The research instrument comprised of a combination of two different validated questionnaires: A core questionnaire (EORTC QLQ-C30, Version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35). A total of 30 and 35 questions respectively were answered in a four-point likert type scale format with responses such as 1(Not at all), 2 (A little), 3 (Quite a bit) and 4 (Very much) for all questions but 2 items related to global health and quality of life in EORTC QLQ-C30 where there is a scale of 1-7 and 5 items of EORTC QLQ-H&N35 where there is a choice between yes or no.
The EORTC QLQ-C30 is known as the core questionnaire and was chosen because its reliability and validity have been researched and implemented using a modular and integrated approach for over a decade and is used in numerous international clinical trials and is reported to be accurate, valid and reliable 15. The newer version, that is version 3.0, was used in this research as it was shown to be more reliable than previous versions based on the physical functioning scale 16. This questionnaire consists of 30 questions with both single item and multi item scales, out of which 5 cover the functional scales (physical, role, cognitive, emotional and social),9 cover the symptom scales (pain, fatigue, nausea, vomiting, diarrhoea, constipation, loss of appetite, financial difficulties and insomnia) and one scale being related to global health status and quality of life 15.
EORTC QLQ- H&N35 is a specific module for head and neck cancer and has been field tested in more than ten countries and was found to possess robust psychometric validity, although some minor modifications were intended to be made 15 17. It has to be used together with the core questionnaire. It is composed of 35 questions containing both single and multiple item scales to assess treatment side effects and symptoms 15. There are 11 single item questions (like mouth opening, dry mouth, sticky saliva, teeth problems, feeling ill, cough, pain killers, nutritional supplements, use of feeding tube, weight loss/gain) and 7 multiple item questions on pain, swallowing, sexuality, social contact, social eating, speech and senses 15.
The English and IsiZulu versions of the questionnaires are both available. Permission from the EORTC Data Centre was obtained prior to using both questionnaires in both languages in this research project. The questionnaires were administered by the researcher (for English-speaking participants) and a research assistant (for IsiZulu-speaking participants).
Approval from the KwaZulu-Natal Department of Health and ethical clearance from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal were given prior to the commencement of the study (BREC Ref: BE041/17). Ethical principles were strictly adhered to.
Demographic details including gender, race, age, municipality, employment history, cancer site and treatment history were recorded. The cancer site was confirmed with the oncologist or oncology nurse from the participants' medical files. The other details were obtained verbally from the participants prior to administering the questionnaires. The data set was captured on Microsoft excel spreadsheet on a password-protected computer and imported onto IBM Statistical Package for Social Sciences (SPSS) Version 24. Demographic details of the participants were calculated using descriptive statistics (mean, frequency, percentages, standard deviation). Pearson Chi-Square test was used to assess possible relationship between the independent and dependent variables. The p-value was set to less than 5% (< 0.05) to be significant.
Both questionnaires have been validated in previous studies 16. The questionnaires (EORTC QLQ-C30 and EORTC QLQ-H&N35) used were aligned to the aims and objectives of this study and this added to the internal validity. The generalisability of this study is limited to the study site which is a tertiary hospital. Reliability was maintained by double checking the data during data entry and eliminating all outliers.
RESULTS
The study population consisted of 235 patients undergoing treatment for cancer of the head and neck. The sample population comprised of 60% (n= 141) male and 40% (n=94) female. The mean age was 54.38 (SD= 12.30). The majority of participants was from Ethekwini municipality (n=175; 74.5%). Amajuba district recorded the least number of participants (n=1; 0.4%). Concerning employment history, 14.5% (n=34) were employed, 46.4% (n=109) were unemployed because of cancer and 39.1% (n=92) were unemployed due to other reasons (old age, housewife). As for treatment history, currently (at the time of data collection) 20.4% (n=48) were on radiotherapy, 28.5 % (n=67) were on chemotherapy and 9.8% (n=23) were on CCRT. Participants who were recently diagnosed with cancer of the head and neck (treatment not yet started) accounted for 8.5% (n=20), while 23.4% (n=55) were on follow up.
The oral cavity cancer was found to be the most common (n=91; 38.7%), followed by laryngeal cancer (n= 53; 22.6%) among all the other head and neck cancer. Males (n=50; 21.3%) were mostly affected by oral cavity cancer as compared to females (n=41; 17.4%). Our study also showed that laryngeal cancer was three times more common in males (n=40; 17%) than in females (n=13; 5.5%). A significant relationship was found between laryngeal cancer and Coloured male and female, Indian male and female and White male. A significant statistical difference for Indian with cancer site variable was found (p < 0.05).
The findings (Table 2) indicate that the majority of participants (n=125; 53.2%) did not experience any pain in the jaw (maxillary and/or mandibular) while the rest of the participants (n=110; 46.8%) had varied responses to perceived pain. Among those who had pain in the jaw, a greater number of males (n=26; 18.4%) than females (n=10; 10.6%) reported minimal/ negligible ("a little") pain in the jaw, while more females (n=24; 25.5%) reported severe ("very much") pain in the jaw than males (n=22; 15.6%). The results also demonstrated that perceived intra-oral discomfort ("soreness in the mouth") was statistically significant (p=0.010). The majority of participants (n=135; 57.4%) did not experience any intra-oral related pain and discomfort (soreness of the mouth). The results indicate that only 13.8% females (n=13) and 7.8% males (n=11) experienced severe intra-oral related pain and discomfort. With reference to swallowing liquids, 10.6% females (n=10) and 5.7% males (n=8) indicated severe difficulty in swallowing. The findings further demonstrate that more female participants (n=7; 7.4%) in the age group of 41-60 reported of severe difficulty in swallowing liquids than males of the same age group. Male participants who perceived severe difficulty to swallow liquids were all in the age group of 51-70. Only one female in the age group of 31-40 reported severe difficulty in swallowing liquids. The majority (=135; 57.4%) of participants did not experience any problem in swallowing pureed foods. Among those who did have difficulty (n=100; 42.6%) to swallow pureed food, equal proportion of males (n=27; 19.1%) and females (n=18; 19.1 %) experienced minimal difficulty to swallow pureed foods. However slightly more females (n=13; 13.8%) experienced severe difficulty in swallowing pureed foods than males (n=17; 12.1%). Most of the participants (n=148; 63.0%) experienced difficulty to swallow solid foods, among whom 65 participants (27.7%) comprising 26.2% (n=37) males and 30% (n=28) females reported severe difficulty in swallowing solid foods. The results indicate that the majority of participants experienced problems with their teeth (n=162; 69.0%).
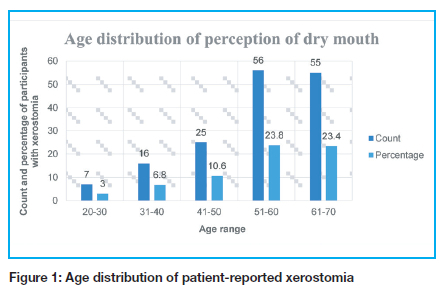
With reference to trismus (difficulty to open the mouth wide), the majority of participants (n=141; 60%) reported difficulty to open their mouth completely and there was a higher proportion of females (n=27; 28.7%) who reported severe trismus compared to male participants (n=33; 23.4%). A significant number of participants experienced xerostomia, ("dry mouth") (n=159; 67.7%). Almost 28% of participants (n=65) experienced severe xerostomia. More females (n=33; 35.1%) than males (n=32; 22.7%) experienced severe xerostomia. Increased viscosity of saliva ("sticky saliva") was also reported by the majority of participants (n=157; 66.8%).
Thirty four percent (34.0%) of females (n=32) reported extremely sticky saliva as compared to 29.8% males (n=42). Further, 44.3% (n=104) participants did not experience dysgeusia (taste alteration/taste distortion), while the majority of participants (n=131; 55.7%) had varied responses to the severity dysgeusia. Among those who perceived dysgeusia, less females (n=13; 13.8%) reported negligible dysgeusia than males (n=25; 17.7%) while 22.3% females (n=21) reported severe dysgeusia as compared to 19.1% males (n=27). The findings also indicate that 41.3% participants (n=97) did not experience any difficulty to eat while the majority of participants (n=138; 58.7%) had varied responses with respect to difficulty in eating. Among those who had difficulty to eat, 35.1% females (n=33) had severe problem in eating as compared to 23.4% males (n=33).
DISCUSSION
This study examined the reported oral-health related symptoms among patients with cancer of the head and neck.
A higher percentage of men were found to be affected by head and neck cancer than women in the ratio of 1.5:1. This is consistent with the literature which reports that head and neck cancer is 2-5 times more prevalent in males than in females globally, depending on the geographical location 18. The results indicate that head and neck cancer was most common in the 61-70 (n=86; 36.6%) age group followed by the 5160 age group (n=74; 31.4%). This finding is in contrast with previous studies which reported of the commonest head and neck cancer cases in the age group 51-60 4,19.
The reason for a higher predominance in the 61-70 age group in this study might be due to illiteracy and lack of awareness among older people about the side effects of lifestyle risk factors 20. Strong cultural beliefs that cancer is a "curse" or a "punishment" might also be another reason for preventing people from seeking treatment and thus presenting late. Further, we found that cancer of the oral cavity was more predominant among all the other head and neck cancer subsites (larynx, pharynx, nasal cavity, paranasal sinuses, salivary gland, ear, eye). This finding is consistent with the literature 19. It was also the most common cancer among both gender, a finding which is equally consistent 4 20. However, the results indicate that males were more affected by cancer of the oral cavity than females. This is in agreement with previous studies conducted among head and neck cancer patients which also found that cancer of the oral cavity was higher among males 4 9. However, the study by Shinde and Hashmi reported of a higher male to female ratio (1.9:1) of oral cavity cancers 4, while the male to female ratio was lower 1.2:1) in our study.
Laryngeal cancer (n=53; 22.6%) was the second most prevalent cancer in our study and it was three times more common in males than in females (n=40 versus n=13 respectively). The National Cancer Registry in South Africa also reported of a higher male predominance for this cancer type 21. Further, it is also reported to be more prevalent in males than in females globally but with a higher sex ratio of 7:1 22. Concerning unemployment, our study demonstrated that 46.4% of the participants were unemployed due to their present state of health as related by them. The majority of them originated from Ethekwini municipality. Added complication like unemployment is reported to be common in cancer 23. A study reported that 45,149 out of 236 993 (19.1%) of cancer participants suffered unemployment after active treatment 23. Our study however, indicated a much higher unemployment ratio.
Cancer of the head and neck or its multimodality treatment often leaves patients with several side effects and support needs. The support needs are purely subjective. The oral health of this population group is affected in a number of ways including difficulty to eat, dysphagia, odynophagia, gustatory and auditory disturbances due to a number of complications like oral mucositis, xerostomia, osteoradionecrosis, periodontal disease, trismus, hypersensitivity and infections, thus compromising the quality of life 7 8.
Soreness in the mouth, difficulty in swallowing and dry mouth are common perceived symptoms which patients often complain of. Cancer therapy can directly affect teeth, tongue and other structures of the oral cavity which very often alter the eating and swallowing patterns 14. Soreness occurs due to oral mucositis which is characterised by atrophy of the oral mucosa resulting in ulceration and accompanied by dysphagia and pain 24. It is a dose-dependent toxicity and developing in the first week after the initiation of radiotherapy and having the potential to last approximately up to 3 months 25. Oral mucositis is one of the most common disturbing patient-reported oral toxicity, accounting for an incidence of 85%-100% 26.
Dysphagia is characterised by fibrosis of the muscles of deglutition and is a major stressful and challenging treatment sequalae which patients are concerned about and like to discuss with their doctors 27. A recent update suggests that the assessment of the swallowing pattern and swallowing therapy as a prophylaxis by a swallowing therapist prior to radiation exposure is essential 27.
Trismus, as reported by the majority of participants, is evident when the interincisal distance is less than 35 mm due contraction of the masticatory muscles after radiotherapy, chemotherapy or surgery of the head and neck region 28. The presence of temporomandibular joint, masseter and pterygoid muscles within the radiation field is a cause for trismus 27 28. Surgical intervention involving the retromolar trigone, buccal mucosa and tonsillar fossa is another etiological factor for trismus 27 28. Varied responses with respect to the degree of trismus were reported among the participants. One factor which determines the varying degree of severity of trismus is the stage of the malignancy. It is further reported that the difference in severity of trismus is also associated to the dose and field of radiation 29 30.
Higher radiation doses contribute to greater reduction of the interincisal distance 29. Trismus occurs at around two months after radiation, progresses rapidly over 9 months before it starts to resolve 29. Trismus is treated by initiating exercise therapy shortly after treatment is over 30.
Sticky saliva and dry mouth (xerostomia) were perceived to different extent by the majority of the participants. Xerostomia is one of the most common reported side effect of radiotherapy. Xerostomia was perceived by more people from the older age group as compared to the younger counterpart. This observation corresponds to an earlier report which also found that the risk of xerostomia was greater as the age advances 31. Xerostomia occurs when the unstimulated and stimulated flow rate of saliva are reduced well below the normal level of 0.3-0.4 ml/min and 1.5-2.0 ml/min respectively 32. Reduction in the flow of saliva is significant in the first week of radiotherapy with 6070 Gy irradiation 33. Radiation doses above 52 Gy causes severe dysfunction of the salivary gland while permanent salivary gland damage can occur with a minimum single radiation dosage of 20 Gy 33.
Our study shows that more than half of the study population (55.7%) perceived an altered taste ranging from "a little" (16.2%), to "quite a bit" (19.1%) to "very much" (20.4%) while the rest (44.3%) did not perceive any taste impairment at all. This might be due to the fact that recent diagnosis was made and treatment had not yet started or they were on follow up and radiotherapy or chemotherapy which are both responsible for taste impairment were not being administered 34. Taste alteration is also a significant patient-reported symptom in head and neck cancer 35. It is, however, dependent on the stage of the cancer and the type of treatment that patients are undergoing 36. Taste impairment is more evident by the 3rd or 4th week of radiotherapy with a minimal dose of 30 Gy 34. Taste alteration usually resolves completely after 2-4 months of treatment but can still linger on for more than a year in those who had had high dose irradiation 34.
Limitations of the study
This was a single site hence the results can only be generalised to the site. Moreover, there was no control group of patients with other cancers, while this could have helped to ascertain whether certain oral health-related conditions are unique to head and neck cancer patients. Despite these limitations, the study makes a substantive contribution to understanding patients' self-reported oral health status. The study can make important contributions to oral health planning in the province.
CONCLUSION
It is apparent from the findings that oral health-related complications are present to varying degrees in head and neck cancer. It is important to educate patients to seek treatment for these complications. Oral health care support including patient counselling is strongly recommended as it is pivotal to psychologically prepare them to cope with any side effect.
Conflict of interest
Both authors consent to publication and declare that there are no conflicting interests.
REFERENCES
1. Sammut L, Ward M, Patel N. Physical Activity and Quality of Life in Head and Neck Cancer Survivors : A Literature Review. International Journal of Sports Medicine. 2014;35(9):794-9. [ Links ]
2. Romesser PB, Riaz N, Ho AL, Wong RJ, Lee NY. Cancer of the Head and Neck. 2012. p. 1037-70. [ Links ]
3. World Health Organization. Pathology and Genetics of Head and Neck Tumours. WHO Classification of Tumours. 2005. 1-435 p. Available from: https://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb9/BB9.pdf. [ Links ]
4. Shinde KJ, Hashmi SIH. Retrospective Study Of Malignant Lesions Of Head & Neck In Rural Area Of Ahmednagar District. IOSR Journal of Dental and Medical Sciences. 2013;4(2):12-9. [ Links ]
5. Tulunay-Ugur OE, McClinton C,Young Z, Penagaricano JA, Maddox A-M, Vural E. Functional Outcomes of Chemoradiation in Patients with Head and Neck Cancer. Otolaryngology-Head and Neck Surgery. 2013;148(1):64-8. Available from: http://journals.sagepub.com/doi/10.1177/0194599812459325. [ Links ]
6. Lieshout HFJ, Bots CP. The effect of radiotherapy on dental hard tissue-a systematic review. Clinical Oral Investigations. 2014;18(1):17-24. [ Links ]
7. Mawardi H., Al-Mohaya M., Treister N. Oral health considerations in cancer survivors. Saudi Medical Journal. 2013;34(5):461-9. Available from: https://www.scopus.com/inward/record.url?eid=2-s2.0-84878361172&partnerID=40&md5=69cc3777ed9f5329ae75e510b93db2ef. [ Links ]
8. Jawad H, Hodson NA, Nixon PJ. A review of dental treatment of head and neck cancer patients, before, during and after radiotherapy: part 1. British Dental Journal. 2015;218(2):65-8. Available from: http://dx.doi.org/10.1038/sj.bdj.2015.28. [ Links ]
9. Shavi GR, Thakur B, Bhambal A, Jain S, Singh V, Shukla A. Oral Health Related Quality of Life in Patients of Head and Neck Cancer Attending Cancer Hospital of Bhopal City, India. Journal of International Oral Health: JIOH. 2015;7(8):21-7. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4588784&tool=pmcentrez&rendertype=abstract. [ Links ]
10. Jablonski RA. Oral Health and Hygiene Content in Nursing Fundamentals Textbooks. Nursing Research and Practice, vol. 2012, Article ID 372617, 7 pages. 2012; Available from: https://www.researchgate.net/publication/224919846_Oral_Health_and_Hygiene_ Content_in_Nursing_Fundamentals_Textbooks. [ Links ]
11. Bhayat A, Chikte U. The changing demographic profile of dentists and dental specialists in South Africa: 2002-2015. International Dental Journal. 2017;1-6. Available from: http://doi.wiley.com/10.1111/idj.12332. [ Links ]
12. Ramphoma KJ. Oral Health in South Africa: Exploring the role of dental public health specialists . South African Dental Journal, 71(9), pp. 402-403. Available at: http://www.scielo.org.za/pdf/sadj/v71n9/05.pdf. [ Links ]
13. Singh S, Myburgh NG, Lalloo R. Policy analysis of oral health promotion in South Africa. Global Health Promotion. 2010;17(1):16-24. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20357348. [ Links ]
14. Chi AC, Day TA, Neville BW. Oral Cavity and Oropharyngeal Squamous Cell Carcinoma-An Update. CA Cancer J Clin. 2015;65:401-21. [ Links ]
15. Aaronson N, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez N, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute. 1993;85(5):365-76. [ Links ]
16. Bjordal K, de Graeff A, Fayers P., Hammerlid E, van Pottelsberghe C, Curran D, et al. A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35) in head and neck patients. European Journal of Cancer. 2000;36(14):1796-807. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0959804900001866 [ Links ]
17. Singer S, Ignacio J, Hofmeister A, KeszteDirk W-CC, Fisher SE, Galalae R, et al. Performance of the EORTC questionnaire for the assessment of quality of life in head and neck cancer patients EORTC QLQ-H&N35: a methodological review. Qual Life Res. 2013;22(8):1927-41. [ Links ]
18. Rettig EM, D'Souza G. Epidemiology of Head and Neck Cancer. Surg Oncol Clin N Am. 2015;24(3):379-96. Available from: http://dx.doi.org/10.1016/j.soc.2015.03.001. [ Links ]
19. Alam M, Siddiqui S, Perween R. Epidemiological profile of head and neck cancer patients in Western Uttar Pradesh and analysis of distributions of risk factors in relation to site of tumor. J Can Res Ther. 2017;13:430-5. Available from: http://www.cancerjournal.net/preprintarticle.asp?id=180687. [ Links ]
20. Joshi P, Dutta S, Chaturvedi P, Nair S. Head and Neck Cancers in Developing Countries. Rambam Maimonides Medical Journal. 2014;5(2):e0009:1-6. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4011474&tool=pmcentrez&rendertype=abstract. [ Links ]
21. National Cancer Registry. Cancer in South Africa 2013 Full Report. 2013. Available from: http://www.nioh.ac.za/assets/files/2013NCR.pdf. [ Links ]
22. Parkin DM, Bray F, Ferlay J, Pisani P. Global Cancer Statistics, 2002. CA Cancer Journal for Clinicians. 2005;55(2):74-108. [ Links ]
23. Carlsen K, Dalton SO, Diderichsen F, Johansen C. Risk for unemployment of cancer survivors: A Danish cohort study. European Journal of Cancer. 2008;44(13):1866-74. [ Links ]
24. Stokman M, Burlage F, Spijkervet F. The effect of a calcium phosphate mouth rinse on (chemo) radiation induced oral mucositis in head and neck cancer patients: a prospective study. International Journal of Dental Hygiene. 2012;10(3):175-80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23046006. [ Links ]
25. Maria O., Eliopoulos N, Muanza T. Radiation-Induced Oral Mucositis. Frontiers in Oncology. 2017; 7, 89. Available from: http://journal.frontiersin.org/article/10.3389/fonc.2017.00089/full. [ Links ]
26. Pattanayak L, Panda N, Dash MK, Mohanty S, Samantaray S. Management of Chemoradiation-Induced Mucositis in Head and Neck Cancers With Oral Glutamine. Journal of Global Oncology. 2016;2(4):200-6. Available from: http://jgo.ascopubs.org/cgi/doi/10.1200/JGO.2015.000786. [ Links ]
27. Starmer HM. Dysphagia in head and neck cancer: prevention and treatment. Current Opinion in Otolaryngology and Head and Neck Surgery. 2014;22:195-200. [ Links ]
28. Johnson J, Johansson M, Rydén A, Houltz E, Finizia C. Impact of trismus on health-related quality of life and mental health. Head and Neck. 2015;37(11):1672-1679. Accepted article. Available from: http://doi.wiley.com/10.1002/hed.23816. [ Links ]
29. Steiner F, Evans J, Marsh R, Rigby P, James S, Sutherland K, et al. Mouth opening and trismus in patients undergoing curative treatment for head and neck cancer. International Journal of Oral and Maxillofacial Surgery. 2015;44(3):292-6. Available from: http://dx.doi.org/10.1016/j.ijom.2014.12.009. [ Links ]
30. Rapidis AD, Dijkstra PU, Roodenburg JLN, Rodrigo JP, Rinaldo A, Strojan P, et al. Trismus in patients with head and neck cancer: etiopathogenesis, diagnosis and management. Clinical Otolaryngology. 2015;40(6):516-26. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26098612%0A http://doi.wiley.com/10.1111/coa.12488 [ Links ]
31. Beetz I, Schilstra C, Burlage F, Koken P, Doornaert P, Bijl H, et al. Development of NTCP models for head and neck cancer patients treated with three-dimensional conformal radiotherapy for xerostomia and sticky saliva: The role of dosimetric and clinical factors. Radiotherapy and Oncology. 2012;105(1):86-93. Available from: http://dx.doi.org/10.1016/j.radonc.2011.05.010. [ Links ]
32. Villa A, Connell CL, Abati S. Diagnosis and management of xerostomia and hyposalivation. Therapeutics and Clinical Risk Management. 2015;11:45-51. [ Links ]
33. Sultana N, Sham EM. Xerostomia : An overview. International Journal of Dental Clinics. 2011;3(2):58-61. [ Links ]
34. Irune E, Dwivedi RC, Nutting CM, Harrington KJ. Treatment-related dysgeusia in head and neck cancer patients. Cancer Treatment Reviews. 2014;40:1106-17. Available from: http://dx.doi.org/10.1016/j.ctrv.2014.06.011. [ Links ]
35. Najafizade N, Hemati S, Gookizade A, Berjis N, Hashemi M, Vejdani S, et al. Preventive effects of zinc sulfate on taste alterations in patients under irradiation for head and neck cancers: A randomized placebo-controlled trial. Journal of Research in Medical Sciences: Official Journal of Isfahan Univiversity of Medical Sciences. 2013;18(2):123-6. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3724372&tool=pmcentrez&r endertype=abstract. [ Links ]
36. Murtaza B, Hichami A, Khan A., Ghiringhelli F, Khan N. Alteration in Taste Perception in Cancer: Causes and Strategies of Treatment. Frontiers in Physiology. 2017;8:134. [ Links ]
 Correspondence:
Correspondence:
Shenuka Singh
Discipline of Dentistry, School of Health Sciences
University of KwaZulu-Natal.
Tel: 031-2608591, Fax: 031-2608069
E-mail: singhshen@ukzn.ac.za
Author contributions:
1 . BS Bauluck-Nujoo: 70%
2 . S Singh: 30%














